Key Points
-
The use of resin composite materials had increased in the five years preceding the survey in 62% of practices.
-
Regarding choice of materials, clinical indications was an important factor, but patients' aesthetic demands were also highly relevant.
-
Half of the respondents place large composite restorations in posterior teeth.
Abstract
Objective This study determined the reasons for dentists' choice of materials, in particular amalgam and resin composite, in Great Britain.
Method A questionnaire was developed to elicit this information. The names and addresses of 1,000 UK-based dentists were selected at random. The questionnaire was mailed to these dentists with an explanatory letter and reply-paid envelope.
Results Six hundred and fifty four replies were received. Regarding choice of material, 100% of respondents cited clinical indication as the most influential factor, although patients' aesthetic demands (99%), patients' choice (95%) and patients' financial situation (92%) were also reported to influence respondents' choice. Thirty-five per cent of respondents used composite 'sometimes', 15% 'often', and 1% 'always' in extensive load-bearing cavities in molar teeth. For composite restorations in posterior teeth, 92% 'always', 'often' or 'sometimes' used the total etch technique and 53% never used rubber dam. Seventy per cent of respondents agreed with the statement 'discontinuation of amalgam restricts a dentist's ability to adequately treat patients'. Eighty-one per cent considered that the growth in the use of composites increased the total cost of oral healthcare.
Conclusions Forty nine per cent of the respondents from England and Wales seldom or never place large composite restorations in molar teeth. Their choice of material is influenced greatly by clinical indications, and patients' aesthetic demands.
Similar content being viewed by others
Introduction
At the start of a new century, dentists in the developed world are predominantly using a material for the restoration of posterior teeth which they used at the start of the previous century, namely, amalgam, despite the considerable advances which have been made in alternative materials over the past two decades. In this respect, in the United States, amalgam was recently considered to be the most commonly used posterior tooth restorative material.1 However, there are indications of a shift away from the use of amalgam, principally because of patient concerns about the use of a mercury-containing filling material and partly because patients' assessment of dental aesthetics appears to indicate that a proportion of the population are unhappy with the colour of the restorations in their teeth.2 Accordingly, it may be considered that provision of tooth-coloured restorations will be increasingly demanded. Nevertheless, amalgam restorations may provide good longevity3 and involve less technique sensitivity in their placement than the alternatives. Composite materials in particular have been considered demanding to place in posterior teeth, principally in respect of counteracting the problems of polymerisation contraction4 and the achievement of a satisfactory contact area in Class II restorations.5 It may be considered that the introduction of new matrix systems and the development of packable, non-stick materials may assist in overcoming the problems of achieving a correctly-contoured contact area. Regarding polymerisation contraction, it is encouraging to note the testing of resins with reduced polymerisation shrinkage by Eick et al.6 Craig et al.7 and Palin and co-workers,8 but no resin-based composite materials which are truly low-shrink are commercially available at the time of writing. Other problems, such as the poor wear resistance of early composite materials, appear largely to have been overcome,9 with a reduction in size of filler particles leading to improved polishability and higher filler loading values.
Regarding clinical performance, a meta-analysis of the performance of resin composites in posterior teeth has concluded that 'considering the limited number of studies of variable length available, the results indicate generally high clinical performance of the various posterior composites for the outcomes analyzed'.10 These workers added that 'with the development of more advanced formulations of posterior composite materials and more advanced technology for polymerisation and placement, the performance of posterior composite restorations will continue to improve'. The suggested indications for resin-based composite (RBC) restorations in posterior teeth have been expanded by the American Dental Association to include pit and fissure sealing, preventive resin restorations, initial to moderate-sized Class I and II restorations and restorations in patients who are allergic to metals.11
RBCs offer a number of advantages over amalgam in the restoration of posterior teeth. Among these are the ability to achieve an aesthetically pleasing restoration, the need to remove less tooth structure because adhesive technology is being employed, and reduced microleakage (compared with amalgam) by using bonding agents. It has been considered that a growing number of dentists are restricting their practices to the use of RBCs as opposed to amalgam in the US, where in 1995, approximately 20% of intra-coronal restorations were tooth-coloured,1 this proportion rising, by the year 1998, to 47% for single-surface direct-placement restorations and circa 30% for multiple surface restorations.12 Some of these restorations will have been replacements for failed or unaesthetic restorations in dental amalgam. There are trends away from amalgam use in parts of Europe,13,14,15 but there is little evidence to indicate whether this trend is also apparent in the United Kingdom.
