Abstract
We analyzed the contributions of structural variants (SVs) to gliomagenesis across 179 pediatric high-grade gliomas (pHGGs). The most recurrent SVs targeted MYC isoforms and receptor tyrosine kinases (RTKs), including an SV amplifying a MYC enhancer in 12% of diffuse midline gliomas (DMG), indicating an underappreciated role for MYC in pHGG. SV signature analysis revealed that tumors with simple signatures were TP53 wild type (TP53WT) but showed alterations in TP53 pathway members PPM1D and MDM4. Complex signatures were associated with direct aberrations in TP53, CDKN2A and RB1 early in tumor evolution and with later-occurring extrachromosomal amplicons. All pHGGs exhibited at least one simple-SV signature, but complex-SV signatures were primarily restricted to subsets of H3.3K27M DMGs and hemispheric pHGGs. Importantly, DMGs with complex-SV signatures were associated with shorter overall survival independent of histone mutation and TP53 status. These data provide insight into the impact of SVs on gliomagenesis and the mechanisms that shape them.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
De novo generated sequencing data from this study are accessible under dbGaP accession number phs002380.v1.p1. Previously published sequencing data4,5,6,7 that were reanalyzed here are available under accession codes EGAS00001000575, EGAS00001001139, EGAS00001000572, EGAS00001000192, GSE128745 (ref. 35), GSE54792 (ref. 36) and GSE126319 (ref. 37) and from the ENCODE project38. COSMIC signatures and cancer genes are available at: https://cancer.sanger.ac.uk/cosmic/download. TAD boundaries are from GSE77565 (ref. 63). Source data are provided with this paper. All other data supporting the findings of this study are available from the corresponding author on reasonable request.
Code availability
Publicly available software was used as indicated in the Methods. The main custom analysis code is available at: https://github.com/FrankDubois/pHGG_SVs. All custom code used to connect and reformat the outputs of the publicly available software, as well as code used to generate the figures, is available upon request.
References
Ostrom, Q. T. et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro Oncol. 20, iv1–iv86 (2018).
Puget, S. et al. Mesenchymal transition and PDGFRA amplification/mutation are key distinct oncogenic events in pediatric diffuse intrinsic pontine gliomas. PLoS ONE 7, e30313 (2012).
Mackay, A. et al. Integrated molecular meta-analysis of 1,000 pediatric high-grade and diffuse intrinsic pontine glioma. Cancer Cell 32, 520–537 (2017).
Bender, S. et al. Recurrent MET fusion genes represent a drug target in pediatric glioblastoma. Nat. Med. 22, 1314–1320 (2016).
Buczkowicz, P. et al. Genomic analysis of diffuse intrinsic pontine gliomas identifies three molecular subgroups and recurrent activating ACVR1 mutations. Nat. Genet. 46, 451–456 (2014).
Wu, G. et al. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat. Genet. 46, 444–450 (2014).
Taylor, K. R. et al. Recurrent activating ACVR1 mutations in diffuse intrinsic pontine glioma. Nat. Genet. 46, 457–461 (2014).
Wu, G. et al. Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat. Genet. 44, 251–253 (2012).
Schwartzentruber, J. et al. Driver mutations in histone H3.3 and chromatin remodelling genes in paediatric glioblastoma. Nature 482, 226–231 (2012).
Shoshani, O. et al. Chromothripsis drives the evolution of gene amplification in cancer. Nature 591, 137–141 (2021).
Koche, R. P. et al. Extrachromosomal circular DNA drives oncogenic genome remodeling in neuroblastoma. Nat. Genet. 52, 29–34 (2020).
Kim, H. et al. Extrachromosomal DNA is associated with oncogene amplification and poor outcome across multiple cancers. Nat. Genet. 52, 891–897 (2020).
Turner, K. M. et al. Extrachromosomal oncogene amplification drives tumour evolution and genetic heterogeneity. Nature 543, 122–125 (2017).
Xu, K. et al. Structure and evolution of double minutes in diagnosis and relapse brain tumors. Acta Neuropathol. 137, 123–137 (2019).
Northcott, P. A. et al. Enhancer hijacking activates GFI1 family oncogenes in medulloblastoma. Nature 511, 428–434 (2014).
Bandopadhayay, P. et al. MYB-QKI rearrangements in angiocentric glioma drive tumorigenicity through a tripartite mechanism. Nat. Genet. 48, 273–282 (2016).
