Abstract
Oncolytic viruses derived from herpes simplex virus (HSV) have shown considerable promise as antitumor agents against solid tumors including ovarian cancer. The current group of oncolytic HSVs was constructed exclusively from type 1 HSV. To exploit further the therapeutic potential of replication-selective viruses, we constructed an oncolytic virus from type 2 HSV by deleting the protein kinase domain of the viral ICP10 gene, which targets the activated Ras signaling pathway in tumor cells. In the study reported here, we administered this HSV-2-derived virus intraperitoneally (i.p.) to nude mice bearing metastatic human ovarian tumor xenografts, evaluated its oncolytic activity, and compared with to that of a virus constructed from HSV-1. Two injections of the HSV-2-derived virus (3 × 106 pfu per dose) led to complete eradication of disseminated tumors in the peritoneal cavity in more than 87% of the mice, whereas the HSV-1-based oncolytic virus, administered at the same dose and on the same schedule, eradicated tumor nodules in only 12% of mice (P<0.01). We conclude that i.p. administration of this HSV-2-based oncolytic virus may provide effective treatment for metastatic human ovarian cancer.
Similar content being viewed by others
Introduction
Ovarian cancer remains the leading cause of death in patients with gynecological malignancies in the United States. Because of ineffective screening strategies and inconspicuous early symptoms, these tumors are usually detected late in the clinical course, when metastases are present. The primary site of metastatic spread is within the peritoneal cavity. Despite improved surgical techniques and chemotherapy, the mortality rate for ovarian cancer has remained largely unchanged over the last decade,1, 2 mandating the development of new treatment strategies.
Replication-selective viruses afford a promising treatment for malignant solid tumors. Oncolytic viruses derived from herpes simplex virus (HSV) were initially designed and constructed for the treatment of brain tumors.3, 4 Subsequently, they have proved effective against a variety of other human solid tumors, including ovarian cancer.5, 6 The current group of oncolytic HSVs were constructed exclusively from type 1 virus (HSV-1), most often by deleting the γ34.5 gene, which encodes a neurovirulent factor, and/or insertional mutation of the ICP6 gene, which encodes the large subunit of ribonucleotide reductase.3, 4, 7, 8, 9 Inactivation of either or both of these genes enables the virus to replicate selectively in dividing cells whereas sparing normal *nondividing cells.10, 11, 12
We have recently constructed a new oncolytic virus from type 2 HSV (HSV-2) to exploit a unique feature of the viral ICP10 gene, which contains in its N terminus a well-defined region that encodes a serine/threonine protein kinase (PK) activity.13 As this PK domain can bind and phosphorylate the GTPase-activating protein Ras-GAP, which leads to activation of the Ras/mitogen-activated protein kinase (MAPK)/extracellular signal-regulated kinase (MEK)/MAPK mitogenic pathway and c-Fos induction and stabilization, it is required for efficient HSV-2 replication.14, 15 A mutant HSV-2 virus (FusOn-H2), deleted for this PK domain, replicated selectively in and thus lysed human tumor cells. Infection with this virus also induced syncytia formation in tumor cells, providing an additional oncolytic mechanism that enhanced its antitumor effect overall.16
Here, we report the therapeutic effects of FusOn-H2 against metastatic human ovarian cancer xenografts growing in the peritoneal cavity of nude mice. Our results indicate that this mutant virus may be an effective oncolytic agent in the treatment of metastatic human ovarian cancer. Indeed, two intraperitoneal (i.p.) injections of the virus at a moderate dose completely eradicated disseminated tumors in the peritoneal cavity of most animals, in contrast to the weak activity of a conventional oncolytic virus derived from type 1 HSV.
Materials and methods
Cell lines and viruses
African green monkey kidney (Vero) cells were obtained from American Type Culture Collection (Rockville, MD). SKOV3 cells derived from a serous cystoadenocarcinoma were kindly provided by Dr Robert Bast (M D Anderson Cancer Center). All cells were cultured in Dulbecco's modified Eagle's medium containing 10% fetal bovine serum (FBS). Female Hsd athymic (nu/nu) mice (obtained from Harlan, Indianapolis, Indiana) were kept under specific pathogen-free conditions and used in experiments when they attained the age of 7–8 weeks.
