Abstract
OBJECTIVE: To comparatively evaluate cut-off points of waist circumference, body mass index and waist to hip ratio with respect to their ability to predict other individual and multiple cardiovascular disease risk factors.
DESIGN: Population-based, cross-sectional surveys.
SUBJECTS: A total of 9913 men and women aged 18–74, selected using health insurance registries from five Canadian provinces.
MEASUREMENTS: Anthropometric measures, other cardiovascular risk factors, receiver operating characteristic curves, sensitivity, specificity, positive and negative predictive values.
RESULTS: Waist circumference may be the best single indicator of other individual and multiple cardiovascular risk factors. Optimal cut-off points of all anthropometric measures are dependent on age, sex and the prevalence of the risk factor(s) being considered. For waist circumference, cut-off points of ≥90 cm in men and ≥80 cm in women may be most appropriate for prediction of individual and multiple risk factors in Caucasian populations.
CONCLUSION: Health professionals should incorporate the use of waist circumference measurements in their routine clinical examination of adult patients.
Similar content being viewed by others
Introduction
In June 1997, the World Health Organization reported overweight and obesity to be ‘an escalating epidemic’,1 with health consequences that are now well recognized. Obesity is associated with five of the 10 leading causes of death in industrialized countries including heart disease, some types of cancer, stroke, diabetes and atherosclerosis.2 In Canada, the prevalence of both obesity and cardiovascular disease risk factors is high.3,4,5,6
The World Health Organization has agreed on an international standard for identifying overweight and obesity in adult populations using the body mass index (weight/height2).7 However, increased risk of cardiovascular disease has been found in individuals presenting with distribution of excess fat in the abdominal region8,9 and at present there is no standard measure of abdominal obesity that is widely accepted. The majority of current studies agree that waist circumference (WC) is probably a better indicator of abdominal fatness and cardiovascular disease than either body mass index (BMI) or waist-to-hip ratio (WHR).10,11,12,13,14 A WC value of approximately 95 cm in both men and women, and WHR values of 0.94 for men and 0.88 for women have been found to correspond to a critical accumulation of visceral adipose tissue (130 cm2).15 WCs of 94 cm or greater in men and 80 cm or greater in women have been reported to be indicative of the need for weight management16 and to identify those at risk for cardiovascular disease.17 Research to date has been limited with respect to evaluation of the ability of anthropometric measures to predict multiple risk factors for cardiovascular disease. It is now recognized that cardiovascular risk increases with the number of risk factors and that even mild elevations of several risk factors may pose as great or a greater risk as a single highly elevated risk factor.18,19,20,21 The present study was designed to determine and comparatively evaluate cut-off points of WC, BMI and WHR with respect to their ability to individually or collectively predict a number of cardiovascular risk factors at different ages, including multiple risk factors.
Methods
Study design and sample
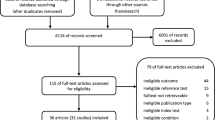
Subjects for this study were participants in the Canadian Heart Health Surveys, which were completed in all 10 Canadian provinces between 1986 and 1992. The present study uses a subgroup of the sample, consisting of individuals living in the provinces of Alberta, Manitoba, Ontario, Quebec and Saskatchewan where waist and hip circumference measurements were taken (9913 individuals).
A detailed description of the survey methods has been given in a previous publication.22 Stratified, two-stage, replicated probability samples were used, with selection made from sampling units based on geographic area, sex and age groups using health insurance registries. Variable response rates were obtained in each province, with the overall response rate for the survey estimated to be 78%.
Measurements
An interview was conducted in the home setting and obtained information regarding physical activity, smoking, diabetes and hypertension status. Blood pressure measurements (systolic and diastolic) were taken according to a standard protocol at the beginning and end of the interview, and repeated two more times in a subsequent clinic visit. Fasting blood samples were obtained and subsequently analyzed at the J. Alick Little Lipid Research Laboratory, University of Toronto, which is certified under the National Heart, Lung and Blood Institute, Center for Disease Control Lipid Standardization Program.
