Key Points
-
Reminds us that general dental practitioners are responsible for the detection and referral of patients with impacted canines.
-
Highlights that early diagnosis at 10 years of age facilitates interceptive extraction of primary canines, which can allow normalisation of eruption.
-
Highlights that early diagnosis can avoid the risk of damage to adjacent teeth.
Abstract
Objective To establish the appropriateness of timing of referrals for patients referred for the management of ectopic maxillary canines, and to evaluate the success of previous recommendations to educate referrers.
Design Retrospective clinical re-audit.
Setting Royal Surrey County Hospital NHS Foundation Trust.
Subjects and methods Data were collected retrospectively for 220 consecutive patients between January 2013 – December 2014 and compared to the gold standard based on the clinical guidelines for management of the palatally ectopic maxillary canine published by the Royal College of Surgeons of England in 2010 which states that all patients with an impacted canine should be referred by 12 years of age.
Results Ectopic maxillary canines represent a significant number of referrals to district general hospitals. One hundred and sixty-seven patients (76%) were referred late (>12 years) at a mean age of 14.1 years, >2 years later than the recommendations made in the Royal College Guidelines. Seventy-six percent of patients were not referred by 12 years of age compared to an audit in 2002 which found 45% delayed referral.
Conclusion Timing of referral was delayed compared with the Royal College Guidelines. An increase in delayed referral suggests that local education programmes introduced after the previous audit did not have a lasting effect.
Similar content being viewed by others
Introduction
A canine that is prevented from erupting into a normal position, either by bone, tooth or fibrous tissue, can be described as impacted. The maxillary canine is the second most commonly impacted tooth, following the mandibular third molar.1 The incidence ranges between 0.8–2.8%.2,3 Palatal impaction occurs more frequently than buccal impaction (ratio 6:1),4,5 and is twice as common in females.6
The cause of impaction is unknown, but is likely to be polygenic7,8 as ectopia occurs more commonly amongst family members,9 and multifactorial.10 Ectopic canines are also often associated with absent, diminutive or malformed lateral incisors and delayed dental development.10
The erupting maxillary canines should be palpable in the buccal sulcus from 10–11 years of age.11 General dental practitioners (GDPs) have a key role and responsibility in early diagnosis and referral. All general dental examinations of patients from the age of 10 years should include this as part of the assessment. British Orthodontic Society guidance12 for referrals for orthodontic treatment recommend early referral when no buccal bulge of the canine is palpable at 10–12 years, as this suggests palatal impaction of canines. According to clinical 2010 guidelines by the Royal College of Surgeons of England,13 all patients with an impacted canine should be referred by 12 years of age. Maxillary canines erupting after 12.3 years in girls and 13.1 in boys may be considered late in their eruption.
If impaired eruption is suspected, early localisation using a clinical assessment with visual, palpation and radiographic methods is indicated so that interceptive measures to encourage eruption can be implemented. Interceptive extraction of the deciduous canine at 10–13 years of age can facilitate improvement of the ectopic canine's position in 12 months.14 This can be a very cost-effective and simple method of correcting ectopic canines with a reported success rate of 62%.15 Although interceptive treatment in suitable cases has been indicated as a useful procedure,16 cases continue to be referred late removing the option for interceptive action. As a result there are consequences of complicated lengthy treatment17,18,19 and costly litigation claims can arise if damage occurs to adjacent permanent teeth.20 The main risk from impaction appears to be root resorption of incisors.21 It has been estimated that 0.6–0.8% of children in the 10–13-year age group have permanent incisors resorbed as a result of canine impaction.5 Interestingly, cone beam computed tomography (CBCT) scanning has detected root resorption in 66.7% of permanent lateral incisors adjacent to impacted maxillary canines.22 Other risks include possible cyst formation.23
Background/rationale
A regional audit published in 2002 assessed over 1,200 patients from nine regional units (including Royal Surrey County Hospital) over a two-year period (2001–2002)24 and found impacted canines to represent nearly a fifth of referrals (17%) to secondary care orthodontic units. Out of the 17% of patients (n = 213) identified with an impacted canine, 45% were referred late thereby removing the chance for simple interceptive treatment. Late referral was found to be complicating treatment in terms of the need for costlier surgery under a general anaesthetic to either remove or expose the impacted tooth, and the associated longer course of orthodontic treatment. Local education programmes were implemented via the then primary care trust (PCT), which were replaced by clinical commissioning groups (CCGs) on 1 April 2013, and also implemented by the local dental committee (LDC). The PCTs and LDCs informed primary care referrers about the importance of appropriate timing of referral for impacted canines. More than 10 years later, this repeat audit aims to review current referral practice of impacted canines.
