Abstract
Background:
STX2484 is a novel non-steroidal compound with potent anti-proliferative activity. These studies aimed to identify STX2484’s mechanism of action, in vivo efficacy and activity in taxane-resistant breast cancer models.
Methods:
Effects of STX2484 and paclitaxel on proliferation, cell cycle and apoptosis were assessed in vitro in drug-resistant (MCF-7DOX) and non-resistant cells (MCF-7WT). STX2484 efficacy in βIII tubulin overexpression in MCF-7 cells was also determined. Anti-angiogenic activity was quantified in vitro by a co-culture model and in vivo using a Matrigel plug assay. An MDA-MB-231 xenograft model was used to determine STX2484 efficacy in vivo.
Results:
STX2484 is a tubulin disruptor, which induces p53 expression, Bcl2 phosphorylation, caspase-3 cleavage, cell cycle arrest and apoptosis. In addition, STX2484 is a potent anti-angiogenic agent in vitro and in vivo. In breast cancer xenografts, STX2484 (20 mg kg−1 p.o.) suppressed tumour growth by 84% after 35 days of daily dosing, with limited toxicity. In contrast to paclitaxel, STX2484 efficacy was unchanged in two clinically relevant drug-resistant models.
Conclusions:
STX2484 is an orally bioavailable microtubule-disrupting agent with in vivo anti-angiogenic activity and excellent in vivo efficacy with no apparent toxicity. Crucially, STX2484 has superior efficacy to paclitaxel in models of clinical drug resistance.
Similar content being viewed by others
Main
Microtubule-targeting agents, such as the taxanes and Vinca alkaloids, are widely used in the treatment of solid tumours, including those of the ovary, prostate and breast, as they selectively target rapidly dividing cells. However, their activity is offset by dose-limiting side effects including neutropenia and neurotoxicity. In addition, some of these drugs also provoke hypersensitivity reactions triggered by the presence of non-ionic surfactant, Cremophor EL, in the formulation. The toxic nature of these compounds means that the optimal anti-tumour dose can only be given intermittently, with a requirement for treatment holidays, thus allowing time for tumour regrowth and drug resistance to develop (Gelderblom et al, 2001; Ring and Ellis, 2005; Mielke et al, 2006).
Drug resistance is a major problem in the effective treatment of breast cancer. Many patients have intrinsic resistance to the taxanes, and even those that do initially respond will eventually acquire resistance to this class of compounds, resulting in disease progression. Clinically, resistance to microtubule-targeting agents is most likely multi-faceted and can be mediated by overexpression of P-glycoprotein, a drug efflux pump (Fojo and Menefee, 2005), overexpression of class III β-tubulin (Burkhart et al, 2001) and tubulin post-translational modifications (Orr et al, 2003). Thus, development of compounds that can hit multiple targets to overcome these drug-resistant mechanisms is a key goal for new drug development.
The current drive for targeted therapies is potentially masking the real need for new cytotoxic agents, as to date all FDA approvals for targeted therapy for breast cancer are in conjunction with/adjunct to a traditional cytotoxic agent. Monotherapy with targeted agents has had minimal effect on survival rates, and their addition to cytotoxic regimes only has a marginal advantage (Normanno et al, 2009). Therefore, there remains an unmet need to develop new cytotoxic agents with an improved toxicity profile, better solubility and less susceptibility to drug-resistant mechanisms to partner new targeted agents. One such new drug class is the epothilones, which are potent microtubule disruptors with efficacy in drug-resistant cell lines in vitro (Hunt, 2009). The lead epothilone, Ixabepilone, has been approved by the FDA for use in taxane-refractory metastatic breast cancer (Cigler and Vahdat, 2008). However, this drug still requires a Cremophor-based infusion and its approval in Europe is delayed owing to concerns regarding the levels of neuropathy seen in the clinical trials (Cavaletti, 2009). To overcome this problem, the epithilone analogue, UTD1 was synthesised and showed better results than the latter in the phase I clinical trial in solid tumours, particularly in terms of myelosuppression (Zhang et al, 2011). A less advanced class of compounds is the steroidal sulphamoylated compounds; the lead compound, 2-methoxyoestradiol-3,17-O,O-bis-sulphamate, is still in pre-clinical development but has shown potent anti-cancer activities both in vitro and in vivo (Chander et al, 2007; Raobaikady et al, 2005; Newman et al, 2008; Day et al, 2009; Meyer-Losic et al, 2013).
We have previously synthesised a novel class of non-steroidal compounds combining reduced toxicity, improved solubility, ease of synthesis and activity in clinically relevant models of drug resistance (Leese et al, 2010). Preliminary in vitro proliferation assays have identified 2-(3,4,5-trimethoxybenzyl)-6-O-sulphamoyl-7-methoxy-1,2,3,4-tetrahydroisoquinoline (STX2484) as a potential pre-clinical lead for this class of compounds. Therefore, the aims of this study were to identify the primary mechanism(s) of action of this compound, to assess its in vivo efficacy in a breast cancer xenograft model, and crucially, to look for activity in clinically relevant drug-resistant models of breast cancer.
Materials and methods
Drug synthesis
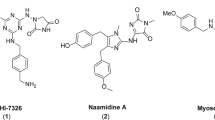
STX2484 was synthesised as described (Leese et al, 2010). The compound exhibited spectroscopic and analytical data in accordance with its structure (Figure 1) and was pure, as determined by high-performance liquid chromatography. This compound was tested together with the known microtubule-stabilising agent, paclitaxel (Sigma, Poole, UK).
