Abstract
Structural and functional elements of biological systems are highly conserved across vertebrates. Many neurological and psychiatric conditions affect both humans and animals. A cross-species approach to the study of brain and behaviour can advance our understanding of human disorders via the identification of unrecognized natural models of spontaneous disorders, thus revealing novel factors that increase vulnerability or resilience, and via the assessment of potential therapies. Moreover, diagnostic and therapeutic advances in human neurology and psychiatry can often be adapted for veterinary patients. However, clinical and research collaborations between physicians and veterinarians remain limited, leaving this wealth of comparative information largely untapped. Here, we review pain, cognitive decline syndromes, epilepsy, anxiety and compulsions, autoimmune and infectious encephalitides and mismatch disorders across a range of animal species, looking for novel insights with translational potential. This comparative perspective can help generate novel hypotheses, expand and improve clinical trials and identify natural animal models of disease resistance and vulnerability.
Similar content being viewed by others
Introduction
Many of the same neurological and psychiatric conditions affect humans and animals, yet clinical and research collaborations between physicians and veterinarians remain infrequent. Rarely, spontaneous animal disorders inform human medicine; for example, scrapie in sheep informs our understanding of kuru and Creutzfeldt–Jakob disease in humans, and photosensitive generalized seizures in baboons inform our understanding of the same seizures in humans. This lack of collaboration reflects our inability to systematically survey animal diseases in natural habitats, to identify clinical and pathological signs (for example, sensory loss or hallucinations) in animals and to recognize spontaneous disorders in animals. For example, the chief doctor of veterinary medicine (DVM) at the Bronx Zoo contacted the Centers for Disease Control (CDC) to report that flamingos, owls and other species were dying from a viral encephalitis that resembled one affecting humans nearby. The CDC dismissed the DVM’s opinion that West Nile virus might be the causative agent both in the avian species and in humans. However, the CDC scientists were wrong1.
Human exceptionalism remains a dominant but faulty framework in evolutionary biology and medicine. This concept is most vigorously entrenched with regard to brain and behaviour, whereby humans are considered the most ‘highly evolved’ species despite our inability to accurately assess the intelligence of other animals, including those with much larger brains than ours, such as whales and elephants. Structural and functional elements of neuroendocrine, muscular and neural systems are highly conserved across vertebrates, yet most physicians remain unaware that mammals and birds exhibit features of many ‘human-like’ neuropsychiatric disturbances.
Consequently, this source of comparative information remains largely untapped, and most models of spontaneously occurring disorders in animals go unrecognized and underutilized by physicians. A cross-species approach can advance our understanding of neurological and psychiatric disorders by looking beyond human-centred perspectives. Furthermore, clinical advances in human neurology and psychiatric disorders can be adapted for veterinary patients. Here, we review pain, cognitive decline syndromes, epilepsy, anxiety and compulsions, autoimmune and infectious encephalitides and mismatch disorders across a range of animal species and look for novel insights with translational potential.
Pain
The International Association for the Study of Pain defines pain as an unpleasant sensory and emotional experience associated with actual or potential tissue damage (or described in terms of such damage)2. Pain compels a person or animal to do, or not do, something to protect the part of the body that hurts3,4. Nociception, on the other hand, is defined as the neural process of encoding mechanical, thermal and chemical noxious stimuli (that is, stimuli that damage or threaten the body) from nociceptors5. Nociception can occur in the absence of pain (for example, in an injured warrior in imminent danger), and pain can occur without activation of nociceptors (for example, in the case of phantom limb pain)5.
Although most humans can communicate pain linguistically to doctors, animals and some human populations, including pre-verbal children and nonverbal individuals with intellectual disabilities, must do so non-linguistically. Vocalization, physiological responses and behaviour are some important ways by which humans and animals express pain6,7. Pain scales for pre-verbal or nonverbal humans (such as the Behavioural Indicators of Infant Pain8 and the Pain Assessment in Advanced Dementia scale9) and for veterinary patients (such as the Short Form Glasgow Composite Measure Pain Scale for dogs10 and the Post Abdominal Surgery Pain Assessment Scale for horses11) share a number of features, such as evaluation of vocalization and/or facial expression. These scales have dramatically improved the ability to identify and grade the severity of pain in these patient populations. However, scales are lacking for some domestic animal species and all wild animal species. Our inability to understand animal communication and our biases against animal consciousness have led to a longstanding and pervasive belief that animals do not experience pain. For centuries, veterinary surgeries were performed without analgesia; the first textbook of veterinary anaesthesia was published in 1941 (ref.12).
The mechanisms of pain are highly conserved, especially across mammalian species. Differentiation between pain mechanisms is important because different pain mechanisms require different approaches to pain management. Nociceptive pain (including inflammatory pain) is generated by activation of peripheral nociceptors and is most commonly associated with acute tissue damage5. Neuropathic pain is caused by a lesion or disease of the somatosensory system and does not require activation of nociceptors (for example, in thalamic stroke, phantom limb pain and peripheral nerve damage from diabetes mellitus)2. Nociplastic, algopathic and nocipathic pain are not associated with activation of nociceptors or with disease of the nervous system; central sensitization can be the underlying mechanism of this pain (such as in fibromyalgia)13. Acute pain (<6 weeks duration), subacute pain (6–12 weeks) and chronic pain (>12 weeks) refer only to pain duration and can be driven by one or more pain mechanisms14.