It was therefore considered timely and appropriate to assess dentists' attitudes to the use of amalgam and RBCs in the restoration of cavities in posterior teeth in the UK. The information gained from such an assessment will be of value in the planning of dental services and the planning of postgraduate education. For the manufacturers of RBC materials, such information will be of value in directing their future research and development.
Purpose of proposed investigation
It was the purpose of the proposed study to assess dentists' attitudes to and behaviour concerning the use of amalgam and RBCs in the restoration of cavities in posterior teeth. A postal questionnaire was distributed to a representative sample of dentists in the UK.
Materials and Methods
A questionnaire was developed from that used by Widstrom and Forss13 in Finland, to determine dentists' attitudes to the use of amalgam and resin composite, the techniques used and side effects noticed. The questionnaire consisted of both open and structured questions about the treatment needs of patients, choice of restorative materials and the properties and usefulness of different materials, and was piloted among 20 general dental practitioners (GDPs) and amended following receipt of their comments.
One thousand dentists' names and addresses were selected at random from health authority lists in England and health board lists in Scotland. Each of the selected dentists was sent the questionnaire during April/May 2001, along with a stamped addressed envelope and an explanatory letter designed to take cognisance of the principles of Dillman's Total Design Method,16 requesting completion and return of the questionnaire within a one month period. One further mailing was sent to those GDPs who did not respond to the first mailing after a two-month period (copies of the questionnaire are available from the corresponding author on request).
The data contained in the returned questionnaires were entered into a Microsoft Access database and subsequently analysed using Minitab (version 12). Statistical analyses were undertaken of 'early' and 'late' responders with regard to demographics in an attempt to identify any late response bias. Further data analysis involved descriptive statistics and cross-tabulations, with potential associations tested for significance using Chi-square tests and appropriate follow-up multiple comparisons as necessary.
Results
General and demographic data
Replies were received from 512 dentists following the first mailing, and 142 dentists following the second mailing, giving an overall response rate of 65%. Seventy-seven per cent (n=502) of respondents were male. Regarding years since graduation, 37% (n=39) had been graduated for between 11 and 20 years, 44% (n=291) had been graduated for 21 years or more, and the remaining 19% (n=122) for 10 years or fewer. A large majority (73%: n=473) were practice owners and 24% (n=160) were associates. Seventy per cent (n=453) practiced in a group or partnership, the remaining 30% (n=195) practising single-handed.
Regarding practice location, 47% (n=303) of practices were in a city or town centre, 38% (n=247) were in a suburban location and 15% (n=99) in a rural location. Regarding attendance at postgraduate courses, 46% (n=297) of respondents had attended up to five courses in the year preceding the survey, while 33% (n=217) had attended 6 to 10 courses and 18% (n=116) had attended more than 11 courses. Three per cent (n=20) of respondents had attended no courses.
No statistically significant differences were noted between the early and late responders in terms of years graduated, sex, single/group practice and attendance at post-graduate courses. However, there were significantly greater numbers of late responders than early responders in suburban practices. A statistically significant association was noted between time of response and respondents' position, with more early responders being practice owners than late responders (p<001).
Changes in treatment needs and choice of materials
Regarding treatment need, 58% (n=360) of respondents indicated that the need for restorations among their patients had remained stable during the five years preceding the survey, while 4% (n=26) reported an increase in need and 32% (n=195) reported a decrease in the need for restorations.
Fifty per cent (n=319) of respondents reported a decreased use of amalgam over the previous five years and 44% (n=276) reported that their use of amalgam had remained stable. The use of resin composite materials increased in 62% (n=393) of respondents' practices. Glass-ionomer and resin-modified glass-ionomer were shown to have a net increase in use, as too did ceramic inlays, dentine-bonded crowns and implants. The use of gold restorations was found to have decreased and the use of metal-ceramic crowns was stable. Seventy-nine per cent (n=492) of respondents did not prescribe implants, 37% (n=233) did not prescribe dentine-bonded crowns, 25% (n=156) did not prescribe gold inlays and 50% (n=318) did not prescribe ceramic inlays. The complete data is presented in Table 1.
Regarding choice of material, 100% of respondents cited clinical indication as the most influential factor, although patients' aesthetic demands (99% of respondents, n=638), patients' choice (95%, n=608), patients' financial situation (92%, n=591), and lecturers' suggestions (81%, n=507) were also reported to influence respondents' choice of materials. The complete data is presented in Table 2.