Cell culture
Oestrogen receptor-positive (ER+ve) human breast cancer MCF-7 cells and ER-negative (ER−ve) human breast cancer MDA-MB-231 cells were obtained from the American Type Culture Collection (LGC Promochem, Teddington, UK) and used within 20 passages, but were not authenticated. MCF-7DOX cells were kindly donated by Dr GL Scheffer (Department of Pathology, Free University Hospital, Amsterdam, The Netherlands). Cells were routinely cultured in RPMI 1640 medium supplemented with 10% (v/v) fetal calf serum, 2 mM L-glutamine, 1% non-essential amino acids and 0.075% sodium bicarbonate from Sigma. Human umbilical vein endothelial cells (HUVECs) were obtained from TCS Cellworks (Claydon, UK) and maintained in a large vessel of endothelial medium supplemented with basic fibroblast growth factor/heparin, epidermal growth factor and cortisol in the presence of amphotericin/gentomycin (TCS Cellworks). All cells were cultured at 37 °C under 5% CO2 in a humidified incubator. HUVECs were used up to passage 10.
Cell proliferation
To ascertain IC50 values, 5000 cells, in their appropriate growth medium, were added to each well of a 96-well microtitre plate (BD Biosciences, Cowley, UK). Plates were incubated for 4–5 h at 37 °C in a 5% CO2 humidified atmosphere before addition of compounds. All compounds were dissolved at 10−2 M in tetrahydrofuran (THF) and added to the cells with a final concentration of 0.1% or less THF. As MCF-7 and MDA-MB-231 cells have a similar doubling time of about 30 h, these assays were done in parallel and the cells were exposed to inhibitors for the same time. Cells were grown in the absence or presence of the compounds for 4 days after which, 10 μl per well of Alamar Blue (Biosource, Camarillo, CA, USA) was added and incubated for 2 h. Fluorescence was quantified using a FluoStar Optima Plate reader (544 nm excitation, 590 nm emission; BMG Labtech, Aylesbury, UK).
Tubulin polymerisation assay
The polymerisation of purified bovine brain tubulin (99% purity) was monitored using the Tubulin Polymerization Assay Kit from CytoDYNAMIX (Screen 03, Cytoskeleton Inc., Denver, CO, USA; Shelanski et al, 1973; Lee and Timasheff, 1977). Briefly, tubulin polymerisation driven by guanosine triphosphate (GTP) and paclitaxel was monitored spectrophotometrically by the change in absorbance at 350 nm. The absorbance was measured at 1-min intervals for 60 min using a Victor spectrophotometer (Perkin-Elmer, Buckinghamshire, UK).
Tubulin-competitive-binding assay
The competitive-colchicine-binding assay is based on a scintillation proximity assay technology using bovine brain tubulin, which has been modified so that random surface lysines contain a covalently linked, long-chain biotin derivative (CytoDYNAMIX screen 15, Cytoskeleton Inc.). Briefly, 10 μl of each compound was added to a well of a 96-well plate (Low PB CorningCostar, Amsterdam, The Netherlands). Tritiated colchicine (100 μl; Perkin-Elmer; specific activity 70–80 Ci mmol−1) was added to 300 μl of tubulin-binding buffer and then 10 μl was added in each well. Premix tubulin–biotin–streptavidin scintillation proximity assay beads (180 μl; 4.4 mg streptavidin yttrium silicate beads are mixed into 15 ml buffer and incubated on a slow 10 r.p.m. rotator at 4 °C for 30 min; Amersham Bioscience, Little Chalfont, Buckinghamshire, UK) were added to each well for 3 h at 37 °C. The plates were then read on a scintillation counter (Packard Instrument, Meriden, CT, USA; Topcount Microplate Reader) and the percentage of inhibition was calculated (Tahir et al, 2000).
Immunohistochemistry
MCF-7 and MDA-MB-231 cells grown on poly-L-lysine-coated coverslips were treated with 0.1 μ M STX2484 or paclitaxel for 24 h. The cells were fixed by placing them in methanol at −20 °C for 10 min, and then in ice-cold acetone for 30 s. The coverslips were rinsed and then rehydrated with PBS. To visualise the microtubules, cells were incubated for 1 h with the FITC-conjugated anti-β-tubulin (clone DM1A, Sigma) in PBS containing 1% BSA. Cells were washed twice with PBS, and the nuclei were counterstained with Hoechst 33 342 at 1 mg ml−1 (Sigma). Coverslips were mounted on slides using the DePex mounting medium (BDH Chemicals Ltd, Poole, UK), observed using a Zeiss (Carl Zeiss Ltd, Welwyn Garden City, UK) inverted microscope ( × 200) and analysed with the Axiovision imaging system (Imaging Associates, Bicester, UK).
Cell cycle analysis
Cells were seeded in T-25 flasks, incubated until 60–70% confluence and exposed to compounds at 0.5 μ M for 24 h, 48 h and 72 h. Cells were harvested, washed with PBS, pooled with the non-adherent cells and centrifuged for 5 min at 600 g. The cells were fixed in ice-cold 70% ethanol and stored at −20 °C for 48 h. After fixation, cells were suspended in 100 μl phosphate–citrate buffer (0.19 mol l−1 Na2HPO4 and 4 mmol l−1 citric acid (both from Sigma)) and incubated for 30 min at room temperature. Cells were then resuspended in 1 ml PBS (Lonza, Verviers, Belgium) containing 10 μg ml−1 propidium iodide (Sigma) and 10 μg ml−1 RNase A (Sigma). The propidium iodide-stained cell samples were analysed with a flow cytometer (FACSCalibur, Becton Dickinson, Oxford, UK) at 620 nm. Further DNA analysis was performed using MultiCycle AV software (Innovative Cell Technologies, San Diego, CA, USA).