Beroukhim, R., Zhang, X. & Meyerson, M. Copy number alterations unmasked as enhancer hijackers. Nat. Genet. 49, 5–6 (2017).
Chen, C. C. L. et al. Histone H3.3G34-mutant interneuron progenitors co-opt PDGFRA for gliomagenesis. Cell 183, 1617–1633.e22 (2020).
Helmsauer, K. et al. Enhancer hijacking determines extrachromosomal circular MYCN amplicon architecture in neuroblastoma. Nat. Commun. 11, 5823 (2020).
Morton, A. R. et al. Functional enhancers shape extrachromosomal oncogene amplifications. Cell 179, 1330–1341.e13 (2019).
Rheinbay, E. et al. Analyses of non-coding somatic drivers in 2,658 cancer whole genomes. Nature 578, 102–111 (2020).
Nik-Zainal, S. et al. Landscape of somatic mutations in 560 breast cancer whole-genome sequences. Nature 534, 47–54 (2016).
Li, Y. et al. Patterns of somatic structural variation in human cancer genomes. Nature 578, 112–121 (2020).
Kim, J. et al. Somatic ERCC2 mutations are associated with a distinct genomic signature in urothelial tumors. Nat. Genet. 48, 600–606 (2016).
Alexandrov, L. B. et al. The repertoire of mutational signatures in human cancer. Nature 578, 94–101 (2020).
Degasperi, A. et al. A practical framework and online tool for mutational signature analyses show intertissue variation and driver dependencies. Nat. Cancer 1, 249–263 (2020).
Angus, L. et al. The genomic landscape of metastatic breast cancer highlights changes in mutation and signature frequencies. Nat. Genet. 51, 1450–1458 (2019).
Puget, S. et al. Biopsy in a series of 130 pediatric diffuse intrinsic Pontine gliomas. Childs Nerv. Syst. 31, 1773–1780 (2015).
Roujeau, T. et al. Stereotactic biopsy of diffuse pontine lesions in children. J. Neurosurg. 107, 1–4 (2007).
Cage, T. A. et al. Feasibility, safety, and indications for surgical biopsy of intrinsic brainstem tumors in children. Childs Nerv. Syst. 29, 1313–1319 (2013).
Gupta, N. et al. Prospective feasibility and safety assessment of surgical biopsy for patients with newly diagnosed diffuse intrinsic pontine glioma. Neuro Oncol. 20, 1547–1555 (2018).
Mermel, C. H. et al. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 12, R41 (2011).
Wala, J. A. et al. SvABA: genome-wide detection of structural variants and indels by local assembly. Genome Res. 28, 581–591 (2018).
Zhang, X. et al. Identification of focally amplified lineage-specific super-enhancers in human epithelial cancers. Nat. Genet. 48, 176–182 (2015).
Krug, B. et al. Pervasive H3K27 acetylation leads to ERV expression and a therapeutic vulnerability in H3K27M Gliomas. Cancer Cell 35, 782–797.e8 (2019).
Suvà, M. L. et al. Reconstructing and reprogramming the tumor-propagating potential of glioblastoma stem-like cells. Cell 157, 580–594 (2014).
Nagaraja, S. et al. Histone variant and cell context determine H3K27M reprogramming of the enhancer landscape and oncogenic state. Mol. Cell 76, 965–980.e12 (2019).
Dunham, I. et al. An integrated encyclopedia of DNA elements in the human genome. Nature 489, 57–74 (2012).
Paolella, B. R. et al. p53 directly represses Id2 to inhibit the proliferation of neural progenitor cells. Stem Cells 29, 1090–1101 (2011).
Frankell, A. M. et al. The landscape of selection in 551 esophageal adenocarcinomas defines genomic biomarkers for the clinic. Nat. Genet. 51, 506–516 (2019).
Pathania, M. et al. H3.3K27M cooperates with Trp53 loss and PDGFRA gain in mouse embryonic neural progenitor cells to induce invasive high-grade gliomas. Cancer Cell 32, 684–700.e9 (2017).
Flavahan, W. A. et al. Insulator dysfunction and oncogene activation in IDH mutant gliomas. Nature 529, 110–114 (2016).
Hadi, K. et al. Distinct classes of complex structural variation uncovered across thousands of cancer genome graphs. Cell 183, 197–210.e32 (2020).
Sondka, Z. et al. The COSMIC Cancer Gene Census: describing genetic dysfunction across all human cancers. Nat. Rev. Cancer 18, 696–705 (2018).
