Abstract
Objective
To introduce the Collaborative Ocular Tuberculosis Study (COTS) Calculator, an online clinical scoring system for initiating antitubercular therapy (ATT) in patients with ocular tuberculosis (TB).
Method
The COTS Calculator was derived from COTS Consensus (COTS CON) data, which has previously published consensus guidelines. Using a two-step Delphi method, 81 experts evaluated 486 clinical scenario-based questions, ranking their likelihood of initiating ATT in each specific scenario. Each scenario was a permutation of the results and/or availability of five following components—clinical phenotype, endemicity, two immunological (tuberculin skin test, interferon-γ release assay) and one radiological (chest X-Ray) test results—and a sixth component further stratifying three of the clinical phenotypes. The median scores and interquartile ranges (IQR) of each scenario were tabulated, representing the expert consensus on whether to initiate ATT in that scenario. The consensus table was encoded to develop the COTS Calculator.
Results
The COTS Calculator can be accessed online at: https://www.oculartb.net/cots-calc. The attending physician can select the conditions present in the patient, which will generate a median score from 1 to 5. 114 out of 486 scenarios (24%) deliberated had a median score of 5 indicating expert consensus to initiate ATT.
Conclusion
The COTS Calculator is an efficient, low-cost, evidence and experience-based clinical tool to guide ATT initiation. While it holds substantial promise in improving standard-of-care for ocular-TB patients, future validation studies can help to as certain its clinical utility and reliability.
Similar content being viewed by others
Introduction
According to the World Health Organisation (WHO) 2021 report, tuberculosis (TB) caused 1.5 million deaths worldwide in 2020 [1]. In patients with culture-proven TB, an estimated 6.8% reported ocular involvement [2], often complicated by significant ocular morbidity and visual loss [3, 4]. Ocular TB may be the first presentation of TB in initially asymptomatic patients [5], especially since 92% of patients with Ocular TB present without evidence of concomitant pulmonary TB [6]. There is substantial existing uncertainty in diagnosing Ocular TB [7]. If ATT is delayed, there is a risk of irreversible ocular complications, delayed treatment of underlying systemic TB, and increased public health risks of TB resurgence.
Timely initiation of antitubercular therapy (ATT) is the major challenge in treating ocular TB due to a lack of robust diagnostic criteria [8] and inconclusive evidence on which to base the management guidelines for initiating ATT [9,10,11,12,13]. As ocular presentations of TB are wide-ranging [8] due to its ability to cause inflammation in any tissue of the eye [14,15,16,17,–18], typical diagnosis requires clinical manifestations of TB uveitis, choroiditis or retinitis, accompanied by the exclusion of other uveitic entities, as well as corroborative immunological or radiological investigations for TB or genomic evidence of TB [19]. Immunological tests for the TB diagnosis include Tuberculin skin test (TST, also known as Mantoux test or purified protein derivative [PPD] test), and Interferon Gamma Release Assays (IGRA), which includes the QuantiFERON-TB Gold or In-Tube or T-SPOT.TB [20].
TST is an affordable and widely available test for skin hypersensitivity towards mycobacterial antigens via cell-mediated immune response [20]. However, TST has only a sensitivity of 89% and specificity of 85% [21], indicating a fair risk of false positives with Bacille Calmette Guérin (BCG) vaccination and exposure to atypical mycobacteria [22]. Although specificity can be improved by increasing the skin induration cut-off diameter to 10 mm in endemic nations based on CDC guidelines, this results in decreased sensitivity [23]. IGRA tests for interferon-γ release from lymphocytes after stimulation with M. tuberculosis specific antigens [24]. IGRA is a more specific test for M. tuberculosis infection as it is not affected by BCG vaccination or atypical mycobacteria exposure, but IGRA is more expensive and less widely available compared to TST [20]. Both TST and IGRA do not distinguish latent infection from active disease and may be falsely negative in immunodeficient individuals [25, 26]. Plain chest X-ray is an affordable and widely available tool to look for pulmonary evidence of TB infection, although radiologically-detected lesions are not specific for TB and most cases of ocular TB do not show any evidence of concomitant active pulmonary TB [27]. Although computer-assisted tomography (CT) can better visualise lymphadenopathy and tuberculoma, it is not routinely ordered due to higher cost and radiation exposure, as well as unavailability in resource-scarce regions [28]. Polymerase chain reaction (PCR) has emerged as a highly sensitive tool for rapidly detecting presence of M. tuberculosis genome in ocular fluid samples, even in latently infected individuals, by nucleic acid amplification [29]. However, PCR testing for M. tuberculosis is also limited to high resource settings [27]. Overall, cautious interpretations of diagnostic investigations [20,21,22,23,24,25,26,27,28,–29], guided by knowledge of the sensitivity and specificity of the test is required for accurate diagnosis of Ocular TB and prompt initiation of ATT [30].
