Abstract
Antenatal screening and diagnostic testing for Down syndrome has greatly advanced over the past 30 years. The goal of this manuscript is to provide a review of the availability and accessibility of prenatal services and selective termination policies across Europe, Australia, New Zealand, and the United States for the period 1990–2021. We collected data from academic peer-reviewed journals, governmental documents, not-for-profit organizations, correspondence with experts, and other online sources without language restrictions. Prenatal screening services from 1990–2021 became increasingly available across countries, enabling expectant couples the opportunity to gain more accurate information earlier in the pregnancy before assuming the risk associated with more invasive techniques like CVS or amniocentesis. Many countries also began adopting prenatal screening as a qualification for prenatal diagnosis. As of 2021, at least 76.9% of countries offered full coverage for diagnostic testing for Down syndrome from government funding. Abortion coverage for a Down syndrome diagnosis was covered fully by government funding in 52.4% of countries in 1990, increasing to 73.8% in 2021. Understanding the changing landscape of prenatal services builds the foundation for future investigation into social policies that affect the prevalence of Down syndrome.
Similar content being viewed by others
Introduction
Technological advances in antenatal screening and diagnostic testing for Down syndrome (DS) mean that expectant couples have earlier and more accurate opportunities to gain insights about their pregnancies. Procedures such as chorionic villus sampling (CVS, commonly performed during first trimester) and amniocenteses (commonly performed during second trimester) have a >99% accuracy, albeit with small, yet real, chances for procedure-related miscarriage [1]. Prenatal screening practices have expanded in recent years to provide indications for when such invasive procedures might be warranted. Non-invasive prenatal screening (NIPS) is the newest form of prenatal screening that isolates cell-free DNA from a simple maternal blood sample [2].
This review provides an overview of the availability of these prenatal services across Europe, Australia, New Zealand, and the United States for the period 1990–2021. While other papers have compiled information on prenatal services provided by countries at a specific time point, we sought to compile multiple sources for each country across a broad timeline. For example, International Planned Parenthood Federation published a collection on abortion legislation in Europe; however, this document details current legislation and focuses only on abortion [3]. Another document created by Eurocat, focuses on prenatal screening policies around Europe [4]. These documents are examples of the collection of information on prenatal policy which is limited to specific years and typically only one type of prenatal service.
This review will allow for qualitative comparisons between countries and their social policies. The availability and financial subsidization of prenatal screening, diagnosis, and termination practices certainly contribute to the prevalence of DS and will be the primary focus of this paper. As the maternal age of a population increases so, too, would the nonselective live birth prevalence for DS increase [5,6,7]. Genetic counseling may also influence pregnancy decision making. Many European countries, for example, have made genetic counseling mandatory and fully subsidized in the prenatal context. The availability and content of this counseling might influence uptake of screening and subsequent actions of expectant parents. Social perception of disabilities and societal laws around reproductive autonomy may also contribute to live birth prevalence for DS. This review lays the foundational work for future studies aimed at understanding the impact of all of these potential contributing factors on the patterns of DS prevalence in different countries.
Materials and methods
We sought a review of information on these questions: is elective abortion free from costs for pregnant women? Are amniocentesis/CVS offered to pregnant women? If amniocentesis/CVS is available, is it free from costs for the pregnant woman? Does the country offer screening tests for DS? If screening tests for DS are available, are these free of cost for the pregnant woman?
Our search for information was extensive. The process for collection of data points was carried out through reviewing literature from journals, governmental documents, not for profit organizations, correspondence with experts and other online sources without language restrictions. Pubmed searches were guided using MeSH search feature with key words including: “[Country],” “Down Syndrome,” “Prenatal Diagnosis,” “Nuchal Translucency,” “Maternal Serum Screening,” “NIPS,” and “NIPT.” The reference section of the manuscripts found through these Pubmed searches were also further analyzed for additional relevant articles. Web searches carried out through Google utilized search terms such as: “[Country],” “Down Syndrome,” “Availability,” “Cost,” “History,” “Abortion,” “Prenatal Diagnosis,” “Prenatal Screening,” “Maternal Serum Screening,” “NIPS,” and “NIPT.” Sources identified through these searches often led to additional source material. One hundred and ninety-three sources were identified through this method in at least four different languages as pertinent material on the topic. Each region of Europe referenced between eighteen to thirty-three sources. Furthermore, we reached out to experts in prenatal services in countries where information was limited and had seven individuals provide correspondence on their country. Experts were found through Down syndrome advocacy organizations in the respective country of interest.
