Abstract
Survivors of natural disasters are at a high risk of cardiovascular disease. Behavioral risk factors, including modifiable diet, need to be identified. Thus far, the association between dairy intake and new-onset hypertension among these survivors is unknown. Therefore, we investigated this relationship. We conducted a longitudinal cohort study of 4475 survivors of the Great East Japan Earthquake in 2011 who participated in a 7-year follow-up survey. New-onset hypertension was assessed using annual health checkup data. Information on the frequency of dairy intake was obtained using a self-report questionnaire. The hazard ratio for developing hypertension according to the frequency of dairy intake was calculated using Cox proportional hazards regression models. The total number of person-years observed was 20,042, with a median follow-up of 5.4 years. During the observation period, 1554 individuals developed hypertension. The multivariable-adjusted hazard ratios of new-onset hypertension were significantly lower in those who consumed dairy products once per day (0.82, 95% confidence interval 0.71–0.94) and twice or more times per day (0.84, 95% confidence interval 0.71–0.99) than in nonconsumers; the inverse linear trend was marginally significant (P = 0.083). This association was not affected by lipid metabolism and was consistent across subgroups by sex, age, behavioral factors, cardiometabolic factors, and housing type due to the disaster. A higher frequency of dairy intake was associated with a lower risk of new-onset hypertension in community-dwelling survivors of earthquakes and tsunamis. Dietary guidance involving dairy intake could reduce the risk of developing hypertension among these survivors.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is a leading cause of death worldwide [1]. Reports from countries that have experienced disasters, such as Japan, the United States, and Italy, indicate that the risk of CVD among disaster survivors is increased by various vicious cycles induced after natural disasters, such as excessive stress, limited access to medical care, and lack of a healthy diet [2]. The short-term impact is quite large in the first few months after a disaster, and the larger the scale of the disaster is, the longer the duration of the health risk [2]. For instance, the Great East Japan Earthquake (GEJE) that occurred in northeast Japan in March 2011 was a disaster of considerable magnitude [3]. Studies have shown that the risk of developing CVD during the first 3 years after the disaster was still higher among the residents of severely flooded areas than among those in nonflooded areas [4, 5].
Hypertension is a major risk factor for CVD. After the GEJE, cardiometabolic factors such as hypertension and diabetes were worse in people who lived in areas that were severely damaged by the disaster [6, 7]. Therefore, we need to identify behavioral risk factors, including modifiable diets, that are aimed at reducing cardiovascular and hypertension risks among natural disaster survivors at a high risk of health problems.
Two meta-analyses of prospective cohorts have reported an inverse association between dairy intake and the development of hypertension [8, 9]; however, most of the reports are from Western countries. As dairy products are not a part of the traditional Japanese diet, dairy intake in the Japanese population is much lower than that in Western populations [10, 11]. A cross-sectional study of the general population [12] and one longitudinal study of male workers [13] reported inverse associations between dairy intake and hypertension risk in the Japanese population. However, there have been no reports examining the association between dairy products and the risk of new-onset hypertension among survivors of massive natural disasters.
This study aimed to investigate the association between dairy intake and new-onset hypertension in natural disaster survivors during the first 7 years after the GEJE.
Methods
Study participants
The Research Project for Prospective Investigation of Health Problems Among Survivors of the 2011 Great East Japan Earthquake and Tsunami (RIAS) study is a population-based longitudinal cohort study that started in 2011. Participants were residents aged 18 years or older living on the southeastern coast of Iwate Prefecture, a region that was heavily damaged by the tsunami. Details of the RIAS study have been reported elsewhere [14,15,16].
In brief, a total of 10,560 community-dwelling residents participated in health checkup examinations for GEJE survivors in Rikuzentakata city, Yamada town, and Otsuchi town. A total of 10,203 people provided written informed consent for participation in the study (acceptance rate: 96.6%). The study protocol was approved by the Institutional Review Board of Iwate Medical University (approval reference number: H23–69), the Institutional Review Board of the National Institute of Health and Nutrition, and the National Institutes of Biomedical Innovation, Health and Nutrition (approval reference number: KENEI99).
