Abstract
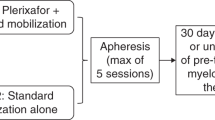
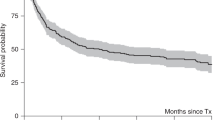
The prognosis for patients with metastatic breast cancer remains poor. Metastatic breast cancer confined to the bones may have a better prognosis, especially hormone receptor-positive disease. We performed a prospective, randomized clinical trial to compare immediate consolidation with high-dose chemotherapy and hematopoietic support versus observation with high-dose consolidation at the time of disease progression in women with metastatic breast cancer and only bone metastases. The patients received chemotherapy with doxorubicin, 5-fluorouracil and methotrexate before randomization. In all, 85 patients were enrolled and 69 were randomized. The median follow-up is 8.1 years from randomization. The median event-free survival (EFS) for the immediate transplant arm is 12 months and for the observation arm is 4.3 months (P<0.0001). The median overall survival for the immediate transplant arm is 2.97 years and for the observation arm 1.81 years, a difference that is not statistically significant. Immediate high-dose chemotherapy and radiation therapy as consolidation offers a clinically and statistically significant improvement in EFS compared with radiation therapy alone following induction chemotherapy for women with metastatic breast cancer confined to the bones.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chu KC, Tarone RE, Kessler LG, Ries LA, Hankey BF, Miller BA et al. Recent trends in US breast cancer incidence, survival and mortality rates. J Nat Cancer Inst 1996; 88: 1571–1579.
Scheid V, Buzdar AU, Smith TL, Hortobagyi GN . Clinical course of breast cancer patients with osseous metastases treated with combination chemotherapy. Cancer 1986; 58: 2589–2593.
Coleman RE, Rubens RD . The clinical course of bone metastases from breast cancer. Br J Cancer 1987; 55: 61–66.
Dunphy FR, Spitzer G, Buzdar AU, Hortobagyi GN, Horwitz LJ, Yau JC et al. Treatment of estrogen receptor negative or hormonally refractory breast cancer with double high-dose chemotherapy intensification and bone marrow support. J Clin Oncol 1990; 8: 1207–1216.
Antman KA, Rowlings PA, Vaughan WP, Pelz CJ, Fay JW, Fields KK et al. High dose chemotherapy with autologous hematopoietic stem cell support for breast cancer in North America. J Clin Oncol 1997; 15: 1870–1879.
Elias AD, Ibrahim J, Richardson P, Avigan D, Joyce R, Reich E et al. The impact of induction duration and the number of high-dose cycles on the long-term survival of women with metastatic breast cancer treated with high-dose chemotherapy with stem cell rescue: an analysis of sequential phase I/II trials from the Dana Farber/Beth Israel STAMP program. Biol Blood Marrow Transplant 2002; 8: 198–205.
Rowlings PA, Williams SF, Antman KH, Fields KK, Fay JW, Reed E et al. Factors correlated with progression-free survival after high-dose chemotherapy and hematopoietic stem cell transplantation for metastatic breast cancer. JAMA 1999; 282: 1335–1343.
Peters WP, Jones RB, Vredenburgh JJ, Sphall EJ, Hussein A, Elkordy M et al. A large, prospective, randomized trial of high dose combination alkylating agents (CPB) with autologous cellular support (ABMS) as consolidation for patients with metastatic breast cancer achieving complete remission after intensive doxorubicin-based induction therapy (AFM). Br Cancer Res Treat 1996; 37 (Suppl): 11 (abstract no. 35).
Biron P, Durand M, Delozier T, Roche T, Battista C, Fargeot P et al. High dose Thiotepa (TTP), cyclophosphamide (CPM) and stem cell transplantation after 4 FEC 100 compared with 4 FEC alone allowed a better disease free survival but the same overall survival in first line chemotherapy for metastatic breast cancer. Results of the PEGASE 03 French Protocole. Proc ASCO 2002; 21: 42a (abstract no. 167).
Crump M, Gluck S, Stewart M, Levine M, Pritchard K, Kirkbride P et al. A randomized trial of high-dose chemotherapy (HDC) with autologous peripheral blood stem cell support (ASCT) compared to standard therapy in women with metastatic breast cancer: a National Cancer Institue of Canada (NCIC) Clinical Trials Group study. Proc ASCO 2001; 20: 21a (abstract no. 82).
Pedrazzoli P, Ferrante P, Kulekci A, Schiavo R, DeGiorgi U, Carminati O et al. Autologous hematopoietic stem cell transplantation for breast cancer in Europe: critical evaluation of data from the European Group for Blood and Marrow Transplantation (EBMT) Registry 1990–1999. Bone Marrow Transplant 2003; 32: 489–494.
Stadtmauer EA, O'Neill A, Goldstein LJ, Crilley PA, Mangan KF, Ingle JW et al. Conventional-dose chemotherapy compared with high-dose chemotherapy plus autologous hematopoietic stem-cell transplanation for metastatic breast cancer. NEJM 2000; 342: 1069–1076.
Jones RB, Shpall EJ, Shogan J, Olsen GA, Bast RC, Gockerman JP et al. The Duke AFM program: intensive induction chemotherapy for metastatic breast cancer. Cancer 1990; 66: 431–436.
Peters WP, Shpall EJ, Jones RB, Oslen GA, Bast RC, Gockerman JP et al. High dose combination alkylating agents with bone marrow support as initial treatment for metastatic breast cancer. J Clin Oncol 1988; 6: 1368–1376.
Vandemark RM, Shpall EJ, Affronti ML . Bone metastases from breast cancer: value of bone windows. J Comput Assist Tomography 1992; 16: 608–614.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Petros WP, Broadwater G, Berry D, Jones RB, Vredenburgh JJ, Gilbert CJ et al. Association of high-dose cyclophosphamide, cisplatin and carmustine pharmacokinetics with survival, toxicity and dosing weight in patients with primary breast cancer. Clin Cancer Res 2002; 8: 698–705.
Berry DA, Broadwater G, Klein JP, Antman K, Aisner J, Bitran J et al. High-dose versus standard chemotherapy in metastatic breast cancer: comparison of Cancer and Leukemia Group B trials with data from the Autologous Blood and Marrow Transplant Registry. J Clin Oncol 2002; 20: 743–750.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vredenburgh, J., Madan, B., Coniglio, D. et al. A randomized phase III comparative trial of immediate consolidation with high-dose chemotherapy and autologous peripheral blood progenitor cell support compared to observation with delayed consolidation in women with metastatic breast cancer and only bone metastases following intensive induction chemotherapy. Bone Marrow Transplant 37, 1009–1015 (2006). https://doi.org/10.1038/sj.bmt.1705367
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1705367
Keywords
This article is cited by
-
Therapeutic utility of engineered myeloid cells in the tumor microenvironment
Cancer Gene Therapy (2023)
-
Long-term survival in a fraction of patients with metastatic breast cancer who received consolidation therapy with high-dose chemotherapy and autologous stem cell transplant between 2000 and 2015: an EBMT registry-based study
Bone Marrow Transplantation (2022)
-
Secondary malignancies following high dose therapy and autologous hematopoietic cell transplantation-systematic review and meta-analysis
Bone Marrow Transplantation (2015)
-
Improvement of survival and prospect of cure in patients with metastatic breast cancer
Breast Cancer (2012)
-
Interleukin-2 and granulocyte–macrophage–colony-stimulating factor immunomodulation with high-dose chemotherapy and autologous hematopoietic stem cell transplantation for patients with metastatic breast cancer
International Journal of Hematology (2009)