Reasons for replacement of restorations
Secondary caries
Secondary caries was the most commonly reported reason for replacement of composite and amalgam restorations, by 87% (n=548) of respondents for composite and 91% (n=583) of respondents for amalgam, with these differences being statistically significantly (p=0.04).
Fractured restoration
The next most frequently reported reason for replacement of amalgam restorations was 'fractured filling', by 90% (n=576) of respondents. By comparison, the figure reported for 'fractured filling' for composite restorations was significantly lower at 79% (n=504) (p<0.01).
Lost restoration
The reason for replacement 'lost restoration' was given by 87% (n=560) of respondents for amalgam restorations. This compares with 72% (n=455) of respondents reporting the reason 'lost restoration' for composite restorations, this difference being statistically significant (p<0.01).
Sensitivity
'Sensitivity' was reported as the reason for replacement of composite restorations by 57% (n=358) of respondents and by 64% (n=405) of respondents for amalgam, a statistically significant difference (p<0.01).
Wear
Wear was reported as the reason for replacement of composite restorations by 72% (n=454) of respondents, while 27% (n=176) of respondents cited this as the reason for replacement for amalgam restorations, this difference being statistically significant (p<0.001).
Pulpal pain
'Pulpal symptoms/pain' as a reason for replacement scored differently for composite and amalgam, with a significantly higher proportion of respondents indicating 'pulpal symptoms' as the reason for replacement for amalgam (75%, n=475) compared with composite (57%, n=358)(p<0.01). There was no difference between amalgam and composite for the reason 'patient's wish'.
Use of composite and techniques employed
When asked how often they placed extensive, occlusion-bearing composite restorations in molar teeth, 1% (n=9) of respondents replied 'always', 15% (n=96) 'often', 35% (n=222) 'sometimes', 42% (n=270) 'seldom' and 7% (n=46) replied 'not at all'.
The most commonly used techniques for placement of composite were as follows:
-
Total etch/dentine bonding, used always, often or sometimes by 92% (n=567) of respondents,
-
Calcium hydroxide in combination with another base by 75% (n=452) of respondents,
-
A thin glass ionomer layer by 66% (n=388) of respondents,
-
A thick glass-ionomer layer ('sandwich restoration') by 65% (n=385) of respondents,
-
A flowable composite 'base' by 45% (n=264) of respondents.
Rubber dam was used for isolation 'always' by 8% (n=49) of respondents, 'often' by 6% (n=38), 'sometimes' by 33% (n=207) and 'never' by 53% (n=327) of respondents. The results were similar for respondents' techniques used in placement of a smaller composite restoration, such as an occlusal, except that the respondents were significantly less likely (p<0.001) to use a thick glass-ionomer layer in such situations.
Influence of demographic factors on use of composite in extensive restorations in molar teeth
Years since graduation
There was evidence of a statistically significant association between use of composite in extensive fillings in posterior teeth and years since graduation (p=0.04). A majority of dentists who had graduated less than 5 years ago either 'sometimes' or 'seldom' used composite. The majority of those who had graduated between 5 to 10 years 'seldom' used composite, while those graduated more than 11 years either 'sometimes' or 'seldom' used composite. There was a significantly smaller percentage of respondents who graduated < 5 years ago who 'never' used composite when compared with dentists in the other age groups. However, in summary, there was no clear trend towards increasing or decreasing composite use with increasing or decreasing years since graduation.
Gender
There was a significant association between gender and the use of composite in extensive restorations in posterior teeth, with a significantly higher proportion of males reporting that they 'always' or 'often' used composite (p = 0.03).
Practice location
While the above differences are apparent, there was no statistical evidence to suggest that practice location (city/town centre, suburban or rural), type (single-handed or group), geographical area, or respondents' pattern of attendance at postgraduate courses had any effect on the use of composite in restorations in molar teeth.
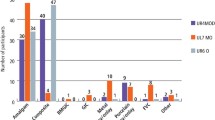
Properties of restorative materials
Respondents were asked to rank the materials amalgam, composite, glass ionomer, RMGI and compomer on a scale of 1 = inadequate to 10 = ideal, for five properties namely: wear resistance, ease of manipulation, value for money for the patient, long term aesthetics and lack of symptoms. The results are presented as mode scores (the number of respondents making the most frequent response) in Figure 1.