Anthropometric measurements were performed in the morning following a 12 h fast. WC was measured at the end of a normal expiration, with the measuring tape positioned at the level of noticeable waist narrowing. When narrowing could not be determined, the circumference was measured at the level of the lower floating rib. For hip circumference, the tape was positioned around the hips at the level of the symphysis pubis and the greatest gluteal protuberance. Height was measured with participants standing on a hard surface against a wall, using a square and tape measure fixed to the wall. All measurements were recorded to the nearest centimeter. Weight was measured to the nearest 100 g using a calibrated balance beam scale. BMI was calculated as the ratio of weight to height squared (kg/m2). WHR was calculated as WC (cm) divided by hip circumference (cm).
Individuals were considered to have hypertension if their average systolic blood pressure was ≥140 mmHg or if their average diastolic blood pressure was ≥90 mmHg, or if they were under treatment for hypertension. Treatment for hypertension included prescription medication or nonpharmacological treatment (weight control or sodium/salt restriction). The presence of abnormal lipid levels was defined as total cholesterol ≥5.2 mmol/l or low-density lipoprotein≥3.4 mmol/l or high density lipoprotein <0.9 mmol/l or a ratio of total cholesterol to high density lipoprotein ≥4.5 mmol/l or triglyceride ≥2.3 mmol/l. Combinations of ‘both hypertension and dyslipidemia’ and ‘either hypertension or dyslipidemia’ were considered as separate risk factor categories. The presence of ‘one or more’, ‘two or more’ and ‘three or more’ of the five major risk factors for cardiovascular disease (hypertension, dyslipidemia, self-reported diabetes, daily cigarette smoking and sedentary lifestyle) were also evaluated. Individuals were considered sedentary if they did not regularly engage in physical activity (at least once a week over the previous month) during their leisure time.
Analyses
Receiver operating characteristic (ROC) curves were used to compare the anthropometric measures.23 Sensitivity, specificity and positive and negative predictive values were calculated over a range of potential cut-off points for WC, BMI and WHR, with respect to predicting the presence/absence of the seven previously described risk factor categories. The optimal cut-off point for each anthropometric measure for men and women was determined by the point of convergence of sensitivity and specificity (ie by simultaneously maximizing the two). This was completed for men and women separately, by 10 y age group, and for all ages combined. McNemar's chi-square statistic was used to determine whether significant differences were present between any two of the three anthropometric measures in terms of accuracy in classifying individuals according to the presence/absence of risk factors (ie percentage of true positives and negatives vs false positives and negatives). This analysis was also used to compare WC with combinations of the anthropometric measures (for example WC compared to WC and BMI).
The means reported in this paper have been weighted to account for the sample design. Standard errors were estimated using the jackknife method. These and other analyses were carried out using SAS computer software (SAS Institute Inc.).
Results
Means and standard errors for WC, BMI and WHR are presented in Table 1. Within any given age category, men have higher anthropometric measurements than women, although BMI is similar for men and women at older ages (55–64 and 65–74). For all men combined the mean WC is approximately 12 cm greater than for all women, and the mean WHR is 0.12 higher for men. The mean BMI is one unit higher for men. All measurements are seen to increase with age for both men and women, up to the 55–64 y age category. Little change is seen in WHR between the 55–64 and 65–74 y age groups, and only a slight increase is seen in WC for men. The mean WC for women declines in the 65–74 y age group, as does BMI for both sexes.
The prevalence of risk factors is shown in Table 2. The categories of ‘one or more risk factors’, dyslipidemia and ‘hypertension or dyslipidemia’ are seen to be most prevalent, while hypertension, ‘both hypertension and dyslipidemia’ and ‘three or more risk factors’ are the least prevalent. An increase in prevalence of all risk factors is seen with increasing age, with the exception of a slight drop in prevalence in some of the risk factors in the older age groups of men. All risk factors are more prevalent in men than women, except in the older age groups. Dyslipidemia is more prevalent in women aged 55–64 and 65–74. The prevalence of ‘one or more risk factors’ is similar in men and women aged 55–64 and greater in women ages 65–74. The prevalence of hypertension and ‘hypertension and dyslipidemia’ is also higher in 65 to 74-y-old women.
The calculated areas under the ROC curves for WC range between 0.68 and 0.76 for both men and women over the selected risk factors (Table 3). Areas range between 0.70 and 0.75 (men) and 0.67 and 0.74 (women) for WHR, and between 0.62 and 0.72 (men) and 0.64 and 0.73 (women) for BMI. The area under the ROC curve is most frequently the highest for WC followed by WHR.
