Abstract
Purpose
Choroidal metastases occur in many patients with systemic cancer and limit quality of life due to visual deterioration or pain. The limited prognosis of these patients demand treatment approaches that aim at a quick response and easy application. We evaluated a robotic assisted radiosurgery device, the CyberKnife, in the treatment of choroidal metastasis.
Methods
Following retrobulbar anaesthesia, target volume was defined by an interdisciplinary team using gadolinium-contrast-enhanced MRI, computer tomography (CT) as well as all previously obtained clinical data. Radiation was delivered in a single fraction with a CyberKnife at a radiation dose of 21 Gy with a 70% isodose. We evaluated tumour height, reflectivity, visual acuity and side effects over the course of the follow-up.
Results
A total of four patients were included in this report. Mean follow-up time was 31 months, and all patients showed decreased tumour volume and signs of fibrosis during follow-up. One patient remained stable in terms of visual acuity, two patients lost visual acuity and one patient improved and had a functional visual acuity at last follow-up. One patient developed radiation retinopathy with subsequent neovascular glaucoma that needed further management. All other patients did not show any signs of radiation induced side effects.
Conclusion
We report on the outcome of robotic CyberKnife radiosurgery in the treatment of uveal metastasis. We believe that single session, outpatient treatment delivery that can be facilitated with CyberKnife radiosurgery offer some benefits for this particularly sick group of patients.
Similar content being viewed by others
Introduction
Choroidal metastases (CM) are the most common malignant lesion in the eye and are reported to occur in 4–12% of patients with solid primary tumours, particularly secondary to breast and lung cancer [1, 2].
Most affected patients report deterioration of visual acuity including scotoma and blurred vision, yet many patients do not notice any symptoms which presumably make the number of patients with undetected CM even higher [3].
Patients who are diagnosed with choroidal metastasis are typically in their mid-50s and are aware of systemic cancer. The median time between diagnosis of the primary tumour and the occurrence of ocular metastasis is around 49 months [4]. In up to 30% of patients however, the diagnosis of choroidal metastasis precedes the diagnosis of any systemic cancer [5, 6].
Since many patients with CM are suffering from an advanced stage of their underlying systemic malignancy, complex treatment approaches for CM are often not reasonable. However, visual acuity diminishment is a severe burden for patients regardless of their life expectancy or disease stage. Treatment of CM should therefore aim at preserving or improving visual acuity on the one hand without evoking a heavy treatment burden on the other hand.
Once a complete oncologic staging has been undergone and other possible locations of metastases have been evaluated, treatment strategies should be discussed. In cases where systemic therapy does not lead to reduction of CM or if there is choroidal metastasis only and the patient’s visual acuity deteriorated due to the choroidal metastasis, localised treatment of the ocular lesion should be considered.
Different radiotherapeutic treatment options for CM have been evaluated and include brachytherapy with isotopes such as iodine-125 or ruthenium-106, external beam radiotherapy (EBRT), stereotactic radiosurgery (SRS) and proton beam therapy (PBT). Among these, EBRT using photons is the most commonly used option in the treatment of choroidal metastasis. While brachytherapy and PBT are well established treatment options in choroidal melanoma, they carry some disadvantages including the need for surgery and hospitalisation.
Robotic CyberKnife radiosurgery is one option in external-beam radiation therapy and has been successfully applied in the treatment of medium- and large-sized uveal melanomas [7,8,9]. CyberKnife can be facilitated in a single outpatient session and allows radiation settings that are possibly below the threshold that is typically being reported for side effects such as radiation retinopathy, papillopathy or neovascular glaucoma.
We report on Cyberknife robotic radiosurgery as a treatment approach in CM, its possible side effects, and clinical outcome in four patients.
Methods
A retrospective review of all patients that were diagnosed with CM and were treated with CyberKnife robotic radiosurgery at the Department of Ophthalmology of the Ludwig-Maximilians-University in Munich, Germany between 2014 and 2019 was performed. A minimum of 12 months follow-up time was necessary to be included in this evaluation. We recorded age, gender, visual acuity, number of lesions, central retinal thickness (CRT) as measured with optical coherence tomography (OCT). Furthermore, tumour thickness and reflectivity using A-scan standardised echography were recorded.