Information was synthesized to answer each of our framing questions, per country, from 1990–2021. In cases where information was incomplete after extensive searches, extrapolations were made to the next known timepoint. Sources that referenced screening or testing tangentially but did not include any reference to the capacity at which it is offered were excluded from our analysis.
Results
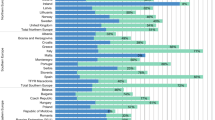
The majority of countries had gestational age limits for DS-selective terminations after twelve weeks (Supplementary Materials Table 1). Abortion coverage for a Down syndrome diagnosis was covered fully by government funding in 52.4% of countries in 1990, increasing to 73.8% in 2021 (Figs. 1, 2). The seven countries that changed from no coverage to full coverage in this time period were: Belgium, Estonia, Ireland, Montenegro, Serbia, Hungary, and Republic of Moldova. One country which shifted from full coverage to none is Poland, which recently passed laws restricting access to abortions services.
Full = full government-provided coverage for the population for which selective abortion for DS is made available; Partial = (a) partial government-provided coverage for the population for which selective abortion for DS is made available or (b) government-provided coverage for only part of the population for which selective abortion for DS is made available; None = no government-provided coverage.
Full = full government-provided coverage for the population for which selective abortion for DS is made available; Partial = (a) partial government-provided coverage for the population for which selective abortion for DS is made available or (b) government-provided coverage for only part of the population for which selective abortion for DS is made available; None = no government-provided coverage.
Prenatal screening services from 1990–2021 became increasingly available across countries (Supplementary Materials Table 2). A typical pattern of screening adoption within a country progressed from nuchal translucency ultrasonographic screening to biochemical screening practices and then to non-invasive prenatal screening, especially within the last decade. In 1990, 73.8% of counties had some form of screening available (Supplementary Materials Table 2). By 2021, every country with data available had some form of screening available (Supplementary Materials Table 2). Coverage of prenatal screening remained relatively stable from 1990 to 2002, before increased adoption of coverage began. Increased coverage, when occurring, mostly came from countries shifting from no coverage to full-coverage situations (Figs. 3, 4). The indications for prenatal diagnostic testing shifted in the 1990s to 2010s from mainly age-based indications toward the inclusion of other risk factors from prenatal screens. More women have thus gained access to conclusive diagnostic testing as a result of more inclusive indications for referral. Coverage of diagnostic testing for DS remained more or less stable throughout from 2000 to 2021, with at least 67% of countries offering full coverage from government funding (Figs. 5, 6). Only Austria, Bosnia-Herzegovina, Bulgaria, Poland, and Romania, and New Zealand increased their coverage of diagnostic procedures over the twenty year period.
Full = full government-provided coverage for the population for which amniocentesis or CVS is made available; Partial = (a) partial government-provided coverage for the population for which amniocentesis or CVS is made available or (b) government-provided coverage for only part of the population for which amniocentesis or CVS is made available; None = no government-provided coverage.
Full = full government-provided coverage for the population for which amniocentesis or CVS is made available; Partial = (a) partial government-provided coverage for the population for which amniocentesis or CVS is made available or (b) government-provided coverage for only part of the population for which amniocentesis or CVS is made available; None = no government-provided coverage.
Discussion
Gestational age limits and government coverage of abortion in the case of a Down syndrome diagnosis
Our data showed that for the majority of European countries abortion was legal for a prenatal diagnosis of DS. Such abortions for “genetic anomalies” or “medical reasons” were often made possible by policy extensions past the typical gestational limit for nonselective abortions. As such, there is an extended period of time for expectant couples to terminate a pregnancy because of a prenatal diagnosis of DS in many countries.
Full governmental funding for selective abortions also increased over time—from 52.4% of studied countries in 1990 to 73.8% in 2021. Focusing on European countries only, there was an increase from 51.3% of countries in 1990 to 74.4% in 2021. Using the published population numbers within Europe, the calculated percentage of the total population in these countries with full coverage of abortion services was about 81.2% in 1990 and 91.1% in 2021 (see Supplementary Materials for calculation) [8]. This represents still some increase in individuals with financial coverage to abortion services. Expectant persons in most European countries do not currently face any financial barriers if they wish to pursue a DS-selective termination. In those European countries with no access to abortion services, individuals may be able to travel to other countries to access such services, but likely at their own expense. There are no such financial barriers for women in Australia and New Zealand. In the United States financial restrictions still exist for many persons [9,10,11,12]. An open question for future research remains whether these policy shifts have had an impact on the birth prevalence of people with DS. An open ethical question asks whether such governmental funding implicitly pressures expectant couples to pursue what might be perceived as a routinized outcome.
