Abstract
Background
Patients with benign eyelid lesions make up a large proportion of referrals to the oculoplastic service and lend themselves well to telemedicine with assessments heavily reliant on history, observation-based examination and photographs to enable management decision-making. Our tertiary unit set up tele-oculoplastics clinics for all new patients referred for benign eyelid lesions comprising tele-consultation with antecedent patient photograph: Benign Eyelid Lesion Pathway (BELP). One year on, we describe a retrospective analysis of 974 patients looking at distinct parameters of effectiveness.
Methods
We retrospectively collected data from electronic patient records (EPR) for BELP patients from July 2020 to August 2021 (n = 974). We analysed time efficiency (referral time to treatment plan, consultation duration in minutes, average waiting times, number of patients seen per clinician and DNA rate), accessibility, safety (via video surveillance clinic) and theatre utilisation.
Results
57.3% (n = 558) were listed for a surgical procedure direct from tele-consultation with 94.9% (n = 513) of these proceeding to surgery; 22.8% (n = 222) were discharged, 10.7% (n = 104) had further video follow-up and 6.7% (n = 65) required face-to-face follow-up. Our results showed efficient referral-to-treatment times, waiting times, consultation times and non-attendance rate. There was only a 2.57% non-attendance rate. There was no missed diagnosis of a malignancy of a presumed benign lesion.
Conclusion
Tele-oculoplastics provides a streamlined, safe, effective, and logistically convenient way to review benign eyelid lesions. With the increased waiting times for referral to biopsy of eyelid lesions, this clinic shows it is imperative to provide digital accessibility for patient assessment and booking to operating theatre.
Similar content being viewed by others
Introduction
In the UK, ophthalmology continues to be the busiest outpatient specialty, with NHS Digital reporting 5.47 million attendances from 2020 to 2021 despite the impact of the coronavirus (COVID-19) pandemic [1]. Eye service demand is projected to rise by 30–40% over the next 20 years and inevitably the balance of capacity versus demand will be increasingly outweighed in what is already a very burdened system [2]. With these escalating predictions, long-term strategies must be realised to evolve the status quo of the conventional outpatient consultation, optimise capacity in a cost-effective way, overcome the busy waiting rooms and improve the patient journey. Telemedicine and digitally enabled outpatient care may be the solution.
In the oculoplastic service, patients with benign eyelid lesions make up the majority of referrals from primary care, with tertiary centres citing as much as 50% as the reason for referral [3]. Oculoplastics as a sub-specialty lends itself well to telemedicine, being a visual specialty heavily reliant on clinician history, observation-based examination and photographs [4]. Specifically, studies looking at asynchronous eyelid lesion assessment have demonstrated comparative diagnostic accuracy when compared to face-to-face examination [3, 5,6,7,8]. General reports of tele-oculoplastics have been published as early as 1999 and describe its uses in providing remote care to limited access areas and increase capacity whilst reducing cost [4, 9,10,11]. However, the recent fervour in its worldwide adoption amongst oculoplastic surgeons has provided more information on its value beyond the pandemic and how it should be specifically utilised. The most common use for tele-oculoplastics amongst oculoplastic surgeons has been for eyelid lesion patients [12, 13]. Despite this, clinician perspectives have been mixed and robust studies are required to discern effectiveness to encourage increased use of tele-oculoplastics for certain diagnoses in the long-term [12, 14].
Our tertiary unit set up tele-oculoplastic clinics for all new patients referred for benign eyelid lesions comprising a synchronous tele-consultation real-time virtual assessment, augmented with antecedent patient photograph [3]. Booking into minor surgery for a biopsy or incision and curettage was carried out based on this assessment so that a patient’s first face-to-face visit into hospital was on the day of surgery. Post-biopsy appointments were also continued virtually. One year on, we describe a retrospective analysis of 974 patients who were booked into this service, looking at individual parameters of effectiveness. Our specific objectives were to assess the following:
-
○
Efficiency
-
Time efficiency
-
Accessibility
-
Theatre utilisation
-
-
○
Safety
By analysing these parameters, we aim to describe a new streamlined approach to the benign eyelid lesion pathway; from now on referred to as BELP (Benign Eyelid Lesion Pathway). To our knowledge this is the first report describing a large-scale analysis of a tele-oculoplastics clinic for benign eyelid lesions.
