Abstract
Background
Striking geographic variations in prostate cancer incidence suggest an aetiological role for spatially-distributed factors. We assessed whether neighbourhood social deprivation, which can reflect limited social contacts, unfavourable lifestyle and environmental exposures, is associated with prostate cancer risk.
Methods
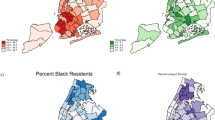
In 2005–2012, we recruited 1931 incident prostate cancer cases and 1994 controls in a case–control study in Montreal, Canada. Lifetime residential addresses were linked to an area-based social deprivation index around recruitment (2006) and about 10 years earlier (1996). Logistic regression estimated adjusted odds ratios (ORs) and 95% confidence intervals (CIs).
Results
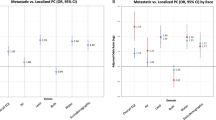
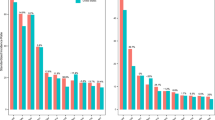
Men residing in areas characterised by greater social deprivation had elevated prostate cancer risks (ORs of 1.54 and 1.60 for recent and past exposures, respectively; highest vs lowest quintiles), independently from area- and individual-level confounders and screening patterns. The increase in risk with recent high social deprivation was particularly elevated for high-grade prostate cancer at diagnosis (OR 1.87, 95% CI 1.32–2.64). Associations were more pronounced for neighbourhoods with higher proportions of separated/divorced or widowed individuals in the past, and with higher percentages of residents living alone recently.
Conclusions
These novel findings, suggesting that neighbourhood-level social deprivation increases the risk of prostate cancer, point out to potential targeted public health interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on reasonable request from the corresponding author, in keeping with ethics regulations. The data are not publicly available for confidentiality reasons.
Code availability
Code is available from the authors upon request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Société canadienne du cancer. Comité consultatif des statistiques canadiennes sur le cancer. Statistiques canadiennes sur le cancer 2021. Toronto (Ontario): Société canadienne du cancer; 2021.
Thun M, Linet MS, Cerhan JR, Haiman CA, Schottenfeld D. Cancer epidemiology and prevention, fourth edition. Oxford: Oxford University Press; 2017.
Conti DV, Darst BF, Moss LC, Saunders EJ, Sheng X, Chou A, et al. Trans-ancestry genome-wide association meta-analysis of prostate cancer identifies new susceptibility loci and informs genetic risk prediction. Nat Genet. 2021;53:65–75.
Klassen AC, Platz EA. What can geography tell us about prostate cancer? Am J Prev Med. 2006;30:S7–15.
Lee J, Demissie K, Lu SE, Rhoads GG. Cancer incidence among Korean-American immigrants in the United States and native Koreans in South Korea. Cancer Control. 2007;14:78–85.
Shimizu H, Ross RK, Bernstein L, Yatani R, Henderson BE, Mack TM. Cancers of the prostate and breast among Japanese and white immigrants in Los Angeles County. Br J Cancer. 1991;63:963–6.
Townsend P. Deprivation. J Soc Policy. 1987;16:125–46.
Madathil S, Blaser C, Nicolau B, Richard H, Parent ME. Disadvantageous socioeconomic position at specific life periods may contribute to prostate cancer risk and aggressiveness. Front Oncol. 2018;8:515.
Nicolau B, Arekunnath Madathil S, Castonguay G, Rousseau MC, Parent ME, Siemiatycki J. Shared social mechanisms underlying the risk of nine cancers: a life course study. Int J Cancer. 2018;144:59–67.
Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20:417–35.
Marså K, Johnsen NF, Bidstrup PE, Johannesen-Henry CT, Friis S. Social inequality and incidence of and survival from male genital cancer in a population-based study in Denmark, 1994-2003. Eur J Cancer. 2008;44:2018–29.
Nilsen TIL, Johnsen R, Vatten LJ. Socio-economic and lifestyle factors associated with the risk of prostate cancer. Br J Cancer. 2000;82:1358–63.
Steenland K, Rodriguez C, Mondul A, Calle EE, Thun M. Prostate cancer incidence and survival in relation to education (United States). Cancer Causes Control. 2004;15:939–45.
Mihor A, Tomsic S, Zagar T, Lokar K, Zadnik V. Socioeconomic inequalities in cancer incidence in Europe: a comprehensive review of population-based epidemiological studies. Radio Oncol. 2020;54:1–13.
DeRouen MC, Schupp CW, Yang J, Koo J, Hertz A, Shariff-Marco S, et al. Impact of individual and neighborhood factors on socioeconomic disparities in localized and advanced prostate cancer risk. Cancer Causes Control. 2018;29:951–66.