Morganella, S. et al. The topography of mutational processes in breast cancer genomes. Nat. Commun. 7, 11383 (2016).
Bayard, Q. et al. Cyclin A2/E1 activation defines a hepatocellular carcinoma subclass with a rearrangement signature of replication stress. Nat. Commun. 9, 5235 (2018).
Hoopes, J. I. et al. APOBEC3A and APOBEC3B preferentially deaminate the lagging strand template during DNA replication. Cell Rep. 14, 1273–1282 (2016).
Hoffman, L. M. et al. Clinical, radiologic, pathologic, and molecular characteristics of long-term survivors of diffuse intrinsic pontine glioma (DIPG): a collaborative report from the International and European Society for Pediatric Oncology DIPG Registries. J. Clin. Oncol. 36, 1963–1972 (2018).
Zack, T. I. et al. Pan-cancer patterns of somatic copy number alteration. Nat. Genet. 45, 1134–1140 (2013).
Lett, J. T., Caldwell, I., Dean, C. J. & Alexander, P. Rejoining of X-ray induced breaks in the DNA of leukaemia cells. Nature 214, 790–792 (1967).
Gerstung, M. et al. The evolutionary history of 2,658 cancers. Nature 578, 122–128 (2020).
Hoffman, L. M. et al. Spatial genomic heterogeneity in diffuse intrinsic pontine and midline high-grade glioma: implications for diagnostic biopsy and targeted therapeutics. Acta Neuropathol. Commun. 4, 1 (2016).
Nikbakht, H. et al. Spatial and temporal homogeneity of driver mutations in diffuse intrinsic pontine glioma. Nat. Commun. 7, 11185 (2016).
Salloum, R. et al. Characterizing temporal genomic heterogeneity in pediatric high-grade gliomas. Acta Neuropathol. Commun. 5, 78 (2017).
Vinci, M. et al. Functional diversity and cooperativity between subclonal populations of pediatric glioblastoma and diffuse intrinsic pontine glioma cells. Nat. Med. 24, 1204–1215 (2018).
Castel, D. et al. Histone H3F3A and HIST1H3B K27M mutations define two subgroups of diffuse intrinsic pontine gliomas with different prognosis and phenotypes. Acta Neuropathol. 130, 815–827 (2015).
Khuong-Quang, D.-A. et al. K27M mutation in histone H3.3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas. Acta Neuropathol. 124, 439–447 (2012).
Cho, S. W. et al. Promoter of lncRNA gene PVT1 is a tumor-suppressor DNA boundary element. Cell 173, 1398–1412.e22 (2018).
Wu, S. et al. Circular ecDNA promotes accessible chromatin and high oncogene expression. Nature 575, 699–703 (2019).
Rausch, T. et al. Genome sequencing of pediatric medulloblastoma links catastrophic DNA rearrangements with TP53 mutations. Cell 148, 59–71 (2012).
Lawrence, M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499, 214–218 (2013).
Carter, S. L. et al. Absolute quantification of somatic DNA alterations in human cancer. Nat. Biotechnol. 30, 413–421 (2012).
Won, H. et al. Chromosome conformation elucidates regulatory relationships in developing human brain. Nature 538, 523–527 (2016).
Imielinski, M., Guo, G. & Meyerson, M. Insertions and deletions target lineage-defining genes in human cancers. Cell 168, 460–472.e14 (2017).
Smith, D. I., Zhu, Y., McAvoy, S. & Kuhn, R. Common fragile sites, extremely large genes, neural development and cancer. Cancer Lett. 232, 48–57 (2006).
Aguet, F. et al. Genetic effects on gene expression across human tissues. Nature 550, 204–213 (2017).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Johnson, W. E., Li, C. & Rabinovic, A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics 8, 118–127 (2006).
Leek, J. T., Johnson, W. E., Parker, H. S., Jaffe, A. E. & Storey, J. D. The sva package for removing batch effects and other unwanted variation in high-throughput experiments. Bioinformatics 28, 882–883 (2012).
Zhang, Y. et al. Model-based analysis of ChIP-Seq (MACS). Genome Biol. 9, R137 (2008).
Rao, S. S. P. et al. A 3D map of the human genome at kilobase resolution reveals principles of chromatin looping. Cell 159, 1665–1680 (2014).
Rajarajan, P. et al. Neuron-specific signatures in the chromosomal connectome associated with schizophrenia risk. Science 362, eaat4311 (2018).