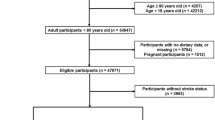
A total of 5317 participants were followed up after excluding those who were pregnant (n = 12) at baseline; missing information regarding recorded blood pressure (n = 133), frequency of dairy intake (n = 92), and other covariates (n = 396) at baseline; those with hypertension (n = 4247) at baseline; and those undergoing dialysis or who had chronic renal failure (n = 6) at baseline. Thus, we included 4475 participants (mean age, 57.2 years; female, 65.5%) in the analysis, excluding those who were lost to follow-up (n = 821) and those who were pregnant during the follow-up period (n = 21) (Fig. 1).
Health checkup examination and follow-up
The annual health checkup examination for the participants of the RIAS study was conducted from baseline (September 2011–March 2012) to December 2018. Body weight (kg) was measured using a digital scale (AD-6400, A&D Co., Tokyo, Japan; BWB-200, Tanita Co., Tokyo, Japan) with an accuracy of ±0.1 kg, with participants wearing light clothing and no shoes. Height was measured using a digital scale (AD-6121A, A&D Co.; YG200D, Yagami Inc., Nagoya, Japan). Body mass index was calculated by dividing the body weight (kg) by height (m2). Blood pressure was measured twice consecutively after the participant sat quietly for 5 min using an automated digital device (BP-103i II, Omron Colin Co., Tokyo, Japan) by a well-trained research staff member, and the average of the two measurements was used according to the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019) [17].
Blood samples were drawn from the antecubital vein while the participants were seated. The samples were transported to the laboratory (Iwate Health Service Association), and measurements were performed on the same day. Serum total cholesterol levels were determined using an enzymatic assay, and serum low-density lipoprotein cholesterol levels were measured using the direct method. The quality of the total cholesterol measurements was controlled by the program of the Centers for Disease Control and Prevention in the USA. Serum creatinine was measured using the enzymatic method. The estimated glomerular filtration rate (eGFR) was calculated by using serum creatinine with an equation based on the Modification of Diet in Renal Disease Study, according to the 2018 clinical practice guidelines by the Japanese Society of Nephrology (JSN) [18]. Proteinuria was assessed using a dipstick.
The outcome was new-onset hypertension at the time of annual health checkups from April 2012 to December 2018. Hypertension was defined as a systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg or as an individual undergoing treatment for high blood pressure. If the incidence occurred more than once during follow-up, only the first outcome was used for the analysis. The incidence date was defined as the midpoint between the examination date before hypertension onset and the examination date when the participant was first noted to have hypertension. The observation period was from the baseline to the date of incidence for participants who developed hypertension and to the date of the final check-up for others.
Self-report questionnaire
The participants were asked about the frequency of intake of dairy products (milk, yogurt, and cheese) during the previous several days using a self-report questionnaire at annual health checkups [19]. The response categories were none, once a day, twice a day, three times a day, and four times or more per day. We converted the five categories into three groups (none, once, and twice or more per day) [16]. Similarly, we obtained information on the frequency of intake of vegetables and fruits at baseline and categorized the intake as below or above the median.
We also used a questionnaire to obtain information on behavioral characteristics, history of diabetes and dyslipidemia, treatment for hypertension, current housing type, and economic status at annual health checkups. Smoking and drinking status were self-reported as never, former, or current. Current drinking status was categorized by the volume of alcohol consumed: light drinking, <20 g pure ethanol/day among females or <40 g ethanol/day among males; and moderate-to-heavy drinking, ≥20 g ethanol/day among females or ≥40 g ethanol/day among males [16]. Physical activity was classified as activity levels of <23 metabolic equivalents of task-h/week and ≥23 metabolic equivalents of task-h/week [20]. We categorized the current housing types as follows: temporary housing, prefabricated temporary housing, and emergency shelter; nontemporary housing (the same house as that before the disaster, the houses of families, friends or relatives, new houses built after the disaster or rental apartments); and others. Economic status was assessed by asking the question “How do you feel about your current economic situation?” Participants were asked to choose one of four answers (very severe, severe, slightly severe, or normal). The response was categorized into poor economic status (very severe, severe, or slightly severe) and normal.