Eylert MF, Bahl A, Hounsome L, Verne J, Jefferies ER, Persad RA. The impact of socio-economic deprivation on incidence, treatment and mortality from prostate cancer in England, 1990–2010. J Clin Urol. 2015;9:93–101.
Rundle A, Neckerman KM, Sheehan D, Jankowski M, Kryvenko ON, Tang D, et al. A prospective study of socioeconomic status, prostate cancer screening and incidence among men at high risk for prostate cancer. Cancer Causes Control. 2013;24:297–303.
Salmon C, Song L, Muir K, Pashayan N, Dunning AM, Batra J, et al. Marital status and prostate cancer incidence: a pooled analysis of 12 case-control studies from the PRACTICAL consortium. Eur J Epidemiol. 2021;36:913–25.
Coughlin SS. A review of social determinants of prostate cancer risk, stage, and survival. Prostate Int. 2020;8:49–54.
Wu Z, Nguyen NH, Wang D, Lynch BM, Hodge AM, Bassett JK, et al. Social connectedness and mortality after prostate cancer diagnosis: a prospective cohort study. Int J Cancer. 2019;147:766–76.
Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. 2010;51:S54–66.
Tangen CM, Goodman PJ, Till C, Schenk JM, Lucia MS, Thompson IM Jr. Biases in recommendations for and acceptance of prostate biopsy significantly affect assessment of prostate cancer risk factors: results from two large randomized clinical trials. J Clin Oncol. 2016;34:4338–44.
Parent ME, Goldberg MS, Crouse DL, Ross NA, Chen H, Valois MF, et al. Traffic-related air pollution and prostate cancer risk: a case-control study in Montreal, Canada. Occup Environ Med. 2013;70:511–8.
Blanc-Lapierre A, Spence A, Karakiewicz PI, Aprikian A, Saad F, Parent M. Metabolic syndrome and prostate cancer risk in a population-based case-control study in Montreal, Canada. BMC public health. 2015;15:913.
Environmental Systems Research Institute Inc. (ESRI). ArcGIS Desktop 9.3.1. Redlands: ESRI Inc.; 2009.
Pampalon R, Hamel D, Gamache P, Raymond G. A deprivation index for health planning in Canada. Chronic Dis Can. 2009;29:178–91.
Pampalon R, Hamel D, Gamache P, Simpson A, Philibert M. Validation of a deprivation index for public health: a complex exercise illustrated by the Quebec index. Chronic Dis Inj Can. 2014;34:12–22.
Salinas CA, Tsodikov A, Ishak-Howard M, Cooney KA. Prostate cancer in young men: an important clinical entity. Nat Rev Urol. 2014;11:317–23.
Wright JL, Salinas CA, Lin DW, Kolb S, Koopmeiners J, Feng Z, et al. Prostate cancer specific mortality and Gleason 7 disease differences in prostate cancer outcomes between cases with Gleason 4 + 3 and Gleason 3 + 4 tumors in a population based cohort. J Urol. 2009;182:2702–7.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–99.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167:268–74.
Hurwitz LM, Agalliu I, Albanes D, Barry KH, Berndt SI, Cai Q, et al. Recommended definitions of aggressive prostate cancer for etiologic epidemiologic research. J Natl Cancer Inst. 2021;113:727–34.
Shafique K, Oliphant R, Morrison DS. The impact of socio-economic circumstances on overall and grade-specific prostate cancer incidence: a population-based study. Br J Cancer. 2012;107:575–82.
Klassen AC, Curriero FC, Hong JH, Williams C, Kulldorff M, Meissner HI, et al. The role of area-level influences on prostate cancer grade and stage at diagnosis. Prev Med. 2004;39:441–8.
Seo HS, Lee NK. Predictors of PSA screening among men over 40 years of age who had ever heard about PSA. Korean J Urol. 2010;51:391–7.
Fone DL, Farewell DM, White J, Lyons RA, Dunstan FD. Socioeconomic patterning of excess alcohol consumption and binge drinking: a cross-sectional study of multilevel associations with neighbourhood deprivation. BMJ Open. 2013;3:e002337.
Lakshman R, McConville A, How S, Flowers J, Wareham N, Cosford P. Association between area-level socioeconomic deprivation and a cluster of behavioural risk factors: cross-sectional, population-based study. J Public Health. 2011;33:234–45.
Xiao Q, Keadle SK, Berrigan D, Matthews CE. A prospective investigation of neighborhood socioeconomic deprivation and physical activity and sedentary behavior in older adults. Prev Med. 2018;111:14–20.