Durand, N. C. et al. Juicebox provides a visualization system for Hi-C contact maps with unlimited zoom. Cell Syst. 3, 99–101 (2016).
Dali, R., Bourque, G. & Blanchette, M. RobusTAD: a tool for robust annotation of topologically associating domain boundaries. Preprint at bioRxiv https://doi.org/10.1101/293175 (2018).
Grasso, C. S. et al. Functionally defined therapeutic targets in diffuse intrinsic pontine glioma. Nat. Med. 21, 555–559 (2015).
Rosenthal, R., McGranahan, N., Herrero, J., Taylor, B. S. & Swanton, C. deconstructSigs: delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution. Genome Biol. 17, 31 (2016).
Cortés-Ciriano, I. et al. Comprehensive analysis of chromothripsis in 2,658 human cancers using whole-genome sequencing. Nat. Genet. 52, 331–341 (2020).
Shinde, J. et al. Palimpsest: an R package for studying mutational and structural variant signatures along clonal evolution in cancer. Bioinformatics 34, 3380–3381 (2018).
Amin, S. B. et al. Comparative molecular life history of spontaneous canine and human gliomas. Cancer Cell 37, 243–257.e7 (2020).
Caravagna, G. et al. Subclonal reconstruction of tumors by using machine learning and population genetics. Nat. Genet. 52, 898–907 (2020).
Acknowledgements
We thank and acknowledge the children and their families who made this research possible through their participation in pHGG clinical trials and tissue banking protocols. We also thank the many clinicians and researchers who led the DIPG-BATS trial. We would also like to thank the members of the Ligon, Beroukhim and Bandopadhayay laboratories, in addition to R. Liu, J. Rhoades, M. Leventhal, J. Hwang, J. So, D. Mayhew, J. Rennhack, M. Touat, A. Cherniack, B. Rondelli and S. Polo for support and helpful discussions, Active Motif, Inc. for performing the H3K27ac ChIP–seq and Hi-C of the CCDC26-SV tumors, and the Mayo Clinic’s Cytogenetics Core, specifically P. T. Greipp, C. Brandt, T. Gliem and R. Knudson, for FISH analyses. We thank and acknowledge the following funding sources: the National Institutes of Health (NIH): NIH R37 5R37CA255245-02 (P.B.), NIH R01 CA188228 (R.B., K.L.L.), R01 CA215489 (R.B., K.L.L.) and R01 CA219943 (R.B., K.L.L.), the German Research Foundation (research fellowship supporting F.D.), Fund for Innovative Cancer Informatics (R.B.), the Gray Matters Brain Cancer Foundation (R.B.), The Bridge Project of MIT and Dana-Farber/Harvard Cancer Center (R.B., K.L.L.), the Sontag Foundation (R.B.), The V Foundation for Cancer Research (P.B.), Michael Mosier Defeat DIPG Foundation (P.B.), the ChadTough Foundation (P.B.), St. Baldrick’s Foundation (R.B., P.B., J.W.T.), Prayers from Maria Foundation (P.B., M.W.K.), Pediatric Brain Tumor Foundation (P.B., R.B., K.L.L.), Friends of DFCI (P.B., R.B.), the Giving for Gabi Fund (P.B.), Alex’s Lemonade Stand Foundation (P.B., R.B., J.W.T.), the Broad Institute Escape Velocity Award (P.B.), the Jared Branfman Sunflowers for Life Fund (P.B., R.B.), McKennaClaire Foundation (P.B., M.W.K.), We Love You Connie Foundation (P.B., R.B., M.W.K., N.J.), Imagine for Margo and Lemos Family (J.G.), Frederic Lemos and the Gustave Roussy Foundation (JG), The Pussycat Foundation Helen Gurley Brown Presidential Initiative (JWT, PB), Canadian Institutes of Health Research (N.J., C.L.K.), Genome Canada (C.L.K.), Compute Canada and Calcul Quebec (C.L.K.), Zach Carson Fund (M.W.K., R.B., P.B.), Ellie Kavalieros DIPG Fund (M.W.K., R.B., P.B.), Ryan Harvey Fund (M.W.K., R.B., P.B.), Mikey Czech DIPG Foundation (M.W.K., R.B., P.B.), Caroline Cronk Fund (M.W.K., R.B., P.B.), Markoff Art in Giving Foundation (M.W.K., R.B., P.B.), Brock Fleming Fund (M.W.K., R.B., P.B.), Stop and Shop Pediatric Brain Tumor Program (M.W.K., R.B., P.B., K.D.W., S.N.C.), the DIPG Collaborative (M.W.K., R.B., P.B.) and The Cure Starts Now (R.B.). The Mayo Clinic Cytogenetics Core Laboratory is supported by the Mayo Clinic Comprehensive Cancer Center Grant, funded by the National Cancer Institute (P30CA15083).