Available technology and government coverage for Down syndrome screening
Prenatal screening techniques have technologically advanced over the course of the timeline our study covered. The most common screening methods available in 1990 were nuchal translucency ultrasonographic screening and biochemical screening. Over the next two decades, triple/combined tests were introduced, incorporating multiple screens to determine a more accurate estimate of DS antenatally. More recently has been the incorporation of NIPS. In almost all countries surveyed, the techniques offered by healthcare providers advanced during this twenty-year period. This increased availability of screening techniques offers expectant couples the opportunity to gain more accurate information earlier in the pregnancy before assuming the risk associated with more invasive techniques like CVS or amniocentesis.
Governmental funding for prenatal screening increased only slightly over the period of interest. One potential reason may be due to the relatively new development of these techniques. Many of the screening practices introduced during the past twenty years may take more time to be incorporated into the health coverage of countries that may still be skeptical of their effectiveness. Another reason might be that some countries do not have the resources to fully cover prenatal screening for the full population, thereby limiting coverage to expectant women with certain risk factors. This barrier might lessen as the costs of prenatal testing technologies decrease in the future. Countries might also make intentional decisions not to cover prenatal screening based on social beliefs or principles. As NIPS companies continue to expand their direct-to-consumer advertisements, however, more expectant couples might be influenced to call upon their governments to subsidize such testing. Equally important, then, will be the need to subsidize associated genetic counseling services.
Many expectant couples opt to pursue pre-test or post-test genetic counseling, which can have an impact on other decisions made during their pregnancy. Genetic counseling is often provided by a medical geneticist, genetic counselor, maternal-fetal medicine physician, or another trained clinician. Historic and systematic information about the availability and coverage for genetic counseling is not within the scope of this paper but does play a role in expectant parents’ decisions regarding testing. Further research efforts can and should take a look at the evolution and subsidization of genetic counseling practices over time and location. Counseling might influence parental decisions. However, prior research has indicated that expectant parents indicate that only about 16% of patients in a cohort of 181 chose whether to utilize NIPS or PND in accordance with the perceived preference of their physician [13]. Nevertheless some expectant parents who decided to continue their pregnancy report that they experienced implicit or explicit pressure to terminate [14, 15]. Furthermore the way prenatal screening services are framed can influence uptake [16]. In the Netherlands, Denmark, and the United Kingdom, differences in genetic counseling practices have been shown to influence the uptake of screening tests [16]. In the Netherlands, where prenatal screening is used considerably less than in Denmark and the UK, researchers believe that the cost of screening and the “right not to know” have impact [16]. The “right not to know” is a practice written into law in the Netherlands that gives the patient ownership over what information will be obtained and delivered to them, especially by genetic counselors. Expectant couples are informed of their right to refrain from certain knowledge prior to genetic screening, a conversation that is centered around a couple’s value system and the statistical outcomes of offered prenatal tests. In contrast, in Denmark –a country with a very high uptake– the offer of prenatal screening is positively framed, both in the social context of family, friends and neighbors, as at the service delivery level [16].
Access to and coverage of prenatal diagnosis for Down syndrome
Prenatal diagnostic testing such as amniocentesis and chorionic villus sampling have largely been available since 1990. However, these tests have been restricted to specific women on the basis of risk factors. Most countries that restricted access to prenatal diagnostic testing typically used maternal age as the risk factor to determine whether a woman would be referred for testing or not. Over the past three decades, the indicators for referral have been expanded or replaced for many countries to include prenatal screening risk assessments. There are increasingly more situations where some expectant couples now first opt for prenatal screening whereas previously they would have started with a CVS or amniocentesis, when age-only criteria were in place. Accordingly, the number of invasive procedures for “maternal age” has dropped steeply. Depending on the prenatal screen used, there will be “false negatives” expected, and such couples might not pursue subsequent diagnostic testing. At the same time, in light of the increased access to prenatal screening, especially for younger pregnant women, there will be more “positive results” on prenatal screens, and, as such, more expectant couples will now have access to CVS and amniocentesis for follow-up testing. This effect is likely to be dominant. During the past two decades, governmental funding for diagnostic testing slightly increased; the majority of countries had already been offering full coverage since 1990.
All of these changes over time suggest that more fetuses with DS are being identified prenatally. More fetuses with DS that are identified may mean that an increased rate of selective terminations for DS may take place. For example, in the United States, whereas the number of potential live births of children with DS (absent DS-related elective terminations) had increased by 38% between 1990 and 2015, there was an approximate 114% increase in the number of DS-related selective terminations in the same period [6, 7, 17]. In Europe, whereas the number of potential live births of children with DS had increased by 44% between 1991 and 2015, there was an approximately 347% increase in the number of selective terminations in the same period [7].