Apoptosis analysis
Cells were seeded and treated as described for the cell cycle analysis. Cells and washings were pelleted by centrifugation at 600 g, washed twice with PBS and resuspended in 600 μl Annexin V-binding buffer (10 mM HEPES pH 7.4, 140 mM NaCl and 2.5 mM CaCl2). A 150-μl aliquot of the cell suspension was stained with 5 μl of propidium iodide (Invitrogen, Carlsbad, CA, USA) at 50 g l−1 and 4 μl of FITC-conjugated Annexin V antibody (BD Biosciences, San Jose, CA, USA). The apoptotic status of the cells was analysed using a FACSCalibur flow cytometer (Becton Dickinson). Cells undergoing apoptosis were defined as positive for Annexin V and negative for propidium iodide staining.
Immunoblotting
Cells were seeded in T-25 flasks at ∼2.5 × 105 cells per flasks in 4 ml of cell-specific media and exposed to compounds at 0.5 μ M for 24 h, 48 h or 72 h. Protein was prepared from treated cells using RIPA lysis buffer (Sigma) and quantified using the Bradford protein assay with Bradford reagent (Sigma). Equal amounts of protein were loaded in all wells (15 μg). Proteins were separated by electrophoresis through a 4–12% NuPAGE Bis-Tris gel (Invitrogen) and subsequently transferred to Hybond-P membrane (GE Healthcare, Buckinghamshire, UK).
Detection was carried out using anti-human cyclin B1 (ref. H433; Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA), phospho-Bcl2 (ref. 2827S; Cell Signaling Technology, Boston, MA, USA), caspase-3 (ref. 9665; Cell Signaling), GAPDH (ref. 2118; Cell Signaling) and p53 (ref. ab28-100; Abcam, Cambridge, UK) primary antibodies. Secondary alkaline phosphatase-conjugated anti-rabbit IgG (ref. 7054; Cell Signaling) or anti-mouse IgG (ref 7056; Cell Signaling) antibodies were used for detection in conjunction with a chemifluorescent substrate (ECF substrate, ref. RPN5785; GE Healthcare). Bands were visualised and quantified using a Storm imaging system (GE Healthcare).
In vitro angiogenesis assay
The effect of STX2484 on in vitro vessel formation was assessed using an angiogenesis kit (TCS Cellworks). For this assay, endothelial cells were cultured in a 24-well plate within a matrix of human diploid fibroblasts of dermal origin in an optimised medium supplied by TCS Cellworks. The co-cultured cells were incubated throughout the experiment at 37 °C under 5% CO2 in a humidified incubator. On day 1, the culture medium was removed and replaced with medium containing STX2484 at concentrations between 10 nM and 0.5 μ M, and VEGF at 2 ng ml−1 (TCS Cellworks). On days 4, 7 and 9, the medium was replaced with fresh medium containing STX2484 and VEGF. On day 11, the cells were washed with PBS and fixed with 1 ml 70% ethanol for 30 min. After fixation, the cells were washed with blocking buffer (1% BSA in PBS) and stained for CD31 in accordance with the manufacturer’s instruction (TCS Cellworks). The extent of vessel formation was then quantified using a high-resolution transmissive scanner (ScanMaker 9800, Microtek, Willich, Germany) as previously described (Newman et al. 2007).
In vivo angiogenesis assay
The anti-angiogenic potential of STX2484 was assessed using a modified Matrigel plug assay as previously described (Passaniti et al, 1992; Prewett et al, 1999; Chander et al, 2007). All experiments were carried out under conditions that complied with institutional guidelines. Female C57BL/6J mice (Harlan, Bicester, UK) were anaesthetised, placed on a heated pad (37 °C) and 0.5 ml of ice-cold Matrigel (BD Biosciences), supplemented with 500 ng of basic fibroblast growth factor (bFGF; R&D Systems, Oxford, UK), and injected subcutaneously into one flank of each mouse. Control mice received Matrigel without bFGF. Twenty-four hours after Matrigel injection the mice were divided into four treatment groups (n=5): vehicle (10% THF and 90% propylene glycol), bFGF+vehicle, bFGF+STX2484 (20 mg kg-1 p.o.) and bFGF+STX2484 (60 mg kg−1 p.o.), and animals were dosed consecutively for 4 days. Quantification of the blood vessels within the Matrigel plugs was facilitated through the i.v. injection of 100 μl of 0.25 mg ml−1 FITC-dextran (125 000 molecular weight; Sigma) 7 days after the Matrigel injection. The animals were culled 20 min after the FITC-dextran injection and Matrigel plugs were removed and photographed before being dissolved in 1 ml Dispase reagent (BD Biosciences) for 16 h at 37 °C. The resulting solution was centrifuged at 15 700 g at 20 °C for 30 s. The fluorescence of the supernatant was measured using a Fluostar Optima plate reader (BMG Labtech). The excitation and emission wavelengths were 480 nm and 520 nm, respectively. The fluorescence of the samples was quantitated using a standard curve of FITC-dextran (0.4–25 μg ml−1).
