Abstract
Aim
We undertook a national survey to establish the management of dense vitreous haemorrhage without obvious cause.
Methods
DesignCross-sectional anonymous self-reporting survey of ophthalmic practitioners within three target groups: vitreoretinal specialists (VRS), nonvitreoretinal specialists (NVRS), and associate specialists (AS).
Intervention
Presentation of the hypothetical scenario of a patient presenting with recent onset (fresh) vitreous haemorrhage with no retinal view and no apparent cause on history taken at presentation.
Outcome measures
The relative importance assigned by respondents to eight examination techniques at presentation. The proportion of respondents stating that they would review patients and perform B-scan examination at or prior to 2 weeks after presentation. The stated time to surgical intervention by VRS, and the time to referral by NVRS and AS.
Results
VRS ranked B-scan examination higher than AS (P<0.001). A total of 98.1% of VRS indicated that they would next review patients within 2 weeks of presentation, this figure fell to 86.5% for NVRS and 47% for AS (P<0.001). A 98.1% of VRS indicated that they would next perform B-scan ultrasound within 2 weeks of presentation, this figure fell to 88.9% for NVRS and 70.6% for AS (P<0.001). The mean time to surgical intervention by VRS was 9.5 weeks without retinal tear demonstrated on B-scan, 1.7 weeks with retinal tear demonstrated on B-scan and 1 week with retinal detachment demonstrated on B-scan. The mean time to referral by NVRS was 6.7 weeks and by AS was 11.9 weeks.
Conclusions
Vitreoretinal specialists considered B-scan the most important examination tool, and typically perform B-scan early and frequently after presentation. Non-VR ophthalmologists (particularly associate specialists) review patients and perform B-scan ultrasound later and less often than vitreoretinal specialists. We recommend early referral to VR specialists, as reported referral even in uncomplicated cases would often be outside the timeframe within which VR specialists would typically choose to operate.
Similar content being viewed by others
Introduction
The incidence of spontaneous vitreous haemorrhage is approximately seven cases per 100 000 population.1, 2 Dynamic vitreoretinal traction is the most common cause and includes posterior vitreous detachment (PVD) with retinal tear (∼30–40%) or detachment (∼5%), or PVD without retinal tear (∼3–8%).1, 2, 3
If all presenting haemorrhages are considered, the diagnosis can be made at presentation in about 80% of cases,3 as there is adequate fundus view. Medical history assists diagnosis, with diabetes and other vascular diseases (eg hypertension, branch retinal vein occlusion, retinal macroaneursym, ARMD) also significant causes of spontaneous vitreous haemorrhage.2 The fellow eye examination and past ocular history likewise provide helpful clues to underlying aetiology of the haemorrhage.1, 3 Diagnosis at presentation is easier when the haemorrhage is minor and an adequate view of the retina is obtained. However, a significant group remains with dense spontaneous vitreous haemorrhage, without good retinal view, and no clear diagnosis at presentation.1 Even with the opportunity of history and B-scan ultrasound examination, one study found a retrospectively accurate diagnosis at presentation could be made in only 1/3 of cases,1 and establishing the cause of dense vitreous haemorrhage was frequently not possible until late in the follow-up period.
Acute, spontaneous, nontraumatic posterior vitreous separation with dense fundus-obscuring vitreous haemorrhage is associated with a high incidence of retinal tears (67%) and detachment (39%), making close follow-up with clinical examination and ultrasonography important.1, 4 Ideally, surgery is carried out before retinal detachment occurs as the prognosis of primary rhegmatogenous retinal detachments with significant vitreous haemorrhage at initial presentation is reduced due to the high incidence of proliferative vitreoretinopathy.4, 5, 6, 7
We report the findings of a national survey undertaken to investigate the range of management practices of this presentation, and discuss pertinent issues.
Methods
Design
Cross-sectional survey of ophthalmic practitioners within three target groups:
-
vitreoretinal specialists (VRS)—that is, consultant ophthalmologists with a subspecialty practice in vitreoretinal surgery;
-
nonvitreoretinal specialists (NVRS)—that is, consultant ophthalmologists practicing either general ophthalmology or with subspecialty practice that does not include vitreoretinal surgery;
-
associate specialists (AS)—that is, career hospital-based ophthalmologists that have completed ophthalmic training but have not obtained a consultant post.
Selection
Nonrandomized sampling was undertaken of VRS at the Britain and Eire Association of Vitreoretinal Specialists (BEAVRS) meeting in Edinburgh 2002. For each of the NVRS and AS groups a random selection of 100 individuals was obtained from the Royal College of Ophthalmologists membership database and a single anonymous mail-out was conducted. No record was kept of these randomly selected participants and consequently no reminder mail-out was performed.