Upon first presentation, all patients received a full ophthalmologic examination, including assessment of best-corrected visual acuity, slit-lamp biomicroscopy, funduscopy, standardised A-/B-scan ultrasound and photo documentation. A complete oncologic workup was initiated at the time of first presentation to our department if not already done so and systemic therapy was started by the oncologist depending on the underlying condition.
Written informed consent was then obtained before treatment and risks and chances as well as other treatment modalities (PBT, plaque brachtytherapy) were discussed with the patient in detail. Each patient had ongoing treatment for primary cancer including chemotherapy, which was not interrupted. This study adhered to the tenets of the Declaration of Helsinki and obtained Institutional Review Board approval.
CyberKnife radiotherapy was performed as a standardised outpatient procedure as described previously [10]. In brief, standard retrobulbar anaesthesia was performed to achieve akinesia of the globe within the orbit. The treatment protocol was planned, created and critically reviewed by an interdisciplinary team of two radiation oncologists, two medical physicists and one specialised ophthalmologist. Target volume was defined using gadolinium-contrast-enhanced MRI, computer tomography (CT) (1.0 and 1.2 mm slices) as well as all previously obtained clinical data including widefield imaging, clinical examination and ultrasonography results. A non-isocentric inverse algorithm was used for treatment planning (Multiplan®, Accuray Incorporated, Sunnyvale, California, USA). Target delineation and plan approval was performed collaboratively by an ophthalmologist and a physician certified for full-body radiosurgery. In addition, the final plan was independently reviewed by another certified radiosurgeon prior to treatment delivery. An example of a treatment plan is depicted in Fig. 1.
Radiation was delivered in a single fraction with a CyberKnife system (Accuray Inc., Sunnyvale, CA, USA) in a net radiation time of ~25 min. (Table 1). Radiation dose was 21 Gy in all four treated patients. Ophthalmologic follow-up examinations were performed on an individual basis.
Results
A total of eight patients was treated with robotic radiosurgery for choroidal metastasis and four patients fulfilled all inclusion criteria. The median age was 57 years (range: 39–73 years). Three patients were female and one patient was male. The follow-up time was up to 39 months [mean: 31.5 months; range 27–39 months]. One patient had bilateral CM, the other patients had a unilateral lesion (Table 2). Three out of four patients had a visual acuity that was already reduced to hand movement or worse at baseline and none of these patients regained visual acuity. One patient started on a visual acuity (VA) of 0.2 LogMAR (20/30) and improved to 0.0 LogMar (20/20) over the course of the follow-up. All patients had a reduction in tumour size following treatment and showed signs of fibrosis as internal reflectivity increased (Table 3). Central retinal thickness (CRT) decreased in two patients, one patient was not evaluable as OCT scans of the fovea were not possible to obtain due to size of metastasis. One patient had an increase in CRT and received multiple anti-VEGF injections subsequently, no sufficient regression of fluid was observed however. Treatment parameters for all patients can be found in Table 1. Figure 2 depicts the ultrasonographic course of all four patients before treatment and at last follow-up.
A A 73 years old woman with a 5.9 mm tumour was treated with CyberKnife radiosurgery in April 2016. At last follow-up the tumour decreased to 3.5 mm (B). C A 59-year old patient with a 5.2 mm prominent lesion in the left eye was treated in July 2017 with CyberKnife radiosurgery. The lesion decreased to 1.7 mm at last follow-up (D). E A 39-year old woman with an 8,1 mm metastasis was treated in January 2017 with CyberKnife. In June 2018 the lesion was 6.5 mm. Due to progressive serous retinal detachment, she had pars-plana-vitrectomy with silicon oil instillation. G A 57-years old woman showed a peripapillary tumour of 2.5 mm height and had CyberKnife treatment. The metastasis decreased to 1.1 mm at last follow-up (H).
