Abstract
Study design:
Biomechanical study using finite element model (FEM) of lumbar spine.
Objectives:
Very high coincidence of spina bifida occulta (SBO) has been reported more than in 60% of lumbar spondylolysis. The altered biomechanics due to SBO is one considerable factor for this coincidence. Thus, in this study, the biomechanical changes in the lumbar spine due to the presence of SBO were evaluated.
Setting:
United States of America (USA).
Methods:
An experimentally validated three-dimensional nonlinear FEM of the intact ligamentous L3-S1 segment was used and modified to simulate two kinds of SBO at L5. One model had SBO with no change in the length of the spinous process and the other had a small dysplastic spinous process. Von Mises stresses at pars interarticularis were analyzed in the six degrees of lumbar motion with 400 N axial compression, which simulates the standing position. The range of motion at L4/5 and L5/S1 were also calculated.
Results:
It was observed that the stresses in all the models were similar, and there was no change in the highest stress value when compared to the intact model. The range of motion was also similar in all the models. The lumbar kinematics of SBO was thus shown to be similar to the intact model.
Conclusion:
SBO does not alter lumbar biomechanics with respect to stress and range of motion. The high coincidence of spondylolysis in spines with SBO may not be due to the mechanical factors.
Similar content being viewed by others
Introduction
Spinal dysraphysm is a congenital anomaly of the spinal column. Spina bifida occulta (SBO) is one such anomaly in which an unfused or split spinous process is seen. The incidence of SBO has been reported to be as high as 20% in the general population, and it is more likely to occur at the L5 or S1 level.1 SBO rarely causes serious primary neurologic defects, and is therefore clinically considered to be very benign; however, it seems to be commonly associated with lumbar spondylolysis.2, 3, 4, 5 Spondylolysis is defined as a stress fracture at the pars interarticularis.6, 7, 8, 9 Oakley and Carley4 reported a 67% incidence of the lesion (SBO) among the spondylolytic population. Although several reports suggest that these two lumbar disorders often coexist, no investigations have been carried out to prove why they are correlated.
Two possibilities that could explain the coexistence of spondylolysis and SBO are:
-
1
The SBO may alter the spine biomechanics; for example, the stresses at the pars interarticularis may increase after the SBO occurs (mechanical factor).
-
2
The genetic predispositions producing these two disorders may affect each other (genetic factor).
The purpose of this study was to investigate the mechanical factor using the finite element approach to compare the stress distributions in a spinal segment with and without the SBO anomaly.
Methods
Finite element model
An experimentally validated three-dimensional nonlinear finite element model (FEM) of the intact ligamentous L3-S1 segment was used. This model has been previously used to investigate a number of clinically relevant issues.7, 8, 10, 11, 12, 13 The model validation has been well documented in these studies. The following is the brief description of the model used in this study.
The geometric data of the L3-S1 motion segment were obtained from CT scans (transverse slices, 1.5 mm thick) of a normal cadaveric ligamentous lumbar spine specimen. Sequentially stacked, digitized cross-sectional data provided the means to generate the model. The commercial software ABAQUS 6.4 (ABAQUS Inc., Pawtucket, RI, USA) was used to construct and analyze the model. The cortical and cancellous bone regions were constructed with three-dimensional hexagonal elements (C3D8), which were assigned different material properties. Eight nodes define such an element, with each node possessing three degrees of freedom. The facet joints were simulated with three-dimensional gap contact elements (GAPUNI), simulating the physiologic nature of the cartilaginous layer lining the articular surface. These elements transferred force between nodes along a single direction as a specified gap between these nodes closed. The elements were able to transmit only compression. The intervertebral disk was modeled as a composite of a solid matrix with embedded fibers oriented at ±30° to the horizontal (via the REBAR parameter) in concentric rings around a pseudo-fluid nucleus. The hydrostatic properties of the nucleus were simulated with C3D8 hexagonal elements assigned a very low stiffness (1 MPa) and near incompressibility (n=0.4999). All seven major spinal ligaments (interspinous, supraspinous, intertransverse, posterior longitudinal, capsular, anterior longitudinal, and ligamentum flavum) were represented as elastic truss elements and assigned nonlinear material properties. Naturally changing ligament stiffness (initially low stiffness at low strains followed by increasing stiffness at higher strains) was simulated through the ‘hypoelastic’ material designation, which allowed the definition of the axial stiffness as a function of axial strain. Three-dimensional 2-node truss elements (T3D2) were used to construct the ligaments.