Mechanisms of pain are conserved across species; therefore, it is not surprising that a number of non-human mammals and even non-mammalian species, such as birds, share painful conditions with humans. As a result, many pain syndromes are treated similarly in human and veterinary medicine, whether acute or chronic, inflammatory or neuropathic. Common causes of pain shared by humans and animals include degenerative diseases (such as osteoarthritis, degenerative disk disease and lumbosacral stenosis), visceral pain (such as inflammatory bowel disease and cystitis) and cancer-related pain. Management of acute pain (such as postoperative pain or trauma) in human and veterinary patients uses many of the same drugs and techniques, including nonsteroidal anti-inflammatory drugs, opioids and locoregional anaesthesia. In addition, drugs such as antiepileptics and antidepressants that are used to treat neuropathic pain in humans are also used to treat neuropathic pain such as post-amputation pain, radiculopathy and nerve sheath neoplasm in many domestic animal species15. Interventional techniques are commonly used to treat chronic pain in humans, and some of these techniques, such as intra-articular and epidural corticosteroid injection, are already used to treat chronic pain in animals, although evidence to support the effectiveness of these practices is sorely needed. Advanced interventional techniques such as peripheral nerve and spinal cord stimulation, radiofrequency ablation and cryoneurolysis, pulsed-dose radiofrequency and implantable intrathecal pumps are being explored in veterinary medicine. Whereas acute pain is usually nociceptive and/or inflammatory and thus responds to anti-inflammatory agents, chronic pain is less likely than acute pain to be associated with a primary nociceptive input and is more likely to be modulated by centrally acting mechanisms. Chronic pain affects ~50 million people in the United States and ~1.5 billion people worldwide, and morbidity and mortality are rising. By contrast, exactly how many animals are afflicted with chronic pain is unknown. In humans, chronic pain is often influenced by psychosocial factors, sleep disturbance, fear of pain and re-injury and avoidance behaviour. Because psychosocial influencers are strong determinants of chronic pain, nonverbal expressions of pain and suffering can be more direct and informative than verbal. Humans with chronic pain can verbally report severe pain without visible signs or affective expression of discomfort16,17,18. For some of these patients, their nonverbal displays may more accurately reflect their pain status; additional research is needed in this area. Such psychosocial influencers respond better to interdisciplinary pain management19. Physicians and veterinarians desperately need evidence-informed interventions that are effective and safe and that address the complex central mechanisms of chronic pain.
The utility of animal models of spontaneous pain is limited by the long time required to develop them and the variability of the pain phenotypes presented20; the advantages of genetically modified mouse strains are from low genetic variability and low cost. Mouse dorsal root ganglion neurons were used to identify transient receptor potential cation channel subfamily V member 1 (TRPV1) as the capsaicin receptor that mediates thermal sensing in animals21. This finding led to a greater understanding of human pain22: activation of TRPV1 simulates pain via central sensitization, causing hyperalgesia and allodynia, features of chronic pain23. However, mouse models primarily focus on acute pain, and their applicability to chronic pain is uncertain24; by contrast, spontaneous models and scales might be even more relevant to chronic pain18.
In summary, alignment of pain assessment, management, outcome measures and pain mechanisms across species would improve data translation and would help to identify pain biomarkers and natural animal models of pain.
Cognitive decline syndromes
Age is the greatest risk factor for cognitive decline in humans and in many animals. By age 50 years, most people experience features of age-related memory decline (such as forgetting names and misplacing keys or eyeglasses) that do not interfere with daily function25,26. Symptom progression produces mild cognitive impairment (MCI). Many patients with MCI who have memory issues (that is, amnestic MCI) go on to develop dementia: 10% within a year and 50% in 5 years27. The major cause of human dementia, Alzheimer disease (AD), which affects ~44 million people worldwide and has no effective cure, is characterized by accumulation of amyloid-β (Aβ) into extracellular plaques in the parenchyma and vasculature (congophilic amyloid angiopathy) and abnormally phosphorylated intraneuronal tau accumulations that form neurofibrillary tangles28,29.
Experimental models are essential to understand AD pathogenesis and develop novel therapeutics such as vaccines. The most common induced models of AD are transgenic mice that overexpress human genes with mutations associated with the rare, early-onset familial AD30. Transgenic mice develop Aβ deposits in their brains and manifest some neurological signs of AD. Studies on natural non-transgenic models of spontaneously occurring pathology with cognitive impairment in non-human primates, dogs, cats31 and other species30 (Table 1) provide complementary data to mouse models. Cognitive impairment occurs in one-third of dogs by age 12 years and in two-thirds of dogs by age 16 years32. Signs include disorientation, reduced interactions with people and other dogs, failure of learned house training and disrupted sleep–wake cycle. Cognitive impairment occurs early in castrated male dogs33. Age-associated models of AD in non-human primates and dogs (such as beagles; Fig. 1) parallel the disease course of sporadic AD without a known gene mutation in humans. Phylogenetic proximity to humans makes non-human primates ideal models. However, their use is extremely limited owing to ethical considerations, cost, restricted availability and maintenance requirements. Dogs, with their relatively long lifespan and shared environment with humans, are accessible spontaneous models of cognitive impairment and demonstrate age-dependent AD pathology and clinical features that can be assessed reliably34,35. Furthermore, canine and human amyloid precursor protein are 98% homologous36,37.
Selegiline is the only FDA-approved medication for dogs with cognitive impairment, although medium-chain triglycerides might also improve cognition38. In addition, propentofylline is used widely by veterinarians in Europe39. Novel disease-course-modifying therapies, such as immunomodulation, are being tested in canine and non-human primate models of AD30,40,41,42. Age-associated cognitive decline also occurs in felines and is linked with the presence of Aβ and abnormally phosphorylated tau pathologies37,43,44.
Epilepsy
Organisms from roundworms to humans can have seizures and seizure-like behaviour that result from hypersynchronous neural electrical activity45. The paroxysmal, unpredictable and brief nature of seizures limits recognition of these episodes in wild species. Although rodent models are most often used for experimentally induced seizures, dogs with spontaneous epilepsy are a valuable translational research platform46.
Consensus statements that are influenced by International League Against Epilepsy (ILAE) recommendations have been published on the classification, diagnostic approach and treatment of epilepsy in companion animals47,48,49,50,51. However, challenges in diagnostic testing have resulted in epilepsy being understood only modestly well in dogs and poorly in cats. Epilepsy affects ~0.75% of domestic dogs, with the first seizure commonly occurring in adolescence or early adulthood (6–36 months of age)52,53. Among dogs with epilepsy, ~25% are treatment-resistant and ~60% have one or more episodes of status epilepticus and a shortened lifespan54. In humans, epilepsy affects ~0.9% of the population and ~33% are treatment-resistant55. Genetic mutations can cause human and canine epilepsy56,57,58 with focal or generalized epileptiform discharges and seizures. Traditionally, EEG recording in dogs was performed with patient sedation to minimize artefacts and could be collected only for short periods of time; differences in sedation protocols and short recording periods have limited the utility of this technique. However, wireless video-EEG of an excellent quality can now be obtained in unsedated dogs over several hours59; standardization of this recording method will aid in better identification of seizure foci and in comparison of data from different clinics.
Long-term intracranial EEG recordings (obtained over the course of one to several months) in dogs with spontaneous epilepsy reveal interictal stereotyped bursts that resemble human seizure-onset patterns60,61. Temporal variability in seizures and interictal bursts after electrode implantation reach steady state after several weeks, similar to humans, which adds to the translational relevance of this model62. The interictal bursts in dogs are tenfold more frequent than seizures, which provides insights into the physiological changes that inhibit transformation of interictal into ictal activity63.
