Abstract
Purpose
Genetic testing is an important diagnostic tool in pediatric genetics clinics, yet many patients face barriers to testing. We describe the outcomes of prior authorization requests (PARs) for genetic tests, one indicator of patient access to clinically recommended testing, in pediatric genetics clinics.
Methods
We retrospectively reviewed PARs for genetic tests (n = 4,535) recommended for patients <18 years of age (n = 2,798) by pediatric medical geneticists at two children’s hospitals in Texas, 2017–2018. We described PAR outcomes, accompanying diagnostic codes, and diagnostic yield.
Results
The majority (79.9%) of PARs received a favorable outcome. PARs submitted to public payers were more likely to receive a favorable outcome compared with private payers (85.5% vs. 70.3%, respectively; p < 0.001). No diagnostic codes were associated with higher likelihood of PAR approval for exome sequencing. Among the 2,685 tests approved and completed, 522 (19.4%) resulted in a diagnosis.
Conclusion
Though there was a high PAR approval rate, our findings suggest that insurance coverage remains one barrier to genetic testing. When completed, genetic testing had a high yield in our sample. Further evidence of clinical utility and development of clinical practice guidelines may inform payer medical policy development and improve access to testing in the future.
Similar content being viewed by others
INTRODUCTION
Genetic testing is an important diagnostic tool for pediatric patients, as results can potentially guide medical management, inform decision-making, and improve access to social services. Evidence on the clinical utility and cost-effectiveness of various forms of genetic testing and genomic sequencing for pediatric patients continues to build.1,2,3,4 However, the rapid evolution of the genetic testing evidence base presents an interrelated challenge to development of both clinical guidelines and insurance coverage policies. Patient access to genetic and genomic tests depends upon several factors that may be unrelated to clinical need. Insurance coverage is one such factor, as medically actionable genetic variants are identified in a similar proportion of patients facing insurance barriers to testing as those who do not face such barriers.5,6
Reviews of US payer medical policies have found variation in coverage of genetic tests and testing technologies.7,8,9,10,11,12 Although coverage analysis has focused on private payers, coverage may also vary between state Medicaid and Children’s Health Insurance Program (CHIP) plans, which are relevant to pediatric patient access to testing. Moreover, the types of evidence used for development of coverage policies differs not only by test type, but also between payers.13 Coverage policies frequently cite published clinical practice guidelines for genetic tests, however, indicating that establishment of consensus clinical opinion may influence policy development.12,13 Yet even clinical consensus and guideline development is challenging given the number of tests available for dozens of pediatric clinical indications.4
For example, there is currently no clinical guideline for the use of exome sequencing (ES) or genome sequencing (GS). Of reviewed private payer policies in the United States, nearly half did not formally cover pediatric ES.7,14 While private payers have indicated recognition of the merit of pediatric ES, concerns about insufficient evidence of clinical utility, potential for inappropriate use, and difficulty in result interpretation remain.15 The definition of clinical utility is itself a further complicating factor in decision-making, as no single definition has been universally accepted by clinicians or payers.16,17
Given this variability in coverage, a preauthorization or predetermination request, which are collectively referred to as a prior authorization request (PAR), is often completed prior to initiation of genetic testing in outpatient settings. Approval of a PAR provides a patient or family reassurance that the claim issued at the time of service will be accepted by their specific payer. PARs contain information about the recommended test including the Current Procedural Terminology (CPT) codes to be billed; International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes; ordering provider credentials; billing institution; and clinical documentation. A PAR is reviewed by a given payer to determine expected coverage for the service. If the PAR is approved and the claim at time of service reflects the PAR, the patient can expect the claim will be accepted by the payer and is reassured to proceed with the test. If the PAR is denied, the claim at time of service is likely to be denied, and the patient may have to pay out of pocket for testing. When a PAR is denied, payers typically offer the opportunity to complete a peer-to-peer appeal or a written appeal that can have restrictive time limits. Additional review of a denial may be available, including a fair hearing or legal proceedings, but these options typically are extremely time-consuming and require outside help. If a denial is upheld, the patient typically will defer testing or pay out of pocket. Some payers issue PAR decisions to indicate PA is not required; the payer does not review the PAR before the claim at time of service or a particular test or a CPT code is always covered and does not require review.