Construction of the HSV-1-derived oncolytic virus Baco-1 is described elsewhere,6, 17 as is construction of FusOn-H2.16 Briefly, Baco-1 was constructed from a bacterial artificial chromosome (BAC)-based construct that contains a mutated HSV genome, in which the diploid gene encoding γ34.5 and both copies of the HSV packaging signal (pac) have been deleted.18 The green fluorescent protein (GFP) gene driven by the cytomegalovirus (CMV) promoter, together with a copy of the HSV-1 pac, were inserted into the unique PacI site of fHSV-delta-pac by direct ligation, to generate the infectious HSV (Baco-1). Thus, Baco-1 has both copies of the γ34.5 gene deleted and contains the GFP marker gene.17
For construction of FusOn-H2, the ICP10 left-flanking region of the wild-type (wt) HSV-2 strain 186 (wt186) genome (equivalent to nucleotide span 85994–86999 in the HSV-2 genome), the ribonucleotide reductase domain and the right-flanking region (equivalent to nucleotide span 88228–89347) were amplified by PCR. These PCR products were cloned together into pNeb193, generating pNeb-ICP10-deltaPK. Hence, the new plasmid contains a mutated ICP10 gene, in which the protein kinase domain (equivalent to nucleotide span 86999–88228) is deleted. Then, the DNA sequence containing the CMV promoter-EGFP gene was PCR amplified from pSZ-EGFP, and the PCR-amplified DNA was cloned into the deleted PK locus of pNeb-ICP10-deltaPK, generating pNeb-PKF-2. During the design of PCR-amplification strategies, the EGFP gene was fused in-frame with the remaining RR domain of the ICP10 gene, so that the new protein product of this gene contained the intact EGFP. The modified ICP10 gene was inserted into the genome of wt186 by homologous recombination. The recombinant virus (FusOn-H2) was identified by screening for GFP-positive plaques. Viral stocks were prepared by infecting Vero cells with 0.01 plaque-forming units (pfu) per cell, harvesting the virus after 2 days, and storing it at −80°C.
Phenotypic characterization and oncolytic activity of FusOn-H2 against a human ovarian cancer cell line
To phenotypically characterize the new virus, we seeded SKOV3 ovarian cancer cells into six-well plates, and then infected them on the following day with Baco-1, wt186 or FusOn-H2 at a dose of 0.01 pfu/cell. Cells were cultured in a maintenance medium (containing 1% FBS) and were incubated for up to 2 days to allow the fusion pattern and plaques to develop. To measure the in vitro killing effect of the viruses, we seeded SKOV3 tumor cell lines into 24-well plates and infected them with Baco-1 or FusOn-H2 at 0.01 and 0.001 pfu/cell, or left them uninfected. Cells were harvested 24, 48 or 72 h later by trypsinization, and the number of viable cells determined with a hemocytometer after Trypan blue staining. The percentage of viable cells was calculated by dividing the number of cells excluding Trypan blue in the infected well by the number excluding the stain in the well that was left uninfected. The experiments were performed in triplicate, with mean cell numbers used for the final calculation.
Animal studies
SKOV3 cells were harvested from subconfluent cultures by a brief exposure to 0.25% trypsin and 0.05% ethylenediaminetetraacetic acid. Trypsinization was stopped with medium containing 10% FBS, and the cells were washed once in serum-free medium and resuspended in phosphate-buffer saline (PBS). Only single cell suspensions with >95% viability were used for in vivo injection. Briefly, on day 0, 2 × 106 SKOV3 cells were inoculated into the peritoneal cavities of 8-week-old female nude mice. The mice were then randomly divided into three groups of eight mice each. On days 8 and 15 after tumor inoculation, the mice in groups 1 and 2 were injected i.p. with either Baco-1 or FusOn-H2 at a dose of 3 × 106 pfu in a total volume of 200 μl. Mice in group 3 received the same volume of PBS as the control. The therapeutic injection was given at a site distant from the area of tumor cell inoculation. On day 36 after tumor cell inoculation, all surviving mice were euthanized by CO2 exposure and evaluated macroscopically for the number and size of tumor nodules in the abdominal cavity.