Intervention
Participants were presented with a single page questionnaire relating to a hypothetical scenario of a patient presenting with recent onset (fresh) vitreous haemorrhage with no retinal view and no apparent cause on history taken at presentation. This clinical scenario was developed to investigate how vitreous haemorrhage and possible underlying retinal tear or detachment is managed by the different participant groups.
A series of questions were posed regarding:
-
relative importance of eight specific presentation examinations,
-
typical follow-up pattern including timing of B-scan ultrasound examinations,
-
for NVRS/AS who performed B-scans, and typical timing of referral to vitreoretinal specialists,
-
and for VRS typical timing of surgical intervention when B-scan showed: no tear; retinal tear; or retinal detachment.
Questionnaire design
Two separate single page questionnaires were designed—one for VRS and the other for NVRS/AS (see Appendix 1 for condensed questionnaire). We had three specific hypotheses regarding aspects of management we sought to test:
-
1)
That B-scan ultrasound is not considered as important in the management of patients with spontaneous vitreous haemorrhage as perhaps it should.
-
a)
Of the eight examination options for ranking at presentation in question 1, our target variable was B-scan ultrasound. The remaining variables were included as potential distracters (albeit each having relevance to the clinical scenario).
-
a)
-
2)
That patients are not reviewed clinically and/or with B-scan early enough after presentation, so that significant pathology might be reasonably excluded most of the time.
-
a)
As the average time to the development of retinal detachment has been reported in this clinical situation at approximately 2 weeks,4 we divided respondents (for questions 2 and 3) into those reviewing patients or performing B scan at or before 2 weeks and those that did not. Question 4 for NVRS/AS provides additional accessibility information for B-scan.
-
a)
-
3)
That VRS would prefer to intervene surgically earlier than when patients are typically referred to them. (survey questions 4–6 for VRS and question 5 for NVRS/AS)
-
a)
Thus questions 4–6 for VRS and 5 for NVRS/AS, which determined how long and how often patients are followed until a decision either for surgical intervention (VRS) or referral for vitreoretinal opinion (NVRS/AS) is made.
-
a)
Questionnaire pretesting and piloting was performed with VRS, NVRS, and AS based at Sussex Eye Hospital with feedback obtained and questionnaire modification so that the questionnaire data collection tool was considered reasonably valid in obtaining responses to the specific hypotheses outlined above.
Outcome measures
-
The relative importance assigned by respondents to eight examination techniques at presentation.
-
The proportion of respondents stating that they would review patients and perform B-scan examination at or prior to 2 weeks after presentation.
-
The stated time to surgical intervention (VRS), and the time to referral (NVRS/AS).
Statistical analysis
Reporting of practice patterns for each of the groups, was planned in both descriptive noncomparative terms, and after statistical analysis looking for any significant differences in management between groups. The relative importance (ranking) of each of the eight examinations were compared between the three practitioner groups using the Mann–Whitney test for unrelated samples. The proportions within each group who stated that they would review patients and perform B-scan examination at or before 2 weeks after initial presentation were compared using Fisher's exact test, as were the proportions within each of the ‘who performs B-scan’ question 4. The Bonferroni correction was used. This adjusts the accepted statistical significance when performing tests on multiple outcome measures to reduce the probability of a type II error (accepting that there is a difference when one does not exist). If alpha is the accepted statistical significance for each test and there are n statistical tests and we accept a probability P of a type II error overall, then alpha approximates to P/n. For this study, alpha approximates to 0.05/26 and we therefore accepted differences between groups when that test had a P-value less than or equal to 0.002.8 Respondents with missing data for a question were excluded from the analysis of that question. Analyses were conducted using the Statistical Package for the Social Sciences SPSS 8.0.0. (SPSS Inc., Chicago, IL, USA).
Results
The overall response rate for the survey was 44%, with 52% of VRS, 44% of NVRS and 36% of AS responding to the questionnaire. The ranking for each of the presentation examinations, the proportion reviewing patients and performing B-scan at or before 2 weeks and the times to intervention for VRS and time to referral for NVRS and AS are shown in Table 1.
All respondents provided data on ranking of importance for the different presentation examinations. VRS ranked B-scan examination higher than AS, the median rank for VRS was 1 (interquartile {IQ} range 1–2) and for AS was 4 (IQ range 1–6) (P<0.001) (see Figure 1). AS ranked both the visual acuity and iris/anterior segment examination higher than VRS, median ranks were 1 (IQ range 1–4) and 3 (IQ range 2–5), respectively, for AS and 4 (IQ range 2–6.75) and 6 (IQ range 4–7) for VRS (P<0.001). There were no other significant differences between the rankings of any other presentation examinations between the three practitioner groups at the Bonferroni-corrected significance level.