Author information
Authors and Affiliations
Contributions
F.D., M.W.K., K.L.L., P.B. and R.B. conceived the project. F.D., O.S., N.G., T.Z., J.W., J.T., D.H., A.C., A.H., K.K., M.B.J., K.S.K., C.S., D.W., P.K., H.M., P.H., R.R., R.G., D.D., J.S., M.S., K.W., S.C., J.G., C.K., L.G., N.J., D.J., M.W.K., K.L.L., R.B. and P.B. acquired samples and generated and analyzed the data. F.D., R.B. and P.B. wrote the manuscript. All authors edited the manuscript. K.L.L., P.B. and R.B. supervised the overall study.
Corresponding authors
Ethics declarations
Competing interests
R.B. and P.B. receive grant funding from the Novartis Institute of Biomedical Research for an unrelated project, R.B. receives grant funding from Merck and P.B. has received grant funding from Deerfield Therapeutics for an unrelated project. P.B consults for QED Therapeutics, R.B. consults for and owns equity in Scorpion Therapeutics, and reports consulting or advisory roles for Novartis, Merck (I), Gilead Sciences (I) and ViiV Healthcare (I); research funding from Novartis; patents, royalties other intellectual property—Prognostic Marker for Endometrial Carcinoma (US patent application 13/911456, filed June 6, 2013), SF3B1 Suppression as a Therapy for Tumors Harboring SF3B1 Copy Loss (international application No. WO/2017/177191, PCT/US2017/026693, filed July 4, 2017), Compositions and Methods for Screening Pediatric Gliomas and Methods of Treatment Thereof (international application No. WO/2017/132574, PCT/US2017/015448, filed 1/27/2017). K.L.L. reports grants and personal fees from BMS, grants from Amgen, personal fees and other from Travera LLC, personal fees from Rarecyte, grants from Tragara, grants from Lilly, grants from Deciphera, grants from X4, grants from Charles River Labs and grants from Specicare, outside the submitted work; and has a patent US20160032359A1 pending. M.W.K. is now an employee of Day One Biopharmaceuticals. L.C.G. is the Co-Founder of Thromboprotea Inc. All the remaining authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Sample characteristics and significantly recurrent variants.
(a) Purity of pretreatment biopsy and autopsy samples were not significantly different (p = 0.5, two-sided Wilcoxon, n = 174 tumors, center line of the boxplot indicates the median, bounds of the box the 25th and 75th percentiles and whiskers extend from the box to the largest or smallest value no further than 1.5x IQR). (b) Significantly recurrent SNVs in nonhypermutant tumors (n = 179 tumors). (c) Significantly recurrent SCNAs (n = 179 tumors). All of these SCNAs have been noted3 except for a non-protein-coding locus in 8q.24.21, near MYC—which is also within a separate recurrently amplified locus. (d) Q-Q plot for the analysis of significantly recurrent SV breakpoints. The most SRBs are within the long noncoding RNA CCDC26, within the TAD encompassing MYC (based on n = 179 tumors). (e) Representative examples of the enhancer amplification through simple tandem-duplications within the long noncoding RNA encoding CCDC26.
Extended Data Fig. 2 Lineage specificity of the enhancer peak in CCDC26.