Systemic and intracerebral virus injections
For systemic administration, the virus was diluted in 100 μl of serum-free medium and injected into the animal through the tail-vein as described.19 Intracranial injection was performed essentially as described.20 Briefly, mice were anesthetized and placed in a stereotactic frame (Stoelting). A bur hole was drilled in the skull 1 mm anterior and 2 mm lateral to the bregma with a 0.9 mm burr to expose the dura. The mice were injected with 3 μl of serum-free medium containing the virus, by use of a 100 μl syringe (Hamilton) fitted with a 26-gauge needle and connected to the manipulating arm of the stereotactic frame. The injection was directed to the caudate nucleus at a depth of 3.5 mm from the dura and given over 2.5 min. The needle was left in place for 3 min and then withdrawn slowly over another minute, to prevent reflux of the virus solution.
Immunohistochemical staining for HSV antigens in liver sections
Livers were removed 3 or 4 days after systemic administration of HSVs, fixed with 4% paraformaldehyde overnight at 4°C, and treated with 25% sucrose overnight at 4°C. Ten micrometer sections were then prepared, air-dried at room temperature overnight and treated with 4% paraformaldehyde for 2 min, before being treated with 1% NP40/PBS for 5 min. This procedure was followed by several washes with PBS. The liver sections were then incubated with a rat anti-HSV serum (prepared by our own lab at a 1:100 dilution), at 37°C for 60 min. After washing, fluorescein isothiocyanate (FITC)-conjugated goat anti-rat IgG antibody (Sigma-Aldrich, St Louis, MO), diluted at 1:200, was added to the tissue section and incubated at 37°C for 60 min. After two washes with PBS, the slides were dehydrated in an ascending series of ethanol for 2 min, cleared in xylene for 2 min, mounted in DPX mounting solution, and observed under a fluorescence microscope.
Statistical analysis
Quantitative results are reported as means±s.d. The statistical analysis was performed by Student's t-test or one-way ANOVA. P-values of less than 0.05 were considered significant.
Results
Growth property and phenotype of FusOn-H2 in human ovarian cancer cells
We initially compared the growth of FusOn-H2 with that of its parental wt186 virus and Baco-1. Cells seeded in six-well plates were infected with the viruses at a relatively low dose (0.01 pfu/cell) and harvested at 48 h post-infection, enabling us to assess both the inherent infectivity of the input virus and its ability to replicate and spread in these cells. The results showed that FusOn-H2 replicated well in SKOV3 cells, reaching a titer of almost 1 × 105 pfu/ml (Figure 1). Overall, the titer was about 1 log lower than that of the wt186 or Baco-1 virus, most likely because of the induction of apoptosis in FusOn-H2-infected cells (Fu et al., unpublished data).
Comparison of the replicative properties of FusOn-H2, Baco-1 and wt HSV-2 in SKOV3 cells. SKOV3 cells were seeded into 24-well plates in triplicate and infected with the viruses at 0.01 pfu/cell. The viruses were harvested at 48 h after infection and titrated by plaque assay on Vero cell monolayers.
FusOn-H2 has a fusogenic phenotype in the human breast cancer cell line MDA-MB-435.16 To determine if it retains this phenotype in human ovarian cancer cells, we infected SKOV3 cells in a six-well plate with either the parental wt186 or FusOn-H2 virus, and monitored the cultures for cytopathic effects and syncytia formation. At 24 h postinfection (Figure 2), syncytia formation was clearly present in cultures infected with FusOn-H2, whereas neither the parental wt186 nor Baco-1 virus produced fusogenic phenotype. Instead, they induced a typical cytopathic effect, represented by cell rounding and swelling. At 48 h after infection, most of the SKOV3 cells infected with FusOn-H2 had detached from the plate, leaving fusion bodies and other cell debris floating in the medium. There was some minimal syncytia formation in the well infected with wt186, but the overall effect differed markedly from that of FusOn-H2 observed at either 24 or 48 h postinfection. At the later stage of infection, the plaques in the well infected with Baco-1 virus were becoming larger, but there were still no sign of syncytia formation (Figure 2).