Aims and objectives
-
To assess the appropriateness of timing of referrals from GDPs for patients with ectopic maxillary canines
-
To evaluate whether recommended education following a previous audit was successful in improving referral behaviour
-
To identify if planned targeted education was necessary.
Method
The audit project was approved by the ethics committee of centre for professional practice (University of Kent) and registered at Royal Surrey County Hospital, Guildford. The gold standard set was:
All patients with an impacted canine should be referred by age 12 years, based on the Royal College of Surgeons of England Guidelines 2010.13
Data was retrospectively collected for a sample of 220 consecutive patients with ectopia of one or both maxillary canines treated who had surgical exposure at Royal Surrey County Hospital over a two-year period (January 2013 – December 2014). The patients in the population sample were identified using codes which represented the expose and bond procedure provided by the RSCH coding department. The information technology department used the codes to compile a list of consecutive patients who were treated at RSCH in between January 2013 – December 2014. Data was captured from medical records using a standardised and agreed data collection proforma that was initially piloted. Data collected included patient age, gender, referral source, radiographic findings, adverse risks and appointments times.
Results
Impacted maxillary canines represent a significant number of referrals to district general hospitals. In this study of a total number of 220 patients, 167 patients (76%) were referred late according to recommendations made in the Royal College Guidelines (12 years of age and over). The mean age of referral was 14.1 years, more than 2 years later than the recommendations made in the Royal College Guidelines (12 years and over) (Fig. 1).
An audit in 2002 from regional units including Royal Surrey County Hospital assessed a sample size of 213 patients identified with an impacted canine over a two-year period (2001–2002). Ninety-six patients (45%) from this group of patients were referred for assessment later than the recommendations made in the Royal College Guidelines. The percentage of late referrals increased from 45% in the earlier study in 2002 to 76% in the present study, losing the opportunity for simple interceptive measures known to have proven positive outcomes. A goodness-of-fit test established the proportion of late referrals had increased (p <0.01).
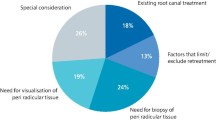
The sources of referral were specialist orthodontists (84%), general dental practitioners (13%) and special care dentists (3%) (Fig. 2). Of the total sample of 220 patients, 133 (65%) were female and 77 (35%) were male, resulting in a male: female ratio of 1:1.7 (Table 1). Fifty-eight patients (26%) were referred for bilateral ectopic canines and the remaining 162 patients (74%) were referred for one ectopic canine only. One third (32%) of referrals included information in the referral letter describing location assessed by palpation (buccal or palatal). Out of this 27%, 63% of canines were found to be palatal, 32% buccal and 5% unknown or in the line of arch.
Forty-three cases referred for ectopic canines had evidence of associated risks. Twenty-five cases (11%) of patients were found to have evidence of root resorption of adjacent incisor teeth as assessed using conventional radiography. Eighteen cases (8%) had radiographic evidence of cystic activity or pathology (supernumeraries or odontomes). Eight referrals had a CBCT as part of the assessment.
Referral to treatment waiting times was calculated from the date of referral to the date of the patient's first NHS consultant-led treatment. Eighty-two percent of patients were seen within the 18 weeks 'referral to treatment' (RTT).
Discussion
Impacted maxillary canines fall into the highest group of Index of Orthodontic Treatment Need – IOTN 5 (5i) and should be referred to an orthodontic specialist. Husain et al.13 detailed relevant clinical guidelines for the management of the palatally ectopic maxillary canine, which were published by the Royal College of Surgeons of England in 2010, confirming that all patients with an ectopic canine should be referred by 12 years of age.