The availability and accessibility of prenatal testing and genetic counseling certainly have an impact on the number of live births with DS. In addition, there is a risk of routinization of prenatal screening, where parents are no longer facilitated to make informed decisions based on their own moral and practical considerations, but counselors, family, and friends alike, implicitly or explicitly expect that couples will choose prenatal screening, diagnostic testing, and, ultimately termination of pregnancy [14]. Such potential societal pressure may increase the effect of the availability of prenatal screening on the live birth rate of children with DS. Other factors—such as religious beliefs, economics, changing maternal ages, cultural beliefs, and social norms—likely play additional roles. The anticipated quality of life for a person with DS might also be an important consideration in the decision-making for some expectant couples [14]. While the genetics of people with DS are the same across countries, the social potential varies widely based on a country’s support and resources for neurodiversity. As a consequence, some expectant couples might either consciously or subconsciously have a “projection bias,” a forecast of what the future might be like for their fetus prenatally diagnosed with DS. Some forecasts, however, may be inaccurate due to anchoring in the present emotional or motivational state or informed by outdated information or experiences [18]. Genetic counseling, when practiced ideally, is meant to provide expectant persons with accurate, up-to-date, balanced information so that informed decisions could be made. Research from the United States and the Netherlands has demonstrated that sometimes expectant couples feel such counseling falls short—sometimes perceived as biased, incomplete, and outdated [14, 15, 19, 20]. Future research will be necessary in order to understand the synergistic impact that all of these factors have on the overall number of live births with DS.
Data availability
All data generated or analyzed during this study are included in this published article and its Supplementary Information files.
Code availability
All data generated or analyzed during this study are included in this published article and its Supplementary Information files.
References
American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 88, December 2007. Invasive prenatal testing for aneuploidy. Obstet Gynecol. 2007;110:1459–67.
Norwitz ER, Levy B. Noninvasive prenatal testing: the future is now. Rev Obstet Gynecol. 2013;6:48–62.
Abortion Legislation In Europe: Updated January 2012 [Internet]. IPPF European Network; 2012 [cited 2021 Jul 15]. Available from: https://europe.ippf.org/resource/abortion-legislation-europe.
Special Report: Prenatal Screening Policies in Europe [Internet]. EUROCAT Central Registry, University of Ulster; 2010 [cited 2021 Jul 9]. Available from: https://www.orpha.net/actor/Orphanews/2010/doc/Special-Report-Prenatal-Screening-Policies.pdf.
de Graaf G, Skladzien E, Buckley F, Skotko BG. Estimation of the number of people with Down syndrome in Australia and New Zealand. Genet Med. 2022;24:2568–77.
de Graaf G, Buckley F, Skotko BG. Estimates of the live births, natural losses, and elective terminations with Down syndrome in the United States. Am J Med Genet A. 2015;167:756–67.
de Graaf G, Buckley F, Skotko BG. Estimation of the number of people with Down syndrome in Europe. Eur J Hum Genet. 2021;29:402–10.
World Population Prospects - Population Division - United Nations [Internet]. [cited 2022 Mar 29]. Available from: https://population.un.org/wpp/Download/Standard/Population/.
Access Denied: Origins of the Hyde Amendment and Other Restrictions on Public Funding for Abortion [Internet]. American Civil Liberties Union. [cited 2021 Jul 16]. Available from: https://www.aclu.org/other/access-denied-origins-hyde-amendment-and-other-restrictions-public-funding-abortion.
Abortion and Medicare - Children by Choice [Internet]. [cited 2021 Oct 11]. Available from: https://www.childrenbychoice.org.au/factsandfigures/abortionandmedicare.
Interactive NV. Decide: National Abortion Telehealth Service, FAQ [Internet]. Decide – National Abortion Telehealth Service. [cited 2022 May 17]. Available from: (https://www.nvinteractive.com/) https://www.decide.org.nz/en/faqs/.
2021. The Hyde Amendment and Coverage for Abortion Services [Internet]. KFF. 2021 [cited 2021 Jul 16]. Available from: https://www.kff.org/womens-health-policy/issue-brief/the-hyde-amendment-and-coverage-for-abortion-services/.
van der Steen SL, Houtman D, Bakkeren IM, Galjaard RJH, Polak MG, Busschbach JJ, et al. Offering a choice between NIPT and invasive PND in prenatal genetic counseling: the impact of clinician characteristics on patients’ test uptake. Eur J Hum Genet. 2019;27:235–43.
Crombag NM, Page-Christiaens GC, Skotko BG, de Graaf G. Receiving the news of Down syndrome in the era of prenatal testing. Am J Med Genet A. 2020;182:374–85.