Efficiency of FusOn-H2-induced killing of human ovarian cancer cells in vitro
To assess the cytolytic activity of FusOn-H2, we infected SKOV3 cells seeded in 24-well plates with this virus, wt186 and Baco-1 at a dose of either 0.01 or 0.001 pfu/cell. The cells were harvested at different times after infection, and cell viability was determined by Trypan blue staining. At 0.01 pfu/cell (Figure 3a), infection with FusOn-H2 killed significantly more tumor cells by 24 h postinfection than did either wt186 or Baco-1 (P<0.05). The extend of FusOn-H2-induced killing was similar to that of wt186 at 48 and 72 h postinfection, but remained significantly greater than that of Baco-1 at these two later time points (P<0.05). At 0.001 pfu/cell (Figure 3b), the oncolytic effect of FusOn-H2 was equivalent to that of wt186 at all the time points, whereas both viruses were significantly more oncolytic than Baco-1 (P<0.05). We also evaluated the in vitro oncolytic activity of FusOn-H2 against another human ovarian cancer line, Hey8. Overall, the antitumor effect was essentially the same as obtained with SKOV3 cells (data not shown).
Oncolytic activity of FusOn-H2 against SKOV3 cells in vitro. SKOV3 cells were seeded into 24-well plates and infected with FusOn-H2, Baco-1, or the wt HSV-2 virus wt186 at 0.01 pfu/cell (a) or 0.001 pfu/cell (b), or left uninfected (not shown). Cells were collected 24, 48 or 72 h after infection, and viable cells were counted after Trypan blue staining. The percent cell viability was determined by dividing the number of viable cells in the infected wells by the number of cells in the uninfected well. The data are reported as means±s.d. *P<0.05 as compared with Baco-1 and wt186; #P<0.05 as compared with Baco-1.
Evaluation of FusOn-H2 oncolytic activity against metastatic ovarian cancer
We chose a peritoneal metastasis model to evaluate the antitumor effects of FusOn-H2 against ovarian cancer. This model is clinically relevant, as peritoneal invasion by ovarian cancer is common and usually represents a serious complication. Freshly harvested SKOV3 cells were inoculated into the peritoneal cavities of nude mice at 2 × 106 cells/mouse. Eight days later, the mice were i.p. injected with 3 × 106 pfu of either Baco-1 or FusOn-H2 or PBS (control) at a site distant from that of tumor cell implantation. At the time of injection, animals lacked any sign of ascites, but they had either visible or microscopic tumors in the peritoneal cavity.
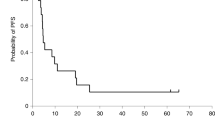
This injection was repeated at the same dose 1 week later. Results from the PBS control group (Figure 4, PBS) showed that implantation of these tumor cells in the specified quantify leads to the formation of disseminated metastatic tumor nodules. On average, there were more than 15 tumor nodules in each mouse, and the tumors from each mouse weighed more than 1 g. Direct injection of FusOn-H2 into the peritoneal cavity produced a highly significant therapeutic effect, completely eradicating all tumor nodules in seven of eight mice (Figure 4, FusOn-H2). The one mouse that was not tumor-free had only a single nodule. Although Baco-1 showed significant oncolytic activity by comparison with the PBS control (Figure 4, also Table 1, P<0.01), it was clearly less effective than FusOn-H2, in terms of both the percentage of tumor-free animals (12.5 vs 87.5%, P<0.01) and the weight of the remaining tumor nodules (0.7±0.4 g vs 0.02±0.05 g, P<0.01). These results clearly demonstrate the ability of FusOn-H2 to eradicate or control metastatic ovarian cancer established in the peritoneal cavity of mice, even when it is administered with limited frequency and in a very moderate dose.
Therapeutic effect of FusOn-H2 against metastatic human ovarian cancer xenografts established in the peritoneal cavity of nude mice. Human ovarian cancer xenografts were established by i.p. inoculation of 2 × 106 SKOV3 cells into the peritoneal cavity (n=eight mice per treatment group). Eight and 15 days after tumor cell inoculation, the mice received an i.p. injection of oncolytic HSVs at a dose of 3 × 106 pfu, at a site distant from the tumor implantation site. Four weeks after the initial virus injection (i.e., 5 weeks after tumor cell implantation), the mice were euthanized. Tumor nodules in the abdomen cavity were examined, counted and excised. The photos show the gross appearance of the excised tumor nodules.