The same antiseizure drugs are effective in humans and in animals that have pharmacokinetics similar to that of humans, and most systematic data on drug metabolism and efficacy come from humans and dogs. Maintenance antiseizure drugs for dogs include phenobarbital, potassium bromide, imepitoin, levetiracetam and zonisamide47. Neither surgical resection nor neuromodulation (such as vagus nerve stimulation or an intracranial responsive neurostimulator system) is routinely available for veterinary patients with epilepsy. The cost of implantable systems has largely precluded their use in veterinary patients (with some exeptions64). Furthermore, in the past, an inability to reliably identify a seizure focus with EEG limited the study of surgical methods of correction.
Movement disorders
A diverse range of animal and human movement disorders are primarily defined by the type (for example, hypokinetic versus hyperkinetic) and frequency (for example, continual versus episodic) of abnormal movements. These include dyskinesias, tremors, fasciculations, myoclonus, asterixis, chorea, ballism, athetosis and dystonia.
Psychotropic medication use in humans results in higher incidences of dyskinesias, parkinsonism and akathisia in humans than in animals. Canine dyskinesias are primarily breed-associated disorders65,66,67,68,69 (Table 2) with signs that can be paroxysmal or constant (such as hypertonicity syndrome in Labrador retrievers)66,69. Causes of dyskinesias include degenerative or acquired disorders of the basal nuclei and upper brainstem (such as in Parkinson disease and Sydenham chorea in humans), suspected serotonin deficiencies within the spinal cord (such as in Scottish terrier cramps) and skeletal muscle ion channel abnormalities (such as in myotonia congenita)65,67,68,70,71. Examples of parallels between human and canine patients include orthostatic tremors in Great Danes that resemble primary orthostatic tremor in humans and dyskinesias in Jack Russell terriers and Labradors that mirror non-paroxysmal dyskinesias in humans. Owing to our knowledge of canine genetics and the genetic homogeneity of inbreed strains, the study of domestic dogs can facilitate the identification of gene defects and mechanisms of inherited diseases65. For instance, a deletion in BCAN (encoding brevican core protein, a brain-specific protein involved in cell adhesion, axon guidance and neuronal plasticity) is associated with episodic falling in Cavalier King Charles spaniels. This dysfunction can be alleviated with clonazepam or acetazolamide and shares features with human paroxysmal dyskinesia72,73.
Treatment of dyskinesias in humans and dogs has limited efficacy. In humans, carbamazepine is the drug of choice for kinesigenic dyskinesias and clonazepam for the non-kinesigenic form. Non-kinesigenic dyskinesia is refractory to therapy in humans, whereas clonazepam, acetazolamide and fluoxetine are effective in Border terriers70.
Kinesigenic dyskinesia in dogs is treated with phenobarbital74. Paroxysmal exertion-induced dyskinesia in humans improves on the ketogenic diet, and although the efficacy of this diet has not been studied in dogs, it can improve canine epilepsy75. Border terriers with epileptoid cramping syndrome have an immunological response directed against transglutaminase and gliadin, and clinical signs can improve on a gluten-free diet76,77. This diet can also help some human patients with Parkinson disease78. Studies of canine dyskinesias might help to shed light on the pathophysiological mechanisms underlying human dyskinesias.
Anxiety and compulsions
Among human mental disorders, anxiety disorders have the earliest onset (median 6 years of age) and the highest prevalence (32% of adolescents)79. Human anxiety disorders are characterized by persistent unrealistic fear or worry inappropriate for age, marked distress or avoidance, interference with daily functioning and time-consuming symptoms. Anxiety disorders are common in companion animals (Table 3). For example, an estimated 14–29% of all dogs show signs consistent with separation anxiety80,81. Furthermore, fear and anxiety contribute to most behaviour disorders seen in companion animals. Clinical and behavioural signs of anxiety in animals include hypervigilance, restlessness or pacing, vocalization, yawning, lip-licking, trembling, hypersalivation, panting, urination, defecation, vomiting, diarrhoea, decreased appetite and hiding or escape attempts that can result in self-trauma.
Obsessive–compulsive disorder (OCD) is a human anxiety disorder characterized by obsessions (for example, recurrent and persistent thoughts or urges) and/or compulsions (such as repetitive grooming or ordering) performed in response to an obsession or to rigidly applied rules. The term ‘compulsive disorders’ is more commonly used in veterinary medicine as it cannot be determined whether animals obsess. In animals, compulsive disorders are abnormal behaviours that are repetitive or sustained and are excessive in duration, frequency or intensity82. Although derived from normal behaviour patterns, compulsive behaviours occur out of context and interfere with the animal’s ability to function. Compulsive behaviours typically arise in genetically predisposed individuals exposed to repeated states of conflict, anxiety or frustration (Table 4). Compulsive behaviours in animals share many features with human OCD. Abnormal serotonergic transmission is thought to be involved in the development of compulsive disorders, as demonstrated by the clinical response in humans and animals to drugs that inhibit serotonin reuptake83.
Spontaneous animal models can model specific aspects of the human OCD phenotype. Parallel use of several such models could help to define the underlying mechanisms, assess the effectiveness of deep brain stimulation and screen potential pharmacological therapies82.
Optogenetic approaches in mice revealed that hyperactivation of the orbitofrontal cortex–ventromedial striatum pathway, which has been linked to human OCD, produced abnormal repetitive grooming behaviour84. Behavioural changes developed only after repetitive stimuli over time, which suggests that synaptic plasticity was required. Chronic treatment with high-dose fluoxetine, effective in human OCD, reversed repetitive grooming behaviour and the associated putative plasticity changes83.
In addition to pharmacotherapy, treatment choices for human and animal anxiety disorders include cognitive behavioural therapy85. Behavioural therapy in animals involves the use of reward-based, predictable and consistent interactions, creation of a structured environment and routine, reinforcement of behaviours that are incompatible with the compulsive or anxious behaviour, provision of mental enrichment and minimization of exposure to stimuli that induce conflict, frustration or anxiety.
Encephalitides
Viral and autoimmune encephalitides occur in humans and animals and share pathophysiological, epidemiological and clinical features. Infectious or autoimmune encephalitis is often accompanied by fever (especially in viral forms of encephalitis), seizures and behavioural and cognitive changes such as confusion, agitation, anxiety, depression, psychosis and memory dysfunction. Here, we focus on encephalitogenic viral families and autoimmune encephalitides that exemplify the value of a cross-species approach.