The Collaborative Ocular Tuberculosis Study (COTS) Group, supported by the International Uveitis Study Group (IUSG), International Ocular Inflammation Society (IOIS) and Foster Ocular Immunology Society (FOIS), was established to address the existing ambiguity faced by ophthalmologists globally about the minimum set of criteria to initiate ATT in presumed ocular-TB infections [19, 31,32,33]. The COTS Group began with the COTS-1 study, performed using retrospective data of patients diagnosed with Ocular TB collected from 25 participating ophthalmic centres globally [19, 31,32,33]. COTS-1 results demonstrated a lack of consensus in the use of diagnostic tests, with majority of experts ordering chest radiography and immunological tests, including TST and IGRA where available, while a small minority of experts relied on PCR from intraocular fluids [32, 33]. Therefore, an expert-led international consensus initiative (COTS CONSENSUS or COTS CON) was developed to consolidate the expertise of 81 uveitis specialists and establish consensus recommendations regarding the initiation of ATT in patients with presumed ocular TB across the wide spectrum of possible clinical scenarios. Consensus was achieved through deliberation amongst experts based on practical experience, supplemented by the limited evidence available from existing literature and data reported in COTS-1 publications [34].
The purpose of this concept paper is to introduce an online clinical scoring system, the COTS Calculator, crafted to guide the initiation of ATT in patients with suspected ocular TB. The COTS Calculator aims to guide physicians globally, including experts and general ophthalmologists, on the initiation of ATT based on minimum diagnostic criteria for Ocular-TB infection and international uveitis specialists’ inputs for initiation of ATT based on those criteria. This paper will evaluate how the COTS calculator differs from traditional clinical scoring systems that are summative by calculation and propose further diagnostic validation studies to test for specificity, sensitivity, positive and negative predictive values of the COTS calculator as a practical tool and unified platform in management of Ocular TB.
Method
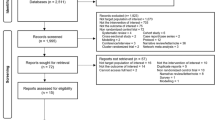
The detailed methodology for obtaining consensus amongst global ocular inflammation and TB experts for COTS CON has been described previously [34]. Briefly, a modified Delphi technique, involving a multistage self-completed questionnaire administered to geographically scattered experts [35, 36], was used to collect responses for 486 clinical scenario-based questions from 81 uveitis experts globally in the COTS CON Delphi Round 1 questionnaire via an online web-based encrypted link [34]. Delphi Round 2, which deliberated scenarios where clear-cut consensus did not exist at the questionnaire phase, was divided into two in-person phases. Phase I deliberated 71 clinical scenario-based questions for initiating ATT and adjunctive therapy with oral corticosteroids or immunosuppressive agents or intravitreal therapy in tubercular choroiditis (TBC) phenotypes on 16 November 2018 in Chandigarh, India [37]. Phase II deliberated 40 clinical scenario-based questions for initiating ATT and adjunctive therapy in tubercular anterior uveitis (TAU), tubercular intermediate uveitis (TIU), tubercular panuveitis (TPU), and tubercular retinal vasculitis (TRV) on 13 November 2019 in Kaohsiung, Taiwan [38]. A total of 54 experts attended the Delphi Round 2 meeting, plus 4 experts joined the meeting online. The 23 experts not present were given the meeting details and an online questionnaire to complete at the time of their convenience (Fig. 1). The final data analysis was performed after completion of all the online responses [34].
Based on the probability that each expert would initiate ATT under a given clinical scenario, every opinion was awarded a score of 1–5 on the five-level Likert’s scale [39, 40]. The statistical analysis calculated median scores and interquartile ranges (IQR). IQRs were stratified into levels of agreement. Clinical scenario-based statements with a median score of 4 indicated a higher level of confidence that ATT should be initiated and were set aside for critical deliberation and discussion amongst the experts for further consensus-generation and literature review during COTS CON Delphi Round 2 meetings [34] (Fig. 2).
Following the diagnostic criteria of tubercular uveitis as defined by the Standardisation of Uveitis Nomenclature (SUN) working group, the following ocular uveitic presentations that can be attributed to ocular TB were evaluated [41]. TIU is defined as the vitreous being the major site of inflammation [42]. TPU is defined as the lack of a predominant site of inflammation with inflammation observed in the anterior chamber, vitreous, and retina and/or choroid [42]. TAU is defined as inflammation limited to the anterior segment, where the primary site of inflammation is the anterior chamber involving the iris and ciliary body [42]. Active TRV involves evidence of ocular inflammation and retinal vascular changes, including perivascular sheathing and vascular leakage or occlusion on fluorescein angiogram [42]. Inactive TRV was defined as retinal vascular changes without evidence of ocular inflammation [42]. Tubercular serpiginous-like choroiditis (TB SLC) is defined as inflammation limited to the choroid, the primary site of inflammation, and is characterised by single or multiple discrete yellow-white fuzzy choroidal lesions with slightly raised edges that show wave-like progression with an active serpiginous-like edge with central healing [42]. Tuberculoma, or choroidal granuloma or choroidal nodule, is defined as inflammation limited to the choroid, the primary site of inflammation, and is characterised by single or multiple yellowish subretinal lesions with indistinct borders and surrounding exudative fluid, along with oval or round lesions in the choroidal stroma [42]. Tubercular non-serpiginous choroiditis (TB NSC) is defined as inflammation limited to the choroid, the primary site of inflammation, and is characterised by unifocal or multifocal choroiditis lesions with a phenotype similar to idiopathic multifocal choroiditis, acute posterior multifocal placoid pigment epitheliopathy (APMPPE) and other phenotypes that do not resemble TB SLC [42].