Cut-off points for WC, BMI and WHR where sensitivity approximates specificity for each risk factor (all ages combined) are shown in Table 4. Values for WHR are between 0.88 and 0.92 for men and 0.76 and 0.80 for women over the various risk factors, while BMI values range between 25 and 26 for men and 23 and 26 for women. Cut-off points for WC range between 89 and 95 cm for men and 75 and 82 cm for women over the various risk factors. In general, values are lowest for dyslipidemia, ‘one or more risk factors’ and ‘either hypertension or dyslipidemia’, (the more prevalent risk conditions), and highest for hypertension, ‘hypertension and dyslipidemia’ and ‘three or more risk factors’ (less prevalent risk conditions).
Across 10 y age categories, cut-off points for BMI vary between 23 and 28 for men and 22 and 28 for women (data not shown). Values are lowest in the 18–24 y age group and increase with age, but consistently drop in the 65–74 y age category for both men and women. Values for WHR are between 0.84 and 0.95 for men and between 0.74 and 0.83 for women, with the lowest values occurring only in a few isolated instances in the 18–24 y age group. The cut-off points for WC (Table 5) vary between 83 and 99 cm for men and 69 and 88 cm for women. Values again increase with age; however, a drop in values is seen in the 65–74 y age group for women only. Across risk factor categories, similar patterns to all ages combined are seen, with the lowest cut-off points for dyslipidemia and ‘one or more risk factors’, and the highest values for hypertension and ‘three or more risk factors’.
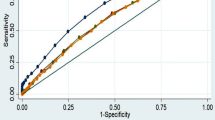
A comparison of the sensitivity, specificity and the average of the total of sensitivity+specificity for ‘two or more risk factors’, using the three indicators as well as combinations of indicators, is depicted in Figures 1 and 2. These comparisons use WC cut-off points of 90 cm for men and 80 cm for women, BMI of 25, and WHR values of 0.9 for men and 0.8 for women. For indicators used alone, the averages of sensitivity+specificity values are within 5% of each other for both men and women. Of the three individual indicators, WC has the highest sensitivity while WHR has the highest specificity and average sensitivity+specificity. No combination of indicators has a higher average sensitivity+specificity than WHR alone. For combinations of one or more indicators, sensitivity is higher than individual indicators, while specificity is lower. For combinations involving both of any two indicators, or all of the three indicators, the reverse is true.
Comparison of the selected anthropometric measures with respect to their ability to predict the presence/absence of ‘two or more risk factors’ is shown in Table 6. Cut-off points for both WC and WHR are seen to have a higher percentage of correct prediction than BMI for both men and women. There is a significant difference between the percentage of individuals whose risk factor status would be correctly predicted using WC but would be incorrectly predicted using BMI and the percentage of individuals whose risk factor status would be correctly predicted using BMI but would be incorrectly predicted using WC (P<0.01). Similarly, significant differences are seen between WHR and BMI. The difference in accuracy of prediction using WC vs WHR is not significant for either men or women, and no combination of measures (ie WC and/or WHR, BMI or both) is significantly more accurate than WC alone at the 0.01 level of significance. However, the combination of WC and WHR is significantly more accurate than WC alone at the 0.05 level of significance for women.
For the other risk factors investigated (data not shown), both WC (90 cm for men and 80 cm for women) and WHR (0.9 for men and 0.8 for women) consistently have a higher average of sensitivity+specificity than BMI25 has. The averages of sensitivity+specificity for WC and WHR are invariably within 1.3% of one another for males. For females and all risk factors, WC has the highest average sensitivity+specificity of the three individual indicators, except in the case of ‘three or more risk factors’, where WHR is 1.6% higher. When comparing the percentage accuracy of risk factor prediction, WC is consistently more accurate in prediction than BMI (however, in one instance the difference between WC and BMI has borderline significance at the 0.01 level). WC is as accurate or more accurate than WHR in prediction for males (many differences are not significant at P<0.05). For females, WC is more accurate than WHR for ‘one or more risk factors’ and ‘hypertension or dyslipidemia’. There is no significant difference between WC and WHR for hypertension or for dyslipidemia, while WHR is more accurate than WC in prediction of ‘hypertension and dyslipidemia’ and ‘three or more risk factors’. For the less prevalent risk factors (hypertension, ‘hypertension and dyslipidemia’, and ‘three or more risk factors’), the use of WC plus another indicator (ie WC and WHR, WC and BMI, all three) is more accurate than WC alone. For more prevalent risk factors (dyslipidemia, ‘hypertension or dyslipidemia’, and ‘one or more risk factors’), the use of any one or more of the indicators (ie WC or WHR, WC or BMI, any of the three) has more accuracy than use of WC alone.