Xenograft models
Athymic female MF-1 nude mice (nu–/nu–) were purchased from Harlan at 5 weeks of age (∼20–25 g in weight). All experiments were carried out under conditions that complied with UK Home Office Animals (Scientific Procedures) Act 1986 and institutional guidelines. MDA-MB-231 cells (2 × 106) were inoculated subcutaneously into one flank of each animal. When tumours reached 100–150 mm3, mice were randomly divided into two treatment groups (n=6): vehicle (10% THF and 90% propylene glycol) or STX2484 (20 mg kg−1). All compounds were given orally, daily for 35 days. Throughout the study, mice were weighed and tumour measurements were taken on a weekly basis. Tumour volumes were calculated using the formula; volume=length × width2/2. For ethical reasons, animals were removed from the study if tumour mean diameter exceeded 1.5 cm, as recommended by Workman et al (2010).
Statistics
In vitro experiments were carried out in triplicate and data presented are representative of one of three such experiments. Unless specified, all errors shown are the mean±s.d. Student’s t-test was used to assess significance.
Results
Efficacy in drug-resistant models
STX2484 is a potent inhibitor of proliferation in both ER−ve and ER+ve breast cancer cell lines, with IC50 values of 0.27 μ M and 0.16 μ M in MCF-7WT and MDA-MB-231 cells, respectively (Table 1). In MCF-7DOX cells, which overexpress P-glycoprotein, STX2484 inhibited proliferation with an IC50 of 0.45 μ M, which is not significantly different to the IC50 in MCF-7WT cells (P>0.05; Table 1). The resistance factor, which reflects the fold increase in the drug-resistant cell line compared with the parental wild type, has previously been shown to be 1000 for paclitaxel in MCF-7DOX cells (Newman et al, 2007).
The efficacy of STX2484 and paclitaxel was also determined in cells under- or overexpressing class III β-tubulin (Stengel et al, 2010). Altering class III β-tubulin protein expression did not alter the efficacy of STX2484 significantly (P>0.05) in MCF-7 cells. In contrast, MCF-7 cells overexpressing class III β-tubulin were significantly less sensitive to paclitaxel, and the knockdown of class III β-tubulin significantly increased their sensitivity to paclitaxel (P<0.01; Table 1).
Microtubule disruption
Microtubule-destabilising agents, such as colchicine, can inhibit GTP- and paclitaxel-stimulated tubulin polymerisation in vitro, as measured by changes in turbidity (MacCarthy-Morrogh et al, 2000). GTP and paclitaxel were used at 10 μ M and mixed with STX2484. In this study, STX2484 significantly inhibited paclitaxel-stimulated tubulin polymerisation (53% inhibition, Figure 2A) and GTP-stimulated tubulin polymerisation (37% inhibition, Figure 2A). It has been shown that that drugs affecting tubulin polymerisation interact with tubulin either at the taxane-binding, Vinca-binding or colchicine-binding sites. The competition-binding scintillation proximity assay (Figure 2A) shows that STX2484 competitively inhibited [3H]colchicine binding on the purified brain bovine tubulin, suggesting that STX2484 directly interacts with tubulin by binding to the colchicine-binding domain. Used as negative controls, paclitaxel was not able to displace labelled colchicine (data not shown). Having demonstrated that STX2484 perturbs tubulin dynamics in a cell-free model, its effect on cytoskeletal and nuclear morphology were examined in vitro. MCF-7 and MDA-MB-231 cells were exposed to 0.1 μ M STX2484 for 24 h and subsequently processed for immunofluorescence microscopy. STX2484 was used at a low concentration compared with its IC50 values to observe STX2484 effect on the cytoskeleton without killing the cells. The exposure of MCF-7 and MDA-MB-231 cells to STX2484 resulted in marked effects on cell morphology and on microtubule structure. Microtubules, which extended throughout the cytoplasm of control cells (Figure 2B), had their integrity affected by STX2484 in both cell lines. Cells were rounded and there was a visible loss of microtubule structure in response to STX2484 treatment, with only diffused microtubule staining visible around nuclei. Untreated cells showed typical nuclear structures, whereas cells treated with STX2484 displayed condensed and fragmented nuclei, which are associated with apoptosis (Figure 2B).
Microtubule disruption. (A) Microtubule polymerisation assay. Tubulin assembly was measured by changes in turbidity. Tubulin was incubated with 10 μ M paclitaxel or GTP in the presence or absence of 10 μ M STX2484 at 37 °C. The change in absorbance was continuously monitored at 350 nm for 40 min. For competitive-colchicine-binding site studies, STX2484 was tested at 10 μ M and the reference compounds paclitaxel and colchicine were tested at 10 μ M. Each point represents the mean±s.d. of three independent experiments. (B) Fluorescent images of MCF-7 and MDA-MB-231 cells after drug exposure. Cells were treated for 24 h with 0.1 μ M STX2484 and stained with FITC-conjugated anti-tubulin antibody (tubulin) and Hoechst (nucleus). This low dose, compared with IC50 values, was used to observe STX2484 effect on the cytoskeleton without killing the cells. Images were taken using a Zeiss inverted microscope under × 200 magnification.