Changes following a decreased use of amalgam
Forty per cent (n=242) of respondents considered that secondary caries had increased as a result of decreased use of amalgam, while 46% (n=280) of respondents considered that the need for root fillings had increased. Thirty-nine per cent (n=239) of respondents considered that loss of fillings had increased as a result of decreased amalgam use, although 47% (n=285) considered that this had remained stable. Patient satisfaction with aesthetics of restorations was considered to have improved by 79% (n=490) of respondents as a result of decreased amalgam use, but 82% (n=502) of respondents considered that technical challenges had increased following decreased amalgam use. Allergic problems of dental personnel were considered to have increased by 7% (n=45) of respondents, with 49% (n=301) considering that this had remained stable, and 42% (n=259) stating that they 'did not know'.
Provision of composite restorations
Respondents were asked whether they considered a low-shrink composite to offer any clinical advantage. In response, all but 2% (n=13) agreed with this statement, with 62% (n=393) of respondents offering strong agreement with it. With regard to the respondents' clinical experience, 31% (n=196) agreed with the statement 'it is possible to provide composite restorations with a life-span equal to amalgam', while 53% (n=336) disagreed. Seventy per cent (n=445) of respondents considered that 'discontinuation of the use of amalgam would restrict a dentist's ability to adequately treat patients'. Ninety-three per cent (n=593) of respondents agreed that 'providing composites in posterior teeth was more time-consuming than placing a corresponding amalgam restoration', and 12% (n=78) of respondents agreed with the statement 'I would provide more amalgam restorations if patients would allow it', with 60% (n=376) disagreeing with it. Eighty-one per cent (n=519) of respondents considered that 'the growth in use of composite materials was increasing the total cost of oral healthcare'. Lastly, when asked their opinion of the statement 'the use of amalgam will be discontinued by the year 2005', 14% of respondents agreed with this statement and 63% disagreed with it.
Discussion
It of interest to note that, whilst so much else has changed in the past 100 years, such as transport, dress, buildings, agriculture and food, dentists are still using a version of a material that they used 100 years ago. With the arrival of a new millennium, it therefore seemed appropriate to investigate the reasons for the continued use of amalgam, or failure of alternative materials to become predominant, and at the same time, to evaluate trends in the use of resin-based materials.
The use of questionnaire responses to determine dentists' attitudes and behaviour is common, although not without difficulties such as non-response bias. The response rate to this questionnaire, which was just above the mean response rate (64%) for questionnaires to dentists reported by Tan and Burke,17 could be considered satisfactory. The validity of the sample appears satisfactory as the results correspond closely to the male/female ratio on the Dentists Register.18 However, there is no information regarding the demographics of the non-respondents, and it may be that the respondents have elected to reply because of an interest in the subject. Additionally, the sample of dentists was chosen from health authority/health board lists, so dentists who operate wholly outside the National Health Service (NHS) arrangements will have been excluded from the survey. As composite restorations are not permitted in load-bearing situations in posterior teeth within the NHS General Dental Services, the results may present a bias against posterior composite. However, this is unlikely to be great, as the number of totally private practices without a health authority/board entry has recently been considered to be between 1% and 10%.19.
The demographic results indicated that a high proportion of practitioners are now practicing in a partnership/group arrangement, and that only a small proportion (3%) do not undertake any postgraduate education. Since partnership/group practice arrangements have been considered by Sarll and co-workers20 to facilitate the introduction of innovations into a practice more readily than for single-handed practitioners, it could be assumed that practitioners in a partnership/group arrangement would have been more likely to have introduced new materials into their practices. However, the results of the present study do not support this, possibly because information on new materials and techniques is more readily available today than in 1982, the date of publication of the paper by Sarll and colleagues.20 In this respect, only a small proportion (3%) of respondents admitted no participation in post-graduate education, which may indicate that the respondents had received information on the materials surveyed in this study, but had decided not to adopt composite as a restorative material for posterior teeth in the light of evidence that they had been given. In this respect, current evidence for the use of composite in posterior teeth is positive, with the American Dental Association suggesting that composite is now indicated for moderate-sized class I and II restorations, as well as smaller cavities.11.
An alternative reason for the low uptake of composite in load-bearing cavities may be its lack of availability to patients treated under National Health Service (NHS) regulations. Patients treated within these regulations are able to obtain composite as an alternative to amalgam, but the fee comparisons between NHS amalgam restorations and privately funded composite may be substantial and may therefore act as a disincentive to patients.