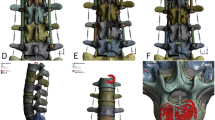
SBO was simulated by modifying the spinous process (unfused) of the intact model. Cracks of 1.0 mm were created at the middle of the spinous process to simulate SBO (SBO model, Figure 1). Sometimes SBO is seen with a small and dysplastic spinous process. Thus, we also simulated the unfused spinous process in the dysplastic small spinous process (Dys-SBO model, Figure 2). Actually, the severity of the dyplasticity of the spinous process varies individually. It is impractical to simulate all of the possible variations in an FEM, although these can be done. In this study, we simulated a spinous process that is of 25% of the intact length.
Analysis
Von Mises stresses at ventral and dorsal pars interarticularis at the affected level (L5) were analyzed in flexion, extension, lateral bending and axial rotation for a moment of 10.6 Nm. A 400 N preaxial compression was applied to simulate the body weight. The stress results from the two SBO models were compared to the intact model.
The range of motion at the affected levels, which were L4/5 and L5/S1, were also calculated for all three models, and the effect of SBO on the motion of L5 was evaluated.
Results
The stresses at the ventral wall of right pars at L5 in the intact model were 9.4, 25.9, 3.7, 1.6, 3.8 and 10.6 MPa for flexion, extension, right bending, left bending, right rotation and left rotation, respectively (Table 1). Corresponding stresses at the dorsal wall were 8.9, 22.2, 6.1, 2.2, 6.9 and 19.7 (Table 2). In the SBO and Dys-SBO models, the stresses values in all degrees of motion, except flexion, were very similar to the intact stresses (Tables 1 and 2). In flexion, the maximum stress at the ventral wall of the pars interarticularis was 9.4, 7.9 and 6.2 MPa for the intact, SBO and Dys-SBO model, respectively. Correspondingly, the stresses at the dorsal wall were 8.9, 8.8, and 6.2. The maximum stresses in the SBO models were lesser than the intact model. In extension, the maximum stress values were equal in all the models at the ventral wall of pars. At the dorsal side of pars, there was a slight increase (<0.5 MPa) in the models with SBO when compared to the intact. In rotation and bending, the change in stress values was similar to the intact stresses. The highest stress (25.9 MPa) was equal in all three models and was seen at the ventral pars during extension.
The ranges of motion at L4/5 in all three models (Figure 3) and L5/S1 (Figure 4) were similar. When compared to the intact model, the flexion at the L4/5 segment in the Dys-SBO model showed a slight increase (0.9°) in motion. In rotation at L5/S1 segment, a slight increase (0.2°) in motion in the dys-SBO model with respect to intact motion was noted.
Discussion
In the present study, we evaluated the biomechanical changes seen due to unfused spinous process (SBO). The occurrence of SBO and spondylolysis together could be due to genetic factors and/or biomechanical factors, as hypothesized in the Introduction section. There seems to be a need to see the effects of SBO on the kinematics of the spine; however, there have been no biomechanical investigations conducted until now.
The biomechanical behavior of spines can be studied by
-
1
Three-dimensional analysis using fresh cadaveric spines.12, 14, 15, 16
-
2
Finite element analyses using a mathematical mode.7, 8, 10, 11, 12, 13
Since the availability of fresh cadaveric specimens with SBO is limited, using an FEM appeared to be the best option to study the biomechanical effects of SBO.