PAR outcomes can therefore serve as an indicator of how payer coverage policy, as applied in practice, impacts access to testing. Research on genetic testing insurance coverage has largely focused on the payer perspective through analysis of medical policies. However, less is known about approval of clinically recommended patient testing in real-world clinical care settings, which is one indicator of patient access to testing. To address this aspect of access, the aim of this study is to describe outcomes of PARs for genetic tests in outpatient pediatric genetics clinics. We analyze PAR outcomes for clinically recommended tests in a diverse patient population covered by both private and public payers in two large pediatric outpatient genetics clinics in Texas. At the test level, we describe recommendation frequency, PAR outcomes, and test outcomes. We also explore clinical diagnostic codes, which may be associated with approval decisions, submitted on PARs by genetic test type.
MATERIALS AND METHODS
Methods
We completed a retrospective electronic medical record review of all PARs that received a decision letter for genetic tests recommended for patients younger than 18 years of age by pediatric medical geneticists at the Children’s Hospital of San Antonio in 2017 and Texas Children’s Hospital in Houston in 2017 and 2018. Only tests submitted by genetics staff under an institutional billing arrangement were included.
Patient records were reviewed to document the age of the patient at time of PAR submission, genetic test name, CPT code(s) for the test, ICD-10-CM code(s), payer, PAR submission date, PAR decision date, PAR outcome (approval, denial, or no PA required), reason for denial (if applicable), outcome of the genetic test (diagnostic, variant of uncertain significance [VUS], not diagnostic) if completed, and diagnosis (if applicable). All analyses were performed at the test level. We grouped tests into five categories: cytogenetic and molecular (including chromosome microarray [CMA] and FMR1 repeat expansion analysis for fragile X syndrome and excluding single-gene or multigene panels), epigenetic, exome (including proband only, duo, and trio analyses), mitochondrial, and single-gene or multigene panels.
We calculated descriptive statistics at the test level on PAR outcome, time to PAR result, diagnostic yield by test type, and reason for PAR denial. We considered PAR approvals and PA not required as favorable outcomes because patients were encouraged to proceed with the recommended genetic test if desired. In contrast, PAR denials were followed by counseling the patient to not proceed with the recommended genetic test and to consider alternative billing or testing options. Within test categories, we analyzed outcomes for several specific tests that are frequently ordered and especially relevant to pediatric patient populations including CMA and FMR1 repeat expansion analysis to diagnose fragile X syndrome. ES analyses included proband only, duo of proband and one parent, and trio of proband and two parents. We analyzed approval rates and calculated odds of a favorable PAR outcome for ES and CMA associated with the following clinical conditions (ICD-10-CM codes): autism (F84.0), developmental delay (F80.4, F82, F88, F80.9, R62.50), intellectual disability (F79, F70–78, F81.9), seizures and epilepsy (G40–40.919), and multiple congenital anomalies (Q89.7), which capture the most common reasons for referral to the genetics clinic. The codes for autism, developmental delay, intellectual disability, and multiple congenital anomalies are also included in consensus practice guidelines for genetic testing recommendations. Additionally, we explored the frequency of ICD-10-CM codes submitted with PARs. We used Student’s t-tests and chi-square tests for continuous and categorical outcomes, respectively, to analyze aspects of PAR decisions according to test type and clinical diagnostic categories. Results were considered statistically significant if p < 0.05. Data analysis was performed in Stata 15 (College Station, TX). This study was approved by the Baylor College of Medicine and CHRISTUS Health Institutional Review Boards. Informed consent was not required for this retrospective electronic medical record review study.
RESULTS
Description of prior authorization requests and clinical codes
Our data included 4,535 unique test PARs for 2,798 patients. Table 1 presents descriptive statistics on PARs. Mean (SD) patient age at PAR submission was 6.0 (4.7) years. Median (Q1, Q3) time between PAR submission and decision was 5.0 (2.0, 12.0) days. Most tests were submitted under public insurance plans (63.8%, n = 2,893). Public payers included 23 Medicaid/CHIP plans and private payers included 61 national, regional, and local payers. Requests for cytogenetic and molecular tests (49.0%, n = 2,224) were most frequent, followed by single-gene and multigene panel tests (31.1%; n = 1,411), exome sequencing (17.0%, n = 773), epigenetic tests (1.9%, n = 86), and mitochondrial tests (0.9%, n = 41).