The key diagnostic criteria of ocular TB from the SUN working group include a compatible uveitic syndrome attributable to TB on clinical presentation and evidence of active systemic TB through a positive CXR, IGRA or TST finding [41]. Hence, each scenario-based question consisted of five components: clinical phenotype, endemicity of the patient’s location, and TST/PPD, IGRA and/or CXR results (or lack-of such testing). An additional sixth component was applied to three of the clinical phenotypes for further stratification. Each scenario-based question was given a reference number. Based on the different permutations and combinations of immunological and radiological test results for TB in each clinical phenotype further binarized based on the TB endemicity of the patient’s country of origin, the total number of possible clinical scenarios was 486.
Results
The median score and IQR for all 486 clinical scenario-based questions from Delphi Round 1 and 2 were tabulated (Supplementary 1, online only). Each of the 486 clinical scenario-based questions was assigned a reference number according to the inputs of the five components, any additional sixth component, median score, and IQR. These data were encoded to produce an algorithm (Supplementary 2, online only) for a novel free online web-based COTS calculator.
The COTS Calculator can be accessed at: https://www.oculartb.net/cots-calc.
The attending physician can input the patient details (Fig. 3), the clinical conditions found in this patient (Fig. 4) and print all these inputs along with the median score and IQR generated by the COTS calculator for the patient (Fig. 4). The printout can thus be incorporated as part of the patient’s clinical records. The COTS calculator will not store any of the patient details keyed in.
The endemicity of the patient selected is “endemic” out of two options (endemic, nonendemic). the tuberculin skin test/mantoux test, interferon gamma release assay (IGRA), and chest X-ray each has three options (positive, negative, not done/unknown) and “positive” was selected for all three. The combinations of these six selections corresponded to the result: Median Score “5” and Interquartile Range (IQR) “0”. TB tuberculosis, QFT-Gold Quantiferon-TB Gold, COTS collaborative ocular tuberculosis study. Two tables interpreting median score of 1–5 and Interquartile range (IQR) of 0–3 are presented. Median score 5 and IQR 0 and their interpretations are highlighted in yellow as corresponding to the patient’s conditions “Median score 5” is interpreted to be a very high probability for most experts to consider initiating Antitubercular therapy (81–100%). IQR 0 is interpreted to be representing absolute consensus, with more than 90% of experts agreeing on the initiation of antitubercular therapy.
The ophthalmologist can select from the 5 drop-down bars the applicable category for a patient in terms of clinical phenotype, endemicity, TST, IGRA, CXR results (Fig. 4). The five clinical phenotypes include TBC, TAU, TIU, TPU and TRV. There is an additional drop-down bar for further stratification of TAU, TRV and TBC phenotypes (Fig. 4). TAU was further stratified into first or recurrent episodes. TRV was stratified into active or inactive disease. TBC was stratified into TB SLC, tuberculoma, and multifocal or unifocal TB NSC.
The combination of conditions will correspond to a specific reference number that is encoded to such a patient (Supplementary 2, online only), and this will generate a median score on the scale of 1–5, calculated based on the responses and deliberation of experts through COTS CON Delphi Round 1 and 2. Median score of 1 represents a very low probability for most experts to initiate ATT (<20%); 2: low probability for most experts to initiate ATT (21–40%); 3: mixed probability for most experts to initiate ATT (41–60%); 4: high probability for most experts to initiate ATT (61–80%); and 5: very high probability for most experts to initiate ATT (81–100%) (Fig. 4).
The IQR corresponding to the same set of conditions in the given patient is also displayed, with an IQR of 0 representing more than 90% of experts agreeing on the initiation of ATT which is considered absolute consensus; an IQR of 1 represents more than 80% of experts’ agreement which is moderate consensus; IQR of 2 represents more than 70% experts’ agreement which is weak consensus; IQR of 3 represents less than or exactly 60% of experts agreeing on the initiation of ATT which is considered poor consensus (Fig. 4).