This study was conducted to investigate whether SBO produces higher stresses at the pars interarticularis due to SBO, which, in turn, could lead to spondylolysis (stress fracture at the pars interarticularis). SBO was simulated using an FEM of the intact lumbar spine. This FEM study reveals that there does not appear to be any significant increase in stresses due to SBO when compared to the intact model. The highest stress value was found in extension, and it was shown to be the same among the three models (25.9 MPa). Furthermore, the range of motion at the segments in all models (L4/5 and L5/S1) was very similar. Thus, in terms of highest stress and range of motion, this study showed that SBO does not significantly alter the lumbar kinematics of the intact spine. These data do not support the hypothesis that the altered mechanics in the SBO spine may cause an increase in stress in the pars, leading to a high incidence of the pars fractures. We can state from this study that the high incidence of spondylolysis in spines with SBO may most likely be due to genetic factors and not mechanical factors.
In this study, Dys-SBO was simulated at L5 as small dysplastic (25% in length) spinous processes. In the results, the highest stress during lumbar motion was 25.9 MPa and it was equal to the other two models. Angular deformity was also similar to the other two models. These results revealed that even though the SBO occurred at the small dysplastic spinous process, the lumbar kinematics did not show any change with respect to the intact case. Clinically, there are some variations in the length of the spinous process. However, it is impractical to simulate all of the possible variations, although theoretically it can be done. From a clinical perspective, the worst-case scenario, which is the complete absence of the spinous process (un-fused lamina), is very rare. However, most of the cases with spondylolysis and SBO have part of the spinous process. Thus, we simulated the case of 25% in length of the spinous process as a worst-case scenario in this study.
Limitation of this study was validation of our SBO FEM. The best way to validate this model is a comparison with motion analysis data using fresh cadaveric spines with SBO. However, to get such spines is very difficult; thus, the comparison is not practical. The SBO model in this study was modification of the intact model. The intact model was previously used for numerous clinical issues and was already experimentally validated.7, 8, 10, 11, 12, 13 The other limitation of our model is the bony age. Most spondylolysis appears in childhood, and the FEM should be simulated using pediatric spines with growth plates and apophyseal rings, which is very challenging to create. Actually, in the literature, there are no reports on pediatric FEMs. If we need to analyze anterior segments such as disc and vertebral body, this anatomical difference is crucial. In this study, we analyzed posterior elements such as pars interarticularis, which is not anatomically different between children and adults. Thus, to use an adult model for the analysis of pars interarticularis may not be crucial. However, the ideal model for this study is using the pediatric spine model; therefore, we have initiated the creation of the pediatric lumbar spine model.17
As for the genetic contribution of SBO on occurrence of spondylolysis, there have been no studies in the literature. Recently, Ucar et al18 reported the significant coexistence of patients with SBO and dysplasia of the hip joint. They did not conduct any genetic studies; however, it can be assumed that the patients with SBO may have a genetic weakness in the ossification or bone metabolism. Likewise, the patients with SBO may be likely to have stress fractures. The SBO has some coexisting skeletal disorders. Recently, the genetic approaches to clarify the unfused neural canal have been conducted.19, 20 Further detailed genetic research for SBO can also clarify the genetic predisposition of coexisting disorders such as spondylolysis.
In conclusion, the lumbar kinematics of SBO was shown to be similar to the intact spine. Thus, the high coincidence of spondylolysis in spines with SBO may not be due to the mechanical factors. Genetic research of SBO and spondylolysis will be required to clarify the coexistence of these two disorders.
References
Ganey TM, Ogden JA . Development and maturation of the axial skeleton. In: Weinstein SL (ed). The Pediatric Spine. 2nd edn. Lippincott Williams & Wilkins: Philadelphia, PA 2001, pp 3–54.
Albanese M, Pizzutillo PD . Family study of spondylolysis and spondylolisthesis. J Pediatr Orthop 1982; 2: 496–499.
Fredrickson BE et al. The natural history of spondylolysis and spondylolisthesis. J Bone Jt Surg [Am] 1984; 66: 699–707.