Methods
Benign Eyelid Lesion Pathway (BELP)
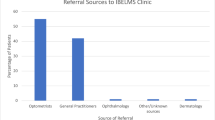
Patients referred with benign eyelid lesions were booked into a video consultation clinic (Fig. 1). Triage of referrals were carried out by consultant ophthalmologists and according to a list of ‘red flags’ which were agreed upon beforehand (Table 1). A red flag in the patient’s referral triggered a face-to-face clinic appointment within two weeks rather than a video consultation. Likewise, any red flag identified within the video consultation triggered a face-to-face clinic review within 2 weeks. Safety netting advice was given verbally to the patient and in their clinic summary letter, explaining to seek review if any red flags appeared. Patients were contacted in advance of the clinic appointment by booking clerks to check if they had a device with a camera and access to the internet. They also confirmed if they were competent users of digital services that enabled them to join a video call. Patients were asked to send self-captured photographs of their eyelid lesions prior to the video consultations by email to a designated inbox or by using a link to a survey, ‘SmartSurveyTM’ (Smartline International Ltd, UK), that enabled them to upload their photos. Patients who did not have video devices or refused virtual consultation were booked into general oculoplastic face-to-face clinics. On the day of the virtual assessment, patients underwent a live video consultation using ‘Attend Anywhere’ (Attend Anywhere Pty Ltd, Victoria, Australia). This platform was accessed via a URL in a web browser on tablets, smartphones, laptops or PCs. The antecedent patient-captured photographs generally provided higher resolution images compared to the video consultation. Patients that required booking into surgery were booked and consented during the video consultation. Eight to ten patients were seen per clinician per clinic. Clinicians included consultant oculoplastic surgeons, oculoplastic fellows, registrars and oculoplastic nurse practitioners.
Data collection
We retrospectively collected data from ‘OpenEyesTM’ electronic patient records (EPR) for all patients who went through the Benign Eyelid Lesion Pathway from 22nd July 2020 to 18th August 2021. Data included age, patient residence postcode, date of referral received, date of the appointment, provisional diagnosis, outcome (surgery, discharge, video follow-up, face-to-face follow-up), whether patients proceeded with surgery on their booked day, reasons for not proceeding and histopathological diagnosis where available. Hospital service managers provided clinic data on referral time to treatment plan, average waiting times within the clinic and consultation duration.
Efficiency analysis
We assessed time efficiency, accessibility and effective theatre utilisation of the BELP service. Time efficiency of BELP was inferred from referral time to treatment plan, consultation duration, average waiting times, number of patients seen per clinician and DNA rate (time lost). To analyse accessibility, we calculated direct distance between the patient’s residence postcode and our unit. Efficient theatre utilisation was determined as a percentage of cases that proceeded to surgery out of those listed for surgery.
Safety analysis
To analyse safety, a sub-study was performed on the first 50 patients seen through the BELP service. All patients deemed fit for discharge at first review were seen in a video surveillance clinic at 3 months for the purpose of analysing if the same diagnosis and management were made. If the outcome from the initial tele-consultation of the BELP service was to come in for surgery or have a face-to-face appointment, the surveillance assessment was carried out during this face-to-face visit and again a comparison was made of the initial diagnosis at the virtual consultation verses the face-to-face follow-up diagnosis.
Results
There were a total of 1101 appointments in the BELP service for 974 patients. The average age of patients was 40 years old, and the age range was from 16 to 97 years old. A total of 438 patients (45%) sent in their photographs by either email (n = 243) or completing a survey (n = 195). Most diagnoses at first tele-consultation were benign eyelid lesions, specifically documented as ‘chalazion’, ‘benign epidermal cyst’, ‘eyelid lesion, unspecified diagnosis’ and ‘benign eyelid lesion’ (Table 2). A minority of patients seen in BELP had diagnoses that were not eyelid lesions and on review of the referrals, were triaged to BELP due to insufficient or inaccurate information in the referral. These patients were seen on tele-consultation and the appropriate outcome was made.
In terms of outcomes, 57.3% (n = 558) were listed for a surgical procedure direct from the tele-consultation; 22.8% (n = 222) were discharged, and 17.3% (n = 169) had an outcome of further follow-up. Within the follow-up patients, 10.7% (n = 104) could be monitored via further virtual assessment whilst 6.7% (n = 65) required face-to-face follow up (Fig. 2). Twenty-five patients (2.57%) did not attend their first tele-consultation and were deemed ‘DNA’. Table 2 demonstrates a breakdown of outcomes according to diagnosis.