Almost one third of respondents indicated that the need for restorations had decreased over the past 5 years, with 58% indicating that need had remained stable. The results (Table 1) indicated a strong, net decrease in amalgam use over the past five years, and this appeared to be balanced by a strong, net increase in the use of composite. Use of glass ionomer and RMGI have also increased. Regarding indirect restorations, the use of metal-ceramic crowns was found to be stable over the past five years, while dentine-bonded crowns and ceramic inlays showed increasing use, although 50% of respondents indicated that they did not use ceramic inlays, and 37% indicated that they did not use dentine-bonded crowns. The adoption of adhesive techniques appears therefore to be less robust for indirect forms of treatment than for direct-placement restorations.
Regarding techniques used during placement of composite restorations in posterior teeth, respondents used total etch/dentine bonding 'sometimes' (18%), 'often' (21%), or 'always' (53%). However, since 45% of respondents used a flowable composite 'base' layer and 66% used a glass-ionomer base, it would appear that total etch was used in combination with the use of these techniques in a proportion of cases. Since these techniques have been considered appropriate in a recent review,21 it would appear that a majority of respondents have embraced contemporary concepts. On the other hand, 53% of respondents never used rubber dam.
Use of RBC materials has been described as 'technique sensitive' due to the need for attention to detail during bonding to tooth substance and during bonding procedures and placement, notwithstanding the difficulties experienced by clinicians in achieving an adequate contact point.5 In this respect, a number of manufacturers have introduced so-called 'packable' materials, which, along with recently introduced sectional matrix systems, may help alleviate the difficulties in achieving a good contact.21 However, respondents to the present survey reported more difficulties in manipulation of composite than with amalgam. This could be considered to be a question of adaptation and learning, since it may be that dentists who work mainly with amalgam lack experience in using composite. The converse has been noted among past dental students in the school of dentistry in Nymegen (The Netherlands) who first gained experience in the use of composite who then found difficulty in manipulating amalgam when presented with this material in their final year of study (J. Roeters, personal communication, July 2002).
Other areas for which composite was reported to be less adequate than amalgam were wear resistance, value for money for the patient and lack of post-operative symptoms. Furthermore, respondents reported an increased incidence of secondary caries, need for root fillings and loss of fillings when amalgam use decreased. Eighty-two per cent of respondents reported that technical challenges increased as amalgam use decreased. Eighty-three per cent of respondents 'agreed strongly' that posterior composites were more time consuming to place than a corresponding amalgam restoration, while 81% agreed with the statement that increased use of composites increased the cost of oral healthcare. Seventy per cent agreed with the statement that discontinuation of amalgam as a restorative material would restrict dentists' ability to adequately treat patient's oral health. These reported views, if typical of the dental profession throughout the UK, may go some way to explain the less-than-enthusiastic adoption of tooth-coloured restorative materials for posterior teeth. In this respect, the polymerisation contraction of resin-based materials on curing is a central aspect of their 'technique sensitivity'. It is therefore not surprising that 92% of respondents agreed with the statement that a low-shrink composite would be an advantage. In this respect, it could be surmised that the development of a low-shrink material could result in wider adoption of the use of resin-based tooth coloured materials for restoration of posterior teeth, provided that the new resins do not inherit alternative, suboptimal, physical characteristics.
Lastly, when the data are compared with the 1998 publication from which the questionnaire used in the present work is derived, there are strong similarities in the overall need for treatment, but differences in the reported use of materials.13 For example, while amalgam use decreased by 58% in Finland between 1992 and 1997,13 and by 50% in Great Britain between 1996 and 2001, only 2% of respondents from Great Britain do not use amalgam, compared with 37% in Finland. Furthermore, although the percentages of respondents who do not use composite are close to zero for both countries, 83% of respondents from Finland reported an increase in the use of composite in the five years preceding the survey,13 compared with 62% of respondents from Great Britiain who reported similarly. Fifty-four per cent of respondents from Finland reported that they never prescribed gold inlays/crowns,13 compared with 25% in the present survey. These differences may, in part, be due to the guidance issued by the Ministry of Social Affairs and Health in Finland in 1994 which recommended that the use of amalgam be reduced for environmental reasons, and the absence of such guidelines in the UK, and reflect the different methods of funding of oral healthcare in the two countries. However, the reported use of glass ionomer is similar in both surveys
Conclusions
It is concluded that 49% of respondents from Great Britain seldom or never place large composite restorations in posterior teeth and that their choice of material is greatly influenced by clinical indications and patients' demands. Reasons for not using composite materials in loadbearing situations included:
-
perceived poorer wear resistance than amalgam,
-
perceived difficulties in manipulation,
-
less good value for money for the patient,
-
increased number of symptoms with composite,
-
more time-consuming placement, and,
-
perceived reduced longevity.