Certain flaviviruses and alphaviruses (Table 5) have a strong CNS tropism and can cause encephalitis and meningitis in humans and animals. Many patients are asymptomatic or develop flu-like features of fever, headache and myalgia, whereas others develop neurological dysfunction including mental status changes, paralysis and convulsions. The incidence of neurological and psychiatric sequelae and mortality depend on the virus and the age of the patient. Viral ecology involves transmission between a reservoir of vertebrate hosts via arthropod vectors that also transmit the virus to other vertebrate species with different disease outcomes. A vertebrate species in which the virus replicates efficiently is termed an ‘amplifying host’. Alternatively, the virus can infect a non-reservoir species in which replication is limited (that is, ‘dead-end hosts’)86.
Flaviviruses
The flexible tropisms of flaviviruses enable them to infect many species and often to cause simultaneous medical and veterinary outbreaks. In other words, these viruses are zoonotic infectious agents. Animals can represent reservoir, amplifying, dead-end or incidental hosts (Table 5); therefore, understanding their contribution to viral ecology is essential87. Animals can be affected by flaviviruses in the same manner as humans, with comparable pathogenic mechanisms and clinical features.
Alphaviruses
The life cycles of alphaviruses are often complex and involve multiple species. For example, the Venezuelan equine encephalitis virus cycles between rodents, bats, opossums and arthropod vectors but can amplify and cause severe encephalitis in horses. This virus occasionally is transmitted to humans and domesticated animals such as dogs that, similar to horses, can develop severe encephalitis. Although alphaviruses were first recognized in horses in the late 1920s, it took 30 years to understand that the same infectious agents underlay horse and human infections86. This fact highlights the need to connect veterinarian and human medical communities to enable early recognition of species-spanning health threats.
Bornaviruses
A consensus now exists that bornavirus infections are neither zoonotic nor associated with human neuropsychiatric disease88. Nevertheless, three cases of fatal human encephalitis were reported following infection with variegated squirrel 1 bornavirus, which raised concern about additional as-yet unknown zoonotic infections that can cause encephalitis89.
Autoimmune encephalitis
Animals and humans can develop autoimmune encephalitis, often as a result of specific autoantibodies that target neuronal surface antigens or synaptic proteins. In human medicine, diagnostic criteria for autoimmune encephalitis are rapidly evolving in line with our increased understanding of the spectrum of clinical features and pathogenic mechanisms. The clinical features of autoimmune encephalitis include psychosis, epileptic seizures, memory impairment and abnormal movements. The high frequency of unexplained encephalitis in animals suggests that autoimmune encephalitis is far more prevalent than currently recognized. The epitopes targeted by autoantibodies are highly conserved across species. The discovery of treatable autoimmune encephalitides in humans should encourage veterinarians to provide early diagnosis and immunotherapy (for example, with corticosteroids) for encephalitis without an infectious cause in animals.
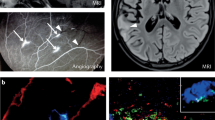
The two most common forms of autoimmune encephalitis target the synaptic proteins N-methyl-d-aspartate receptor (NMDAR; also known as GRIN) and leucine-rich glioma-inactivated protein 1 (LGI1), and affect the hippocampus, amygdala or cerebellum (Fig. 2). Both forms respond to immunosuppressive treatment. Patients with LGI1 antibodies frequently develop encephalitis with faciobrachial dystonic seizures (stereotyped hyperkinesias that typically affect one arm and the ipsilateral face)90. LGI1 antibodies have been detected in cats with complex focal seizures and orofacial movement91. Humans and cats with LGI1 antibody-associated encephalitis have antibody and complement deposition in affected brain areas, which suggests that similar pathogenic mechanisms are at work in these species.
Human cerebrospinal fluid containing antibodies against N-methyl-d-aspartate receptor (NMDAR; green) binds to NMDAR-expressing human embryonic kidney (HEK) 293 cultured cells (part a) and NMDAR-expressing brain sections from mouse (part b). Similarly, antibodies from human cerebrospinal fluid against leucine-rich glioma-inactivated protein 1 (LGI1; part c) and glial fibrillary acidic protein (GFAP; part d) show a specific immunohistochemical staining pattern on neuronal surfaces and astrocytes in the mouse brain, respectively. All images ×63 magnification.
Public awareness of shared autoimmune mechanisms between humans and animals was raised by the death of Knut the polar bear, who drowned in 2011 following seizures. Autopsy revealed encephalitis with inflammatory infiltrates predominantly composed of plasma cells, but exhaustive screening failed to identify an infectious aetiology92. Young humans with unexplained, non-infectious severe encephalitides often have NMDAR encephalitis with NMDAR antibodies, which causes psychosis, epileptic seizures and hyperkinesias93. Similarly, Knut’s cerebrospinal fluid had high levels of NMDAR autoantibodies, which makes him the first non-human case of NMDAR encephalitis92.
Antibodies against the astrocytic glial fibrillary acidic protein (GFAP) were identified in a patient with novel autoimmune meningoencephalitis, which caused encephalopathy, headache, tremor and ataxia94. GFAP antibodies are also present in the cerebrospinal fluid of dogs with necrotizing meningoencephalitis, which suggests the existence of a lethal canine equivalent95.
Many autoimmune encephalitides cause cognitive and behavioural changes without paralysis or convulsions, which makes diagnosis in animals extremely difficult. The development of more accurate and systematic neurobehavioural assessment in companion and domestic animals will not only improve diagnosis but also advance the development of spontaneous and experimental models.
Mismatch and evolution
Neurologic and psychiatric diseases in humans and animals are often explained through biologically reductionist mechanisms. To fully understand why and how disorders arise requires us to look beyond the proximate explanations of pathophysiology to the evolutionary roots of disease. Proximate levels of causation describe how particular mechanisms (usually cellular and molecular mechanisms) lead to a disease, whereas ultimate levels of causation (usually evolutionary mechanisms) explain why the disease occurs in the first place. Both levels are often linked via the environment because natural selection favours adaptations that help organisms to survive and reproduce in specific environmental conditions. Consequently, when humans or animals find themselves in new environments, they often face mismatch conditions: problems that are more common or severe because the organism is inadequately adapted to its novel environment96. In individuals, mismatches increase morbidity and mortality. In macroevolution, mismatches foster natural selection or extinction.