The current study showed two important findings. Firstly, the timing of referral was significantly delayed, with 76% referred more than 2 years later than recommendations made in the Royal College Guidelines, and, secondly suggests local education programmes introduced after the audit in 2002 did not have a lasting effect.
The initial audit in 2002 involved reminders communicated to all referring clinicians highlighting findings of the project and current guidelines. Furthermore, support was gained from the PCT and LDC to enforce these guidelines. It may well have been that there was an improvement of referral timing in the initial stages, which gradually reduced during the 10-year period as new providers arrived and clinicians moved or retired. Unfortunately, any behaviour change was not maintained and changes did not have a lasting effect in the population even though the guidelines are widely available.
Although there has been some research in the area of information retention in dentistry by patients, there has been very little research in the area of information retention by clinical professionals on guidelines and standards in dentistry. The lack of influence of referral guidelines for orthodontic referrals on the behaviour of GDPs has previously been reported.25,26 In this case, local education programmes had been implemented to disseminate referral guidelines to GDPs. The information understood and retained is not known but can in part be measured by the worsened outcomes for patients seen by the results. In a profession where keeping up to date with guidelines and continuing professional development (CPD) is a GDC standard, this outcome was disappointing. It is important to remember that appropriate referral is a GDC requirement according to GDC's 'Standards for the dental team'.27 Standard 1.4.2 states dental professionals must provide patients with treatment that is in their best interests, providing appropriate oral health advice and following clinical guidelines relevant to their situation. Standard 6.3 clearly states dental professionals must delegate and refer appropriately and effectively.
The authors recognise that the current study has a number of limitations which should be discussed. Sample bias could have been introduced increasing the percentage of delayed referrals due to the method of data collection skewing the results. The source data was limited to patients with ectopic canines managed with surgical exposure only and excluded patients who had been successfully managed with interceptive treatment or treatment under local anaesthetic. Limiting the data collection to patients requiring surgical intervention biased the sample towards late referrals and could artificially over report the number of delayed referral patients. The sample should have been derived from a review of all new patient assessments to ensure all canine referrals were included to give a more accurate representation of the proportion of late referrals as had been carried out in the 2002 study.
Also the authors were unable to identify and report the reasons for delay(s) in referral or the stage where the delay in referral occurred. Possible reasons for delay influencing different stages in the referral pathway could have been considered. Delayed referral could have been caused by the patient, GDPs and/or the orthodontist:
-
1
The patient may have presented late, had an erratic attendance, and/or had low motivation for referral
-
2
The GDP may not have identified the need for referral to an orthodontic specialist
-
3
The orthodontist may not have identified the impacted canine, or referral to their service was delayed due to lack of capacity. The 18-week referral to treatment time (RTT)28 is not applicable in a primary care specialist setting and only applies to patients starting NHS consultant-led treatment. Patients referred to primary care specialist practice can find they are placed on a waiting list for many months. Significantly, the largest group referring late was practice orthodontic specialists, which may reflect delayed referral to the specialist from the GDP for the reasons described or a delayed referral from the orthodontist to secondary care.
However, accepting the shortcomings of the study it is clear from the findings that a large number of patients had delayed referral for management of impacted maxillary canines. Eleven percent of the 167 patients referred late were found to have evidence of root resorption of adjacent incisor teeth on plain radiographs posing significant litigation risk. Furthermore, in the majority of cases referred late, delayed diagnosis and referral of ectopic canines led to the need for more complicated lengthy treatment which can be stressful for patients. This involved either surgical exposure or surgical removal, often under general anaesthetic, and more comprehensive orthodontic treatment. Delayed referral may remove the opportunity for interceptive treatment by extracting primary canine(s) (10–13 years) in the hope that this would encourage eruption of impacted permanent canines. However, a Cochrane review in 201229 was critical of the main evidence in support of this practice from a study by Ericson and Kurol.15 The study was excluded from the review, as it was a prospective case series with no control group. The review concluded that there was no evidence to support the removal of primary canines to intercept palatal impaction of the permanent canine.