FusOn-H2 toxicity in vivo
Our previous data showed that FusOn-H2 could not replicate in normal nondividing cells such as primary hepatocytes,16 indicating that it is probably a safe oncolytic agent for in vivo use. To assess its toxicity in vivo more extensively, we injected the virus systemically (via the tail vein) into immune-competent Balb/c mice at two different doses: 1 × 106 and 1 × 107 pfu. We included the parental wt HSV-2 as a control, but in doses 2 logs lower than that used with FusOn-H2. Toxicity was assessed by two criteria: mortality and liver function measured by monitoring levels of alanine transaminase (ALT) and aspartate transaminase (AST) activity in blood samples collected at different times after virus administration. Liver function was chosen as an endpoint because oncolytic HSV particles are distributed to the liver after systemic delivery,21, 22 and infection of both human and murine liver by HSV can cause hepatitis.23, 24 All animals receiving the wt HSV-2 died before day 10 after virus injection, in contrast to the survival of the entire group receiving FusOn-H2, even at significantly high doses (Table 2). When autopsied, the animals killed by wt HSV-2 had extensive gross necrotic foci in their livers, whereas in mice euthanized at day 4 after FusOn-H2 administration, the livers appeared normal (Figure 5a). Histologic examination of liver tissue sections confirmed these gross observations. Hepatic structures from FusOn-H2-treated mice were intact with no obvious cytopathic effects, whereas liver tissue from wt HSV-2-treated mice showed extensive necrosis and complete destruction of structural elements (Figure 5b). Immunohistochemical staining revealed widespread evidence of viral antigen in liver treated with wt virus but only a few positive cells in liver from FusOn-H2-treated mice (Figure 5b).
Evaluation of the in vivo toxicity of FusOn-H2. Eight-week-old immune-competent Balb/c mice were systemically injected (via the tail vein) with either FusOn-H2 or wt HSV-2 (labeled as HSV-2) at different doses (n=8 mice per group). (a) Photographs showing the gross appearance of a typical liver from mice dying at day 3 after wt HSV-2 inoculation and mice receiving FusOn-H2 that were euthanized at day 4 after virus inoculation. (b) H&E staining and immunohistochemical staining (using rat anti-HSV polyclonal antibody as the first antibody and FITC-conjugated goat anti-rat IgG as the second antibody) of tissue sections prepared from the livers shown in (a) Original magnification × 200.
In blood samples collected periodically during the first month after administration of FusOn-H2, there was only a slight increase of ALT and AST levels on day 3 post-treatment that returned to normal by the next test interval and remained there throughout the study period. By contrast, blood collected on day 3 after wt virus administration (samples were not collected at later time points as all mice died before day 10) showed a significant increase in both ALT and AST (more than 20-fold and 10-fold, respectively, P<0.01) by comparison with the pretreatment enzyme levels (Table 3). These data indicate that FusOn-H2 had little toxicity in the liver after systemic delivery.
Finally, we injected the viruses into the brains of immune-competent mice through stereotactic injection, again using two different doses and the parental wt virus as a control. Animal mortality was recorded up to 58 weeks after virus administration (Table 2). All animals receiving an intracranial injection of wt HSV-2 at the dose of either 1 × 104 or 1 × 105 pfu died within 1 week, whereas those receiving FusOn-H2 at 1 × 106 pfu survived for the duration of the experiment. One animal from the group injected with FusOn-H2 at a 10-fold higher dose (107 pfu) died on day 7 after virus administration; the rest of the animals in this group survived until the end of the experiment.