Rigorous studies in humans demonstrate that mismatches contribute to a large proportion of global disease96, from infectious diseases that result from the agricultural revolution (owing to high population densities or zoonoses from domesticated animals, for example)97 to the modern epidemics of obesity, heart disease, type 2 diabetes mellitus and hypertension — preventable age-related diseases primarily caused by novel high-sugar and high-caloric diets and physical inactivity. Increased sugar consumption is tightly correlated with insulin resistance and obesity, which are complicated by type 2 diabetes mellitus, hypertension and vascular disease. Long-term sugar excess fosters the creation of advanced glycation end products that can induce the formation of the β-sheet structure in Aβ, α-synuclein, transthyretin, copper-zinc superoxide dismutase 1 and prion proteins and thus potentially contributes to neurodegenerative disorders98. These effects can impair cognition and mood, increase the risk of AD and white matter changes and increase the risk of stroke via hypertension.
Humans have undergone strong selection for daily endurance physical activity, with co-evolution of brain size and endurance physical activity99. Apes rest most of the day, feeding and digesting, and engage in only occasional, short bouts of vigorous activity. For 2 million years, humans were mostly tropical hunter-gatherers, walking 9–15 km daily, often carrying children and food, digging tubers for 2–3 hours a day and sometimes running long distances to hunt100. Strong evolutionary selection on musculoskeletal, cardiovascular and mental systems adjusted the capacity of the human body to these demands. Endurance activity evolved to become an essential stimulus for the development and maintenance of normal capacity in the body and brain, where it upregulated neurotransmitters (such as dopamine, serotonin and noradrenaline) and growth factors (such as brain-derived neurotrophic factors (BDNFs), insulin-like growth factor 1 (IGF1) and vascular endothelial growth factor (VEGF))101. Low levels of physical activity can impair development and accelerate body and brain ageing. Physical inactivity is associated with reduced memory; increased rates of depression and anxiety; and increased risks of AD, other dementias102 and epilepsy103. Physical inactivity also affects animals and is best documented in laboratory rodents104.
These data support the hypothesis that reduced sugar intake and increased physical activity can improve neurological and mental health. Further recognition and validation of mismatches in humans and animals might inspire health-care providers to encourage changes in behaviour in human and veterinary patients to prevent some neurological and mental health conditions.
Conclusion
Many neurological and psychiatric disorders affect humans and animals. Review and analysis of the occurrence and non-occurrence of pain, cognitive decline, movement disorders, epilepsy, anxiety and compulsions across the animal kingdom can advance clinical, educational and investigational efforts. This comparative perspective can help to generate novel hypotheses, expand and improve clinical trials and related research and identify natural animal models of disease resistance and vulnerability. Naturally occurring animal diseases (for example, inherited canine narcolepsy) can be studied in much greater depth than the same diseases in humans105. Mechanisms identified using this approach can be translated by inserting human disease-causing genetic variants into mice or other species. The study of shared disease across species can also cast light on the increasingly important effects of our shared environment on the health of all animals. Advances in human medicine can often be readily translated into improvements in animal care, as exemplified by the rapid spread of levetiracetam therapy for epilepsy from human to canine patients, with an excellent safety profile in dogs106.
The species-spanning occurrence of these neuropsychiatric conditions calls for increased collaboration between human and veterinary doctors. Neuroscience advances have closed the gap between psychiatry and neurology to reveal shared pathophysiologies and therapies for neurological and psychiatric disorders. Similarly, recognition of the common evolutionary and mechanistic origins of disease across the animal kingdom should yoke veterinary and human medicine to benefit humans as well as non-human animals.
References
Lanciotti, R. S. et al. Origin of the West Nile virus responsible for an outbreak of encephalitis in the northeastern United States. Science 286, 2333–2337 (1999).
International Association for the Study of Pain. Terminology. IASP. http://www.iasppain.org/Education/Content.aspx?ItemNumber=1698 (2017).
Wall, P. D. & McMahon, S. B. The relationship of perceived pain to afferent nerve impulses. Trends Neurosci. 9, 254–255 (1986).
Moseley, G. L. & Vlaeyen, J. W. S. Beyond nociception: the imprecision hypothesis of chronic pain. Pain 156, 35–38 (2015).
Loeser, J. D. & Treede, R.-D. The Kyoto protocol of IASP basic pain terminology. Pain 137, 473–477 (2008).
Belin, P., Fillion-Bilodeau, S. & Gosselin, F. The Montreal affective voices: a validated set of nonverbal affect bursts for research on auditory affective processing. Behav. Res. Methods 40, 531–539 (2008).
Briefer, E. F. Vocal expression of emotions in mammals: mechanisms of production and evidence. J. Zool. 288, 1–20 (2012).
Holsti, L. & Grunau, R. E. Initial validation of the behavioral indicators of infant pain (BIIP). Pain 132, 264–272 (2007).
Mosele, M. et al. Psychometric properties of the pain assessment in advanced dementia scale compared to self assessment of pain in elderly patients. Dement. Geriatr. Cogn. Disord. 34, 38–43 (2012).
Reid, J. et al. Development of the short-form Glasgow composite measure pain scale (CMPS-SF) and derivation of an analgesic intervention score. Anim. Welf. 16, 97–104 (2007).
Graubner, C., Gerber, V., Doherr, M. & Spadavecchia, C. Clinical application and reliability of a post abdominal surgery pain assessment scale (PASPAS) in horses. Vet. J. 188, 178–183 (2011).
Wright, J. G. Veterinary Anaesthesia (Alexander Eger, Inc., 1941).
Kosek, E. et al. Do we need a third mechanistic descriptor for chronic pain states? Pain 157, 1382–1386 (2016).
Tollison, C. (ed.) in Handbook of Chronic Pain Management (Williams & Wilkins, 1989).
Primason, L., Gleed, R. & Boesch, J. Epidural anaesthesia for treatment of neuropathic pain associated with pelvic limb amputation in a domestic shorthair cat. Vet. Rec. Case Rep. https://doi.org/10.1136/vetreccr-2017-000527 (2017).
Looney, A. Oncology pain in veterinary patients. Top. Companion Anim. Med. 25, 32–44 (2010).
de Grauw, J. C. & van Loon, J. P. Systematic pain assessment in horses. Vet. J. 209, 14–22 (2016).
Klinck, M. P. et al. Translational pain assessment: could natural animal models be the missing link? Pain 158, 1633–1646 (2017).