More recently a randomised control trial carried out by Naoumova et al.30 in 2014 analysed the effect of interceptive extraction of the primary canine in children with palatally displaced canines (PDCs). These workers found that 69% of the PDCs erupted in the extraction group compared with 38% in the non-extraction group. This was a statistically significant discovery supported by a good level of evidence. Risks of removing the primary canine are low, in comparison to complicated lengthy treatment often involving general anaesthetic and potential litigation risks associated with root resorption. Hence, interceptive removal of the primary canine to encourage eruption of an ectopic canine would be a reasonable consideration. This would be subject to an assessment and radiographs checking for the presence and/or position of the PDC. If there is no improvement to the ectopic canine's position 12 months after extraction of the primary canine, or no evidence that interceptive extraction of the primary canine can result in improved position of ectopic permanent canine then referral is indicated.
To ensure an increase in the uptake of changes and improvement of patient outcomes, the authors propose the following recommendations:
-
1
Gaining support from local area teams to enforce guidelines and implement delivery of education and training to GDPs. i.e. CPD courses about the importance of appropriate timing and orthodontic referral
-
2
The 18-week RTT should apply to primary orthodontic services as well as secondary care
-
3
Reminders communicated to all referring clinicians highlighting findings of this project and the current guidelines
-
4
Delivery of feedback to those who consistently delay referral
-
5
The implementation of electronic referral systems may improve the referral process by prompting the referrer to assess for impacted canines.
Conclusions
In the population studied, the findings indicated that 76% of impacted canines referred to a secondary care unit were delayed by 2 years. Although it is accepted that study design could have over-reported the number of delayed cases. Surprisingly, an increase in delayed referral was found despite the implementation of education to referrers since the previous audit in 2002. Delayed referral of impacted canines adds on additional burden of care to the patient and family and leads to use of resources that timely referral may have avoided. The authors propose strategies are implemented to reduce the incidence of late referrals with support from local area teams, commissioners and local dental committees to remind dentists about the importance of timely referral of impacted canines.
This study has re-enforced the importance of continued education. The authors believe continued education for GDPs is of great importance in reducing the burden of care for the patient and costs to the NHS, as well as the need for GDC registrants to meet the GDC's Standards for the dental team and ensure patients are treated at the right location, by the right service, at the right time.
Remember
-
1
Canines erupt between 11 and 12 years of age
-
2
Interceptive treatment by extraction of the deciduous canine (10–13 years)
-
3
The crown of the upper canine should be detectable as a bulge in the buccal sulcus by 10 years of age. If not, or you are not sure, refer for a specialist opinion
-
4
Fifty percent of ectopic upper canines have an adjacent lateral incisor absent or small. This is a good indicator of possible ectopic canines at 8–9 years old when the upper lateral incisor should erupt
-
5
Twelve percent of cases with impacted maxillary canines have associated root resorption of incisors. Recent work has shown that the resorption risk can be up to 40%
-
6
Delayed referral of impacted canines is a medico-legal risk. Parents are increasingly asking would earlier referral have been more appropriate.
References
Bass T P . Observation on the misplaced upper canine tooth. Dent Pract Dent Rec 1967; 18: 25–33.
Cooke J, Wang H L . Canine impactions: Incidence and management. Int J Periodontics Restorative Dent 2006; 26: 483–491.
McSherry P F . The ectopic maxillary canine: A review. Br J Orthod 1998; 23: 209–216.
Ericson S, Kurol J . Longitudinal study and analysis of clinical supervision of maxillary canine eruption. Community Dent Oral Epidemiol 1986; 14: 172–176.
Ericson S, Kurol J . Radiographic examination of ectopically erupting maxillary canines. Am J Ortho Dentofacial Orthop 1987; 91: 483–492.
Bishara S E . Impacted maxillary canines: A review. Am J Orthod Dentofacial Orthop 1992; 101: 159–171.
Peck S, Peck L, Kataja M . The palatally displaced canine as a dental anomaly of genetic origin. Angle Orthod 1994; 64: 249–256.
Peck S, Peck L, Kataja M . Concomitant occurrence of canine malposition and tooth agenesis: evidence of orofacial genetic fields. Am J Orthod Dentofacial Orthop 2002; 122: 657–660.
Zilberman Y, Cohen, Becker A. Familial trends in palatal canines, anomalous lateral incisors, and related phenomena. Euro J Orthod 1990; 12: 135–139.