Statistical analyses
The distributions of characteristics according to the frequency of dairy intake among the study participants are presented as the means and standard deviations for continuous variables and as percentages for categorical variables. The differences in characteristics according to the frequency of dairy intake were assessed using trend analysis or the chi-squared test. The differences in characteristics of the follow-up study participants were assessed by Student’s t tests.
Multivariable-adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) for the incidence of new-onset hypertension by the frequency of dairy intake were calculated using Cox proportional hazards regression models while controlling for the effects of established confounders of hypertension. Model 1 was adjusted for age and sex. Model 2 was adjusted for Model 1 plus the frequency of intake of vegetables and fruits per day. Model 3 was adjusted for Model 2 plus body mass index, systolic blood pressure, history of diabetes and dyslipidemia, behavioral characteristics (drinking and smoking status and regular exercise), economic status, residential area, and current housing. Baseline values were used for all the covariates and the frequency of dairy intake. Dairy products contain saturated fatty acids, which are associated with elevated serum cholesterol levels. We further adjusted for serum lipid levels to determine the effects of lipid metabolism on the association between the frequency of dairy intake and the incidence of new-onset hypertension. Finally, we assessed the associations between the frequency of dairy intake and the incidence of new-onset hypertension across subgroups stratified by sex, age, behavioral factors, blood pressure levels, obesity, history of cardiometabolic risk factors, and housing type due to the disaster using a fully adjusted model. We further tested the multiplicative interactions among these groups. In the sensitivity analysis, we performed the corresponding analysis, excluding those who developed hypertension in the year following the baseline survey, limiting the analysis to only those aged 30 years or older or those who had undergone at least two health checkups.
All statistical analyses were performed using SAS version 9.4 for Windows (SAS Institute Inc., Cary, NC). Analysis items with a two-tailed P value of <0.05 were considered statistically significant.
Results
Table 1 shows the baseline characteristics of the study participants according to the frequency of dairy intake. Participants with a higher frequency of dairy intake were older and predominantly female, with fewer current drinkers and smokers, without exercise habits and without poorer economic status, with a higher intake of fruits and vegetables, and with a history of diabetes and dyslipidemia. As the frequency of dairy intake increased, total cholesterol increased. As the frequency of dairy intake increased, the number of health checkups also increased. In contrast, there was no association between the frequency of dairy intake and body mass index or systolic/diastolic blood pressure. There were also no associations related to housing type due to the disaster, such as temporary housing, at the time of the survey.
The participants who were lost to follow-up were younger, predominantly male, smokers, more likely to be in a difficult economic status, and consumed fruits and vegetables less frequently than the analyzed participants. In contrast, they were less likely to have a history of diabetes or dyslipidemia, and their blood pressure and serum lipid levels were lower (Supplementary Table 1).
The observed total person-years was 20,042, and the median follow-up period was 5.4 years. During the follow-up period, 1554 participants developed hypertension. Table 2 shows multivariate-adjusted HRs and 95% CIs according to the frequency of dairy intake. The HRs of new-onset hypertension were similar in Model 1, adjusted for sex and age; Model 2, which added the frequency of vegetable and fruit intake to Model 1; and Model 3, which added established confounders of hypertension and other related factors. The HRs of new-onset hypertension during the 7-year follow-up were significantly lower in the once per day group (HR 0.82 [95% CI 0.71–0.94]) and the twice or more per day dairy intake group (HR 0.84 [95% CI 0.71–0.99]) than in nonconsumers in Model 3; the inverse linear trend was marginally significant in Model 3 (P = 0.083). Moreover, we performed an analysis that considered serum lipid levels to confirm the effects of lipid metabolism. The associations were similar to those observed in the analysis of the development of hypertension described above (Supplementary Table 2). Furthermore, further adjustment of Model 3 for eGFR and/or proteinuria did not change the inverse association (data not shown).
In addition, subgroup analyses showed that the associations between the frequency of dairy intake and the development of hypertension were not significantly different among the subgroups based on sex, age (<65 vs. ≥65 years), the absence of behavioral factors (alcohol drinking, smoking, regular exercise, and high frequency of vegetables and fruits), blood pressure level, obesity (body mass index <25 kg/m2 vs. ≥25 kg/m2), history of diabetes or dyslipidemia, poor economic status, and housing type due to the disaster (all P for interaction > 0.05) (Table 3). Notably, there was no difference in the association between dairy intake and new-onset hypertension, depending on whether the participants were living in temporary housing at baseline or follow-up.