A result of 5 with IQR of 0, 1, 2, 3 is considered to have reached consensus to initiate ATT in that particular clinical scenario (Fig. 2) and should guide the ophthalmologist to consider initiating ATT based on the COTS group consensus guidelines [37, 38]. A result of 4 indicates a high level of confidence that ATT should be initiated, with an IQR of less than or equal to 1 being a good indicator of consensus among experts (Fig. 2). A result of 1, 2, 3 indicate a lower level of confidence for initiating ATT, with no consensus and mixed opinions amongst experts, but do not constitute consensus that “ATT need not be initiated” [34].
Amongst the 486 possible clinical scenarios, the distribution of median scores 1, 2, 3, 4, 5 are 98 (20%), 89 (18%), 120 (25%), 65 (13%) and 114 (24%) respectively (Table 1, Supplementary Fig. 1). 24% of all scenarios have a median score of 5 indicating a very high probability (81–100%) of initiating ATT in these scenarios (Supplementary Fig. 1). Amongst these 114 scenarios with a median score of 5, 72 scenarios have IQR 1 indicating moderate consensus (80–90% agreement), 24 scenarios have IQR 0 indicating strong consensus (>90% agreement), 13 scenarios with IQR 2 and 5 scenarios with IQR 3 are considered weak and poor consensus (70–80% and <70% agreement) respectively (Supplementary Fig. 1).
Discussion
This concept paper introduces the COTS Calculator, a simplified clinical aid to guide ATT initiation based on evidence, statistics, and expert consensus. Ocular TB is a rare entity that overlaps between respiratory medicine, infectious diseases, and ophthalmology, requiring a high level of subspecialist experience to manage. For the general ophthalmologist that lacks experience in ocular TB, this calculator consolidates global consensus in a practical and accessible manner, allowing them to balance the risks and benefits of initiating ATT.
The principle of assigning clinical scores based on a panel of clinical findings is not new [43]. For a clinical scoring system to be useful, it should include common physical examination or imaging findings, commonly ordered laboratory investigations, be easy to interpret unambiguously, backed by accurate data and statistics, and easily accessible to attending physicians [44].
One difference between the COTS Calculator and most traditional clinical scoring systems is its derivation from the two-step Delphi consensus method, where experts decided on initiating ATT under 486 different clinical scenarios. Most other scoring systems consist of a fixed number of measurable variables—each variable allocated points—and the sum of points produces a total score. Cut-off scores are then established by validation studies which test the thresholds against an existing gold-standard diagnostic method. This was not a plausible method in the case of ocular TB.
Realistically, certain newer or more advanced immunological and radiological investigations (while ideal for ocular-TB diagnosis) may not be available in resource-scarce settings where TB is endemic. The COTS CON group considered the need for the COTS Calculator to retain its utility in resource-scarce TB endemic regions. Hence, the calculator does not mandate a fixed number of measurable variables, but rather incorporates possible scenarios where one, two, or all three ancillary investigations were not available [35]. Hence, the COTS Calculator is able to account for the unavailability of certain investigations in the real-life setting. As diagnostic classifications necessarily need consensus among experts before studies to validate this classification can be carried out [12], global expert consensus was achieved through COTS CON.
The attending physician can refer to Delphi Round 2 Phase I published report [37] for seventy consensus statements addressing the initiation of ATT and 10 consensus statements detailing the use of adjunctive therapy in TBC, as well as the Delphi Round 2 Phase II published report [38] for forty-four consensus statements addressing initiation of ATT in TAU, TIU, TPU, and TRV. These two COTS CON guidelines used a median score of 5 with an IQR of 0 to 3 to define “consensus to initiate ATT”. The COTS Calculator similarly follows this definition of consensus. The median score of 5 represents at least more than half of the global experts choosing to initiate ATT 81–100% of the time when met with that particular clinical scenario [34], hence the majority choice to initiate ATT with an 81–100% probability is defined to be consensus to initiate ATT. A median score of 4 means that at least more than half of the global experts will choose to initiate ATT 61–80% of the time, reflecting lower confidence that the diagnosis of ocular TB is definitive and ATT should thus be initiated. The two-step Delphi process allowed for reconsideration of clinical-based scenario questions with a median score of 4 in Round 1. These questions were brought forth for further expert deliberation in Round 2 and reassessed so that consensus to initiate ATT may be achieved should a median score of 5 be attained in Round 2. As the COTS CON group is gathered to address when to initiate ATT instead of when not to initiate ATT, median scores of 4, 3, 2 and 1 are not part of the COTS CON guidelines and do not imply that ATT should not be initiated in these cases. Within the 114 scenarios with a median score of 5, 72 scenarios have IQR 1 and 24 scenarios have IQR 0 indicating moderate and absolute consensus (80–90% and >90%) respectively. This means that the COTS calculator would offer clear recommendations to initiate ATT most of the time when the median score of 5 is obtained. This potential clinical utility of the COTS calculator is therefore promising.