Hainline, B. et al. International olympic committee consensus statement on pain management in elite athletes. Br. J. Sports Med. 51, 1245–1258 (2017).
Gregory, N. S. et al. An overview of animal models of pain: disease models and outcome measures. J. Pain 14, 1255–1269 (2013).
Caterina, M. J. et al. The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 389, 816–824 (1997).
Facer, P. et al. Differential expression of the capsaicin receptor TRPV1 and related novel receptors TRPV3, TRPV4 and TRPM8 in normal human tissues and changes in traumatic and diabetic neuropathy. BMC Neurol. 7, 11 (2007).
O’Neill, J. et al. Unravelling the mystery of capsaicin: a tool to understand and treat pain. Pharmacol. Rev. 64, 939–971 (2012).
Mogil, J. S. Animal models of pain: progress and challenges. Nat. Rev. Neurosci. 10, 283–294 (2009).
Leal, S. L. & Yassa, M. A. Neurocognitive aging and the hippocampus across species. Trends Neurosci. 38, 800–812 (2015).
Tromp, D., Dufour, A., Lithfous, S., Pebayle, T. & Després, O. Episodic memory in normal aging and Alzheimer disease: insights from imaging and behavioral studies. Ageing Res. Rev. 24, 232–262 (2015).
Espinosa, A. et al. A longitudinal follow-up of 550 mild cognitive impairment patients: evidence for large conversion to dementia rates and detection of major risk factors involved. J. Alzheimers Dis. 34, 769–780 (2013).
Scheltens, P. et al. Alzheimer’s disease. Lancet 388, 505–517 (2016).
Lane, C. A., Hardy, J. & Schott, J. M. Alzheimer’s disease. Eur. J. Neurol. 25, 59–70 (2018).
Drummond, E. & Wisniewski, T. Alzheimer’s disease: experimental models and reality. Acta Neuropathol. 133, 155–175 (2017).
Head, E. et al. Beta-amyloid deposition and tau phosphorylation in clinically characterized aged cats. Neurobiol. Aging 26, 749–763 (2005).
Neilson, J. C., Hart, B. L., Cliff, K. D. & Ruehl, W. W. Prevalence of behavioral changes associated with age-related cognitive impairment in dogs. J. Am. Vet. Med. Assoc. 218, 1787–1791 (2001).
Hart, B. L. Effect of gonadectomy on subsequent development of age-related cognitive impairment in dogs. J. Am. Vet. Med. Assoc. 219, 51–56 (2001).
Sarasa, M. & Pesini, P. Natural non-trasgenic animal models for research in Alzheimer’s disease. Curr. Alzheimer Res. 6, 171–178 (2009).
Rusbridge, C. et al. An aged canid with behavioral deficits exhibits blood and cerebrospinal fluid amyloid beta oligomers. Front. Aging Neurosci. 10, 7 (2018).
Gunn-Moore, D., Kaidanovich-Beilin, O., Gallego Iradi, M. C., Gunn-Moore, F. & Lovestone, S. Alzheimer’s disease in humans and other animals: a consequence of postreproductive life span and longevity rather than aging. Alzheimers Dement. 14, 195–204 (2018).
Youssef, S. A. et al. Pathology of the aging brain in domestic and laboratory animals, and animal models of human neurodegenerative diseases. Vet. Pathol. 53, 327–348 (2016).
Pan, Y. et al. Dietary supplementation with medium-chain TAG has long-lasting cognition-enhancing effects in aged dogs. Br. J. Nutr. 103, 1746–1754 (2010).
Kapl, D. & Rudolphi, K. A. New pharmacologic aspects in the neurologic profile of propentofylline (Karsivan ad us. vet.) [German]. Tierarztl. Prax. Ausg. K. Klientiere Heimtiere 26, 317–321 (1998).
Lemere, C. A. et al. Alzheimer’s disease abeta vaccine reduces central nervous system abeta levels in a non-human primate, the Caribbean vervet. Am. J. Pathol. 165, 283–297 (2004).
Scholtzova, H. et al. Innate immunity stimulation via toll-like receptor 9 ameliorates vascular amyloid pathology in Tg-SwDI mice with associated cognitive benefits. J. Neurosci. 37, 936–959 (2017).
Davis, P. R. et al. Aβ vaccination in combination with behavioral enrichment in aged beagles: effects on cognition, Aβ, and microhemorrhages. Neurobiol. Aging 49, 86–99 (2017).
Gunn-Moore, D., Moffat, K., Christie, L.-A. & Head, E. Cognitive dysfunction and the neurobiology of ageing in cats. J. Small Anim. Pract. 48, 546–553 (2007).
Gunn-Moore, D. A. et al. Ageing changes in cat brains demonstrated by beta-amyloid and AT8-immunoreactive phosphorylated tau deposits. J. Feline Med. Surg. 8, 234–242 (2006).
Grone, B. P. & Baraban, S. C. Animal models in epilepsy research: legacies and new directions. Nat. Neurosci. 18, 339–343 (2015).
Potschka, H., Fischer, A., von Rüden, E.-L., Hülsmeyer, V. & Baumgärtner, W. Canine epilepsy as a translational model? Epilepsia 54, 571–579 (2013).
Podell, M. et al. 2015 ACVIM small animal consensus statement on seizure management in dogs. J. Vet. Intern. Med. 30, 477–490 (2016).
Berendt, M. et al. International veterinary epilepsy task force consensus report on epilepsy definition, classification and terminology in companion animals. BMC Vet. Res. 11, 182 (2015).
Bhatti, S. F. M. et al. International veterinary epilepsy task force consensus proposal: medical treatment of canine epilepsy in Europe. BMC Vet. Res. 11, 176 (2015).
De Risio, L. et al. International veterinary epilepsy task force consensus proposal: diagnostic approach to epilepsy in dogs. BMC Vet. Res. 11, 148 (2015).
Hülsmeyer, V.-I. et al. International veterinary epilepsy task force’s current understanding of idiopathic epilepsy of genetic or suspected genetic origin in purebred dogs. BMC Vet. Res. 11, 175 (2015).
Kearsley-Fleet, L., O’Neill, D. G., Volk, H. A., Church, D. B. & Brodbelt, D. C. Prevalence and risk factors for canine epilepsy of unknown origin in the UK. Vet. Rec. 172, 338 (2013).
Licht, B. G. et al. Clinical presentations of naturally occurring canine seizures: similarities to human seizures. Epilepsy Behav. 3, 460–470 (2002).