The number of ICD-10-CM codes per test ranged from 1 to 15. There were 1,113 unique ICD-10-CM codes across all tests, 349 of which were used at least five times. Overall, the three most frequent ICD-10-CM codes were R62.50 (Unspecified lack of expected normal physiological development in childhood; n = 779), F84.0 (Autistic disorder; n = 688), and F88 (Other disorders of psychological development, n = 364). Among PARs for exome sequencing, the same three codes were also the most frequent (n = 165, n = 114, n = 77, respectively).
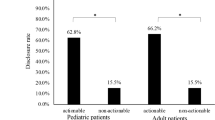
Prior authorization request outcome
The majority of PARs were approved (71.3%, n = 3,235) or did not require PA (8.6%, n = 392), whereas 20.0% (n = 908) were denied. Among the 3,627 (80.0%) tests with a favorable outcome (PA approved or not required), 26.0% (n = 942) were not completed by the patient. Among the 908 denied PARs, the most frequently cited reasons for denial (Table 2) were that the test was not medically necessary/not essential for medical management (31.1%) and the test was considered experimental or investigational (23.7%). Overall, tests requested for patients with public insurance were more likely to receive a favorable outcome (85.5%) compared with requests for patients with private insurance (70.3%; p < 0.001; Table 3).
Among PARs for CMA, those with an autism ICD-10-CM code (F84.0) were more likely to receive a favorable outcome than PARs without an autism diagnostic code (odds ratio: 1.79; 95% confidence interval: 1.09, 2.94). No other clinical diagnostic codes that we examined were associated with approval of ES or CMA (Table 4). The vast majority of cytogenetic PARs accompanied by the three most frequent codes, R62.50 (Unspecified lack of expected normal physiological development in childhood), F84.0 (Autism), and F88 (Other disorders of psychological development), received favorable PAR outcomes (90.7%, 95.0%, and 90.0%, respectively).
Diagnostic yield of completed tests
The overall diagnostic yield among the 2,685 tests that were approved and completed was 19.4% (n = 522) and varied by test type (Table 5). Of cytogenetic tests, CMA had a diagnostic yield of 13.4% (135/1,011) and FMR1 repeat expansion analysis for fragile X had a yield of 1.0% (4/390). Single-gene sequencing and deletion/duplication analyses (n = 435) and multigene panel tests (n = 312) resulted in a diagnosis in 29.9% (223/747) of cases.
Exome sequencing results
Patient age and time to PAR decision did not differ between ES and other tests. The number of PARs for exomes compared with all other genetic tests collectively varied by payer type, with a larger portion of exomes billed to private insurance (49.2%) than other genetic tests (33.5%; p < 0.001). There were 250 PARs for ES that were denied, 110 from public payers and 140 from private payers. Slightly more than half of the patients who completed ES had public insurance (n = 225, 54.48%).
A total of 413 ES tests were approved and completed, including 35 proband only, 18 duos of proband and one parent, and 360 trios of proband and two parents. The diagnostic yield of trio exomes (31.4%) did not differ from proband exomes (20.0%; p = 0.162). Although duo testing had the highest yield (44.4%), it was not significantly different from the proband (p = 0.061) or trio yield (p = 0.247). The overall diagnostic yield of ES (31.0%) was higher than that for other types of testing combined (394/3,762, 17.3%; p < 0.001). In addition to the 31.0% of ES tests overall with a diagnostic result, 48 (6.2%) ES results were inconclusive (i.e., resulted in a VUS that was considered potentially clinically significant by the patient’s medical geneticist).