Time efficiency
BELP clinic consultations lasted on average 8 minutes. Waiting time was on average 13 minutes. Time from referral to clinic appointment was 11 weeks. The first appointment DNA rate was 2.57%.
Accessibility
The total sum of distances from the 974 patient resident postcodes to our unit was 7443.91 miles. Average distance from patients’ resident postcode to our unit was 7.67 miles.
Theatre utilisation
Out of the 558 patients listed for surgery, 94.9% (n = 513) proceeded to surgery. Out of the 45 patients who did not proceed to surgery, 48.9% (n = 22) was due to ‘DNA’, 37.8% (n = 17) had resolved lesions and were cancelled on the day of surgery, 11.1% (n = 5) were recorded as ‘declined surgery’ and 2.2% (n = 1) had their procedure cancelled due to high blood pressure. A summary is shown in Table 3.
Safety
For the first 50 patients seen in the BELP, all patients deemed fit for discharge at first review were seen in a video surveillance clinic at 3 months. There was no significant disagreement in diagnosis or management plans during this review: 7 patients with a diagnosis of chalazion at the first visit were deemed fit for discharge. They were all seen in a surveillance clinic at 3 months: 1 patient had a persistent chalazion and was listed for surgery and the other 6 patients had resolved lesions and were therefore safely discharged. 3 patients had a slightly different diagnosis from initial review to face-to-face: they were all initially suspected as having suspicious lesions on video consultation which turned out to be benign on face-to-face review; two of these were sent for biopsy of which the histological results were benign, and one case was sent for further face-to-face follow up. There were no missed diagnoses of a malignancy being incorrectly diagnosed as a benign lesion in the surveillance clinic.
142 patients had lid lesion biopsy and therefore histopathological diagnoses. Out of these, 60.6% (n = 86) had exactly the same clinical diagnosis made during virtual assessment as their histological diagnosis. The remainder of diagnoses were unspecified descriptions and did not permit concurrence with histology. There were no cases deemed to be benign on video assessment that came back as atypical or malignant except for one case diagnosed as ‘conjunctival lesion’ which had a histological report of ‘mild cytological atypia’. Four cases of ‘eyelid lesion, unspecified diagnosis” had histological diagnosis of basal cell carcinoma; in all cases biopsy was booked as ‘urgent’ and was performed within a week of being seen.
Discussion
Rising eye service demand, exacerbated by the protracted COVID-19 pandemic, forces us to consider alternate pathways for safe patient management and care. Telemedicine, already at the forefront of health service innovation, has fast gained usefulness and has transformed the way patient care is delivered. Our study has shown the effectiveness of its role within oculoplastics, specifically for benign eyelid lesions, and has shown validity in multiple measured parameters: time efficiency, accessibility, effective theatre utilisation and safety. The majority of the patients in our study were referred for benign eyelid lesions, ranging from chalazions to innocuous cysts and naevi, were diagnosed correctly and were effectively managed without the need for face-to-face assessment. This demonstrates that video assessment is an adequate and reliable platform for examining and assessing these types of patients. Additionally, a relatively high percentage of these patients were discharged after their first virtual assessment in a safe manner. In this way, the patient journey is effectively rationed to remove non-essential visits, whilst those patients that need face-to-face hospital appointments or surgical procedures can be triaged to receive this through tele-oculoplastics, allowing a streamlined service and efficient use of resources.
Most patients in our study were referred to the BELP service correctly with relatively low numbers of inappropriate referrals of eventual non-benign eyelid lesion diagnoses. Despite patients with non-eyelid lesions being triaged to this clinic (likely due to insufficient or inaccurate information in the referral) only 6.7% of patients required further face-to-face assessment. This raises the question of whether patients with other oculoplastic presenting complaints have the scope to be examined through tele-oculoplastic means to reach an accurate diagnoses and management plan.