Patterson, E. E. et al. Canine status epilepticus treated with fosphenytoin: a proof of principle study. Epilepsia 56, 882–887 (2015).
Kwan, P. et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc task force of the ILAE commission on therapeutic strategies. Epilepsia 51, 1069–1077 (2010).
Lohi, H. et al. Expanded repeat in canine epilepsy. Science 307, 81 (2005).
Alves, L. et al. Polymorphisms in the ABCB1 gene in phenobarbital responsive and resistant idiopathic epileptic Border Collies. J. Vet. Intern. Med. 25, 484–489 (2011).
Wielaender, F. et al. Generalized myoclonic epilepsy with photosensitivity in juvenile dogs caused by a defective DIRAS family GTPase 1. Proc. Natl Acad. Sci. USA 114, 2669–2674 (2017).
James, F. M. K. et al. Diagnostic utility of wireless video-electroencephalography in unsedated dogs. J. Vet. Intern. Med. 31, 1469–1476 (2017).
Davis, K. A. et al. A novel implanted device to wirelessly record and analyze continuous intracranial canine EEG. Epilepsy Res. 96, 116–122 (2011).
Davis, K. A. et al. Mining continuous intracranial EEG in focal canine epilepsy: relating interictal bursts to seizure onsets. Epilepsia 57, 89–98 (2016).
Sillay, K. A. et al. Long-term measurement of impedance in chronically implanted depth and subdural electrodes during responsive neurostimulation in humans. Brain Stimul. 6, 718–726 (2013).
Ung, H. et al. Temporal behavior of seizures and interictal bursts in prolonged intracranial recordings from epileptic canines. Epilepsia 57, 1949–1957 (2016).
Martlé, V. et al. Vagus nerve stimulator placement in dogs: surgical implantation technique, complications, long-term follow-up, and practical considerations. Vet. Surg. 45, 71–78 (2016).
Richter, A., Hamann, M., Wissel, J. & Volk, H. A. Dystonia and paroxysmal dyskinesias: under-recognized movement disorders in domestic animals? A comparison with human dystonia/paroxysmal dyskinesias. Front. Vet. Sci. 2, 65 (2015).
Urkasemsin, G. & Olby, N. J. Canine paroxysmal movement disorders. Vet. Clin. North Am. Small Anim. Pract. 44, 1091–1102 (2014).
de Lahunta, A., Glass, E. N. & Kent, M. Classifying involuntary muscle contractions. Compend. Contin. Educ. Pract. Vet. 28, 516–530 (2006).
Vanhaesebrouck, A. E. et al. A novel movement disorder in related male Labrador Retrievers characterized by extreme generalized muscular stiffness. J. Vet. Intern. Med. 25, 1089–1096 (2011).
Geiger, K. M. & Klopp, L. S. Use of a selective serotonin reuptake inhibitor for treatment of episodes of hypertonia and kyphosis in a young adult Scottish Terrier. J. Am. Vet. Med. Assoc. 235, 168–171 (2009).
Lowrie, M. & Garosi, L. Natural history of canine paroxysmal movement disorders in Labrador retrievers and Jack Russell terriers. Vet. J. 213, 33–37 (2016).
Garosi, L. S., Rossmeisl, J. H., de Lahunta, A., Shelton, G. D. & Lennox, G. Primary orthostatic tremor in Great Danes. J. Vet. Intern. Med. 19, 606–609 (2005).
Forman, O. P. et al. Parallel mapping and simultaneous sequencing reveals deletions in BCAN and FAM83H associated with discrete inherited disorders in a domestic dog breed. PLOS Genet. 8, e1002462 (2012).
Gill, J. L. et al. A canine BCAN microdeletion associated with episodic falling syndrome. Neurobiol. Dis. 45, 130–136 (2012).
Harcourt-Brown, T. Anticonvulsant responsive, episodic movement disorder in a German shorthaired pointer. J. Small Anim. Pract. 49, 405–407 (2008).
Law, T. H. et al. A randomised trial of a medium-chain TAG diet as treatment for dogs with idiopathic epilepsy. Br. J. Nutr. 114, 1438–1447 (2015).
Lowrie, M. et al. The clinical and serological effect of a gluten-free diet in border terriers with epileptoid cramping syndrome. J. Vet. Intern. Med. 29, 1564–1568 (2015).
Lowrie, M. et al. Characterization of paroxysmal gluten-sensitive dyskinesia in Border Terriers using serological markers. J. Vet. Intern. Med. https://doi.org/10.1111/jvim.15038 (2018).
Di Lazzaro, V., Capone, F., Cammarota, G., Di Giuda, D. & Ranieri, F. Dramatic improvement of parkinsonian symptoms after gluten-free diet introduction in a patient with silent celiac disease. J. Neurol. 261, 443–445 (2014).
Merikangas, K. R. et al. Lifetime prevalence of mental disorders in U. S. adolescents: results from the national comorbidity survey replication—adolescent supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 49, 980–989 (2010).
Scarlett, J. M., Salman, M. D., New, J. G. & Kass, P. H. Reasons for relinquishment of companion animals in U. S. animal shelters: selected health and personal issues. J. Appl. Anim. Welf. Sci. 2, 41–57 (1999).
Flannigan, G. & Dodman, N. H. Risk factors and behaviors associated with separation anxiety in dogs. J. Am. Vet. Med. Assoc. 219, 460–466 (2001).
Szechtman, H. et al. Obsessive-compulsive disorder: insights from animal models. Neurosci. Biobehav. Rev. 76, 254–279 (2017).
Geller, D. A. et al. Which SSRI? A meta-analysis of pharmacotherapy trials in pediatric obsessive-compulsive disorder. Am. J. Psychiatry 160, 1919–1928 (2003).
Ahmari, S. E. et al. Repeated cortico-striatal stimulation generates persistent OCD-like behavior. Science 340, 1234–1239 (2013).
March, J. S. et al. The treatment for adolescents with depression study (TADS): long-term effectiveness and safety outcomes. Arch. Gen. Psychiatry 64, 1132–1143 (2007).
Go, Y. Y., Balasuriya, U. B. R. & Lee, C.-K. Zoonotic encephalitides caused by arboviruses: transmission and epidemiology of alphaviruses and flaviviruses. Clin. Exp. Vaccine Res. 3, 58–77 (2014).