There are significant differences in the proportion of individuals that would be correctly predicted when the BMI varies between 25 and 26 for men and 23 and 25 for women. A lower BMI is significantly more accurate in prediction of risk factors that are more prevalent, while a higher BMI is more accurate in prediction of the less prevalent risk factors. For WC, a 1–3 cm change in the cut-off value in either direction may or may not make a significant difference in the overall accuracy of prediction. For example, WC of 80 cm for women is not significantly different from the previously identified optimal cut-off point of 77 cm in predicting the presence/absence of dyslipidemia. However, significant differences are seen between WC cut-off points of 80 and 81 cm in prediction of hypertension in women.
Discussion
This study has attempted to determine and comparatively evaluate cut-off points of WC, BMI and WHR as predictors of cardiovascular risk factors, primarily based on analysis of sensitivity, specificity and positive and negative predictive values. Results indicate that ranges of cut-off points for each of these anthropometric variables may be considered. Optimal cut-off points are dependent on sex, age and the prevalence of the risk factor being screened. Lower cut-off points are more appropriate for women, at younger ages, and for more prevalent risk factors such as dyslipidemia. Higher values are more suitable at older ages (although a drop is often seen in the highest age category 65–74), and for less prevalent risk factors such as hypertension and multiple risk factors. When looking at all ages combined, there is little variation in cut-off points for WHR, with 0.9 for men and 0.8 for women considered optimal. These figures are in close agreement with findings of previous studies.24 For BMI, optimal cut-off points range between 23 and 26 for women and 25 and 26 for men. The global standard of BMI≥25 for measurement of overweight for both sexes7 falls in both of these ranges. Optimal values of WC fall into a wider range (89–94 cm for men and 77–82 cm for women) and are dependent on the prevalence of the risk factor considered. The optimal WC cut-off points of 94 cm for men and 81 cm for women for hypertension are close to the waist circumference ‘Action Level 1’ proposed by Han et al.17
The findings of this research concur with previous studies in concluding that WC is probably the best single anthropometric measure to use in identifying individuals with cardiovascular disease risk factors.25 This was reflected in the calculated areas under the ROC curves, as well as in comparison of accuracy of the cut-off points in risk factor prediction. When compared to a BMI cut-off point of 25, WC cut-off points of 90 cm for men and 80 cm of women were consistently more accurate in predicting all risk factors considered. WHR also appears to be a better screening tool for cardiovascular risk factors than BMI; however, it does not appear to offer any distinctive advantage over WC. There was often no significant difference between WC and WHR in the accuracy of risk factor prediction, but the former was usually as good or better than the latter.
The WC measure has several advantages over both BMI and WHR. Of primary importance is the simplicity by which it may be used in a clinical setting, and the ease of interpretation. It requires only the use of a tape measure, alleviating the expense of the equipment and space needed to measure height and weight. By requiring a single measurement as opposed to the ratio of two measures, it is less susceptible to measurement and calculation errors. Given these advantages, it is likely that physicians and clinicians would be more accepting of WC measurement. There are a number of problems inherent in the use of a ratio indicator such as WHR, including biological interpretation.26 Because of the equation used to determine this value, both lean and massively obese individuals may end up having the same WHR. The use of the waist-to-height ratio has been reported to be a useful predictor of coronary heart disease risk factors in other studies.27 However, previous reports of an association between WC and height28 were confirmed at the outset of this study. The minimal improvement that might result from the use of waist-to-height ratio was not felt to be sufficient to recommend the calculation of a ratio value.