Case 1
A 73-year-old woman was referred to our hospital in January 2016 due to blurred vision for 3 days, which was eventually attributed to an acute vitreous haemorrhage in the left eye. Visual acuity was hand movement at first presentation. She had cataract surgery a few years ago but no other significant history of eye related diseases. The ultrasound examination revealed a prominent lesion (5.9 mm height, reflectivity 65%) of the choroid with surrounding serous retinal detachment. Her past medical history included lung and breast cancer, which was treated with chemotherapy and radiotherapy 12 years ago. Table 4. The vitreous haemorrhage resolved spontaneously. Due to her past medical history, the clinical appearance of the lesion as well as the ultrasonographic findings, a choroidal metastasis was diagnosed, which we treated using CyberKnife radiosurgery in April 2016. The patient was additionally treated with capecitabine by her oncologist. We did follow-up examinations after 3 months and every 6 months thereafter. We observed a subsequent reduction in tumour height, although no increase in visual acuity was recorded. Visual acuity at last follow-up visit remained at hand movement and the last ultrasound examination showed a decrease of the tumour prominence to 3.5 mm with an internal reflectivity of 65%.
Case 2
A 59-year old patient was referred to the clinic in November 2016 due to choroidal mass with blurred vision and distortion of the left eye for 1 week. The initial visual acuity was 0.4 [logMAR]. The ultrasound examination revealed a 5.2 mm prominent tumour with 66% reflectivity with serous retinal detachment. The clinical examination revealed multiple prominent lesions in the right eye as well, the visual acuity was 0.00 [logMAR]. However, onocologic staging showed metastasis of lung, liver and choroid with an atypic lung carcinoid as the primary tumour. After consultation with the local tumour board for the treatment of the eyes, the patient received systemic bevacizumab and a series of three anti-VEGF intravitreal injections in the left eye, which led to a reduction of the metastasis’ height [11]. The patient was also treated with systemic chemotherapy using the intravenous FOLFIRI regime.
As the metastasis progressed again after initial reduction following anti-VEGF treatment on his left eye, the patient was treated with CyberKnife radiosurgery in July 2017 following a consensus decision in the interdisciplinary tumour board. Visual acuity decreased to no light perception due to total serous retinal detachment and remained at this level over the follow-up period. The other eye showed a visual acuity of 0.1 [logMAR] but received a total of 31 intravitreal anti-VEGF injections over the course of follow-up
Case 3
A 39-year old woman came to our hospital in December 2017 as she has noticed a slow decrease of visual acuity over the last 4 weeks in her left eye. At presentation, the initial visual acuity was hand movement. Upon clinical examination a choroidal mass was seen and due to her past medical history, including lung cancer, a choroidal metastasis was suspected. The ultrasound examination revealed a 8.1 mm prominent tumour with a reflectivity of 58% and a serous retinal detachment. The patient was treated with CyberKnife radiosurgery in January 2017 and had surgery for a partial lung resection immediately thereafter. She had an ongoing chemotherapy with cisplatin and vinorelbine. Although no increase in visual acuity was recorded, the tumour height decreased to 6.5 mm. In July 2018 the patient had an increased eye pressure, which was managed with topical eye drops and oral acetazolamide treatment. Due to progressive serous retinal detachment, the patient had pars-plana-vitrectomy with exodrainage and silicon oil instillation. She developed radiation retinopathy with subsequent neovascular glaucoma and therefore received a total of three intravitreal bevacizumab injections. As the eye pressure increased again, the silicon oil was subsequently removed. The eye pressure was within normal limits with two different anti-glaucomatous eye drops until the last follow-up. The visual acuity was no light perception.
Case 4
A 57-year old female patient was referred to our hospital due to visual disturbances that she noticed for several weeks. A choroidal mass in her left eye was appreciated by her ophthalmologist. Her past medical history included lung carcinoma. The ultrasound examination results showed a peripapillary tumour of 2.5 mm height with an internal reflectivity of 52%. Due to the clinical results and the known history of lung carcinoma, the diagnosis of a choroidal metastasis was established. Her visual acuity at this time was 0.2 (LogMAR). After careful consideration and discussion with the patient, we decided to treat her single metastasis in the choroid with CyberKnife radiosurgery. Following staging by her oncologist, no other locations of metastases were found and she was treated with gemcitabine by her oncologist. The metastatasis showed subsequent size reduction and fibrosis with a decrease to 1.1 mm in height and a reflectivity of 90%. Due to a macular oedema, the patient received a total of six intravitreal injections. Her visual acuity increased to 0.0 (LogMAR) and remained stable over the course of follow-up for 31 months (Fig. 3).