DISCUSSION
In this retrospective review of 4,535 PARs for genetic tests at two large outpatient genetics clinics at children’s hospitals in Texas, the vast majority of tests (80.0%) received a favorable outcome providing the opportunity for a patient to proceed with a recommended genetic test. Public payers were significantly more likely than private payers to give a favorable decision for all test categories other than mitochondrial. One potential explanation could be that the public payers in our sample had medical policies that were more easily accessible and interpreted by health-care providers. For example, during the study period, one of the public payers altered its medical policy to state that ES was not a covered benefit. After this notification, PARs for ES were no longer submitted; instead, PARs for large gene panels were submitted in an effort to obtain a molecular diagnosis for patients unable to complete ES due to this payer policy change. It is challenging, however, for health-care providers to be versed in the details of all medical policies and track their changes. Moreover, clinically indicated testing that is not covered may not always have a reasonable substitute, which can potentially lead to underutilization of genetic testing and underdiagnosis of genetic conditions.7
To improve access to and appropriate utilization of genetic testing, professional organizations and clinicians are continually working toward development of consensus recommendations for genetic testing in a pediatric population. For example, in 2010, the American College of Medical Genetics and Genomics (ACMG) published a practice guideline on the utility of array-based technologies and recommended CMA as a first-tier test for individuals with autism spectrum disorder, apparent nonsyndromic developmental delay or intellectual disability, and multiple congenital anomalies.18 Shortly thereafter, another practice guideline from ACMG was published highlighting the importance of genetics evaluation and genetic testing via CMA and FMR1 repeat expansion analysis for fragile X syndrome in individuals with autism spectrum disorder.19 These practice guidelines are frequently cited as evidence in payer medical policies.7 In our data, the majority of cytogenetic PARs accompanied by ICD-10-CM codes for autism spectrum disorder, developmental delay, and intellectual disability received favorable outcomes (90.7%, 95.0%, and 90.0%, respectively). Specifically, PARs submitted with the autism F84.0 code were associated with an approval (Table 2). This may demonstrate the value of practice guidelines to improve patient access to medically recommended genetic tests. ACMG recently published a systematic evidence-based review on outcomes of ES and GS in pediatric patients with congenital anomalies or intellectual disability, but it is unclear whether or how this review will influence payer policy or the potential downstream impact on patient access to ES and GS.20
When considering the development and use of practice guidelines, stakeholders should acknowledge the wide variety of clinical indications for genetic testing. We analyzed five common ICD-10-CM code groups submitted with PARs for ES, representing some of the most common reasons to recommend genetic testing in a pediatric population, and the inclusion of none of these codes was independently associated with a higher likelihood of a favorable PAR outcome. This may be because some payers have policies excluding ES regardless of ICD-10-CM code or clinical indication for testing. Our finding of 349 ICD-10-CM codes used at least five times across PARs demonstrates the vast range of clinical indications for genetic testing that should be considered and addressed in practice guidelines.
In our data, the most commonly cited reasons for denying a PAR were because the payer considered the genetic test to be not medically necessary/not essential for medical management (31.1%) or considered the genetic test to be experimental/investigational (23.7%). This suggests that further documentation and evidence of the utility of genetic testing is still needed. Medical policies about genetic testing can evolve, albeit slowly, as new evidence accumulates over time, with favorable implications for patient access to genetic tests.7 The data used in this analysis is from 2017 and 2018 and may not reflect current practices.15
Clinical experience over time may help build the evidence base for genetic testing utility, and in turn, also improve patient access to testing. Array-based technology was first described in the 1980s and has been used routinely for clinical testing for approximately 20 years.21 The frequent usage and favorable PAR outcomes for CMA in our data may reflect the lengthy experience of health-care providers, laboratories, and payers with the test. Cytogenetic and molecular tests including karyotype, CMA, and FMR1 repeat expansion analysis for fragile X syndrome have been performed in a clinical setting longer than many of the other genetic test types. These tests were requested and approved more frequently, and the utility of these tests are widely accepted. For example, CMA is routinely utilized, by both genetics and nongenetics providers, as a first-tier genetic test in the setting of nonspecific symptoms such as developmental delay with or without dysmorphic features, congenital anomalies, and short stature. CMA also often serves as a complement to ES, which is not designed to detect small copy-number variants.