The inverse association between frequency of dairy intake and development of hypertension remained unchanged, and its inverse linear trend was statistically significant even after excluding those who developed new hypertension in the year following the baseline survey as a sensitivity analysis (n = 3999) (Supplementary Table 3). Furthermore, the results did not differ when only those who had undergone two or more health checkups or those aged 30 years or older were included in the analysis (data not shown).
Discussion
This community-based longitudinal study found that the frequency of dairy intake was inversely associated with new onset of hypertension among natural disaster survivors during the first 7 years after the GEJE. This association was unaffected by lipid metabolism in the presence of saturated fatty acids in dairy products. This significant inverse association was still present after excluding those with new-onset hypertension in the year following baseline, those younger than 30 years of age, or those with only one health checkup. Furthermore, the associations among subgroups by sex, age, behavioral factors, blood pressure level, obesity, history of cardiometabolic disease, economic status, and housing type due to the disaster were consistent. To the best of our knowledge, this is the first study to evaluate the association between dairy intake and the development of hypertension in survivors of natural disasters. The present analysis does not include individuals with disaster hypertension, which is a sudden and persistent rise in blood pressure after a disaster [21].
Meta-analyses of prospective cohort studies [8, 9] and large cohort studies [22, 23] in Western countries have reported an inverse association between dairy intake and the development of hypertension. A similar association has also been reported in a study on male workers in Japan [13]. The associations between dairy intake and the development of hypertension in the present study were consistent with those of previous studies conducted in Western countries and in Japan. This association was robust when examined by various strata and was maintained even when new cases of hypertension in the year following the baseline survey were excluded, limiting the analysis to those aged 30 years or older and those who had undergone at least two health checkups. In contrast, in a previous cross-sectional study of baseline survey participants in the present cohort [16], the inverse association between dairy intake and prevalence of hypertension was stronger in temporary housing residents than in the rest. However, in the present longitudinal study, the association between the frequency of dairy intake and new onset of hypertension did not differ by housing type. The effect of living in temporary housing on blood pressure may have almost disappeared throughout the long-term follow-up.
The participants who could not be followed were predominantly male and younger than those analyzed and had physical and behavioral characteristics appropriate to their sex and age. In other words, they smoked more and ate less healthy diets than the analysis participants, but their cardiometabolic factors, such as blood pressure, were better than those of the analysis participants. Whether or not they lived in temporary housing was not related to their follow-up status. Thus, in the RIAS study, CVD, hypertension, and disasters may not have been the reasons why participants lost to follow-up did not undergo subsequent health checkups.
The protective mechanism of the risk of new-onset hypertension with dairy intake may be due to the combined effects of potassium [24], lactotripeptides [25], and other substances in dairy products as antihypertensive components. Low-fat dairy products are also a component of the Dietary Approach to Stop Hypertension (DASH) dietary pattern developed to prevent hypertension [26]. In contrast, dairy products contain saturated fatty acids, which are associated with elevated serum cholesterol but had no effect on the association between dairy products and the new onset of hypertension observed in this study.
There are several limitations to the present study. First, information on the amount of dairy intake, types of dairy products, and fat content was not obtained; as such, only the frequency of dairy intake was analyzed. Second, the RIAS study did not have available information on salt (sodium) intake and excretion. Therefore, we could not use it as a covariate in the present analysis. Sodium works to raise blood pressure, while potassium, which is abundant in dairy products, works to lower blood pressure. Hence, the lack of adjustment for salt intake might have weakened or strengthened our findings. Incidentally, Japanese individuals [10] consume over 90% of their dairy products from milk and fermented dairy products, which do not contain salt. Third, misclassification of information on the incidence of hypertension may have been erroneous because some individuals had intermittent health checkups. Fourth, we did not have information on lactase gene polymorphisms. However, most Japanese populations are likely to have lactase nonpersistence phenotypes [27]. Moreover, it has been reported that in a multiethnic U.S. cohort including Asian Americans, dairy intake is estimated by ethnic background rather than gene polymorphism [28]. Fifth, the frequency of dairy intake was obtained from a baseline survey conducted 6 months after the GEJE. Since some participants lived in temporary housing, this may not indicate habitual frequency of intake. Sixth, there may still be unadjusted confounding factors, such as educational attainment and salt intake. Nonetheless, we have comprehensively controlled for various well-established dietary, behavioral, and cardiometabolic factors for hypertension in this study. Finally, as the present study participants were survivors of massive earthquakes and tsunamis only in specific regions of Japan, our results cannot be generalized to other populations. However, the results may be applicable to survivors of disasters with a similar racial genetic background.