Ultimately, the COTS Calculator is meant to serve as a statistically-derived and expertise-based treatment recommendation guide. Experienced clinical judgement based on the attending physician’s direct knowledge of the patient’s holistic conditions and local epidemiological risk factors is imperative to making the final decision to initiate ATT or not. It is also up to the attending physician’s clinical judgement to decide whether to initiate ATT when other non-ATT treatments are ineffective, or conversely to stop ATT if the patient’s ocular inflammation is not responding to ATT. Users of the COTS Calculator should also take into consideration differential diagnosis of ocular TB and exclude other causes of uveitis in keeping with the diagnostic criteria of ocular TB as established by the SUN working group [41].
Like all established clinical scoring systems, validation studies of the COTS Calculator are needed to assess its specificity and sensitivity in guiding therapy targeted at Ocular TB. Usually, validation studies test against a current gold-standard diagnostic method. However, in the reality of ocular TB, gold-standard diagnostic methods may be unavailable in resource-scarce settings where TB is endemic. Moreover, the current gold standard for diagnosing ocular TB is the detection of M. tuberculosis in ocular fluids or tissues [31] is extremely difficult due to the small volume of ocular tissue biopsy samples and low ocular tissue load of M. tuberculosis [45, 46]. Even PCR has low sensitivity for detecting TB genome in ocular samples reliably in real-world settings [31]. Therefore, the typical diagnosis of Ocular TB remains principally presumptive, based on epidemiology, ocular phenotype and corroborative immunologic tests, and radiological findings. Thus, the COTS Calculator is developed based on consensus from experienced experts of endemic and nonendemic regions to guide prompt initiation of ATT if ancillary investigations are unavailable or the results of which are unclear. Future prospective studies will be useful to validate the COTS Calculator as a clinical scoring system, via exploring associations between ATT initiation using the COTS Calculator, and longitudinal treatment outcomes or adverse events.
Regarding SLC, absolute consensus to initiate ATT was reached in patients with both immunologic tests (both TST and IGRA) and radiologic tests positive, irrespective of endemicity, and in patients from endemic regions with one positive immunological test result (either TST or IGRA) and a positive radiologic test. However, for nonendemic regions, the consensus reached for these given scenarios was moderate. For the remaining scenarios with only one of the immunological tests (TST or IGRA) showing positive result, the median score indicated a higher likelihood to initiate ATT, but with weak to moderate consensus among experts. From our results on SLC, it appears that experts deem that only one positive immunologic test is considered sufficient to start ATT, perhaps because the clinical picture of SLC is highly suggestive of ocular TB. Similarly, TB is also known to manifest as a focal lesion in the choroid, with choroidal tubercles and tuberculomas representing the most common and best-documented clinical manifestation of ocular TB. The results from our consensus confirmed that most experts deem choroidal tubercles and tuberculomas to be very suggestive of ocular TB, since it was recommended to start ATT with any corroborative immunologic evidence for TB, and also with radiologic findings alone in endemic areas. In fact, absolute consensus was achieved in patients with both immunologic tests (TST and IGRA) and radiologic test positive. If either of the two immunologic tests showed positive results and the radiologic evidence was positive, in an endemic region, absolute consensus to initiate ATT existed, however, the perception differed in a nonendemic region with moderate consensus. If either immunologic test was positive and no radiologic evidence supported those findings, the consensus to initiate ATT was moderate in both regions. The observation was similar in endemic regions in the absence of immunologic evidence but with positive radiologic findings. In contrast to SLC and tuberculoma, tubercular focal or multifocal choroiditis phenotypes have a relatively weaker association with TB. Hence, the use of ATT must be supported by immunologic evidence together with radiologic signs suggestive of old healed or active pulmonary TB. In fact, absolute consensus to start ATT was reached in patients with both immunologic tests (TST and IGRA) and radiologic test positive, and moderate consensus was achieved if either of the immunologic tests showed positive results together with positive radiologic test, irrespective of endemicity.
Regarding anterior uveitis, in the case of the first episode, there was moderate consensus to initiate ATT when all three tests were positive. Absolute consensus was achieved in the case of recurrent episodes of anterior uveitis when all three tests were positive. These findings were irrespective of the endemicity. Moderate consensus was achieved for patients coming from an endemic region with recurrent episodes of anterior uveitis and one immunological test positive supported by positive radiological findings, whereas for nonendemic regions, the consensus reached was moderate or weak.
Regarding panuveitis, there was absolute consensus to start ATT when two immunological tests (PPD and IGRA) and radiological test were positive. Moderate consensus was achieved in the case of one of the two immunological tests positive (either PPD or IGRA) and radiological test positive. The findings were irrespective of endemicity. Regarding intermediate uveitis, the consensus was lower when compared to panuveitis. In fact, there was moderate consensus to start ATT when two immunological tests (PPD and IGRA) and radiological test were positive; the consensus achieved was also moderate in the case of one of the two immunological tests positive (either PPD or IGRA) and radiological test positive in endemic areas, but either moderate or weak in nonendemic areas. From the data it emerged that in endemic area, where the pre-test probability of tubercular uveitis is higher, experts are more likely to treat patients, and it is clearly evident that panuveitis have a stronger predictive value for ocular TB compared to intermediate uveitis.