However, some individuals still face insurance barriers to completing CMA and other well-established genetic testing technologies despite practice guidelines and an abundance of peer-reviewed literature citing the clinical utility and medical necessity of the test. This raises concern about the ability and willingness of stakeholders to adapt genetic test recommendations to quickly evolving testing technologies. For example, although ES has been commercially available as a clinical test for approximately ten years, our findings are consistent with the literature and suggest a significant proportion of patients face insurance barriers to ES and many payers still consider this test experimental or investigational.21
ES had the second highest denial rate behind mitochondrial testing and was comparable to the denial rate of PARs for single-gene and gene panel tests. While much attention in the coverage policy literature has focused on ES, this may indicate that insurance barriers to genetic testing for next-generation sequencing and ES are similar. Diagnostic yield among approved and completed tests was also similar, with 29.8% of single-gene and panel tests and 31.0% ES cases resulting in a diagnosis. The similar PAR outcomes and diagnostic rates for ES and single-gene and gene panels are notable because single-gene tests and panels are most commonly used when there is clinical suspicion for a particular genetic condition or group of conditions while ES is typically used when a differential diagnosis is broad and not reminiscent of a particular syndrome.
The diagnostic yield of ES in our data was 31.0%, which is consistent with previous reports.1,3,22,23 ES was significantly more likely to yield a diagnosis when compared against all other types of testing collectively, which reflects the usefulness of ES as a diagnostic tool in the pediatric genetics clinic. That the most common ICD-10-CM codes submitted with PARs for ES were the same as those most frequently submitted with cytogenetic and molecular tests (R62.50, F84.0, and F88) may be a reflection of the most common referrals to the genetics clinic, but also may be because patients with nondiagnostic, first-tier cytogenetic and molecular tests were then recommended for more comprehensive genetic testing such as ES. Further analysis of the diagnoses made by ES, including the changes to medical management and potential downstream cost savings, should be explored to further demonstrate clinical utility of ES and support the establishment of practice guidelines.
Unlike ES, the diagnostic yield of CMA in our study was 13.4%, which is lower than expected. A majority of PARs for CMA included ICD-10-CM codes related to autism spectrum disorder, developmental delay, or intellectual disability, and the diagnostic rate of CMA for these clinical indications is reported to be up to 15–20%.24 Testing for fragile X syndrome was diagnostic in 1.0% of tested patients. Both outpatient genetics clinics in this study follow ACMG recommendations to complete testing for fragile X syndrome as a first-tier genetic test for a patient with developmental delay, intellectual disability, or autism spectrum disorder. However, recent studies have presented similarly low fragile X syndrome diagnostic rates in cohorts of patients with intellectual disability and autism spectrum disorder in absence of specific symptoms or family history.25,26
Although a majority of tests in our sample (79.9%) received a favorable PAR, patients did not complete 26.0% of those tests, which suggests that insurance coverage considerations were not the only potential barrier to testing. During the study period, patients had to return to the billing institution to provide a blood sample for testing after PAR approval, which might have deterred patients in our sample from completing genetic testing. Known barriers to pediatric genetic testing access include transportation issues, concern about costs, lack of perceived benefit of test, and unclear changes to management based on test,27,28 all of which we suspect are relevant for patients in our sample, the majority of whom were able to qualify for public insurance. Moreover, although the cost of genetic testing is decreasing, patients with private insurance who have a high deductible may still face financial barriers to genetic testing regardless of PAR outcome. Further analysis of the barriers to access of genetic testing from a patient perspective in a general genetics pediatric outpatient clinic is warranted.
Our findings should be interpreted in light of several limitations. First, we only include PARs submitted from two institutions in Texas, so our results might not be generalizable to other regions of the country. However, both clinics are large and serve a diverse patient population; Texas Children’s Hospital genetics clinic alone serves more than 3,000 families each year from across the state and nation.29 Second, we cannot make any inferences about whether PAR outcomes are consistent with medical policy of each payer or with clinical guidelines, which would require a comparison of PARs to policy language and is outside the scope of this paper. Third, as discussed above, one of the public payers changed its medical policy during the study period. Our data, therefore, reflect a shift in behavior to respond to this policy change. If all patients who were recommended for ES and covered by this payer had been submitted, there would have been more denied ES PARs. Finally, we do not examine the appeal process to overturn denied PARs. To provide further evidence on patient access to testing, further work should examine billing claims and medical policies using a sample frame of clinically indicated tests.