It should be noted that individuals with impaired renal function and limited protein, potassium, and phosphorus intake should follow their physician’s instructions regarding the appropriate quantity of dairy products to consume because dairy products are high in these nutrients.
In conclusion, a higher frequency of dairy intake was associated with a lower incidence of new-onset hypertension in community-dwelling survivors affected by the earthquake and tsunami at 7 years of follow-up after the disaster. The fact that dairy intake was effective in reducing the new onset of hypertension in survivors at increased risk for CVD and hypertension due to damage from a large-scale disaster could provide a modifiable, simple, and effective therapy for reducing the risk of hypertension.
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982–3021.
Babaie J, Pashaei Asl Y, Naghipour B, Faridaalaee G. Cardiovascular Diseases in Natural Disasters; a Systematic Review. Arch. Acad Emerg Med. 2021;9:e36.
Iwate Prefecture. IWATE Moving toward Reconstruction. 2014. https://www.pref.iwate.jp/_res/projects/default_project/_page_/001/002/302/iwatefukkounoayumi.pdf. Accessed 2021.
Nakamura M, Tanaka F, Komi R, Tanaka K, Onodera M, Kawakami M, et al. Sustained Increase in the Incidence of Acute Decompensated Heart Failure After the 2011 Japan Earthquake and Tsunami. Am J Cardiol. 2016;118:1374–9.
Nakamura M, Tanaka K, Tanaka F, Matsuura Y, Komi R, Niiyama M, et al. Long-Term Effects of the 2011 Japan Earthquake and Tsunami on Incidence of Fatal and Nonfatal Myocardial Infarction. Am J Cardiol. 2017;120:352–8.
Ohira T, Hosoya M, Yasumura S, Satoh H, Suzuki H, Sakai A, et al. Evacuation and Risk of Hypertension After the Great East Japan Earthquake: The Fukushima Health Management Survey. Hypertension. 2016;68:558–64.
Takahashi S, Nakamura M, Yonekura Y, Tanno K, Sakata K, Ogawa A, et al. Association between relocation and changes in cardiometabolic risk factors: a longitudinal study in tsunami survivors of the 2011 Great East Japan Earthquake. BMJ Open. 2016;6:e011291.
Ralston RA, Lee JH, Truby H, Palermo CE, Walker KZ. A systematic review and meta-analysis of elevated blood pressure and consumption of dairy foods. J Hum Hypertens. 2012;26:3–13.
Soedamah-Muthu SS, Verberne LD, Ding EL, Engberink MF, Geleijnse JM. Dairy consumption and incidence of hypertension: a dose-response meta-analysis of prospective cohort studies. Hypertension. 2012;60:1131–7.
Ministry of Health, Labour and Welfare. The National Health and Nutrition Survey. https://www.mhlw.go.jp/bunya/kenkou/kenkou_eiyou_chousa.html. Accessed 2021.
Beydoun MA, Gary TL, Caballero BH, Lawrence RS, Cheskin LJ, Wang Y. Ethnic differences in dairy and related nutrient consumption among US adults and their association with obesity, central obesity, and the metabolic syndrome. Am J Clin Nutr. 2008;87:1914–25.
Takashima Y, Iwase Y, Yoshida M, Kokaze A, Takagi Y, Taubono Y, et al. Relationship of food intake and dietary patterns with blood pressure levels among middle-aged Japanese men. J Epidemiol. 1998;8:106–15.
Umesawa M, Kitamura A, Kiyama M, Okada T, Shimizu Y, Imano H, et al. Association between dietary behavior and risk of hypertension among Japanese male workers. Hypertens Res. 2013;36:374–80.