Cell cycle/apoptosis
To further investigate the potential apoptotic effects of STX2484, FACS analysis was undertaken. As STX2484 has efficacy in the MCF-7DOX P-glycoprotein+ve cell line, this was included in these experiments. STX2484 and paclitaxel were used at the same dose for a direct comparison of efficacy in vitro. The dose selected was 0.5 μ M, which is approximately the IC50 value of STX2484 in both MCF-7WT cells and MCF-7DOX cells, and is 30-fold the IC50 value of paclitaxel in MCF-7WT cells; but this is not a dose that significantly affects the proliferation of MCF-7DOX cells (Newman et al, 2008).
The majority of untreated MCF-7WT cells (59.3%) were in the G1 phase, whereas those exposed to 0.5 μ M STX2484 or paclitaxel, 56.0% and 77.4% cells, respectively, were arrested in the G2/M phase, and only 13.7% (P=0.004) and 5.7% (P=0.022) cells were in the G1 phase, respectively, after 48 h treatment (Figure 3A). The number of cells undergoing apoptosis was two-fold higher and 1.7-fold higher in response to STX2484 and paclitaxel, respectively, compared with untreated cells after 72 h (Figure 3B). In MCF-7DOX cells, paclitaxel failed to induce G2/M arrest and apoptosis, whereas STX2484 arrested cells in G2/M (25.8% cells in the G1 phase and 59.3% cells in the G2/M phase with P=0.006 and P=0.035, respectively, compared with control) and induced a two-fold increase in the number of cells undergoing apoptosis (Figures 3A and B).
Cell cycle and apoptosis. (A) Cell cycle arrest. Cells were exposed to STX2484 for 24 h before being trypsinised, fixed, treated with RNase, stained with propidium iodide and analysed. (B) Apoptosis. Cells were stained with FITC-conjugated Annexin V antibody and propidium iodide, and analysed by flow cytometry. Apoptotic cells were the cells positive for Annexin V and negative for propidium iodide. Results are shown as % apoptotic cells of total cells analysed. Each point represents the mean±s.d. of three independent experiments (*P<0.05). (C) Immunoblotting. Cells were exposed to STX2484 for 24, 48 and 72 h before being trypsinised. Total protein extracts were prepared and analysed by SDS–PAGE and immunoblotting with the appropriate antibodies as described in the Materials and Methods. Data shown represent one of three such experiments.
Proteins associated with the cell cycle and apoptosis were analysed to further investigate the mechanism of action of STX2484 in both MCF-7WT and MCF-7DOX cells. Protein extracts were prepared from MCF-7WT and MCF-7DOX cells treated with 0.5 μ M STX2484 or 0.5 μ M paclitaxel for 24, 48 and 72 h.
Cyclin B1 was only weakly expressed in untreated cells but was strongly induced in MCF-7WT cells after 24 h treatment with either STX2484 (15-fold vs MCF-7WT control) or paclitaxel (24-fold vs MCF-7WT control). STX2484 also strongly induced cyclin B1 in MCF-7DOX cells (12-fold vs MCF-7DOX control); in contrast, only a limited induction was seen after 24 h treatment with paclitaxel (five-fold vs MCF-7DOX control). Cyclin B1 protein expression returned to baseline after 48 h in both cell lines (Figure 3C). In MCF-7WT cells treated with either STX2484 or paclitaxel, p53 protein expression increased after 24 h (three-fold and five-fold vs MCF-7WT control, respectively). In MCF-7DOX cells, STX2484 increased p53 expression but little increase was seen in response to paclitaxel (three-fold and 1.5-fold, respectively, vs MCF-7DOX control; Figure 3C). Phosphorylation of Bcl2 protein negates its anti-apoptotic activity and allows apoptosis to occur via the mitochondrial pathway. In this study, both STX2484 and paclitaxel strongly induced the phosphorylation of Bcl2 in MCF-7WT cells after 24 h (six-fold and 10-fold, respectively, vs MCF-7WT control), but only STX2484 strongly induced Bcl2 phosphorylation in MCF-7DOX cells (14-fold vs MCF-7DOX control; Figure 3C). Caspase-3, which is activated by cleavage, has an important role in the apoptotic response. Both STX2484 and paclitaxel induced caspase-3 cleavage after 24 h treatment in MCF-7WT, but only STX2484 induces caspase-3 cleavage in MCF-7DOX (Figure 3C). To ensure equal protein loading and successful transfer, the housekeeping protein GAPDH was used as a loading control and its detection showed steady expression.
Anti-angiogenic activity
As STX2484 is a potent inhibitor of HUVEC proliferation (Table 1), its ability to inhibit angiogenesis was assessed both in vitro and in vivo. In vitro, a co-culture model was used in which endothelial cells are cultured with fibroblasts in 24-well plates. Representative high-resolution scans of the wells show STX2484 completely and partially inhibited vessel formation at 500 nM and 100 nM, respectively (Figure 4A). Quantification of vessel formation revealed that STX2484 significantly inhibited vessel formation by 92.4% at 500 nM (P<0.001), 20% at 100 nM (P<0.01), 20% at 50 nM (P<0.01) and 26% at 20 nM (P<0.01). No significant effect was seen at 10 nM (Figure 4B).