Regarding active retinal vasculitis, when two immunological tests (PPD and IGRA) and radiological tests were positive, the consensus to start ATT was absolute in endemic regions and weak in nonendemic regions. With one of the two immunological tests positive (either PPD or IGRA) and radiological positive findings the consensus reached was absolute to moderate in endemic regions and very weak in nonendemic areas. The results confirmed once again that in endemic areas where the pre-test probability of tubercular uveitis is higher, experts are more likely to treat patients, and that in nonendemic settings, other causes of retinal vasculitis need to be considered and ruled out in the differential diagnosis.
Some limitations of this study to provide treatment recommendations for ocular TB are inherent to the diagnosis of ocular TB which is partially a priori. Diagnosis is only as certain as the clinician’s ability to identify ocular phenotypes attributable to TB, thereby raising clinical need to perform ancillary investigations to search for systemic TB. Clinical impression is subject to possible error, thus initial diagnosis may be wrong and other disease entities causing uveitis may not be fully excluded. In addition, validity of CXR, IGRA, and TST results may vary across regions, but was assumed to be uniform across all labs and of accurate interpretation for the purpose of this study. The clinical applications of this study could be further enhanced in the future with a greater number of global uveitis experts coming together for a more representative and stronger global consensus, and take into more clinical characteristics such as a previous history of TB or ATT, as well as results of other molecular diagnostic tests such as polymerase chain reaction (PCR) detection of TB genome in ocular fluids. This study only assessed the minimum diagnostic criteria which can be further expanded to be more comprehensive. Lastly, the COTS Calculator is not yet reviewed by respiratory physicians, or other infectious disease experts who can help to validate the interpretation of ancillary investigations and epidemiology.
In conclusion, the COTS Calculator is an efficient, cost-effective, and automatically generated clinical score used to guide the initiation of ATT in five clinical subtypes of Ocular TB, developed based on the review of published literature and expert opinion derived from clinical practical experience, to bridge the gap between clinical demand and available medical evidence. The COTS Calculator is further supported by two sets of published consensus guidelines that are also important in informing public policy considering TB resurgence due to globalisation. Future diagnostic validation studies for the COTS Calculator are needed to prove the clinical utility and reliability of the COTS Calculator.
Summary
What was known before
-
Diagnosis of Ocular TB remains principally presumptive, based on epidemiology, ocular phenotype and corroborative immunologic tests and radiological findings.
-
Ocular TB can present in many different clinical phenotypes, due to TB ability to infect any tissue of the eye.
-
There has been no group before COTS CON to achieve global expert consensus on the diagnostic classification of Ocular TB.
What this study adds
-
The COTS Calculator is an online, low-cost, accessible clinical scoring system designed to guide the challenging decision to initiate ATT in cases of presumed ocular TB.
-
It holds promise in improving standard-of-care for ocular-TB patients.
-
The attending physician can also print out the results of the COTS Calculator with respect to the specific patient and keep it as part of the patient’s medical records.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available. Nevertheless, interested researchers are invited to direct data access requests to the corresponding author.
References
World Health Organization. Global Tuberculosis Report. 2021. https://www.who.int/publications/i/item/9789240037021.
Bouza E, Merino P, Muñoz P, Sanchez-Carrillo C, Yáñez J, Cortés C. Ocular tuberculosis. A prospective study in a general hospital. Medicine 1997;76:53–61.
Biswas J, Badrinath SS. Ocular morbidity in patients with active systemic tuberculosis. Int Ophthalmol. 1995;19:293–8.
Basu S, Monira S, Modi RR, Choudhury N, Mohan N, Padhi TR, et al. Degree, duration, and causes of visual impairment in eyes affected with ocular tuberculosis. J Ophthalmic Inflamm Infect. 2014;4:3.
Shah JS, Shetty N, Shah SK, Shah NK. Tubercular uveitis with ocular manifestation as the first presentation of tuberculosis: a case series. J Clin Diagn Res. 2016;10:NR01–3.
Agrawal R, Gunasekeran DV, Raje D, Agarwal A, Nguyen QD, Kon OM, et al. For the Collaborative Ocular Tuberculosis Study Group; Global variations and challenges with tubercular uveitis in the collaborative ocular tuberculosis study. Investig Ophthalmol Vis Sci. 2018;59:4162–71.
Betzler BK, Gupta V, Agrawal R. Clinics of ocular tuberculosis: a review. Clin Exp Ophthalmol. 2021;49:146–60.
Gupta A, Sharma A, Bansal R, Sharma K. Classification of intra-ocular tuberculosis. Ocul Immunol Inflamm. 2015;23:7–13.