Skotko BG. Prenatally diagnosed Down syndrome: mothers who continued their pregnancies evaluate their health care providers. Am J Obstet Gynecol. 2005;192:670–7.
Crombag NM, Vellinga YE, Kluijfhout SA, Bryant LD, Ward PA, Iedema-Kuiper R, et al. Explaining variation in Down’s syndrome screening uptake: comparing the Netherlands with England and Denmark using documentary analysis and expert stakeholder interviews. BMC Health Serv Res. 2014;14:437.
de Graaf G, Buckley F, Skotko B. People living with Down syndrome in the USA: BIRTHS AND POPULATION [Internet]. 2022 [cited 2022 Apr 22]. Available from: https://go.downsyndromepopulation.org/usa-factsheet.
Kahneman D, Thaler R. Anomalies: Utility Maximization and Experienced Utility. J Econ Perspect. 2006;20:221–34.
Allyse M, Aypar U, Bonhomme N, Darilek S, Dougherty M, Farrell R, et al. Offering prenatal screening in the age of genomic medicine: a practical guide. J Women’s Health 2002. 2017;26:755–61.
Skotko B, Bedia RC. Continuación del embarazo después de un diagnóstico prenatal de síndrome de Down. Estudio de cuatro casos. Diagn Trat Prenat. 2006;17:189–92.
Acknowledgements
We would like to thank and acknowledge Dr. Anila Laku from Mother Teresa Hospital & Emanuela Zaimi, MA., from Down Syndrome Albania Foundation for their aid in finding information on prenatal services in Albania; Marge Kato from Down Syndrome Association Estonia for her information on prenatal services in Estonia; Yuliya Dmytrenko from Ukraine Down Syndrome Organization for her information on prenatal services in Ukraine; Dr. Ellen Skladzien from Down Syndrome Australia and Dr. Melody Menezes Bsc, GDipGenetCouns, Ph.D., MHGSA from Monash Ultrasound for Women for their information on prenatal services in Australia; Zandra Vaccarino, National Executive Officer of the New Zealand Down Syndrome Association (NZDSA); Kate Alvrez from Family Planning New Zealand for her information on prenatal services in New Zealand; and Maria-Madalina Turza, President, European Centre for the Rights of Children with Disabilities for her information on prenatal services in Romania.
Funding
No funding was received for the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: GdG, HCW, PvC, FB, BGS; Data curation: HCW; Formal analysis: HCW; Funding Acquisition: n/a; Investigation: HCW; Methodology: HCW; Project Administration: HCW, BGS; Resources: n/a.; Software: HCW; Supervision: GdG, PvC, FB, BGS; Validation: HCW; Visualization: HCW: Writing-original draft: HCW, BGS; Writing-review & editing: GdG, HCW, PvC, FB, BGS.
Corresponding author
Ethics declarations
Competing interests
Dr. Skotko occasionally consults on the topic of Down syndrome through Gerson Lehrman Group. He receives remuneration from Down syndrome non-profit organizations for speaking engagements and associated travel expenses. Dr. Skotko receives annual royalties from Woodbine House, Inc., for the publication of his book, Fasten Your Seatbelt: A Crash Course on Down Syndrome for Brothers and Sisters. Within the past two years, he has received research funding from F. Hoffmann-La Roche, Inc. and LuMind Research Down Syndrome Foundation to conduct clinical trials for people with Down syndrome. Dr. Skotko is occasionally asked to serve as an expert witness for legal cases where Down syndrome is discussed. Dr. Skotko serves in a non-paid capacity on the Honorary Board of Directors for the Massachusetts Down Syndrome Congress and the Professional Advisory Committee for the National Center for Prenatal and Postnatal Down Syndrome Resources. Dr. Skotko has a sister with Down syndrome. Dr. de Graaf had a daughter with DS, who passed away in 2005 at the age of 15. He works as science and education officer at the Dutch Down Syndrome Foundation, a nonprofit organization. Frank Buckley serves as CEO of Down Syndrome Education International and Down Syndrome Education USA, nonprofits engaged in research and support for young people with Down syndrome. He had a sister with Down syndrome, who passed away in 2020. Dr. van Casteren has a daughter with Down syndrome. Henry Wilmot declares no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wilmot, H.C., de Graaf, G., van Casteren, P. et al. Down syndrome screening and diagnosis practices in Europe, United States, Australia, and New Zealand from 1990–2021. Eur J Hum Genet 31, 497–503 (2023). https://doi.org/10.1038/s41431-023-01330-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-023-01330-y