Angiogenesis inhibition. (A and B) In vitro angiogenesis. Co-cultures of fibroblasts and endothelial cells were treated for 11 days in presence of VEGF at 2 ng ml−1. The cells were scanned and processed with Photoshop. The number of newly formed tubules was determined with the Angiosys software. Each point represents the mean±s.d. of three independent experiments (*P<0.05; **P<0.01; ***P<0.001). (C) In vivo angiogenesis. The inhibition of angiogenesis in the C57BL/6J mouse Matrigel plug-based model shows the extent of vascularisation after the mice had received the following treatments: control, bFGF only (1 ng ml−1), bFGF and STX2484 (20 mg kg−1 p.o.) and bFGF and STX2484 (60 mg kg−1 p.o.). The plugs were subsequently dissolved with Dispase and the fluorescence of the FITC-dextran was used to quantify the extent of angiogenesis. Data represent mean±s.d., n=5. The bFGF-only group was compared with control (a) and each drug treatment was compared with the bFGF-only group for statistical significance (***P<0.001).
The anti-angiogenic activity of STX2484 in vivo was tested in mice using a Matrigel plug assay (Passaniti et al, 1992; Prewett et al, 1999). The addition of bFGF (1 ng ml−1) to the Matrigel caused a marked increase in vascularisation, and quantification of angiogenesis showed a two-fold (P<0.001) increase in fluorescence in response to bFGF (Figure 4C). Plugs removed from animals dosed with STX2484 (20 or 60 mg kg−1 p.o.) for 4 days showed a marked reduction in the level of neovascularisation compared with bFGF alone. The formation of new blood vessels was significantly (P<0.001) inhibited by both 20 mg kg−1 p.o. and 60 mg kg−1 p.o. STX2484 compared with Matrigel plugs that received bFGF in non-STX2484-dosed animals.
In vivo efficacy
An MDA-MB-231 breast cancer xenograft model was used to assess the efficacy of STX2484 in vivo. Tumours in untreated mice increased by ∼2400% in size (2429±329%, Figure 5A) over 28 days, whereas dosing with STX2484 (20 mg kg−1 p.o., daily) reduced tumour size by 84% compared with control-treated (10% THF and 90% PG) mice at this time point (413±166%; P<0.001; Figure 5A). Owing to large tumour volumes, and to comply with published guidelines on animal welfare in cancer research (Workman et al, 2010), all mice in the control group were removed from the study after 28 days. After 35 days of treatment, xenograft volumes in STX2484-treated animals were still suppressed. No significant weight loss was observed in the STX2484-treated group, perhaps indicating a favourable toxicological profile for this compound (Figure 5A inset).
Inhibition of MDA-MB-231 tumour growth in a xenograft model in nude mice. Mice were treated daily for 28 days with STX2484 at 20 mg kg−1 p.o. Points show mean percentage change in tumour volume or mouse weight (n=6–9); bars=s.e.m. (**P<0.01, ***P<0.001; compared with control). No significant reduction in animal weight was observed as compared with day 0 (inset).
Discussion
Microtubule-targeting agents are widely used in the clinic to treat a variety of solid and haematological cancers (Jordan and Wilson, 2004). However, their efficacy is compromised by resistance mechanisms, and their dosing is often limited by severe toxicity. Therefore, there remains an unmet need for new therapies that are active against treatment-refractory tumours and have a more favourable toxicity profile. We demonstrate here one such candidate, STX2484, a novel non-steroidal compound, which has previously shown potent in vitro anti-proliferative activity in preliminary screening assays.
The multiple methoxy groups and sulphamate group within the structure of STX2484 strongly suggest that this compound may interact with microtubules in a similar fashion to colchicine and 2-methoxyoestradiol-3,17-O,O-bis-sulphamate (Kumar 1981; Newman et al, 2007). To investigate this, STX2484 was tested in the paclitaxel-stimulated tubulin polymerisation assay, and like both colchicine and 2-methoxyoestradiol-3,17-O,O-bis-sulphamate, STX2484 blocked GTP- and paclitaxel-stimulated tubulin polymerisation, and furthermore was a competitive inhibitor at the colchicine-binding site of tubulin. Further evidence of STX2484 targeting microtubules can be seen from its marked effect on the cellular microtubule structure.
It was also anticipated that STX2484 would induce apoptosis as observed in cells treated with related compounds (Foster et al, 2008). The DNA profile obtained with propidium iodide showed cells in G1, S and G2/M phases, with apoptotic and dead cells being represented by a sub G0/G1 population. However, in order to be seen in the sub-G1 area, a cell must have lost enough DNA to appear there; so if cells enter apoptosis from the S or G2/M phase of the cell cycle, they may not appear in the sub-G1 peak. This may explain the small difference comparing the sub-G1 peak of STX2484- and paclitaxel-treated MCF-7DOX cells. Cells may be committed to die by apoptosis, but they have not lost enough DNA to be seen in the sub-G1 population.
The accumulation of cyclin B1 provokes mitotic catastrophe that induces apoptosis. In our case, the microtubule disruption caused by STX2484 led to cell cycle arrest in the G2/M phase with accumulation of cyclin B1 (24 h treatment). Cyclin B1 was then degraded (48 h treatment), and it is the absence of Cdk1/cyclin B1 activity that induces apoptosis (48 h treatment) as shown previously (Yuan et al, 2004). Further investigation revealed that STX2484 induced p53 protein expression and the cleavage of caspase-3. Moreover, as Cdk1/cyclinB1 can phosphorylate BCL2 to inhibit apoptosis, we showed the absence of phospho-BCL2 after 48 h treatment, which is consistent with the loss of cyclin B1 signal. This implies that tumour cells activate the intrinsic apoptosis pathway, although more work needs to be undertaken to confirm the nature and details of the apoptosis pathway induced by STX2484.