Lou SM, Montgomery PA, Larkin KL, Winthrop K, Zierhut M, Rosenbaum JT, et al. Diagnosis and treatment for ocular tuberculosis among uveitis specialists: the international perspective. Ocul Immunol Inflamm. 2015;23:32–9.
Lou SM, Larkin KL, Winthrop K, Rosenbaum JT, Uveitis Specialists Study Group. Lack of consensus in the diagnosis and treatment for ocular tuberculosis among uveitis specialists. Ocul Immunol Inflamm. 2015;23:25–31.
Gupta V, Gupta A, Rao NA. Intraocular tuberculosis—an update. Surv Ophthalmol. 2007;52:561–87.
Agrawal R, Gupta B, Gonzalez-Lopez JJ, Rahman F, Phatak S, Triantafyllopoulou I, et al. The role of anti-tubercular therapy in patients with presumed ocular tuberculosis. Ocul Immunol Inflamm. 2015;23:40–6.
Pefkianaki M, Westcott M, Liew G, Lee R, Pavesio C, et al. Diagnostic and therapeutic challenges. Retina. 2014;34:1247–52.
Agrawal R, Gunasekeran DV, Gonzalez-Lopez JJ, Cardoso J, Gupta B, Addison PKF, et al. Peripheral retinal vasculitis: analysis of 110 consecutive cases and a contemporary reappraisal of tubercular etiology. Retina. 2017;37:112–7.
Gupta V, Shoughy SS, Mahajan S, Khairallah M, Rosenbaum JT, Curi A, et al. Clinics of ocular tuberculosis. Ocul Immunol Inflamm. 2015;23:14–24.
Gupta A, Bansal R, Gupta V, Sharma A, Bambery P. Ocular signs predictive of tubercular uveitis. Am J Ophthalmol. 2010;149:562–70.
Ang M, Vasconcelos-Santos DV, Sharma K, Accorniti M, Sharma A, Gupta A, et al. Diagnosis of ocular tuberculosis. Ocul Immunol Inflamm. 2018;26:208–16.
Knecht PB, Papadia M, Herbort CP. Secondary choriocapillaritis in infectious chorioretinitis. Acta Ophthalmol. 2013;91:e550–5.
Agrawal R, Gunasekeran DV, Grant R, Agarwal A, Kon OM, Nguyen Q, et al. Clinical features and outcomes of patients with tubercular uveitis treated with antitubercular therapy in the Collaborative Ocular Tuberculosis Study (COTS)-1. JAMA Ophthalmol. 2017;135:1318–27.
Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al. A systematic review of rapid diagnostic tests for the detection of tuberculosis infection. Health Technol Assess. 2007;11:1–196.
Centers for Disease Control and Prevention. Updated guidelines for using interferon gamma release assays to detect mycobacterium tuberculosis infection—United States, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:1–25.
Wang L, Turner MO, Elwood RK, Schulzer M, FitzGerald JM. A meta-analysis of the effect of Bacille Calmette Guérin vaccination on tuberculin skin test measurements. Thorax. 2002;57:804–9.
Centers for Disease Control and Prevention. Nationwide shortage of tuberculin skin test antigens: CDC recommendations for patient care and public health practice. MMWR Morb Mortal Wkly Rep. 2019;68:552–3.
Metcalfe JZ, Everett CK, Steingart KR, Cattamanchi A, Huang L, Hopewell PC, et al. Interferon-γ release assays for active pulmonary tuberculosis diagnosis in adults in low- and middle-income countries: systematic review and meta-analysis. J Infect Dis. 2011;204 Suppl 4:S1120–9.
Albini TA, Karakousis PC, Rao NA. Interferon-gamma release assays in the diagnosis of tuberculous uveitis. Am J Ophthalmol. 2008;146:486–8.
Kurup SK, Buggage RR, Clarke GL, Ursea R, Lim WK, Nussenblatt RB, et al. Gamma interferon assay as an alternative to PPD skin testing in selected patients with granulomatous intraocular inflammatory disease. Can J Ophthalmol. 2006;41:737–40.
Vasconcelos-Santos DV, Zierhut M, Rao NA. Strengths and weaknesses of diagnostic tools for tuberculous uveitis. Ocul Immunol Inflamm. 2009;17:351–5.
Jeong YJ, Lee KS. Pulmonary tuberculosis: up-to-date imaging and management. AJR Am J Roentgenol. 2008;191:834–44.
Sugita S, Ogawa M, Shimizu N, Morio T, Ohguro N, Nakai K, et al. Use of a comprehensive polymerase chain reaction system for diagnosis of ocular infectious diseases. Ophthalmology. 2013;120:1761–8.
Rosenbaum JT. To be or not TB? Br J Ophthalmol. 2014;98:999e1000.
Agarwal A, Agrawal R, Gunasekaran DV, Raje D, Gupta B, Agrawal K, et al. The Collaborative Ocular Tuberculosis Study (COTS)-1 Report 3: polymerase chain reaction in the diagnosis and management of tubercular uveitis: global trends. Ocul Immunol Inflamm. 2017;27:465–73.