Optimal values of WC are age dependent, in agreement with earlier studies.29 The identification of higher cut-off points in the lower ages may relate to findings that, for a given WC, older individuals have higher amounts of visceral adipose tissue.15,30 No single cut-off point of WC is optimal for all ages and for different cardiovascular risk factors. For practical reasons, the values of 90 cm for men and 80 cm for women may be the best measures to use for the population at large and in a clinical setting. They are easy numbers to remember and are most predictive of ‘two or more risk factors’, which fall into the middle of the range in terms of risk factor prevalence, and probably in terms of predicting risk of cardiovascular disease.
For any indicator and risk factor, there is a constant tradeoff between sensitivity and specificity, with an increase in sensitivity corresponding to a decrease in specificity, and the overall accuracy of prediction depending on the population prevalence of the risk factor.23 It is therefore not surprising that no combination of measures consistently yielded better accuracy than the use of a single measurement. The use of an ‘either/or’ indicator option (for example WC or WHR) will result in higher sensitivity and lower specificity, while the use of a two- or three-indicator combination (for example WC and BMI) will have lower sensitivity but higher specificity.
It could be argued that it might be wise to identify as many individuals with cardiovascular risk factors as possible by simply maximizing the sensitivity and erring extensively on the side of false positives. However, there is always necessary caution in labeling individuals in need of weight management. For this study, it is felt that a conservative approach was chosen in attempting to find a tradeoff between sensitivity and specificity by choosing cut-off points where the two converge. In using these cut-off points as a screening tool it is likely there will be a number of individuals who will be erroneously classified as at risk, but who might nonetheless benefit from nutrition and lifestyle counseling. It is not suggested that individuals who fail the screening and appear to be risk-free undergo further expensive diagnostic testing. However, given the high prevalence of dyslipidemia and hypertension in this population, as well as previous reports of a high number of individuals in this and other populations who are unaware of their hypertensive status,31,32 full attention should be provided to those individuals who may possibly be at risk.
In order to increase the sensitivity and specificity of risk factor prediction using WC, one could consider adjusting the base cut-off points of 90 cm for men and 80 cm for women within a range of 10 cm on either side of these values. The amount of adjustment would be dependent on the age of the individual and the risk factor being considered. The base value could be adjusted 2 cm downward for every 10 y in age below 35 and upward 2 cm for every 10 y in age above 45. The base cut-off point could be adjusted an additional 2 cm downward to predict individuals at risk for ‘one or more risk factors’ and dyslipidemia, and 4 cm higher when considering risk of hypertension, ‘both hypertension and dyslipidemia’ or ‘three or more risk factors’.
This study has examined the relationship between anthropometric cut-off points and intermediary factors that are likely to lead to incident coronary events or other health problems. For this reason, behavioral risk factors such as smoking and sedentary lifestyle were included. It is understood that the relationship between the anthropometric measures and such risk factors is complex. In addition, many of the risk factors are interrelated, and confound the relationship between abdominal fat distribution and other cardiovascular risk factors. For example, smoking is positively associated with sedentary lifestyle, diabetes and high cholesterol, and inversely associated with high blood pressure.33 Smoking is reported to double the risk of ischemic heart disease for a person with one other risk factor and quadruple the risk when a second additional risk factor is present.34 Smoking has been inversely associated with BMI but positively associated with central adiposity in men35,36 and women.35,37 In this study, smokers were generally found to have a lower mean WC and BMI. A slightly higher mean WHR was seen in smokers in many of the age groups for both men and women.
The site of waist measurement in this study was the point of noticeable waist narrowing, which may have resulted in lower WC cutoff values than might be obtained using other common sites of measurement. While the WHO Expert Committee on Physical Status recommends measurement midway between the lower rib and the iliac crest,23 the NHANES III guidelines38 prescribe use of a point just above the right ilium, and the recommendation of the North American Association for the Study of Obesity (NAASO) and the National Heart, Lung, and Blood Institute (NHLBI)39 is to use the right iliac crest. The lack of a standard measurement for WC is unfortunate, and makes comparison with other studies difficult. It is believed that the use of narrowest waist measurement offers greater ease of acceptance and interpretation by the public and may facilitate self-measurement in addition to clinical use. While it is suggested that a standardized body location is necessary to obtain reliable measures of abdominal circumference,38 it is thought that location of bony landmarks may be difficult for both patients and clinicians.
The sampling process used in this study was complex, and although means were weighted and standard errors could be computed using the jackknife method, special macros were not designed for the chi-square statistic. Some accuracy may be lost in the determination of McNemar's chi-square statistic for comparison of the predictive ability of the different anthropometric measures.