(a) ATAC-seq (top) and H3K27ac ChIP-seq (bottom) enrichment (vertical axis) of samples from different lineages (indicated on right; ‘27 y’ indicates the sample was obtained from a 27-year-old person) across the TAD encompassing MYC (horizontal axis). The location of the MYC coding sequence is highlighted in red. The CCDC26 amplicon boundaries for the 15 samples with the amplicon are indicated by the paired red arrows at the top. The consensus amplicon is indicated by the green dotted lines and centers on an H3K27ac peak present only in glial samples. (b) Hi-C heatmaps depicting DNA interaction profiles (5 kb resolution) from a midline glioma (top), iPSC-derived neural progenitor cells (2nd from top) and two cell lines harboring H3.3K27M mutations (bottom). Red and white indicate high and low interaction frequencies, respectively. MYC interacts more frequently with the H3K27ac peak within CCDC26 (black oval) relative to neighboring loci. The minimal common region of the CCDC26 amplicon is indicated at the bottom of the heatmaps (SV MCR; blue rectangle). (c, d) Correlation between MYC expression and genomic CN of (C) its enhancer amplified in the CCDC26-SV (p = 0.01, two-sided Spearman rank correlation test, samples with MYC CN > 2.5 excluded, n = 94 tumors), or (d) the MYC coding sequence (p = 0.0003, two-sided Spearman rank correlation test, n = 114 tumors). (e, f) Lineage specificity of E1 enhancer activity in (E) neural lineage/BT245 p-value(E1 vs.Backbone) = 0.0056; p-value(LUAD vs. Backbone) = 0.99 and (f) lung epithelial lineage/ A549, p-value(E1 vs. Backbone) = 0.96; p-value(LUAD vs. Backbone) = 0.0071, n = 3 independent experiments, Nested One-Way Anova: Tukey’s Multiple Comparisons. Analogous to Fig. 1g; center line of the boxplot indicates the median, bounds of the box the 25th and 75th percentiles and whiskers extend from the box to the largest or smallest value no further than 1.5x IQR.
Extended Data Fig. 3 Significantly recurrent juxtaposition between MYCN and ID2.
(a) (top) Count matrix showing all possible juxtapositions between pairs of genomic loci. (bottom) Illustration of the principle behind the analysis of recurrent juxtapositions, as exemplified by the MYCN-ID2 loci. First, we count the number of SVs connecting each pair of genomic loci. Using a background model for the probability of juxtapositions generated from an analysis of 2658 cancers21, we then determine the probability of observing this number of SVs due to chance alone, corrected for multiple hypothesis testing. This analysis revealed the MYCN-ID2 juxtaposition as the only significantly recurrent juxtaposition in the window shown. (b) Overlay of amplification frequencies on ChIP-seq data in the ID2 and MYCN loci. The top two tracks show, among tumors with MYCN-ID2 rearrangements (top track, n = 4 tumors or MYCN amplifications without ID2 involvement (second track, n = 4 tumors), the percentage of tumors with amplifications (y-axis) at each genomic locus (x-axis). The bottom eight tracks indicate H3K27ac ChIP-seq profiles across these loci for four H3K27M and four H3WT pHGGs tumors. Coding sequences of ID2 and MYCN are highlighted with yellow and red lines respectively. Significantly enriched H3K27ac peaks (q-value < 0.01) are indicated below each ChIP-seq track. The small region at the ID2 locus that is amplified in all MYCN-ID2 pHGGs shows an H3K27ac peak in the ChIP tracks from all six pHGG tumor samples. Tumors that amplify MYCN without ID2 take in a much larger region of the MYCN TAD into the amplicon. (c) G-track plots indicating copy-number profiles and genome topology after consideration of local SVs, for two examples of pHGGs with focal MYCN amplicons without incorporation of ID2. For both tumors the CN and SV profiles support several possible reconstructions of extrachromosomal circular amplicons. All are limited to the neighborhood of MYCN, presumably incorporating endogenous enhancers from the MYCN TAD.
Extended Data Fig. 4 Structures of recurrent RTK amplicons.
(a) Average amplicon profile for all pHGGs with amplifications in the PDGFRA TAD reaching a CN of at least four (n = 15 tumors). The top track shows the percentage of those tumors with amplifications (vertical axis) at each location (horizontal axis). The track below shows the average CN across all tumors with amplifications in the PDGFRA TAD. The segments included in the PDGFRA amplicon in 80% of tumors are highlighted in the red box. Most amplicons range over several Mbp, often including KIT. (b) Average amplicon profile for all pHGGs with amplifications in the EGFR TAD reaching at least four copies (n = 7 tumors) displayed as in (A). The segments included in all the EGFR amplicons are highlighted in the red box. The pHGG EGFR amplicons always include upstream enhancers elements around SEC61G. (c) Structure of a simple EGFR-TAD amplicon that encompasses enhancers that are also amplified in all tumors with EGFR amplifications. (d) SVs, CN tracks and reconstructions for all pHGGs with high-level MET amplifications. The observed high-level MET amplicons are a few 100kbp in size. Three out of four MET-amplified pHGGs incorporate a downstream region including an enhancer (bottom H3K27ac track) into the amplicon. For all four MET-amplified pHGGs possible reconstructions of the extrachromosomal amplicon are shown above the CN and SV track. (A-D) From bottom to top the tracks show: the genes of interest at the location, a q-value H3K27ac track calculated from eight pHGG tumor samples, the CN and SV for the indicated tumor at the location and reconstructions of possible extrachromosomal amplicons if applicable. (e) FISH with probes for the GATA4 locus on chr8 (red) and the FGFR2 locus on chr10 (green) in tissue from a pHGG with SVs within high-level amplicons that connect these two loci. Scale bar indicates 2 µm. Representative image from n = 200 nuclei.