Six questionnaires had missing data for follow-up examination, all from the NVRS group. 98.1% of VRS indicated that they would next review patients within 2 weeks of presentation, this figure fell to 86.5% for NVRS and 47% for AS, and this difference was statistically significant (P<0.001) (see Figure 2). When all missing data was recoded as review within 2 weeks this difference between groups remained statistically significant (P<0.001).
Nine questionnaires had missing data for next B-scan examination, seven from the NVRS group and two from the AS group. A 98.1% of VRS indicated that they would next perform B-scan ultrasound within 2 weeks of presentation, this figure fell to 88.9% for NVRS and 70.6% for AS, and this difference was statistically significant (P<0.001) (see Figure 3). When all missing data was recoded as B-scan within 2 weeks this difference between groups remained statistically significant (P=0.001).
There were two questionnaires with missing data on who performed B-scan, one within NVRS and one within AS. Of the remaining NVRS, 24 (57.1%) performed B-scan themselves, six (14.3%) had local radiologists perform B-scan and 12 (28.6%) referred on for B-scan. Of the remaining AS 28 (80%) performed B-scan themselves, two (5.7%) had local radiologists perform B-scan and five (14.3%) referred on for B-scan. We found no evidence of a significant difference between these figures and no significant effect of who performed B-scan on the proportion of respondents performing B-scan at or before 2 weeks from initial presentation.
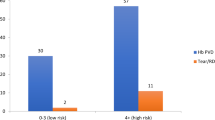
The mean time to surgical intervention by VRS was 9.5 weeks (SD=7.2) without retinal tear demonstrated on B-scan ultrasound, 1.7 weeks (SD=1.4) with retinal tear demonstrated on B-scan, and 1.0 week (SD=0.2) with retinal detachment demonstrated on B-scan. The mean time to referral by NVRS was 6.7 weeks (SD=6.7) and by AS was 11.9 weeks (SD=10.5). 31.7% of NVRS stated that they would refer patients after 9.5 weeks, the average time for intervention by VRS without retinal tear demonstrated on B-scan, while 42.9% of AS stated that they would refer after this time.
Discussion
The established treatment option for persistent/nonclearing vitreous haemorrhage is pars plana vitrectomy. 2 However, historically the management recommendation for vitreous haemorrhage of unknown cause has been conservative.2 At presentation, strict rest with head upright in the first few days may allow sufficient settling of blood and view of superior retina where pathology will most likely exist.9 As spontaneous clearing of the vitreous may occur, it can sometimes be reasonable to monitor patients closely.10 However, even though uncommon, dense fundus-obscuring vitreous haemorrhage represents an important clinical management problem.1, 4 With 67% of such eyes having retinal tears and 39% retinal detachment,4 failure to diagnose underlying visually threatening pathology raises potential medicolegal consequences,11, 12 as delayed management can be associated with adverse visual outcome.4 If retinal detachment develops behind a dense vitreous haemorrhage this will not typically be recognized by the patient (although they may do so). If a conservative management approach is taken, then regular and repeated review including B-scan ultrasound is necessary, and if this is not possible then referral to a vitreoretinal service should occur, so that no delays occur in the management should retinal tears with or without retinal detachment develop.1, 4 Early vitrectomy has been recommended if there are significant risk factors, such as a history of retinal detachment in the contralateral eye, high myopia or previous BRVO.1, 4, 13 However, surgical intervention in itself is also not without risk, with potentially sight-threatening complications of vitrectomy surgery such as iatrogenic retinal tears and lens touch in up to 5% and endophthalmitis and suprachoroidal haemorrhage about 0.1%. Consequently, the balance of risks and benefits of intervention vs observation should lead to an informed consent decision with each patient.
In this survey, even when retinal detachment can be confidently excluded, many VRS consider early intervention standard. Interestingly, the reported mean time to referral of uncomplicated cases to a vitreoretinal service was 9.1 weeks (SD=8.9), which was also to the mean time at which VRS would typically intervene for vitreous haemorrhage without retinal tear or detachment evident on B-scan.