Nishi N, Yoshimura E, Ishikawa-Takata K, Tsuboyama-Kasaoka N, Kubota T, Miyachi M, et al. Relationship of living conditions with dietary patterns among survivors of the great East Japan earthquake. J Epidemiol. 2013;23:376–81.
Takahashi T, Tanaka F, Shimoda H, Tanno K, Sakata K, Takahashi S, et al. Five-year blood pressure trajectories of survivors of the tsunami following the Great East Japan Earthquake in Iwate. Hypertens Res. 2021;44:581–90.
Miyagawa N, Tsuboyama-Kasaoka N, Nishi N, Tsubota-Utsugi M, Shimoda H, Sakata K, et al. Association between the prevalence of hypertension and dairy consumption by housing type among survivors of the Great East Japan Earthquake. J Hum Hypertens. 2022;36:299–307.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
The Japanese Society of Nephrology. Evidence-based Clinical Practice Guideline for CKD 2018. Tokyo Igakusha: Tokyo, 2018. [in Japanese]
Yoshimura E, Ishikawa-Takata K, Hasegawa Y, Murakami H, Nozue M, Sarukura Y, et al. [The food intakes in the survivor of the Great East Japan Earthquake living in temporary houses in Kamaishi city]. Iwate Koshu Eisei Zasshi. 2014;25:7–14. [in Japanese]
Murakami H, Yoshimura E, Ishikawa-Takata K, Hasegawa Y, Kubota T, Tsuboyama-Kasaoka N, et al. [Validity and reproducibility of a physical activity questionnaire used for health surveying among victims of the Great East Japan Earthquake]. Nihon Koshu Eisei Zasshi. 2013;60:222–30. [in Japanese]
Kario K. Disaster hypertension - its characteristics, mechanism, and management. Circ J. 2012;76:553–62.
Livingstone KM, Lovegrove JA, Cockcroft JR, Elwood PC, Pickering JE, Givens DI. Does dairy food intake predict arterial stiffness and blood pressure in men?: Evidence from the Caerphilly Prospective Study. Hypertension. 2013;61:42–7.
Wang H, Fox CS, Troy LM, McKeown NM, Jacques PF. Longitudinal association of dairy consumption with the changes in blood pressure and the risk of incident hypertension: the Framingham Heart Study. Br J Nutr. 2015;114:1887–99.
WHO Guideline: sodium intake for adults and children. 2012. https://apps.who.int/iris/bitstream/handle/10665/77985/9789241504836_eng.pdf?sequence=1&isAllowed=y. Accessed 2021.
Ricci I, Artacho R, Olalla M. Milk protein peptides with angiotensin I-converting enzyme inhibitory (ACEI) activity. Crit Rev Food Sci Nutr. 2010;50:390–402.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24.
Kato K, Ishida S, Tanaka M, Mitsuyama E, Xiao JZ, Odamaki T. Association between functional lactase variants and a high abundance of Bifidobacterium in the gut of healthy Japanese people. PLoS ONE. 2018;13:e0206189.
Chin EL, Huang L, Bouzid YY, Kirschke CP, Durbin-Johnson B, Baldiviez LM, et al. Association of Lactase Persistence Genotypes (rs4988235) and Ethnicity with Dairy Intake in a Healthy U.S. Population. Nutrients. 2019;11:1860.
Funding
This study was supported by grants from the Ministry of Health, Labor and Welfare, Health and Labor Sciences Research Grants, Japan (H23-Tokubetsu-Shitei-002; H24-Kenki-Shitei-001, H25-Kenki-Shitei-001(Fukkou)), JSPS KAKENHI (18K10108), the Dairy Products Health Science Council and the Japan Dairy Association. None of the study sponsors had any role in the study design, conduct of the study, data collection, data interpretation, or preparation of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Miyagawa, N., Tsubota-Utsugi, M., Tsuboyama-Kasaoka, N. et al. Seven-year incidence of new-onset hypertension by frequency of dairy intake among survivors of the Great East Japan Earthquake. Hypertens Res 45, 1459–1467 (2022). https://doi.org/10.1038/s41440-022-00933-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-00933-0
Keywords
This article is cited by
-
Dairy intake and the risk of incidental hypertension
Hypertension Research (2022)