Extended Data Fig. 5 Associations between SV signatures, genetic variants and SNV signatures.
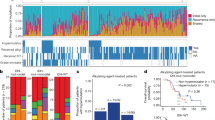
(a) The statistical significance (as determined by Wilcoxon Tests) of positive (enriched, shown in red) and negative (depleted, shown in blue) associations between each SV signature and of all recurrently altered somatic genetic alterations that are documented in the Cancer Gene Census44. Shading within each box indicates level of significance as determined by the q value. (b) De-novo extracted SNV signatures (based on n = 179 tumors). (c) Cosine similarity between de novo extracted SNV signatures and the COSMICv3 SBS-signatures. (d) SNV signature activity in every tumor. The hypermutant tumors on the left show signatures associated with hypermutation in COSMICv3. Signature 3, which is similar to the SBS3 homologous recombination deficiency signature, features prominently in many nonhypermutant tumors.
Extended Data Fig. 6 SV signatures in pHGG based on size, SV type and complexity.
(a) The horizontal axis indicates the size and type of SVs. Del stands for deletion, dup for duplication, inv for inversion, and int for interchromosomal rearrangement. The vertical axis indicates the fraction of SVs within each signature that are contributed by each SV type (based on n = 179 tumors). (b) The statistical significance of positive (enriched) and negative (depleted) associations (Wilcoxon Tests) between each SV signature and of all recurrently altered somatic genetic alterations that are documented in the Cancer Gene Census44. (c) Consensus clustering of the normalized SNV and SV signature activities in each tumor sample (columns). Rows indicate signature activities (top) and potentially oncogenic variants (bottom). (D) Correlations between SV and SNV signatures. Signature labels from this analysis are indicated on the left; the nearest COSMICv3 signatures are indicated on the right, with their proposed mechanisms in parentheses. Complex-SV signatures show a close correlation with APOBEC and homologous recombination deficiency SNV signatures (SBS3). q-values are based on Spearman rank correlations. (e) Enrichment analysis for signature activities in each cluster from panel B. FDR q-values are based on Wilcoxon tests. (f) Significance of signature cluster associations for all variants with correlations reaching q < 0.1; q-values are based on Fisher’s exact tests. Tumors in the complex-SV clusters are enriched for copy-number changes in cancer genes and SNVs in TP53, whereas simple-SV pHGGs tend to exhibit SNVs in different cancer genes. (g) Number of SVs per tumor in each cluster (n = 179 tumors). All differences are significant to q < 0.003 by Wilcoxon tests, center line of the boxplot indicates the median, bounds of the box the 25th and 75th percentiles and whiskers extend from the box to the largest or smallest value no further than 1.5x IQR.
Extended Data Fig. 7 Chromothripsis and homology length at the breakpoints in size/SV-type/complexity SV signatures.
(a, b) SV signature activities in samples that contain or lack (a) chromothriptic regions or (b) extrachromosomal amplifications (n = 179 tumors, center line indicates the median). (c) SV signature analysis including homology length channels reveals five signatures. The horizontal axis indicates the size and type of SVs. Del stands for deletion, dup for duplication, inv for inversion, and int for interchromosomal rearrangement. The vertical axis indicates the amount of SVs within each signature that are contributed by each SV type. (d) SV signature activity in every tumor of the homology SVsigs. Tumors with higher SV counts on the left show complex-SV signature activity whereas tumors with lower SV counts on the right show a mix of simple-SV signatures mimicking the SVsig distribution without homology information (n = 179 tumors). (E) By sample correlation between SVsigs with and without homology.
Extended Data Fig. 8 Associations between SV-defined groups and extended comut plot split by histone groups.
(a) Correlations between SVs and SNV signatures in included in the COSMICv3 signatures database. SNV signatures with well-established links to mechanisms are indicated in parentheses. These include mismatch repair (MMR), homologous recombination (HR) deficiency, APOBEC and aging. q-values were calculated using Spearman rank correlations. (b) Enrichment analysis for signature activities present in Complex-SV and SNV-dominant clusters. q-values were calculated using Wilcoxon tests. (c) Comut plot of the 176/179 (98.3%) tumors with somatic variants in at least one well-known oncogene. Columns represent tumors, ordered within histone mutation-defined subgroups by HC of all potential driver variants. The top two rows show signature metadata.