This retrospective review of PARs for genetic tests in pediatric outpatient genetics clinics provides a novel description of how insurance PARs can impact patient access to genetic testing. The outcome of a PAR does not guarantee payer coverage or denial of a genetic testing claim, but it can be useful for patient decision-making from a financial perspective about whether to pursue recommended genetic testing. Our findings regarding ICD-10 codes suggest that professional societies’ practice guidelines and length of clinical experience with a test may help improve patient access to a genetic test. However, the variability of clinical indications for genetic testing in pediatrics and lack of systematic evidence on clinical utility of a test represent current barriers to patient access to genetic tests regardless of payer. While individuals with public insurance had higher proportions of favorable PAR outcomes than patients with private insurance, individuals who qualify for public insurance may have fewer financial resources to pay for recommended genetic testing out of pocket if a PAR is denied, potentially contributing to health disparities if genetic testing leads to improved health. Genetic testing in a pediatric population is expected to continue to be a valuable diagnostic tool. However, to realize the maximum level of health benefits that the availability of such diagnostics might provide, better understanding of the factors that influence patient access to testing is critical.
Data availability
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Niguidula, N. et al. Clinical whole-exome sequencing results impact medical management. Mol. Genet. Genomic Med. 6, 1068–1078 (2018).
Clark, M. M. et al. Meta-analysis of the diagnostic and clinical utility of genome and exome sequencing and chromosomal microarray in children with suspected genetic diseases. NPJ Genom. Med. 3, 16-018-0053-8 (2018).
Vissers, L. E. L. M. et al. A clinical utility study of exome sequencing versus conventional genetic testing in pediatric neurology. Genet. Med. 19, 1055–1063 (2017).
Phillips, K. A. et al. Payer coverage policies for multigene tests. Nat. Biotechnol. 35, 614–617 (2017).
Reuter, C. M. et al. Yield of whole exome sequencing in undiagnosed patients facing insurance coverage barriers to genetic testing. J. Genet. Couns. 28, 1107–1118 (2019).
Amendola, L. M. et al. Insurance coverage does not predict outcomes of genetic testing: the search for meaning in payer decisions for germline cancer tests. J. Genet. Couns. 28, 1208–1213 (2019).
Babu, D. et al. Understanding genomic testing utilization and coverage in the US. 2020 http://www.personalizedmedicinecoalition.org/Userfiles/PMC-Corporate/file/PMC_Understanding_Genomic_Testing_Utilization_and_Coverage_in_the_US2.pdf?utm_source=hs_email&utm_medium=email&_hsenc=p2ANqtz-8ElNl42Kvj9gsBfDJ2Ccyl94nnM6VAYUeLgdCpiN9wkkJc9SOJTj5a8AgLxMbK_k-M9yro.
Phillips, K. A. et al. Genomic sequencing: Assessing the health care system, policy, and big-data implications. Health Aff. (Millwood) 33, 1246–1253 (2014).
Trosman, J. R., Weldon, C. B., Kelley, R. K. & Phillips, K. A. Challenges of coverage policy development for next-generation tumor sequencing panels: experts and payers weigh in. J. Natl Compr Canc Netw. 13, 311–318 (2015).
Deverka, P. A. & Dreyfus, J. C. Clinical integration of next generation sequencing: coverage and reimbursement challenges. J. Law Med. Ethics 42, 22–41 (2014).
Graf, M. D., Needham, D. F., Teed, N. & Brown, T. Genetic testing insurance coverage trends: a review of publicly available policies from the largest US payers. Per. Med. 10, 235–243 (2013).
Khoury, M. J. et al. The evidence dilemma in genomic medicine. Health Aff. (Millwood) 27, 1600–1611 (2008).
Chambers, J. D. et al. Examining evidence in U.S. payer coverage policies for multigene panels and sequencing tests. Int. J. Technol. Assess. Health Care 33, 534–540 (2017).
Douglas, M. P., Parker, S. L., Trosman, J. R., Slavotinek, A. M. & Phillips, K. A. Commercial payer coverage policies for exome sequencing (ES) in pediatric patients: trends over time and analysis of evidence cited. Genet. Med. 21, 152–160 (2019).
Trosman, J. R. et al. Perspectives of US commercial payers on insurance coverage for pediatric and prenatal exome sequencing: results of a study from the program in prenatal and pediatric genomic sequencing (P3EGS). Genet. Med. 22, 283–291 (2020).