Gunasekeran DV, Agrawal R, Agarwal A, Carreno E, Raje D, Aggarwal K, et al. The Collaborative Ocular Tuberculosis Study (COTS)-1: a multinational review of 251 patients with tubercular retinal vasculitis. Retina. 2019;39:1623–30.
Agrawal R, Gunasekeran DV, Agarwal A, Carreno E, Aggarwal K, Gupta B, et al. The Collaborative Ocular Tuberculosis Study (COTS)-1: a multinational description of the spectrum of choroidal involvement in 245 patients with tubercular uveitis. Ocul Immunol Inflamm. 2018;29:1–11.
Agrawal R, Testi I, Mahajan S, Yuen YS, Agarwal A, Rousselot A, et al. The Collaborative Ocular Tuberculosis Study (COTS) Consensus (CON) Group Meeting Proceedings. Ocul Immunol Inflamm. 2020. https://doi.org/10.1080/09273948.2020.171602.
Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–80. https://doi.org/10.1136/bmj.311.7001.376.
McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016;38:655–62. https://doi.org/10.1007/s11096-016-0257-x.
Agrawal R, Testi I, Mahajan S, Yuen YS, Agarwal A, Kon OM, et al. Collaborative Ocular Tuberculosis Study consensus guidelines on the management of tubercular uveitis report 1: guidelines for initiating anti- tubercular therapy in tubercular choroiditis. Ophthalmology. 2021;128:266–76.
Agrawal R, Testi I, Bodaghi B, Barisani-Asenbauer T, Mccluskey P, Agarwal A, et al. Collaborative Ocular Tuberculosis Study Consensus Guidelines on the Management of Tubercular Uveitis Report 2: Guidelines for Initiating Antitubercular Therapy in Anterior Uveitis, Intermediate Uveitis, Panuveitis, and Retinal Vasculitis. Ophthalmology. 2021;128:277–87.
Derrick B, White P. Comparing two samples from an individual Likert question. Int J Math Stat. 2017;18:1–13.
Armstrong R. The midpoint on a five-point Likert-type scale. Percept Mot Skills. 1987;64:359–62. https://doi.org/10.2466/pms.1987.64.2.359.
The Standardization of Uveitis Nomenclature (SUN) Working Group. Classification criteria for sarcoidosis-associated uveitis. Am J Ophthalmol. 2021;228:142–51.
Collaborative Ocular Tuberculosis Study (COTS) Group. Standardization of Nomenclature for Ocular Tuberculosis—Results of Collaborative Ocular Tuberculosis Study (COTS) Workshop. Ocul Immunol Inflamm. 2019. https://doi.org/10.1080/09273948.2019.1653933.
Apgar V. A Proposal for a New Method of Evaluation of the Newborn Infant. Originally published in July 1953, volume 32, pages 250–259. Anesth Analg. 2015;120:1056–9.
Ibrahim LF, Hopper SM, Donath S, Salvin B, Babl FE, Bryant PA. Development and validation of a cellulitis risk score: the Melbourne ASSET score. Pediatrics. 2019;143:e20181420.
Ang M, Chee SP. Controversies in ocular tuberculosis. Br J Ophthalmol. 2017;101:6e9.
Gupta V, Gupta A, Rao NA. Intraocular tuberculosis—an update. Surv Ophthalmol. 2007;52:561e587.
Acknowledgements
All authors contributed to the intellectual development of this paper. RA and VG conceived and planned the study. ZL wrote the first draft of the paper. ZL and RA performed the literature review. RA, ZL, BB, IT, SM, AR, JHK, JRS, PM, QDN, CP and VG contributed to interpreting the results and provided critical feedback to the paper. The final version of the paper has been seen and approved by all authors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
RA, ZL, BB, IT, SM, AR, JHK, JRS, PM, QDN, CP and VG report no competing interests, financial or propriety, in the subject matter or materials discussed in this paper. JHK is a consultant for Gilead Pharma, a company evaluating a treatment for non-infectious uveitis, and equity owner for Betaliq, a company developing an intraocular pressure-lowering treatment. RA is supported by a grant from the National Medical Research Council (NMRC) by Ministry of Health, Singapore, for the Clinician Scientist Award (CSA) from 2020 to 2023. He has not received funding for his work in this publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Agrawal, R., Ludi, Z., Betzler, B.K. et al. The Collaborative Ocular Tuberculosis Study (COTS) calculator—a consensus-based decision tool for initiating antitubercular therapy in ocular tuberculosis. Eye 37, 1416–1423 (2023). https://doi.org/10.1038/s41433-022-02147-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02147-7
This article is cited by
-
Infectious eye disease in the 21st century—an overview
Eye (2024)
-
Advanced drug delivery and therapeutic strategies for tuberculosis treatment
Journal of Nanobiotechnology (2023)