Time efficiency
In terms of waiting times, the BELP service surpassed our centres 15-week average waiting time for a general oculoplastic clinic appointment, with an average waiting time of 11 weeks for referral to treatment. This is comparatively shorter than the NHS benchmark for maximum waiting time for referral to treatment of 18 weeks, making the BELP significantly better than the national standard. Within clinics themselves, the BELP service demonstrated waiting times of 13 minutes on average, in comparison to 1–2 hours in our centre’s routine face-to-face outpatient oculoplastic clinics. Coupled with the elimination of travel time and travel cost, tele-oculoplastics would be a seemingly easier and more efficient option for patients. Patients who fail to attend their appointment, incur significant economic costs to the NHS due to rescheduling and inefficient use of resources; the cost of missed outpatient clinic appointments in the NHS in England in 2017/2018 was projected to be £1 billion [15]. The overall DNA rate of 2.57% for the BELP service was significantly lower than the average overall DNA rate of 18.43% for comparative face-to-face clinics in our centre. Although the costs of DNAs were not calculated, we can only assume this is a significant economic saving. The BELP DNA rate was also significantly lower than the average DNA rate for national first outpatient appointments of 8.7%, according to NHS England’s quarterly activity return data (2008–2018) [16]. The reasons for this were not explored in this study but these figures imply tele-oculoplastics is more convenient for these patients. It is also likely that the administrative support used to contact patients in advance of the clinic appointment allowed a careful explanation and instructions of the new pathway to allow patients effective access to the video consultations and reduce non-attendance.
Within the BELP session, clinicians saw 8–10 patients compared to 8 profiled patients in an average face-to-face clinic. The average consultation time of 8 minutes was also a significant reduction in comparison to our centres’ face-to-face consultation time of on average 15 minutes. Both of these figures contribute to improving the patient turn-around time, operational clinic flow and ultimately the patient journey. Improved time efficiency consequently leads to better affordability. National calculations are currently being conducted to estimate the cost of a video consultation but inference in comparison to a face-to-face clinic can be made. Specifically, for the BELP Service, there is no need for a clinic space and consequently no overhead costs. Nursing support is also not required, and a virtual receptionist is usually shared between several video clinics running alongside each other. In contrast, an equivalent face-to-face clinic, requires a clinic space, clinician, nursing staff and allocated receptionist. With less resources required, video clinics are much more likely to be cost effective compared to face-to-face clinics. In addition, tele-consultation is easier to scale without the restrictions of requiring physical space. This allows us to address the increasing demand amidst limited resources, improve access to care, reduce referral to treatment time and improve outpatient efficiency.
Accessibility
Although the initial implementation of tele-medicine was to prevent infections in the community during the pandemic, it is likely to remain a highly relevant means of primary access to healthcare, more so in a digital age when travel to the workplace is being cut down to reduce the impact on the environment. The convenience of avoidable travel for an appointment, triage or treatment plan has clearly demonstrated a high take-up rate from patients as indicated by the low DNA numbers in our study. This is also supported by the results of other studies [17]. In addition, the significant number of miles saved in travel (7443.91 miles or 11979.8 kilometres) by 974 patients is the exact flight distance between Cancun International Airport (Mexico) to Tokyo-Narita International Airport (Japan) across the Pacific Ocean. The total carbon footprint of this flight is approximately 1.7 metric tonnes of carbon dioxide emission (CO2e). This is just a distance figure for first appointments and did not include second virtual appointments which would make this distance even higher. Healthcare service provision in general is extremely energy intensive and produces a significant amount of hazardous and non-hazardous materials that contribute to polluting emissions [18]. The need for patient safety and quality of care as a primary objective means an environmental strategy is a low priority. However, the growing environmental awareness from individuals and regulations is a problem that requires consideration; telemedicine is a logistically easy but significant means to minimise impact on climate derived from the travel industry and is an effective solution.