ACMG Board of Directors. Clinical utility of genetic and genomic services: a position statement of the american college of medical genetics and genomics. Genet. Med. 17, 505–507 (2015).
Burke, W., Laberge, A. M. & Press, N. Debating clinical utility. Public Health Genomics 13, 215–223 (2010).
Manning, M. & Hudgins, L., Professional Practice and Guidelines Committee. Array-based technology and recommendations for utilization in medical genetics practice for detection of chromosomal abnormalities. Genet. Med. 12, 742–745 (2010).
Schaefer, G. B. & Mendelsohn, N. J., Professional Practice and Guidelines Committee. Clinical genetics evaluation in identifying the etiology of autism spectrum disorders: 2013 guideline revisions. Genet. Med. 15, 399–407 (2013).
Malinowski, J. et al. Systematic evidence-based review: outcomes from exome and genome sequencing for pediatric patients with congenital anomalies or intellectual disability. Genet. Med. 22, 986–1004 (2020).
National Human Genome Research Institute. Genetic timeline, 2020. https://www.genome.gov/Pages/Education/GeneticTimeline.pdf (2020).
Smith, H. S. et al. Clinical application of genome and exome sequencing as a diagnostic tool for pediatric patients: a scoping review of the literature. Genet. Med. 21, 3–16 (2018).
Smith, H. S. et al. Exome sequencing compared with standard genetic tests for critically ill infants with suspected genetic conditions. Genet. Med. 22, 1303–1310 (2020).
Miller, D. T. et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am. J. Hum. Genet. 86, 749–764 (2010).
Borch, L. A., Parboosingh, J., Thomas, M. A. & Veale, P. Re-evaluating the first-tier status of fragile X testing in neurodevelopmental disorders. Genet. Med. 22, 1036–1039 (2020).
Weinstein, V., Tanpaiboon, P., Chapman, K. A., Ah Mew, N. & Hofherr, S. Do the data really support ordering fragile X testing as a first-tier test without clinical features? Genet. Med. 19, 1317–1322 (2017).
Kiely, B., Vettam, S. & Adesman, A. Utilization of genetic testing among children with developmental disabilities in the united states. Appl. Clin. Genet. 9, 93–100 (2016).
Kutscher, E. J., Joshi, S. M., Patel, A. D., Hafeez, B. & Grinspan, Z. M. Barriers to genetic testing for pediatric medicaid beneficiaries with epilepsy. Pediatr. Neurol. 73, 28–35 (2017).
Texas Children’s Hospital. Genetics, 2020. https://www.texaschildrens.org/departments/genetics (2020).
Acknowledgements
We thank all individuals and clinical staff who assisted with the PAR process during the study period. No funding was received or utilized.
Author information
Authors and Affiliations
Contributions
Conceptualization: H.S.S., H.S. Data curation: R.F., A.M.L., A.G., R.O.L, K.N., J.R. H.S. Formal analysis: H.S.S., H.S. Investigation: R.F., A.M.L., A.G., R.O.L, K.N., J.R. H.S. Methodology: H.S.S., H.S. Project administration: H.S. Supervision: H.S. Visualization: H.S.S. Writing—original draft: H.S.S., H.S. Writing—review & editing: H.S.S., R.F., A.M.L., A.G., R.O.L, K.N., J.R., H.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics Declaration
This study was approved by the Baylor College of Medicine and CHRISTUS Health Institutional Review Boards. Informed consent was not required for this retrospective electronic medical record review study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smith, H.S., Franciskovich, R., Lewis, A.M. et al. Outcomes of prior authorization requests for genetic testing in outpatient pediatric genetics clinics. Genet Med 23, 950–955 (2021). https://doi.org/10.1038/s41436-020-01081-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-01081-x
This article is cited by
-
Exploring genetic testing requests, genetic alterations and clinical associations in a cohort of children with autism spectrum disorder
European Child & Adolescent Psychiatry (2024)
-
Physicians’ use and perceptions of genetic testing for rare diseases in China: a nationwide cross-sectional study
Orphanet Journal of Rare Diseases (2023)
-
Rare diseases, common barriers: disparities in pediatric clinical genetics outcomes
Pediatric Research (2023)
-
The diagnostic trajectory of infants and children with clinical features of genetic disease
npj Genomic Medicine (2021)