Curtis S, Setia MS, Quesnel-Vallee A. Socio-geographic mobility and health status: a longitudinal analysis using the National Population Health Survey of Canada. Soc Sci Med 2009;69:1845–53.
Hamano T, Li X, Sundquist J, Sundquist K. Neighborhood social capital and incidence and mortality of prostate cancer: a Swedish cohort study. Aging Clin Exp Res. 2021;33:3333–42.
Lynch SM, Mitra N, Ross M, Newcomb C, Dailey K, Jackson T, et al. A Neighborhood-Wide Association Study (NWAS): example of prostate cancer aggressiveness. PLoS ONE. 2017;12:e0174548.
Macintyre S, Ellaway A. Neighborhoods and health: an overview. Neighborhoods Health. 2003;20:42.
VanderWeele DJ, Brown CD, Taxy JB, Gillard M, Hatcher DM, Tom WR, et al. Low-grade prostate cancer diverges early from high grade and metastatic disease. Cancer Sci. 2014;105:1079–85.
Penney KL, Stampfer MJ, Jahn JL, Sinnott JA, Flavin R, Rider JR, et al. Gleason grade progression is uncommon. Cancer Res. 2013;73:5163–8.
World Cancer Research Fund International, American Institute to Cancer Research. Diet, nutrition, physical activity and prostate cancer. 2014. https://dietandcancerreport.org.
Gilham K, Gu Q, Dummer TJB, Spinelli JJ, Murphy RA. Diet quality and neighborhood environment in the Atlantic Partnership for Tomorrow’s Health Project. Nutrients. 2020;12:3217.
Ngamini Ngui A, Apparicio P, Philibert M, Fleury M-J. Neighborhood characteristics associated with the availability of alcohol outlets in quebec, Canada. J Addict. 2015;2015:876582-.
Crouse DL, Ross NA, Goldberg MS. Double burden of deprivation and high concentrations of ambient air pollution at the neighbourhood scale in Montreal, Canada. Soc Sci Med. 2009;69:971–81.
Pinault L, Crouse D, Jerrett M, Brauer M, Tjepkema M. Spatial associations between socioeconomic groups and NO2 air pollution exposure within three large Canadian cities. Environ Res. 2016;147:373–82.
Short H, Al Sayah F, Ohinmaa A, Lahtinen M, Johnson JA. The relationship of neighbourhood-level material and social deprivation with health-related quality of life. Qual Life Res. 2018;27:3265–74.
McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–9.
Reiche EM, Nunes SO, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004;5:617–25.
Keyes KM, Hatzenbuehler ML, Grant BF, Hasin DS. Stress and alcohol: epidemiologic evidence. Alcohol Res Curr Rev. 2012;34:391–400.
Zellner DA, Loaiza S, Gonzalez Z, Pita J, Morales J, Pecora D, et al. Food selection changes under stress. Physiol Behav. 2006;87:789–93.
Gamache P, Hamel D, Blaser C. Material and social deprivation index: a summary. 2019. https://www.inspq.qc.ca/publications/2639.
Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–78.
Leech JA, Nelson WC, Burnett RT, Aaron S, Raizenne ME. It’s about time: a comparison of Canadian and American time–activity patterns. J Expo Sci Environ Epidemiol. 2002;12:427–32.
Garcia-Closas M, Berrington, de Gonzalez A. Invited commentary: Screening and the elusive etiology of prostate cancer. Am J Epidemiol. 2015;182:390–3.
Acknowledgements
The authors would like to thank all members of the Epidemiology and Biostatistics Unit at INRS-Centre Armand-Frappier Santé Biotechnologie who were involved in the conduct of the study. In particular, we want to highlight the contribution of Hughes Richard in the preparation of the databases. We also thank the urologists from the participating hospitals for their collaboration in patients’ access.
Funding
This work was supported financially by the Canadian Institutes of Health Research (grant CCP-155423) and the Canadian Cancer Society (grant 705562). CS held doctoral training awards from the Fonds de recherche du Québec – Santé.
Author information
Authors and Affiliations
Contributions
CS conducted the analysis, interpreted the results and prepared the manuscript. M-EP supervised the work, designed and conducted the PROtEuS study and reviewed the manuscript. All authors participated in the interpretation of data and have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All individual studies were approved by local ethics committees and adhered to the principles of the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salmon, C., Quesnel-Vallée, A., Barnett, T.A. et al. Neighbourhood social deprivation and risk of prostate cancer. Br J Cancer 129, 335–345 (2023). https://doi.org/10.1038/s41416-023-02299-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02299-7