It has been reported that the association between WC and risk factors for cardiovascular disease may be population-dependent.26 Although there was a large number of subjects in this study, only five of the Canadian provinces from the original sample are included. While regional differences exist in the prevalence of obesity and risk factors, there is no reason to believe that this group of individuals differs with respect to the association between the anthropometric cut-offs and risk factor prevalence. Unfortunately, data were not available with respect to ethnic origin, however, the majority of the participants in the survey were Caucasian. Further research is necessary to determine population-specific cut-off points before generalizations may be made to populations that are more diverse.40
The objective of this study was to present a simplified approach to predicting cardiovascular risk in the general population. Ideally, it would be most advantageous to determine the relationship between these anthropometric cut-off points and coronary events or other health outcomes. Similar to other studies supporting the use of WC as a predictor of cardiovascular risk, the current research has used cross-sectional rather than prospective data. However, in a 7-y prospective study, WC has been found the best predictor of diabetes.41 Future research in this area is warranted. In the meantime, public health policy recommending the use of cut-off points for WC might be beneficial in prevention and management of these intermediary risk factors. Family physicians and other health care providers should incorporate the measurement of WC into routine clinical examinations or screenings. Patients should be advised of the health risks associated with a high waist measurement and the benefits of waist reduction. While providing another means by which individuals may be labeled based on their body size and shape, promotion of WC measurement must be sensitive to issues related to body dissatisfaction and eating disorders. Global awareness of the health risks associated with a large WC should be promoted at the community level, but with appropriate guidelines for interpretation and management.
References
World Health Organization . Obesity epidemic puts millions at risk from related diseases Press Release WHO/46 (Online) June 12 1997; www.who.int/inf-prp1997/en/pr97-46.html.
Berg FM . Health risks of obesity: 1993 special report. In: Hettinger ND (ed) Obesity and health. Healthy Living Institute, c 1992.
Macdonald SM, Reeder BA, Chen Y, Despres JP . Obesity in Canada: a descriptive analysis. Canadian Heart Health Surveys Research Group Can Med Assoc J 1997 157 (Suppl 1): S3–S9.
Joffres MR, Hamet P, Rabkin SW, Gelskey D, Hogan K, Fodor G . Prevalence, control and awareness of high blood pressure among Canadian adults. Canadian Heart Health Surveys Research Group Can Med Assoc J 1992 146: 1997–2005.
Connelly PW, MacLean DR, Horlick L, O'Connor B, Petrasovits A, Little JA . Plasma lipids and lipoproteins and the prevalence of risk for coronary heart disease in Canadian adults. Canadian Heart Health Surveys Research Group Can Med Assoc J 1992 146: 1977–1987.
MacDonald S, Joffres MR, Stachenko S, Horlick L, Fodor G . Multiple cardiovascular disease risk factors in Canadian adults. Canadian Heart Health Surveys Research Group Can Med Assoc J 1992 146: 2021–2029.
World Health Organization . Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity, 3–5 June 1997, WHO/NUT/NCD/98.1 WHO: Geneva 1997.
Larsson B, Svardsudd K, Welin L, Wilhelmsen L, Bjorntorp P, Tibblin G . Abdominal adipose tissue distribution, obesity and risk of cardiovascular disease and death: 13-y follow-up of participants in the study of the men born in 1913 Br Med J 1984 288: 1401–1404.
Lapidus L, Bengtsson C, Larsson B, Pennert K, Rybo E, Sjostrom L . Distribution of adipose tissue and risk of cardiovascular disease and death: a 12-y follow-up of participants in the population study of women in Gothenburg, Sweden Br Med J 1984 289: 1257–1260.
Ledoux M, Lambert J, Reeder BA, Despres JP . A comparative analysis of weight to height and waist to hip circumference indices as indicators of the presence of cardiovascular disease risk factors. Canadian Heart Health Surveys Research Group Can Med Assoc J 1997 157 (Suppl 12): S32–S38.
Reeder BA, Senthilselvan A, Despres JP, Angel A, Liu L, Wang H, Rabkin SW . The association of cardiovascular disease risk factors with abdominal obesity in Canada. Canadian Heart Health Surveys Research Group Can Med Assoc J 1997 157 (Suppl 1): S39–S45.