Safety
Our study portrayed the BELP service as a clinically safe alternative to face-to-face consultation. Those lesions that were deemed ‘suspicious’ were correctly identified and booked in for further management. In the initial safety audit of 50 consecutive cases, three lesions initially identified as suspicious were deemed to be benign on face-to-face review. This is entirely appropriate as a higher level of suspicion needs to be used when assessing a patient virtually. Feasibility of assessing eyelid lesions using asynchronous telemedicine has already been validated in a study looking at 44 cases using patient photographs [3]. Not only does our study corroborate these conclusions but adds to it by demonstrating validity in a significantly high number of assessed patients (949 individuals) rendering the BELP service safe for patient management and clinician utilisation. Additionally, our study consultations were conducted by several clinicians of different levels including nurse practitioners imitating a real clinic scenario of multiple healthcare professionals of varying experience, expertise and knowledge. Regardless, we had a safe service and high diagnostic accuracy. Our study also improves upon the two-dimensional character of photographic evaluation in previously published studies by way of video assessment, which would likely ameliorate the examination process of a 3D lesion. It is also acceptable to assume that patients would find the consenting process more satisfactory over video than telephone given they have direct visualisation of the healthcare professional and non-verbal communication remains intact. This would likely make the consultation more effective and increase patient understanding. Further study is required to properly evaluate the consenting process over video in comparison to telephone and face-to-face appointment. Visual acuity although not assessed was deemed unnecessary for benign eyelid lesion examination since the majority of these patients would not have visual disturbance. No patient in our study had a diagnosis that would have benefited or changed through visual acuity assessment. They were advised to seek further ophthalmological evaluation by their local optometrist or local eye unit if they expressed concerns about their vision.
Theatre utilisation
The BELP service led to efficient theatre utilisation with a low rate of on-the-day cancellations. This supports the concept of providing a telemedicine service for benign and non-urgent eyelid lesion patients. The high number of patients proceeding to surgery (513 out of 558) infers that the correct initial diagnosis and outcome was made via tele-consultation and patients had enough information to follow-through with a procedure.
Limitations
The BELP service occurred during the Covid-19 pandemic and so practice patterns may be different compared to pre-pandemic. During the pandemic, patients who are listed for surgery might be more likely to proceed with surgery resulting in a lower on-the-day cancellation rate. A formal assessment of patient satisfaction was not performed during this study. Clinician satisfaction was also not assessed but has been assessed in other studies specifically within the realm of tele-oculoplastics and has proven to be an important barrier that needs addressing in order to implement telemedicine as the primary service [14]. Even though the current video consultation resolutions were sufficient to safely list for theatre for some patients, especially for chalazions, the role of good quality video with a minimum resolution requirement requires formal evaluation. Additionally, antecedent photographs were taken by patients themselves and these are limited by angle, resolution and focus.
An important limitation of the BELP service is digital exclusion of particular patients unable to access the Attend Anywhere platform. There are various reasons for barriers to access including cost to patients, age-related difficulty in use of technology and systemic and ophthalmic disease-related difficulty with using digital platforms. This exposes our study to a patient selection bias and in turn limits the effectiveness of the pathway. Future study should explore specific reasons of digital exclusion and ways to improve this. An adjunct role of photographs taken at local optometrists may resolve one aspect of digital exclusion and reduce the number of face-to-face consultations in the NHS oculoplastic service [3]. In terms of hospital barriers for tele-medicine implementation, these may include lack of administrative support, technology costs, integration with existing electronic medical record systems, and education and training of staff using these systems [19].
Conclusion
We introduce our digitally powered benign eyelid lesion service that shows promise in addressing the increased oculoplastic outpatient burden by delivering a safe and efficient high-volume benign eyelid lesion patient care pathway. Further safety audit and user satisfaction survey are warranted to ensure continued safety of a newly introduced service.
Summary
What was known before
-
The role of asynchronous telemedicine in Ophthalmology is well established particularly in medical retina and glaucoma. The Covid-19 pandemic has accelerated the adoption of synchronous telemedicine in the management of oculoplastic patients.
What this study adds
-
Our study demonstrates the effectiveness and safety of synchronous teleophthalmology service in the management of patients with benign eyelid lesions.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to patient identifiable data but are available from the corresponding author on reasonable request.
References
NHS Digital. Hospital Outpatient Activity 2020-21—NHS Digital. 2021. Accessed 21 Nov 2021. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-outpatient-activity/2020-21#
Royal College of Ophthalmology. Workforce Census 2018. 2019. Accessed 21 Nov 2021 https://www.rcophth.ac.uk/wp-content/uploads/2019/02/RCOphth-Workforce-Census-2018.pdf
Kang S, Dehabadi M, Sim DA, Thomas PBM, Appiah Ewusi D, Ezra D. Accuracy of periocular lesion assessment using telemedicine. BMJ Health Care Inform. 2021;28:e100287.