Discussion
Widespread metastasis of established primary tumors is the major factor contributing to cancer-related deaths. Patients with late-stage ovarian cancer often incur peritoneal invasion of tumor cells, usually contributing directly to their death. Hence, the peritoneal model of metastatic ovarian cancer we used in this study appears highly relevant to the clinical course of this malignant disease. Because of the relatively confined space it occupies and its ready accessibility for therapeutic intervention, the peritoneal cavity also represents an especially attractive site for investigative virotherapy. In our previous studies,6 we used the human ovarian cancer cell line Hey8 to establish ovarian tumor xenografts in the peritoneal cavity for evaluation of potentially useful oncolytic viruses. Implantation of Hey8 cells led to the formation of fewer (1 or 2) but larger tumor nodules in the peritoneal cavity than did implantation of SKOV3 cells, which led to widespread dissemination of relatively small tumor nodules across the pelvic and abdominal surfaces, more closely resembling the clinical scenario. In the present study, two injections of FusOn-H2 at a moderate dose into the peritoneal cavity produced a clear antitumor effect, leading to complete eradication of metastases in over 87% of the animals. In sharp contrast, treatment with Baco-1, an oncolytic virus derived from HSV-1, yielded only a modest antitumor effect (one tumor-free mouse among eight tested). These results indicate that FusOn-H2 is an effective oncolytic agent for the treatment of metastatic human ovarian cancer in the peritoneal cavity.
What could account for the superior oncolytic effect of this HSV-2-derived virus? FusOn-H2, but not its parental wt virus, showed a clear fusogenic phenotype in the human breast cancer cell line MDA-MB-435.16 Phenotypic characterization of this virus, wt186 and Baco-1, an HSV-1-based virus, on SKOV3 cells at 24 h after infection demonstrated syncytia formation by FusOn-H2 only, although by 48 h wt186 also induced weak cell-membrane fusion. As neither Baco-1 nor its wt HSV-1 parent was fusogenic in these cells6 it appears that HSV-2 is probably inherently more fusogenic than HSV-1 in this human ovarian cancer cell line and that the mutagenesis procedure for the deletion of the PK domain enhanced the fusogenic property of the virus. Work by us and others has demonstrated that incorporation of cell membrane fusion activity into an oncolytic virus can significantly enhance its antitumor effect,19, 25 hence we attribute the potent antitumor activity of FusOn-H2 in this metastatic ovarian cancer model, at least in part, to the presence of a fusogenic property related to deletion of the PK domain from the parental HSV-2 virus.
Although the genomes of HSV-1 and HSV-2 are largely collinear and their sequences share a high homology, there are certain differences among the functions of the gene products. For example, several proteins encoded by HSV-2, including the secreted form of glycoprotein G and the virion host shutoff protein, but not their counterparts in HSV-1, are involved in evading the host's innate immunity against viral infection.26, 27 Both NK cells and interferons are key components of the host's innate immunity, which plays a crucial role in controlling HSV infection.28, 29, 30 Thus, the HSV-2-derived FusOn-H2 mutant might have gained a therapeutic advantage over its HSV-1 counterpart (Baco-1) by virtue of mechanisms that protect it from the innate immune response of the host. This would help to explain the observation that FusOn-H2 had significantly better antitumor efficacy than Baco-1, even though its replication capacity in tumors was about 1 log lower.
The replication capacity of FusOn-H2 depends not only on the proliferative status of the host cell, as do HSV-1-based oncolytic viruses, but also on the activation status of the Ras signaling pathway. Although Ras gene mutations in ovarian cancer cells are not common, the Ras signaling pathway in such cells is frequently activated through other mechanisms, such as phosphoinositide-3 kinase or protein kinase B upregulation,31, 32 making ovarian cancer an attractive target for FusOn-H2 treatment. Indeed, by exploiting both Ras signaling and cell-cycle status for its oncolytic activity, FusOn-H2 would be expected to show enhanced tumor cell-specificity and thus increased safety in patients with ovarian cancer, a prediction that is supported by the in vivo toxicity data collected after systemic and intracranial inoculations of FusOn-H2. Administration of the virus by either route at a relatively large dose (up to 1 × 107 pfu) was considerately less toxic than the parental wt virus given at a much lower dose, and was well-tolerated by the animals. These results indicate that FusOn-H2 is severely attenuated as compared with its parental wt186 virus and likely retains the safety profile of a conventional oncolytic HSV.
References
Greenlee RT, Hill-Harmon MB, Murray T, Thun M . Cancer statistics, 2001. CA Cancer J Clin 2001; 51: 15–36.
Landis SH, Murray T, Bolden S, Wingo PA . Cancer statistics, 1999. CA Cancer J Clin 1999; 49: 8–31.
Martuza RL, Malick A, Markert JM, Ruffner KL, Coen DM . Experimental therapy of human glioma by means of a genetically engineered virus mutant. Science 1991; 252: 854–856.