In addition to inducing apoptosis, STX2484 is a potent anti-angiogenic agent both in vitro and in vivo as shown by the lack of vessel formation in the co-culture model and the Matrigel plug assay. These two models are driven by different pro-angiogenic growth factors; bFGF drives the in vivo model and VEGF drives the in vitro model; despite this STX2484 was efficacious in both models. Inhibiting VEGF-stimulated angiogenesis alone by the use of bevacizumab (Avastin) has yielded disappointing clinical results to date (Normanno et al, 2009). This suggests there are multiple pathways involved in stimulating angiogenesis, and agents such as STX2484, which target more than one pathway, may have greater clinical potency (Gaur et al, 2009; Korc and Friesel, 2009).
Many microtubule disrupters and other chemotherapeutic agents have been investigated for potential anti-angiogenic activity by the use of ‘metronomic’ dosing schedules. The rationale behind this is that tumour-associated endothelial cells are sensitive to such drugs as they rapidly divide, and the vasculature that they are part of is immature and unstable (Kerbel and Kamen, 2004). However, owing to the highly toxic nature of these compounds, the dose used for regular metronomic dosing is far lower than the optimal ‘traditional’ intermittent anti-tumour dose. Although low-dose regular administration of such agents may have anti-angiogenic effects, the direct anti-tumour efficacy may be diminished. In this study, STX2484 was dosed orally for 35 consecutive days at the optimal anti-tumour dose (20 mg kg−1), which inhibited growth by 84% compared with control (at day 28) with no visible signs of toxicity. Although we used paclitaxel-sensitive MDA-MB-231 xenografts, this combination of regular oral dosing, anti-angiogenic activity and direct anti-tumour efficacy bodes well for the future development of STX2484 as a new generation cytotoxic agent. Future comparison of STX2484 vs paclitaxel in paclitaxel-resistant MCF-7DOX and MCF-7-TUBB3 xenografts will be critical to support these findings. Future experiments will also investigate STX2484’s safety profile and, as its structure is based on 2-MeOE2 and 2-methoxyoestradiol-3,17-O,O-bis-sulphamate, we anticipate that STX2484 will have a similar acceptable toxicity profile with no effect on plasma neutrophil concentrations (Meyer-Losic et al, 2013). Furthermore, as STX2484's core structure is based on 2-MeOE2, we will also investigate this compound's metabolism in vitro and in vivo; 17β-hydroxysteroid dehydrogenase type-2 activity is known to inactivate 2-MeOE2 and, also with extensive metabolic conjugation, is one of the main reasons for this compound's clinical failure and poor bioavailibility (Newman et al, 2006). STX2484 possesses no free hydroxyl groups and thus will not be a substrate for 17β-hydroxysteroid dehydrogenase type-2 nor for conjugating enzymes, giving it a clear advantage.
One of the major problems facing current cytotoxic agents, such as paclitaxel, is drug resistance, both intrinsic and acquired. Although many mechanisms of drug resistance have been described in vitro, such as tubulin point mutations, few have been demonstrated in clinical specimens (Kelley et al, 2001; Orr et al, 2003; Fojo and Menefee, 2005). Two mechanisms, which have been shown in the clinic, are the expression of a drug efflux pump, P-glycoprotein, and the overexpression of the βIII tubulin isoform (Burkhart et al, 2001; Orr et al, 2003). In this study, the efficacy of STX2484 was unaffected by either overexpression of P-glycoprotein or βIII tubulin; in contrast, paclitaxel was significantly less active in both models. If these data can be confirmed in future in vivo PK-PD pre-clinical models and in the clinic, this would potentially make STX2484 an extremely promising agent for the treatment of breast cancer.
In summary, the results of this study demonstrate that STX2484 is a potent anti-proliferative agent, which is active in taxane-resistant models of breast cancer. It acts as a microtubule-disrupting agent arresting cells in the G2/M phase with subsequent apoptosis. In addition, STX2484 is a potent inhibitor of angiogenesis both in vitro and in vivo. These activities, combined with excellent solubility and regular oral dosing, are reflected in the virtually complete inhibition of tumour growth in the MDA-MB-231 breast cancer xenograft model in this study.
Change history
15 July 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Burkhart CA, Kavallaris M, Band Horwitz S (2001) The role of beta-tubulin isotypes in resistance to antimitotic drugs. Biochim Biophys Acta 1471: 1–9.
Cavaletti G (2009) Chemotherapy-induced peripheral neurotoxicity: how can we improve knowledge? Lancet Oncol 10: 539–540.
Chander SK, Foster PA, Leese MP, Newman SP, Potter BVL, Purohit A, Reed MJ (2007) In vivo inhibition of angiogenesis by sulphamoylated derivatives of 2-methoxyoestradiol. Br J Cancer 96: 1368–1376.
Cigler T, Vahdat L (2008) Integrating epothilones into the treatment of patients with metastatic breast cancer: clinical perspectives on incorporating recent data in the practice setting. Clin Breast Cancer 8: S166–S170.
Day JM, Foster PA, Tutill HJ, Newman SP, Ho YT, Leese MP, Potter BVL, Reed MJ, Purohit A (2009) BCRP expression does not result in resistance to STX140 in vivo, despite the increased expression of BCRP in A2780 cells in vitro after long-term STX140 exposure. Br J Cancer 100: 476–486.
Fojo AT, Menefee M (2005) Microtubule targeting agents: basic mechanisms of multidrug resistance (MDR). Semin Oncol 32: S3–S8.