Our survey illustrates that there is a range of current practice, both within and between the different practitioner groups. While history and clinical examination may assist a diagnosis, multiple publications emphasize that B-scan ultrasound is essential in the assessment and monitoring of these patients.1, 4, 14, 15 Our results demonstrated that VRS concurred with this and ranked B-scan ultrasound most important, a finding significantly different from the other participant groups. Interestingly, AS considered visual acuity the most important examination, even though the scenario indicated dense fundus obscuring haemorrhage. As such visual acuity would be unlikely to be better than CF. Even a total retinal detachment would be unlikely to have NPL vision at presentation, which would be the only visual acuity likely to influence management. Pupil responses and projection of light would be much more useful clinical tests in the absence of B-scan ultrasound in the setting of fundus obscuring haemorrhage.
B-scan ultrasound is not always readily available and we found that 40% of NVRS and 20% of AS respondents need to refer to either local radiology service or specialist B-scan service if B-scan is considered necessary. Through-the-lid eye scanning with general radiology ultrasound equipment has been shown to be reasonably sensitive and specific,16 and should be considered if urgent ultrasound is required and significant delays in patient referral or review anticipated.
Because of the common diagnostic difficulties and the frequent need for surgical intervention, it has been recommended that eyes with vitreous haemorrhage be followed up in centres with ultrasonographic and surgical expertise.1, 4 We found that VRS would typically intervene within 1 week for RRD and 1.7 weeks for retinal tear seen on ultrasound.
If B-scan at presentation does not suggest either retinal tear or detachment, then continued close monitoring of the patient is required as these may develop. While it may be possible to diagnose retinal tear on B-scan ultrasound, it is often not possible to confidently exclude this complication, as B-scan ultrasound has limitations both in sensitivity and specificity for excluding retinal tear and detachment, as well as operator dependent variability. A patient with B-scan interpreted as normal at presentation, may go on to develop significant visually threatening pathology in the subsequent weeks.4 As retinal tears can quickly progress to detachment,4 especially if significant retinal traction exists (as might occur in the setting of avulsed vessel with retinal break),17 such review should be early and frequent. Our survey revealed that essentially all VRS felt that the patient should be next seen within 2 weeks of presentation and that repeat B-scan should also be within this timeframe. Significant percentages of NVRS and AS indicated they would next see and B-scan the patient beyond this time (see Figures 2 and 3).
One limitation of hypothetical surveys is the relevance of the hypothetical scenario to actual clinical practice. Many patients will have some clues to the aetiology of their vitreous haemorrhage—for example, medical and ophthalmic history and age. Such clues will clearly influence how a patient is managed, and determining best practice for each clinical scenario well beyond the scope of this questionnaire. Nonetheless, we felt our scenario is validated by previous publications supporting the clinical relevance and importance, and allows general management conclusions to be made.1, 4, 7, 10, 18 Furthermore, this survey provides useful preliminary structure for a more formalized assessment of actual clinical practice by national audit—such an audit would also overcome self-reporting bias inherent in surveys such as ours.
A number of other sources of bias exist in our cross-sectional survey. There was potential selection bias in the VRS group as sampling of this group was not randomized. We chose sampling at the BEAVRS meeting as most UK VRS attend this meeting and we wanted to capture the highest response rate possible with single sampling of this numerically smaller (nationally) target group. Ultimately, it was deemed the practices of this group in the hypothetical scenario presented that would provide a standard against which the other groups would be compared. The anonymous survey sampling occurred at the beginning of the meeting, without preamble and no meeting content related to any aspect of the survey topic. Response rates will also influence selection bias as lower response rates may make sample groups less representative of the broader population as respondents may have given different responses to nonrespondents. It is very difficult to predict the likely effect of this type of bias. Nonresponders may have less time to respond to the survey or may have less experience or knowledge of the topic and therefore feel less able to provide adequate answers to the questions.19 However, it is likely that each of the practitioner groups were affected in the same way making a comparison between these groups justifiable. Our response rates though low are typical of single sampling anonymous surveys.19 The purpose of this survey was not to audit an individual's practice, rather look at general trends between the study sample groups and report on these for the educational purpose of updating practice patterns. Consequently, we were prepared to accept lower response rates and preserve anonymity, than have nonparticipation because respondents might be indentifiable. Finally, our survey has not investigated actual practices which may not differ between the groups we have examined. However as there were sufficient self-reported differences between the groups, and the hypothetical scenario described important clinically, our survey findings reinforce the need to update on changing trends in vitreoretinal management of dense fundus-obscuring haemorrhage without obvious cause.