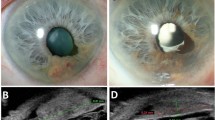
A 57-year old female patient was referred to our hospital due to a peripapillary choroidal metastasis of 2.5 mm and an internal reflectivity of 52% in her left eye. Her visual acuity at this time was 20/25. She was treated with CyberKnife and the tumour reduced from 2.5 mm (A, C) to 1.1 mm (B, D). Her central retinal thickness decreased slightly (pre treatment (E); post treatment (F)). Her visual acuity increased to 20/20 and remained stable over the course of followup of 31 months.
Discussion
Detection of uveal metastasis is associated with a 1-year survival of ~65% and <35% after 5 years [12]. Treatment should therefore aim at improving or preserving vision at a low treatment burden [12].
External beam radiotherapy is most commonly applied in this situation but is usually carried out with multiple radiation fractions over several weeks with a minimum radiation dose of 30 Gy [13,14,15]. We report a total of four patients with a mean follow-up time of 31 months that had been treated using CyberKnife for their uveal metastasis. In all of these patients a reduction in tumour height (mean reduction of 41%) and volume was observed with signs of increasing fibrosis suggested by the increased internal reflectivity (mean increase of 32%) as measured with standardised echography.
Case 2 for example had multiple CM and several treatment options were discussed in the interdisciplinary tumour board, including external beam radiation therapy. Since the detection of CM preceded his underlying atypical lung carcinoid and metastases in other locations, we decided to proceed with a treatment approach as less time consuming as possible as he was still under treatment, including surgery, radiation therapy and chemotherapy for his lung carcinoid. A first approach with systemic and intraviteal anti-VEGF therapy stabilised the choroidal metastasis first, but growth was detected over the course of follow-up so that one session CyberKnife treatment was discussed and eventually executed in one eye. Alternatively, a multiple session fractionated external beam radiation therapy could have been considered in which a dose of 30 Gy in 10 fractions would have been delivered. However, due to multiple treatment sessions regarding his other cancers, an outpatient, single session treatment approach was preferred. Roy et al. [16] described 8 patients who received 30 Gy in 10 fractions and 2 patients with a total of 20 Gy in 5 fractions using radiotherapy and reported complete resolution in 7 patients and partial resolution in 2 patients [16]. Bellmann et al. [17] used SRS in either a single session with dosages between 12 and 20 Gy or in 10 fractions with a total of 30 Gy. They observed a regression of the metastases in 5 out of 6 cases when a single fraction with higher dose was used but in none of the three patients who received 30 Gy in 10 fractions. We therefore believe that a single fraction with a higher radiation dose in this particular case was the most considerate treatment option, also taking into account that he had multiple appointments for his other malignancies. Tsina et al. [14] reported on 63 patients that were treated with PBT with two fractions of 14 cobalt grey equivalents. Complete tumour regression was observed in 84% of patients within 5 months. Rosset et al. described 58 patients treated with multiple fractions using PBT and report complete resolution in 72% of patients when a dosage of 35.5 Gy was administered and in 33% when a dose lower than that was used [1].
Visual acuity increased in 18% of patients of these patients treated with PBT [1] while others report that 62% of their patients remained stable or improved regarding visual acuity. Visual acuity however was measured 3 months after treatment [14]. In our collective, visual acuity remained unchanged in one patient, two patients lost vision, yet both started on hand movement and light perception, and one patient increased in visual acuity. The last patient had good visual acuity upon first presentation, improved slightly and remained on this level for the whole follow-up period. These results are comparable to Ares et al., who report on Gamma Knife treated patients. They showed that in their series of three patients, one remained stable, one worsened and one improved [18]. The mean follow-up time with ~8 months was rather short however.
Patients with metastatic tumours have numerous treatment and follow-up visits due to their primary disease and it seems reasonable to reduce follow-up visits to a minimum, which can be facilitated by reducing the number of fractions needed and avoid hospitalisation which is often necessary in PBT.
Cho et al. [19] reported regression in tumour size in all seven patients following GammaKnife with recurrence in two patients at the end of follow-up (median: 8 months) although no measurements were provided. Subjective worsening of visual acuity was the most common complaint in 85.7% of patients. Other studies showed good results in terms of tumour regression but due to the limited number of patients and short follow-up time, no reliable statement regarding visual acuity outcome could be made [20, 21]. Demirci et al. reported a visual acuity increase or stabilisation in 57% of cases following external beam radiation therapy [12] and other studies are in a similar range with 50% to ~80% [13, 22]. Most of these studies which investigated visual outcome and side effects in EBRT had a follow-up time between 3 and 11 months after treatment and limited information was given on side effects.