Seidell JC, Cigolini M, Charzewska J, Ellsinger BM, di Biase G . Fat distribution in European women: a comparison of anthropometric measurements in relation to cardiovascular risk factors Int J Epidemiol 1990 19: 303–308.
Seidell JC, Cigolini M, Charzewska J, Ellsinger BM, Deslypere JP, Cruz A . Fat distribution in European men: a comparison of anthropometric measurements in relation to cardiovascular risk factors Int J Obes Relat Metab Disord 1992 16: 17–22.
Ledoux M, Lambert J, Reeder BA, Despres JP . Correlation between cardiovascular disease risk factors and simple anthropometric measures. Canadian Heart Health Surveys Research Group Can Med Assoc J 1997 157 (1 Suppl): S46–S53.
Lemieux S, Prud'homme D, Bouchard C, Tremblay A, Despres JP . A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue Am J Clin Nutr 1996 64: 685–693.
Lean ME, Han TS, Morrison CE . Waist circumference as a measure for indicating need for weight management Br Med J 1995 311: 158–161.
Han TS, van Leer EM, Seidell JC, Lean ME . Waist circumference action levels and the identification of cardiovascular risk factors: prevalence in a random sample Br Med J 1995 311: 1401–1405.
Criqui MH, Barrett-Connor E, Holdbrook MJ, Austin M, Turner JD . Clustering of cardiovascular disease risk factors Prev Med 1980 9: 525–533.
Shaper AG, Pocock SJ, Walker M, Phillips AN, Whitehead TP, Macfarlane PW . Risk factors for ischaemic heart disease: the prospective phase of the British Regional Heart Study J Epidemiol Community Health 1985 39: 197–209.
Levy D, Wilson PW, Anderson KM, Castelli WP . Stratifying the patient at risk from coronary heart disease: new insights from the Framingham Heart Study Am Heart J 1990 119: 712–717.
Wilhelmsen L . Synergistic effects of risk factors Clin Exper Hypertens A 1990 12: 845–863.
MacLean DR, Petrasovits A, Nargundkar M, Connelly PW, MacLeod E, Edwards A, Hessel P . Canadian heart health surveys: a profile of cardiovascular risk. Survey methods and data analysis Can Med Assoc J 1992 146: 1969–1974.
WHO Expert Committee on Physical Status . The use and interpretation of anthropometry. Report of a WHO Expert Committee World Health Organization: Geneva 1995.
Egger G . The case for using waist to hip ratio measurements in routine medical checks Med J Aust 1992 156: 280–285.
Pouliot MC, Despres JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, Nadeau A, Lupien PJ . Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women Am J Cardiol 1994 73: 460–468.
Molarius A, Seidell JC . Selection of anthropometric indicators for classification of abdominal fatness—a critical review Int J Obes Relat Metab Disord 1998 22: 719–727.
Hsieh SD, Yoshinaga H . Abdominal fat distribution and coronary heart disease risk factors in men—waist/height ratio as a simple and useful predictor Int J Obes Relat Metab Disord 1995 19: 585–589.
Han TS, Seidell JC, Currall JE, Morrison CE, Deurenberg P, Lean ME . The influences of height and age on waist circumference as an index of adiposity in adults Int J Obes Relat Metab Disord 1997 21: 83–89.
Han TS, van Leer EM, Seidell JC, Lean ME . Waist circumference as a screening tool for cardiovascular risk factors: evaluation of receiver operating characteristics (ROC) Obes Res 1996 4: 533–547.
Despres JP, Prud'homme D, Pouliot MC, Tremblay A, Bouchard C . Estimation of deep abdominal adipose-tissue accumulation from simple anthropometric measurements in men Am J Clin Nutr 1991 54: 471–477.
Joffres MR, Ghadirian P, Fodor JG, Petrasovits A, Chockalingam A, Hamet P . Awareness, treatment, and control of hypertension in Canada Am J Hypertens 1997 10: 1097–1102.
Gifford RW Jr . New hypertension guidelines set aggressive goals based on risk factors. Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure Cleve Clin J Med 1998 65: 18–24.
Stachenko SJ, Reeder BA, Lindsay E, Donovan C, Lessard R, Balram C . Smoking prevalence and associated risk factors in Canadian adults Can Med Assoc J 1992 146: 1989–1996.