Verma M, Raman R, Mohan RE. Application of tele-ophthalmology in remote diagnosis and management of adnexal and orbital diseases. Indian J Ophthalmol. 2009;57:381–4. http://www.who.int/archives/int-pr-1997/en/pr97-98.html
Rossato LA, Carneiro RC, Miyazaki A, Matayoshi S. Accuracy of clinical examination in the diagnosis of eyelid lesions. Rev Brasileira de Oftalmologia 2014;73:324–8.
Soto JL, Vrcek I, Ozgur O, Mancini R. Evaluating the growth of eyelid lesions: comparison of clinical evaluation and a software-based model. Int Ophthalmol. 2017;37:1257–61.
Kersten RC, Ewing-Chow D, Kulwin DR, Gallon M. Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology 1997;104:479–84.
Hind J, Edington M, McFall K, Salina E, Diaper C, Drummond S. et al. An image-based eyelid lesion management service—evaluation of a pilot. Eye. 2022;36:1314–8.
Rayner S, Beaconsfield M, Kennedy C, Collin R, Taylor P, Murdoch I. Subspecialty adnexal ophthalmological examination using telemedicine. J Telemed telecare. 2001;7:29–31.
Threlkeld AB, Fahd T, Camp M, Johnson MH. Telemedical evaluation of ocular adnexa and anterior segment. Am J Ophthalmol. 1999;127:464–6. https://www.sciencedirect.com/science/article/abs/pii/S0002939498003559
Hwang CJ, Eftekhari K, Schwarcz RM, Massry GG. The aesthetic oculoplastic surgery video teleconference consult. Aesthetic Surg J. 2019;39:714–8.
Lelli GJ, Luo S, Liu Y, van Landingham SW. Telemedicine Use by Oculoplastic Surgeons During the COVID-19 Pandemic. Telemed e-Health. 2021.
Kang S, Thomas PBM, Sim DA, Parker RT, Daniel C, Uddin JM. Oculoplastic video-based telemedicine consultations: Covid-19 and beyond. Eye. 2020;34:1193–5.
Kang S, Raja L, Sim DA, Thomas PBM, Ezra DG Telemedicine in oculoplastic and adnexal surgery: clinicians perspectives in the UK. Br J Ophthalmol. 2021. https://bjo.bmj.com/content/early/2021/04/27/bjophthalmol-2020-318696
Kiruparan P, Kiruparan N, Debnath D. Impact of pre-appointment contact and short message service alerts in reducing ‘Did Not Attend’(DNA) rate on rapid access new patient breast clinics: a DGH perspective. BMC Health Serv Res. 2020;20:1–9.
NHS England. NHS England. Quarterly Hospital Activity Data. 2018-2019.
Almathami HKY, Win KT, Vlahu-Gjorgievska E. Barriers and Facilitators That Influence Telemedicine-Based, Real-Time, Online Consultation at Patients’ Homes: Systematic Literature Review. J Med Internet Res. 2020;22:e16407–e16407. https://pubmed.ncbi.nlm.nih.gov/32130131
Karlsson M, Öhman DP. Material consumption in the healthcare sector: Strategies to reduce its impact on climate change—The case of Region Scania in South Sweden. J Clean Prod. 2005;13:1071–81.
Fryer K, Delgado A, Foti T, Reid CN, Marshall J. Implementation of Obstetric Telehealth During COVID-19 and Beyond. Matern child health J. 2020;24:1104–10. https://pubmed.ncbi.nlm.nih.gov/32564248
Acknowledgements
We would like to thank the clinicians who see patients in the BELP clinic and Caroline Kilduff for creating the illustrations.
Author information
Authors and Affiliations
Contributions
Conception: SK, DS, PT, CD, JU, DE Methodology: LA, SK, AG, HT Investigation: LA, SK, AG, HT Formal analysis: LA, AB, AG Initial drafting: LA, AB Revision: LA, AB, SK, HT, AG Final approval: SK, DS, PT, CD, JU, DE.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Permission to perform this study as a clinical audit was granted by Moorfields Eye Hospital NHS Foundation Trust. Ethical approval was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ah-Kye, L., Butt, A., Gupta, A. et al. Introducing the ‘Benign Eyelid Lesion Pathway’: 1 year experience of synchronous tele-oculoplastics in a tertiary hospital. Eye 37, 1458–1463 (2023). https://doi.org/10.1038/s41433-022-02166-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02166-4