In conclusion, management decisions are based on the benefits and risks of surgical intervention vs conservative regular monitoring. Vitreoretinal specialists considered B-scan the most important examination tool, and typically perform B-scan early and frequently after presentation. Non-VR ophthalmologists (particularly AS) review patients and perform B-scan ultrasound later and less often than vitreoretinal specialists. As referral to VR specialists was often outside the timeframe within which VR specialists would operate, we recommend early referral of all cases so that appropriate investigation and management can occur. This is as dense fundus-obscuring vitreous haemorrhage without obvious cause should be considered due to retinal tear/detachment until proven otherwise. Further prospective national audit using actual clinical practice would be worthwhile as well as subsequent development of college guidelines.
References
Lindgren G, Sjodell L, Lindblom B . A prospective study of dense spontaneous vitreous hemorrhage. Am J Ophthalmol 1995; 119 (4): 458–465.
Spraul C, Grossniklaus H . Vitreous haemorrhage. Surv Ophthalmol 1997; 42 (1): 3–39.
Lean J, Gregor Z . The acute vitreous haemorrhage. Br J Ophthalmol 1980; 64: 469–471.
Sarrafizadeh R, Hassan TS, Ruby AJ, Williams GA, Garretson BR, Capone Jr A et al. Incidence of retinal detachment and visual outcome in eyes presenting with posterior vitreous separation and dense fundus-obscuring vitreous haemorrhage. Ophthalmology 2001; 108 (12): 2273–2278.
Asaria R, Gregor Z . Simple retinal detachments: identifying the at-risk case. Eye 2002; 16 (4): 404–410.
Asaria R, Kon C, Bunce C, Charteris D, Wong D, Luthert P et al. How to predict proliferative vitreoretinopathy—a prospective study. Ophthalmology 2001; 108 (7): 1184–1186.
Fournier P, Aracil P, Bonnet M . [Rhegmatogenous retinal detachment and retinal tear with intravitreous hemorrhage]. J Fr Ophtalmol 1988; 11 (1): 7–14.
Bland M . An Introduction to Medical Statistics. Oxford University Press: Oxford, 2000.
AAO Prefered Practice Pattern. Management of Posterior vitreous detachment, retinal breaks and lattice degeneration. In: AAO (San Francisco)2003.
Verbraeken H, Van Egmond J . Non-diabetic and non-oculotraumatic vitreous haemorrhage treated by pars plana vitrectomy. Bull Soc Belge Ophtalmol 1999; 272: 83–89.
Fung WE . Opportunities for maloccurrence in delivery of specialized care in the managed care environment. [comment]. Surv Ophthalmol 1998; 43 (3): 280–282.
Frankel J . Avoiding misplacement of blame for medical maloccurrence.[comment]. Surv Ophthalmol 2000; 44 (4): 362–363.
Tanaka M, Ninomiya H, Kobayashi Y, Qiu H . Studies on vitrectomy cases associated with complicated branch retinal vein occlusion. Jpn J Ophthalmol 2001; 45 (4): 397–402.
Hasenfratz G . [Acute vitreous haemorrhage–possibilities for differential diagnostic, echographic assessment]. Fortsch der Ophthalmol 1990; 87 (6): 641–645.
Scott IU, Flynn Jr HW, Hughes JR . Echographic evaluation of a patient with diabetes and dense vitreous haemorrhage: an avulsed retinal vessel may mimic a tractional retinal detachment. Am J Ophthalmol 2001; 131 (4): 515–516.
Fielding JA . Ultrasound imaging of the eye through the closed lid using a non-dedicated scanner. Clin Radiol 1987; 38 (2): 131–135.
Theodossiadis GP, Koutsandrea CN . Types of avulsed retinal vessels associated with rhegmatogenous retinal detachment: treatment and results. Graefes Arch Clin Exp Ophthalmol 1987; 225 (3): 185–188.
Isernhagen R, Smiddy W, Michels R, Glaser B, de Bustros S . Vitrectomy for nondiabetic vitreous hemorrhage. Not associated with vascular disease. Retina 1988; 8 (2): 81–87.
Barclay S, Todd C, Finlay I, Grande G, Wyatt P . Not another questionnaire! Maximizing the response rate, predicting non-response and assessing non-response bias in postal questionnaire studies of GPs. Fam Pract 2002; 19 (1): 105–111.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial interest in any of the instruments or techniques used in this manuscript.
Appendix 1: Questionnaire design—the hypothetical scenario and first three questions were identical for each questionnaire, as follows:
Appendix 1: Questionnaire design—the hypothetical scenario and first three questions were identical for each questionnaire, as follows:

Rights and permissions
About this article
Cite this article
Vote, B., Membrey, W. & Casswell, A. Vitreous haemorrhage without obvious cause: national survey of management practices. Eye 19, 770–777 (2005). https://doi.org/10.1038/sj.eye.6701649
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701649