While both Gamma Knife and CyberKnife are SRS options, they are different in many aspects. CyberKnife does not demand a fixed metal frame that needs not be mounted to the patient’s head. A firm plastic mask is put on the patient’s face as opposed to the frame screwed to the patient’s head, and a series of X-ray images of the skull is taken during treatment, updated in real-time and delivered to the robotic arm to maximise treatment accuracy and allowing for improved treatment comfort of the patient.
Mathis et al. reported a good outcome in a single case 3 months after CyberKnife radiosurgery but no other reports on CyberKnife in the treatment of CM exist [23].
Radiation induced side effects are often limiting the overall treatment success. Adverse radiation effects include but are not limited to radiation retinopathy or opticopathy, neovascular glaucoma, retinal detachment or cataract development. We did observe one case of neovascular glaucoma following radiation retinopathy in a particularly large choroidal metastasis (case 3). None of the other patients showed signs of radiation related complications during the follow-up of up to 39 months [range 27–39 months]. It is difficult to compare these results with Gamma Knife or any of the other treatment approaches as all of the published reports have rather short follow-up times. Overall, the results are difficult to compare among the different studies due to the heterogeneous group of patients. Many patients seem to show complete or partial regression following treatment and some patients remain stable or even improve in terms of visual acuity.
This report has some limitations and these include the small number of cases and the low visual acuity of treated patients at baseline making it difficult to estimate visual acuity outcome in patients with better initial visual acuity. The average tumour height in our collective was also rather large with 5.4 mm. Reports on visual acuity with similar results had metastases with heights of ~2.5–3.9 mm [17, 22] and the best outcome in our group was seen in the patient with the smallest metastasis initially. Due to the small number of patients however, a general statement cannot be made.
We believe that our results are encouraging to further elucidate a possible role of CyberKnife in the management of selected cases of uveal metastasis. With an interdisciplinary team of ophthalmologists, radiation oncologists and medical physicists, treatment can be delivered in a single session within a 3 h workflow in this particularly sick group of patients.
Summary
What was known before
-
Choroidal metastasis are the most frequent intraocular malignancies occurring in around 10% of all patients with metastasizing primary cancers - some choroidal metastasis would benefit from local therapy but no gold standard exist - treatment approaches are based on radiation procedures but often require hospitalisation and/or surgery that might interfere with treatment needs for the primary condition.
What this study adds
-
Report on robotic assisted radiation therapy in choroidal metastasis - comparable results to other treatment options but only one single session needed in an outpatient setting.
References
Rosset A, Zografos L, Coucke P, Monney M, Mirimanoff RO. Radiotherapy of choroidal metastases. Radiother Oncol: J Eur Soc Therapeutic Radiol Oncol. 1998;46(Mar):263–8.
Bloch RS, Gartner S. The incidence of ocular metastatic carcinoma. Arch Ophthalmol (Chic, Ill: 1960). 1971;85(Jun):673–5.
Wiegel T, Kreusel KM, Bornfeld N, Bottke D, Stange M, Foerster MH, et al. Frequency of asymptomatic choroidal metastasis in patients with disseminated breast cancer: results of a prospective screening programme. Br J Ophthalmol. 1998;82(Oct):1159–61.
Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104(Aug):1265–76.
Konstantinidis L, Rospond-Kubiak I, Zeolite I, Heimann H, Groenewald C, Coupland SE, et al. Management of patients with uveal metastases at the Liverpool Ocular Oncology Centre. Br J Ophthalmol. 2014;98(Jan):92–8.
Mathis T, Jardel P, Loria O, Delaunay B, Nguyen AM, Lanza F, et al. New concepts in the diagnosis and management of choroidal metastases. Prog Retinal Eye Res. 2019;68(Jan):144–76.
Eibl-Lindner K, Furweger C, Nentwich M, Foerster P, Wowra B, Schaller U, et al. Robotic radiosurgery for the treatment of medium and large uveal melanoma. Melanoma Res. 2016;26(Feb):51–7.