However, composite scored positively with regard to its better aesthetic properties. A high proportion of respondents supported the introduction of a low-shrink composite.
References
Clinical Research Associates. Product use survey. CRA Newsletter.1995; 19; 1––2.
Todd JE, Lader D . Adult Dental Health Survey 1988. London: Her Majesty's Stationery Office, 1991.
Downer MC, Azli NA, Bedi R, Moles DR, Setchell DJ . How long do routine dental restorations last? A systematic review. Br Dent J 1999; 187: 432–439.
Feilzer AJ, DeGee AJ, Davidson CL . Setting stress in composite resin in relation to the configuration of the restoration. J Dent Res 1987; 66: 1636–1639.
Cunningham J, Foster MA, Mair LH, Ireland RS . Clinical evaluation of three posterior composite and two amalgam restorative materials: 3 year results. Br Dent J 1990; 169: 319–323.
Eick D, Laughlin G, Krenkel D, Rozzi S, Craig B, Reiman M . A new oxirane/polyol low shrink/low stress dental composite. J Dent Res 2001; 80: 271. Abstract No 1885.
Craig BD, Reiman MG, Oxman JD, Jacobs DW, Rozzi SM . Mechanical properties of oxirane-based dental composite materials J Dent Res 2001; 0: 271. Abstract No.1887.
Palin W, Fleming G, Burke F, Marquis P, Randall RC . Evaluation of the volumetric shrinkage of a novel resin-based restorative. J Dent Res 2002: 81: A–36. Abstract No. 59.
El-Mowafy OM . Wear of posterior composite restorations. A problem of the past. Ontario Dentist 1994; 71: 13–17.
El-Mowafy OM, Lewis DW, Benmergui C, Levinton C . Meta-analysis on long-term clinical performance of posterior composite restorations. J Dent 1994; 22: 33–43.
ADA Council on Scientific Affairs: ADA Council on dental benefit programs. Statement on posterior resin-based composites. J Amer Dent Assoc 1998; 129: 1627–1628.
Brown LJ, Wall T, Wassesnaar JD . Trends in resin and amalgam use as recorded on insurance claims submitted by dentists from the early 1990s and 1998. J Dent Res 2000; 79: 461. Abstract No. 2542.
Widstrom E, Forss H . Dental practitioner's experiences on the usefulness of restorative materials in Finland 1992–1996. Br Dent J 1998; 185: 540–542.
Mjor IA . Selection of restorative materials in general dental practice in Norway. Acta Odontol Scand 1997; 55: 53–57.
Forss H, Widstrom E . From amalgam to composite:selection of restorative materials and restoration longevity in Finland. Acta Odontol Scand 2001; 59: 57–62.
Dillman DA . Mail and telephone surveys: the total design method. New York: John Wiley and Sons,1977.
Tan RT, Burke FJT . Response rates to questionnaires mailed to dentists. A review of 77 publications. Int Dent J 1997; 47: 349–354.
The Dentists Register 2001. London: General Dental Council.
Audit Commission. Dentistry: primary dental care services in England and Wales. P15, para 20.2002, Audit Commission, London.
Sarll DW, Holloway PJ . Factors influencing innovation in general dental practice. Br Dent J 1982; 1153: 264–266.
Burke FJT, Shortall ACC . Successful restoration of load-bearing cavities in posterior teeth with direct-placement resin-based composite. Dent Update 2001; 28: 388–398.
Acknowledgements
The authors acknowledge the financial support of 3M ESPE, St.Paul, MN, USA for this project and wish to thank the practitioners who completed and returned their questionnaires.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Burke, F., McHugh, S., Hall, A. et al. Amalgam and composite use in UK general dental practice in 2001. Br Dent J 194, 613–618 (2003). https://doi.org/10.1038/sj.bdj.4810258
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4810258
This article is cited by
-
A Novel Silane System for Amalgam Repair with Resin Composite: an in vitro Study
Silicon (2019)
-
Class II composite resin restorations: faster, easier, predictable
British Dental Journal (2016)
-
General dental practitioners' knowledge of polymerisation of resin-based composite restorations and light curing unit technology
British Dental Journal (2011)
-
State-of-the-art techniques in operative dentistry: contemporary teaching of posterior composites in UK and Irish dental schools
British Dental Journal (2010)
-
Teaching of direct posterior resin composite restorations in UK dental therapy training programmes
British Dental Journal (2010)