Mineta T, Rabkin SD, Yazaki T, Hunter WD, Martuza RL . Attenuated multi-mutated herpes simplex virus-1 for the treatment of malignant gliomas. Nat Med 1995; 1: 938–943.
Coukos G, Makrigiannakis A, Montas S, Kaiser LR, Toyozumi T, Benjamin I et al. Multi-attenuated herpes simplex virus-1 mutant G207 exerts cytotoxicity against epithelial ovarian cancer but not normal mesothelium and is suitable for intraperitoneal oncolytic therapy. Cancer Gene Ther 2000; 7: 275–283.
Nakamori M, Fu X, Meng F, Jin A, Tao L, Bast RCJ et al. Effective therapy of metastatic ovarian cancer with an oncolytic herpes simplex virus incorporating two membrane-fusion mechanisms. Clin Cancer Res 2003; 9: 2727–2733.
Randazzo BP, Kesari S, Gesser RM, Alsop D, Ford JC, Brown SM et al. Treatment of experimental intracranial murine melanoma with a neuroattenuated herpes simplex virus 1 mutant. Virology 1995; 211: 94–101.
Andreansky SS, He B, Gillespie GY, Soroceanu L, Markert J, Chou J et al. The application of genetically engineered herpes simplex viruses to the treatment of experimental brain tumors. Proc Natl Acad Sci USA 1996; 93: 11313–11318.
Mineta T, Rabkin SD, Martuza RL . Treatment of malignant gliomas using ganciclovir-hypersensitive, ribonucleotide reductase-deficient herpes simplex viral mutant. Cancer Res 1994; 54: 3963–3966.
Martuza RL . Act locally, think globally. Nat Med 1997; 3: 1323.
Alemany R, Gomez-Manzano C, Balague C, Yung WK, Curiel DT, Kyritsis AP et al. Gene therapy for gliomas: molecular targets, adenoviral vectors, and oncolytic adenoviruses. Exp Cell Res 1999; 252: 1–12.
Pennisi E . Will a twist of viral fate lead to a new cancer treatment? Science 1996; 274: 342–343.
Chung TD, Wymer JP, Smith CC, Kulka M, Aurelian L . Protein kinase activity associated with the large subunit of herpes simplex virus type 2 ribonucleotide reductase (ICP10). J Virol 1989; 63: 3389–3398.
Smith CC, Nelson J, Aurelian L, Gober M, Goswami BB . Ras-GAP binding and phosphorylation by herpes simplex virus type 2 RR1 PK (ICP10) and activation of the Ras/MEK/MAPK mitogenic pathway are required for timely onset of virus growth. J Virol 2000; 74: 10417–10429.
Farassati F, Yang AD, Lee PW . Oncogenes in Ras signalling pathway dictate host-cell permissiveness to herpes simplex virus 1. Nat Cell Biol 2001; 3: 745–750.
Fu X, Tao L, Cai R, Prigge J, Zhang X . A Mutant Type 2 Herpes Simplex Virus Deleted for the Protein Kinase Domain of the ICP10 Gene Is a Potent Oncolytic Virus. Mol Ther 2006; 13: 882–890.
Fu X, Tao L, Jin A, Vile R, Brenner M, Zhang X . Expression of a fusogenic membrane glycoprotein by an oncolytic herpes simplex virus provides potent synergistic anti-tumor effect. Mol Ther 2003; 7: 748–754.
Saeki Y, Ichikawa T, Saeki A, Chiocca EA, Tobler K, Ackermann M et al. Herpes simplex virus type 1 DNA amplified as bacterial artificial chromosome in Escherichia coli: rescue of replication-competent virus progeny and packaging of amplicon vectors [In Process Citation]. Hum Gene Ther 1998; 9: 2787–2794.
Fu X, Zhang X . Potent systemic antitumor activity from an oncolytic herpes simplex virus of syncytial phenotype. Cancer Res 2002; 62: 2306–2312.
Chen SH, Shine HD, Goodman JC, Grossman RG, Woo SL . Gene therapy for brain tumors: regression of experimental gliomas by adenovirus-mediated gene transfer in vivo. Proc Natl Acad Sci USA 1994; 91: 3054–3057.