Extended Data Fig. 9 Associations between SV + histone defined groups.
(a) Jaccard distances between tumor pairs (vertical axis), calculated from the combination of variants in each tumor, across subgroups of H3K27M DMGs. Tumor groups were determined by H3.1 or H3.3 mutations and the combined complex-SV signatures exceeding 20% of all SV signature activity. Tumors were paired within or between these groups, as indicated on the horizontal axis. All differences were significant with q < 0.005 (FDR-corrected two-sided Wilcoxon test) unless indicated otherwise. n = 165 DMGs) (b) Association between MDM4 expression (vertical axis) and CN (horizontal axis). MDM4 gains universally represent arm-level gains of 1q. *** indicates adjusted p = 0.004, ANOVA with two-sided Tuckey post-test, n = 114 tumors. (c, d) Volcano plot indicating the significance (vertical axis; FDR-corrected Fisher’s exact tests) of associations between genetic variants and pHGG subgroups (horizontal axis). (C) Arm-level SCNAs in TP53-disrupted (n = 97 tumors) vs. TP53WT pHGGs (n = 77 tumors). TP53 disruption represented SNVs (n = 88 tumors, often with copy loss) or copy loss alone (n = 9 tumors). (d) Arm-level SCNAs in TP53-disrupted (n = 56 tumors) vs. TP53WT H3K27M mutant DMGs (n = 39 tumors). TP53 disruption represented SNVs (n = 53 tumors often with copy loss) or copy loss alone in (n = 3 tumors). Only significantly recurrent arm-level SCNAs are shown. (e, f) Comparison between pretreatment biopsy and autopsy samples. These groups exhibit no significant differences in (e) the number of SVs per sample (q = 0.6, Wilcoxon, n = 174 tumors) or (f) the activity of the combined complex-SV signatures (q = 0.7, Wilcoxon, n = 174 tumors). Center line of the boxplots indicates the median, bounds of the box the 25th and 75th percentiles and whiskers extend from the box to the largest or smallest value no further than 1.5x IQR. (g) Kaplan–Meier plot indicating OS for (top) H3.1K27M and H3.3K27M DMGs and (bottom) H3.3K27M DMG with and without TP53 SNVs. p-values are from log-rank tests. Error bands show the 95% confidence interval.
Extended Data Fig. 10 Timing analysis of somatic variant acquisition in histone mutation-defined pHGG subgroups.
For each subgroup the individual (per-sample) timing of recurrent variants is fed into a Bradley-Terry model. This results in a strength parameter for each variant which is indicated on the x-axis in log scale and can be interpreted as the relative log odds of the variant being an early event in this subgroup. Each distribution indicates the results of 100 random subsamples of the respective subgroup. Only potential driver variants recurrent in more than two samples are shown. Subgroups: (a) H3.1K27M, n = 24 tumors (b) H3.3K27M, n = 73 tumors (c) H3.3G34R, n = 14 tumors (d) H3WT, n = 63 tumors (e) hypermutant pHGGs, n = 5 tumors. Center line of the boxplot indicates the median, bounds of the box the 25th and 75th percentiles and whiskers extend from the box to the largest or smallest value no further than 1.5x IQR.
Supplementary information
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 9
Statistical source data.
Source Data Extended Data Fig. 10
Statistical source data.
Rights and permissions
About this article
Cite this article
Dubois, F.P.B., Shapira, O., Greenwald, N.F. et al. Structural variants shape driver combinations and outcomes in pediatric high-grade glioma. Nat Cancer 3, 994–1011 (2022). https://doi.org/10.1038/s43018-022-00403-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-022-00403-z
This article is cited by
-
Ppm1d truncating mutations promote the development of genotoxic stress-induced AML
Leukemia (2023)
-
SMARCB1 loss activates patient-specific distal oncogenic enhancers in malignant rhabdoid tumors
Nature Communications (2023)
-
(B)On(e)-cohistones and the epigenetic alterations at the root of bone cancer
Cell Death & Differentiation (2023)
-
Form follows function in cancer genomes
Nature Cancer (2022)
-
K27M in canonical and noncanonical H3 variants occurs in distinct oligodendroglial cell lineages in brain midline gliomas
Nature Genetics (2022)