Roehrig, J. T. et al. Mutation of the dengue virus type 2 envelope protein heparan sulfate binding sites or the domain III lateral ridge blocks replication in Vero cells prior to membrane fusion. Virology 441, 114–125 (2013).
Tizard, I., Ball, J., Stoica, G. & Payne, S. The pathogenesis of bornaviral diseases in mammals. Anim. Health Res. Rev. 17, 92–109 (2016).
Hoffmann, B. et al. A variegated squirrel bornavirus associated with fatal human encephalitis. N. Engl. J. Med. 373, 154–162 (2015).
Irani, S. R. et al. Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann. Neurol. 69, 892–900 (2011).
Pakozdy, A. et al. Suspected limbic encephalitis and seizure in cats associated with voltage-gated potassium channel (VGKC) complex antibody. J. Vet. Intern. Med. 27, 212–214 (2013).
Prüss, H. et al. Anti-NMDA receptor encephalitis in the polar bear (Ursus maritimus) knut. Sci. Rep. 5, 12805 (2015).
Prüss, H. et al. Retrospective analysis of NMDA receptor antibodies in encephalitis of unknown origin. Neurology 75, 1735–1739 (2010).
Fang, B. et al. Autoimmune glial fibrillary acidic protein astrocytopathy: a novel meningoencephalomyelitis. JAMA Neurol. 73, 1297–1307 (2016).
Matsuki, N. et al. Prevalence of autoantibody in cerebrospinal fluids from dogs with various CNS diseases. J. Vet. Med. Sci. 66, 295–297 (2004).
Lieberman, D. The Story of the Human Body: Evolution, Health, and Disease (Pantheon Books, New York, 2013).
Ewald, P. W. & Burch, G. E. Evolution of infectious disease (Oxford Univ. Press, 1997).
Salahuddin, P., Rabbani, G. & Khan, R. H. The role of advanced glycation end products in various types of neurodegenerative disease: a therapeutic approach. Cell. Mol. Biol. Lett. 19, 407–437 (2014).
Raichlen, D. A. & Polk, J. D. Linking brains and brawn: exercise and the evolution of human neurobiology. Proc. Biol. Sci. 280, 20122250 (2013).
Marlowe, F. W. Hunter-gatherers and human evolution. Evol. Anthropol. Issues News Rev. 14, 54–67 (2005).
Cotman, C. W. & Berchtold, N. C. Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci. 25, 295–301 (2002).
Duzel, E., van Praag, H. & Sendtner, M. Can physical exercise in old age improve memory and hippocampal function? Brain J. Neurol. 139, 662–673 (2016).
Nyberg, J. et al. Cardiovascular fitness and later risk of epilepsy: a Swedish population-based cohort study. Neurology 81, 1051–1057 (2013).
Vivar, C., Potter, M. C. & van Praag, H. All about running: synaptic plasticity, growth factors and adult hippocampal neurogenesis. Curr. Top. Behav. Neurosci. 15, 189–210 (2013).
Mieda, M. The roles of orexins in sleep/wake regulation. Neurosci. Res. 118, 56–65 (2017).
Charalambous, M., Shivapour, S. K., Brodbelt, D. C. & Volk, H. A. Antiepileptic drugs’ tolerability and safety – a systematic review and meta-analysis of adverse effects in dogs. BMC Vet. Res. 12, 79 (2016).
Schmidt, F. et al. Detection and quantification of β-Amyloid, Pyroglutamyl Aβ, and Tau in aged canines. J. Neuropathol. Exp. Neurol. 74, 912–923 (2015).
Braak, H., Braak, E. & Strothjohann, M. Abnormally phosphorylated tau protein related to the formation of neurofibrillary tangles and neuropil threads in the cerebral cortex of sheep and goat. Neurosci. Lett. 171, 1–4 (1994).
Nelson, P. T., Greenberg, S. G. & Saper, C. B. Neurofibrillary tangles in the cerebral cortex of sheep. Neurosci. Lett. 170, 187–190 (1994).
Roertgen, K. E. et al. A beta-associated cerebral angiopathy and senile plaques with neurofibrillary tangles and cerebral hemorrhage in an aged wolverine (Gulo gulo). Neurobiol. Aging 17, 243–247 (1996).
Cork, L. C. et al. Neurofibrillary tangles and senile plaques in aged bears. J. Neuropathol. Exp. Neurol. 47, 629–641 (1988).
Bons, N., Rieger, F., Prudhomme, D., Fisher, A. & Krause, K.-H. Microcebus murinus: a useful primate model for human cerebral aging and Alzheimer’s disease? Genes Brain Behav. 5, 120–130 (2006).
Rosen, R. F. et al. Tauopathy with paired helical filaments in an aged chimpanzee. J. Comp. Neurol. 509, 259–270 (2008).
Cramer, P. E. et al. Aging African green monkeys manifest transcriptional, pathological, and cognitive hallmarks of human Alzheimer’s disease. Neurobiol. Aging 64, 92–106 (2018).
Packer, R. A. et al. Characterization and mode of inheritance of a paroxysmal dyskinesia in Chinook dogs. J. Vet. Intern. Med. 24, 1305–1313 (2010).
Ramsey, I. K., Chandler, K. E. & Franklin, R. J. A movement disorder in boxer pups. Vet. Rec. 144, 179–180 (1999).
Kolicheski, A. L. et al. A homozygous PIGN missense mutation in Soft-Coated Wheaten Terriers with a canine paroxysmal dyskinesia. Neurogenetics 18, 39–47 (2017).
Platt, S. R., Stefani, A. D. & Wieczorek, L. Primary orthostatic tremor in a Scottish deerhound. Vet. Rec. 159, 495–496 (2006).
Acknowledgements
Reviewer information
Nature Reviews Neurology thanks Á. Pákozdy, C. Rusbridge and T. Sabin for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to writing the article. O.D. and B.N.-H. reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Devinsky, O., Boesch, J.M., Cerda-Gonzalez, S. et al. A cross-species approach to disorders affecting brain and behaviour. Nat Rev Neurol 14, 677–686 (2018). https://doi.org/10.1038/s41582-018-0074-z
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-018-0074-z
This article is cited by
-
Going beyond established model systems of Alzheimer’s disease: companion animals provide novel insights into the neurobiology of aging
Communications Biology (2023)
-
Autoantibodies in neurological disease
Nature Reviews Immunology (2021)
-
Feline cognitive dysfunction as a model for Alzheimer’s disease in the research of CBD as a potential treatment—a narrative review
Journal of Cannabis Research (2020)