Schellingerhout D, Bogdanov Jr A, Marecos E, Spear M, Breakefield X, Weissleder R . Mapping the in vivo distribution of herpes simplex virions. Hum Gene Ther 1998; 9: 1543–1549.
Wood M, Perrotte P, Onishi E, Harper ME, Dinney C, Pagliaro L et al. Biodistribution of an adenoviral vector carrying the luciferase reporter gene following intravesical or intravenous administration to a mouse. Cancer Gene Ther 1999; 6: 367–372.
Ulbricht A, Farber I, Wutzler P . Herpes simplex virus hepatitis in mice: effects of treatment with trisodium phosphonoformate. Acta Virol 1985; 29: 493–498.
Goodman ZD, Ishak KG, Sesterhenn IA . Herpes simplex hepatitis in apparently immunocompetent adults. Am J Clin Pathol 1986; 85: 694–699.
Ebert O, Shinozaki K, Kournioti C, Park MS, Garcia-Sastre A, Woo SL . Syncytia induction enhances the oncolytic potential of vesicular stomatitis virus in virotherapy for cancer. Cancer Res 2004; 64: 3265–3270.
Su HK, Eberle R, Courtney RJ . Processing of the herpes simplex virus type 2 glycoprotein gG-2 results in secretion of a 34,000-Mr cleavage product. J Virol 1987; 61: 1735–1737.
Duerst RJ, Morrison LA . Herpes simplex virus 2 virion host shutoff protein interferes with type I interferon production and responsiveness. Virology 2004; 322: 158–167.
Ashkar AA, Rosenthal KL . Interleukin-15 and natural killer and NKT cells play a critical role in innate protection against genital herpes simplex virus type 2 infection. J Virol 2003; 77: 10168–10171.
Grubor-Bauk B, Simmons A, Mayrhofer G, Speck PG . Impaired clearance of herpes simplex virus type 1 from mice lacking CD1d or NKT cells expressing the semivariant V alpha 14-J alpha 281 TCR. J Immunol 2003; 170: 1430–1434.
Ahmad A, Sharif-Askari E, Fawaz L, Menezes J . Innate immune response of the human host to exposure with herpes simplex virus type 1: in vitro control of the virus infection by enhanced natural killer activity via interleukin-15 induction. J Virol 2000; 74: 7196–7203.
Patton SE, Martin ML, Nelsen LL, Fang X, Mills GB, Bast Jr RC et al. Activation of the ras-mitogen-activated protein kinase pathway and phosphorylation of ets-2 at position threonine 72 in human ovarian cancer cell lines. Cancer Res 1998; 58: 2253–2259.
Downward J . Targeting RAS signalling pathways in cancer therapy. Nat Rev Cancer 2003; 3: 11–22.
Acknowledgements
We thank Dr Lawrence Stanberry (University of Texas Medical Branch, Galveston, TX) for providing the wild-type HSV-2 strain 186, and John Gilbert for critical reading of this paper. This work was supported in part by a grant from Department of Defense Ovarian Cancer Research Program (DAMD17-03-1-0434).
Grant support: Department of Defense Ovarian Cancer Research Program (DAMD17-03-1-0434).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fu, X., Tao, L. & Zhang, X. An oncolytic virus derived from type 2 herpes simplex virus has potent therapeutic effect against metastatic ovarian cancer. Cancer Gene Ther 14, 480–487 (2007). https://doi.org/10.1038/sj.cgt.7701033
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cgt.7701033
Keywords
This article is cited by
-
IL-12 Expressing oncolytic herpes simplex virus promotes anti-tumor activity and immunologic control of metastatic ovarian cancer in mice
Journal of Ovarian Research (2016)
-
Designing herpes viruses as oncolytics
Molecular Therapy - Oncolytics (2015)
-
Advance in herpes simplex viruses for cancer therapy
Science China Life Sciences (2013)
-
Construction of an Oncolytic Herpes Simplex Virus That Precisely Targets Hepatocellular Carcinoma Cells
Molecular Therapy (2012)
-
Virotherapy induces massive infiltration of neutrophils in a subset of tumors defined by a strong endogenous interferon response activity
Cancer Gene Therapy (2011)