Brin I, Becker A, Shalhav M . Position of the maxillary permanent canine in relation to anomalous or missing lateral incisors: a population study. Euro J Orthod 1986; 8: 12–16.
Hurme V O . Ranges of normalcy in the eruption of permanent teeth. J Dent Child 1949; 16: 11–15.
British Orthodontic Society. Managing the developing dentition. A guide for dental practitioners. 2010. Available online at http://www.bos.org.uk/Portals/0/Public/docs/Making%20a%20Referral/Managing-the-Developing-Occulusion-Updated-Apr10.pdf (accessed October 2016).
Husain J, Burden D, McSherry P . Management of the palatally ectopic maxillary canine (Update of 1997 Guideline written by Burden D, Harper C, Mitchell L et al.). The Royal College of Surgeons of England, Faculty of Dental Surgery Clinical Guidelines, 2010. Available online at https://www.rcseng.ac.uk/-/media/files/rcs/dental-faculties/publications/manpalectmaxcan2010.pdf?la=en. (accessed October 2016)
Bruks A, Lennartsson B . The palatally displaced maxillary canine. A retrospective comparison between an interceptive and a corrective treatment group. Swed Dent J 1999; 23: 149–161.
Ericson S, Kurol J . Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Euro J Orthod 1988; 10: 283–295.
Power S M, Short M B . An investigation into the response of palatally displaced canines to the removal of deciduous canines and an assessment of factors contributing to favourable eruption. Br J Orthod 1993; 20: 215–223.
Stewart J A, Heo G, Glover K E . Factors that relate to treatment duration for patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop 2001; 119: 216–425.
Becker A, Chaushu S . Success rate and duration of orthodontic treatment for adult patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop 2003; 124: 509–514.
Fleming P S, Scott P, Heidari N, DiBiase A T . Influence of radiographic position of ectopic canines on the duration of orthodontic treatment. Angle Orthod 2009; 79: 442–446.
Mathews D P, Kokich V G . Palatally impacted canines: The case for preorthodontic uncovering and autonomous eruption. Am J Orthod Dentofacial Orthop 2013; 43: 450–458.
Ericson S, Kurol J . Resorption of incisors after ectopic eruption of maxillary canines: A CT study. Angle Orthod 2000; 70: 415–423.
Walker L, Enciso R, Mah J . Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2005; 128: 418–423.
Mourshed F . A roentogenographic study of dentigerous cysts. I. Incidence in a population sample. Oral Surg Oral Med Oral Pathol 1964; 18: 47–53.
Hepworth C, Taylor N G, Jones A G et al. A regional audit of patients referred with impacted maxillary canines. South West Thames Clinical Effectiveness Group, 2002.
O'Brien K, Wright J, Conboy F et al. Orthodontics: The effect of orthodontic referral guidelines: a randomised controlled trial. Br Dent J 2000; 188: 392–397.
Hassan T, Nute S J . An audit of referral practice for patients with impacted palatal canines and the impact of referral guidelines. Br Dent J 2006; 200: 493–496.
General Dental Council. Standards for the Dental Team. 2013. Available online at http://www.gdc-uk.org/Dentalprofessionals/Standards/Documents/Standards%20for%20the%20Dental%20Team.pdf (accessed October 2016).
NHS England. Consultant-led referral to treatment waiting times. March 2008 to September 2015. Available online at www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/ (accessed October 2016).
Parkin N, Furness S, Shah A, Thind B, Marshman Z, Glenroy G, Dyer F, Benson P E . Extraction of primary (baby) teeth for unerupted palatally displaced permanent canine teeth in children. Cochrane Database Syst Rev. 2012; 12.
Naoumova J, Kurol J, Kjellberg H . Extraction of the deciduous canine as an interceptive treatment in children with palatal displaced canines–part I: shall we extract the deciduous canine or not? Euro J Orthod 2014; cju040.
Acknowledgements
The authors would like to acknowledge the support of the Royal Surrey County Hospital NHS Foundation Trust Research & Development scheme.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Patel, D., Taylor, N. Are patients with impacted canines referred too late?. Br Dent J 221, 561–564 (2016). https://doi.org/10.1038/sj.bdj.2016.816
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.816