Joffres MR, MacLean DR, O'Connor BA, Petrasovits A, Stachenko S (eds) . Canadians and heart health: reducing the risk (Catalogue no. H39-328/1995E) Ministry of National Health and Welfare: Ottawa 1995.
Barrett-Connor E, Khaw KT . Cigarette smoking and increased central adiposity Ann Intern Med 1989 111: 783–787.
Shimokata H, Muller DC, Andres R . Studies in the distribution of body fat III. Effects of cigarette smoking JAMA 1989 261: 1169–1173.
Lissner L, Bengtsson C, Lapidus L, Bjorkelund C . Smoking initiation and cessation in relation to body fat distribution based on data from a study of Swedish women Am J Public Health 1992 82: 273–275.
Chumlea NC, Kuczmarski RJ . Using a bony landmark to measure waist circumference J Am Diet Assoc 1995 95: 12.
National Heart, Lung and Blood Institute . The practical guide: identification, evaluation, and treatment of overweight and obesity in adults (Online), June 1998 www.nhlbi.nih.gov/guidelines/obesity/practgde.htm
Molarius A, Seidell JC, Sans S, Tuomilehto J, Kuulasmaa K . Varying sensitivity of waist action levels to identify subjects with overweight or obesity in 19 populations of the WHO MONICA Project J Clin Epidemiol 1999 52: 1213–1224.
Wei M, Gaskill SP, Haffner SM, Stern MP . Waist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans—a 7-y prospective study Obes Res 1997 5: 16–23.
Acknowledgements
We wish to acknowledge other members of the Canadian Heart Health Research Group: Dr Christopher Balram from the Department of Health and Community Services, Fredericton NB; Lynne Blair from the BC Ministry of Health, Victoria; Dr David Butler-Jones from Saskatchewan Health, Regina, Saskatchewan; Dr Roy Cameron from the University of Waterloo, Waterloo; Dr Ruth Collins-Nakai from the University of Alberta, Edmonton; Dr Philip W Connelly from St Michael's Hospital and University of Toronto, Toronto; Dr Catherine Donovan, Alison C Edwards and Dr Kevin Hogan, from Memorial University of Newfoundland, St John's; Dr Ron Dyck from Alberta Health, Edmonton; Dale Gelskey and Dr Sharon Macdonald from the University of Manitoba, Winnipeg; Dr Richard Lessard from Public Health Directorate, Montreal; Ella MacLeod from the Prince Edward Island Heart Health Program, Charlottetown; Mukund Nargundkar from Satistics Canada, Ottawa; Dr Brian A O'Connor from the University of British Columbia, Vancouver; Dr Gilles Paradis from McGill University, Montreal; Dr Andres Petrasovits from the Cardiovascular Disease Prevention Unit, Health and Welfare Canada, Ottawa; Dr Bruce A Reeder from the University of Saskatchewan, Saskatoon; Dr Richard Schabas from the Ontario Ministry of Health; Dr Sylvie Stachenko from Health Canada, Ottawa; Dr Lamont Sweet from the PEI Department of Health and Social Services, Charlottetown; and Rosemary White from the Heart and Stroke Foundation of PEI, Charlottetown.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Dobbelsteyn, C., Joffres, M., MacLean, D. et al. A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors. The Canadian Heart Health Surveys. Int J Obes 25, 652–661 (2001). https://doi.org/10.1038/sj.ijo.0801582
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801582
Keywords
This article is cited by
-
A new approach to quantify visceral fat via bioelectrical impedance analysis and ultrasound compared to MRI
International Journal of Obesity (2024)
-
Population-based references for waist and hip circumferences, waist-to-hip and waist-to-height ratios for children and adolescents, and evaluation of their predictive ability
European Journal of Pediatrics (2023)
-
Cut-off points for anthropometric indices to screen for hypertension among Iranian adults of the Bandare-Kong cohort: a cross-sectional study
BMC Public Health (2022)
-
Age-appropriate BMI cut-points for cardiometabolic health risk: a cross-sectional analysis of the Canadian Longitudinal Study on Aging
International Journal of Obesity (2022)
-
An assessment of anthropometric indices and its association with NCDs among the older adults of India: evidence from LASI Wave-1
BMC Public Health (2021)