Oakley RH, Carty H . Review of spondylolisthesis and spondylolysis in paediatric practice. Br J Radiol 1984; 57: 877–885.
Seitsalo S et al. Progression of spondylolisthesis in children and adolescents. A long-term follow-up of 272 patients. Spine 1991; 16: 417–421.
Sairyo K et al. Three successive stress fractures at the same vertebral level in an adolescent baseball player. Am J Sports Med 2003; 31: 606–610.
Sairyo K et al. Athletes with unilateral spondylolysis are at risk of stress fracture at the contra-lateral pedicle and pars interarticularis: a clinical and biomechanical study. Am J Sports Med 2005; 33: 583–590.
Sairyo K et al. MRI signal changes of the pedicle as an indicator for early diagnosis of spondylolysis in children and adolescents. A clinical and biomechanical study. Spine (in press).
Wiltse LL, Wildell Jr EH, Jackson DW . Fatigue fracture. The basic lesion in isthmic spondylolisthesis. J Bone Jt Surg [Am] 1975; 57: 17–22.
Goel VK et al. Effects of rigidity of an internal fixation device – a comprehensive biomechanical investigation. Spine 1991; 16(Suppl.): S155–S161.
Goel VK et al. Interlaminar shear stresses and laminae separation in a disc: finite element analysis of the L3-4 motion segment subjected to axial compressive loads. Spine 1995; 20: 689–698.
Konz RJ et al. The pathomechanics of spondylolytic spondylolisthesis in immature primate lumbar spines – in vitro and finite element studies. Spine 2001; 26: E38–E49.
Sairyo K et al. Biomechanical rationale of endoscopic decompression for lumbar spondylolysis as an effective minimally invasive procedure – a study based on the finite element analysis. Minimally Invasive Neurosurg 2005; 48: 119–122.
Kajiura K et al. Slippage mechanism of pediatric spondylolysis: biomechanical study using immature calf spines. Spine 2001; 26: 2208–2212.
Kuroki H et al. Contributions of flexion-extension cyclic loads to the lumbar spinal segment stability following different discectomy procedures. Spine 2004; 29: E39–E46.
Sairyo K et al. The pathomechanism of isthmic lumbar spondylolisthesis. A biomechanical study in immature calf spines. Spine 1998; 23: 1442–1446.
Sairyo K et al. Three dimensional finite element analysis of the pediatric lumbar spine: Part I: Pathomechanism of apophyseal bony ring fracture. Eur Spine J (in press).
Ucar DH et al. Occult spinal dysraphism and its association with hip dysplasia in females. Int Orthop 2003; 27: 70–72.
Harris MJ, Juriloff DM . Mini-review: toward understanding mechanisms of genetic neural tube defects in mice. Teratology 1999; 60: 292–305.
Payne J, Shibasaki F, Mercola M . Spina bifida occulta in homozygous patch mouse embryos. Dev Dyn 1997; 209: 105–116.
Acknowledgements
This work was supported in part by a fellowship grant from DePuy Spine, Inc., Raynham, MA, USA.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sairyo, K., Goel, V., Vadapalli, S. et al. Biomechanical comparison of lumbar spine with or without spina bifida occulta. A finite element analysis. Spinal Cord 44, 440–444 (2006). https://doi.org/10.1038/sj.sc.3101867
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101867
Keywords
This article is cited by
-
Investigating the landscape and trajectory of spina bifida research in Asia: a bibliometric analysis
Child's Nervous System (2022)
-
Spinal dysraphism at the Syrian Neolithic site of Dja’de el-Mughara
Archaeological and Anthropological Sciences (2018)
-
Two types of laminolysis in adolescent athletes
Journal of Orthopaedics and Traumatology (2012)
-
Adolescents with symptomatic laminolysis: report of two cases
Journal of Orthopaedics and Traumatology (2010)
-
Incidence and etiology of lumbar spondylolysis: review of the literature
Journal of Orthopaedic Science (2010)