Zorlu F, Selek U, Kiratli H. Initial results of fractionated CyberKnife radiosurgery for uveal melanoma. J Neuro-Oncol. 2009;94(Aug):111–7.
Liegl R, Schmelter V, Fuerweger C, Foerster MH, Muacevic A, Priglinger SG, et al. Robotic CyberKnife Radiosurgery for Ciliary Body Melanoma. Ophthalmol Retina. 2020;4:954–6. https://doi.org/10.1016/j.oret.2020.03.031.
Muacevic A, Nentwich M, Wowra B, Staerk S, Kampik A, Schaller U. Development of a streamlined, non-invasive robotic radiosurgery method for treatment of uveal melanoma. Technol Cancer Res Treat. 2008;7(Oct):369–74.
Lai CL, Fan KS, Lee YH, Chen HC, Fan WH. Intravitreal administration of bevacizumab in the treatment of choroidal metastasis in a patient with erlotinib-failed pulmonary adenocarcinoma. Lung Cancer (Amst, Neth). 2012;76(Jun):496–8.
Demirci H, Shields CL, Chao AN, Shields JA. Uveal metastasis from breast cancer in 264 patients. Am J Ophthalmol. 2003;136(Aug):264–71.
d’Abbadie I, Arriagada R, Spielmann M, Le MG. Choroid metastases: clinical features and treatments in 123 patients. Cancer. 2003;98(Sep):1232–8.
Tsina EK, Lane AM, Zacks DN, Munzenrider JE, Collier JM, Gragoudas ES. Treatment of metastatic tumors of the choroid with proton beam irradiation. Ophthalmology. 2005;112(Feb):337–43.
Amer R, Pe’er J, Chowers I, Anteby I. Treatment options in the management of choroidal metastases. Ophthalmologica J Int d’ophtalmologie Int J Ophthalmol Z fur Augenheilkd. 2004;218(Nov-Dec):372–7.
Roy S, Madan R, Gogia A, Tripathy K, Sharma D, Julka PK, et al. Short course palliative radiotherapy in the management of choroidal metastasis: an effective technique since ages. J Egypt Natl Cancer Inst. 2016;28(Mar):49–53.
Bellmann C, Fuss M, Holz FG, Debus J, Rohrschneider K, Völcker HE, et al. Stereotactic radiation therapy for malignant choroidal tumors: preliminary, short-term results. Ophthalmology. 2000;107(Feb):358–65.
Ares WJ, Tonetti D, Yu JY, Monaco EA, Flickinger JC, Lunsford LD. Gamma Knife Radiosurgery for Uveal Metastases: report of Three Cases and a Review of the Literature. Am J Ophthalmol. 2017;174(Feb):169–74.
Cho KR, Lee KM, Han G, Kang SW, Lee JI. Gamma Knife Radiosurgery for Cancer Metastasized to the Ocular Choroid. J Korean Neurosurgical Soc. 2018;61(Jan):60–5.
Lally DR, Duker JS, Mignano JE, Martin S, Witkin AJ. Regression of choroidal metastasis from breast carcinoma treated with gamma knife radiosurgery. JAMA Ophthalmol. 2014;132(Oct):1248–9.
Marchini G, Babighian S, Tomazzoli L, Gerosa MA, Nicolato A, Bricolo A, et al. Gamma Knife stereotactic radiosurgery of ocular metastases: a case report. Stereotact Funct Neurosurg. 1995;64(Suppl 1):67–71.
Rudoler SB, Shields CL, Corn BW, De Potter P, Hyslop T, Curran WJ Jr., et al. Functional vision is improved in the majority of patients treated with external-beam radiotherapy for choroid metastases: a multivariate analysis of 188 patients. J Clin Oncol: Off J Am Soc Clin Oncol. 1997;15(Mar):1244–51.
Mathis T, Caujolle JP, Thariat J. Choroidal Metastasis From Melanoma Treated by Cyberknife Irradiation. JAMA Ophthalmol. 2020;138(Jan):e190388.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schmelter, V., Heidorn, S., Fuerweger, C. et al. Robotic assisted CyberKnife radiosurgery for the treatment of choroidal metastasis. Eye 35, 3376–3383 (2021). https://doi.org/10.1038/s41433-020-01299-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01299-8