Foster PA, Ho YT, Newman SP, Kasprzyk PG, Leese MP, Potter BVL, Reed MJ, Purohit A (2008) 2-MeOE2bisMATE and 2-EtE2bisMATE induce cell cycle arrest and apoptosis in breast cancer xenografts as shown by a novel ex vivo technique. Breast Cancer Res Treat 111: 251–260.
Gaur P, Bose D, Samuel S, Ellis LM (2009) Targeting tumor angiogenesis. Semin Oncol 36: S12–S19.
Gelderblom H, Verweij J, Nooter K, Sparreboom A (2001) Cremophor EL: the drawbacks and advantages of vehicle selection for drug formulation. Eur J Cancer 37: 1590–1598.
Hunt JT (2009) Discovery of ixabepilone. Mol Cancer Ther 8: 275–281.
Jordan MA, Wilson L (2004) Microtubules as a target for anticancer drugs. Nat Rev Cancer 4: 253–265.
Kelley MJ, Li S, Harpole DH (2001) Genetic analysis of the beta-tubulin gene, TUBB, in non-small-cell lung cancer. J Natl Cancer Inst 93: 1886–1888.
Kerbel RS, Kamen BA (2004) The anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer 4: 423–436.
Korc M, Friesel RE (2009) The role of fibroblast growth factors in tumor growth. Curr Cancer Drug Targets 9: 639–651.
Kumar N (1981) Taxol-induced polymerization of purified tubulin. Mechanism of action. J Biol Chem 256: 10435–10441.
Lee JC, Timasheff SN (1977) In vitro reconstitution of calf brain microtubules: effects of solution variables. Biochemistry 16: 1754–1764.
Leese MP, Jourdan F, Kimberley MR, Cozier GE, Thiyagarajan N, Stengel C, Regis-Lydi S, Foster PA, Newman SP, Acharya KR, Ferrandis E, Purohit A, Reed MJ, Potter BVL (2010) Chimeric microtubule disruptors. Chem Commun 46: 2907–2909.
MacCarthy-Morrogh L, Townsend PA, Purohit A, Hejaz HAM, Potter BVL, Reed MJ, Packham G (2000) Differential effects of estrone and estrone-3-O-sulfamate derivatives on mitotic. Arrest, apoptosis, and microtubule assembly in human breast cancer cells. Cancer Res 60: 5441–5450.
Meyer-Losic F, Newman SP, Day JM, Reed MJ, Kasprzyk PG, Purohit A, Foster PA (2013) STX140, but not paclitaxel, inhibits mammary tumour initiation and progression in C3(1)/SV40 T/t-antigen transgenic mice. PLoS One 8: e80305.
Mielke S, Sparreboom A, Mross K (2006) Peripheral neuropathy: a persisting challenge in paclitaxel-based regimes. Eur J Cancer 42: 24–30.
Newman SP, Foster PA, Ho YT, Day JM, Raobaikady B, Kasprzyk PG, Leese MP, Potter BVL, Reed MJ, Purohit A (2007) The therapeutic potential of a series of orally bioavailable anti-angiogenic microtubule disruptors as therapy for hormone-independent prostate and breast cancers. Br J Cancer 97: 1673–1682.
Newman SP, Foster PA, Stengel C, Day JM, Ho YT, Judde JG, Lassalle M, Prevost G, Leese MP, Potter BVL, Reed MJ, Purohit A (2008) STX140 is efficacious in vitro and in vivo in taxane-resistant breast carcinoma cells. Clin Cancer Res 14: 597–606.
Newman SP, Ireson CR, Tutill HJ, Day JM, Parsons MF, Leese MP, Potter BVL, Reed MJ, Purohit A (2006) The role of 17beta-hydroxysteroid dehydrogenases in modulating the activity of 2-methoxyestradiol in breast cancer cells. Cancer Res 66: 324–330.
Normanno N, Morabito A, De Luca A, Piccirillo MC, Gallo M, Maiello MR, Perrone F (2009) Target-based therapies in breast cancer: current status and future perspectives. Endocr Relat Cancer 16: 675–702.
Orr GA, Verdier-Pinard P, McDaid H, Horwitz SB (2003) Mechanisms of Taxol resistance related to microtubules. Oncogene 22: 7280–7295.
Passaniti A, Taylor RM, Pili R, Guo Y, Long PV, Haney JA, Pauly RR, Grant DS, Martin GR (1992) A simple, quantitative method for assessing angiogenesis and antiangiogenic agents using reconstituted basement membrane, heparin, and fibroblast growth factor. Lab Invest 67: 519–528.
Prewett M, Huber J, Li Y, Santiago A, O’Connor W, King K, Overholser J, Hooper A, Pytowski B, Witte L, Bohlen P, Hicklin DJ (1999) Antivascular endothelial growth factor receptor (fetal liver kinase 1) monoclonal antibody inhibits tumor angiogenesis and growth of several mouse and human tumors. Cancer Res 59: 5209–5218.
Raobaikady B, Reed MJ, Leese MP, Potter BVL, Purohit A (2005) Inhibition of MDA-MB-231 cell cycle progression and cell proliferation by C-2-substituted oestradiol mono- and bis-3-O-sulphamates. Int J Cancer 117: 150–159.
Ring AE, Ellis PA (2005) Taxanes in the treatment of early breast cancer. Cancer Treat Rev 31: 618–627.
Shelanski ML, Gaskin F, Cantor CR (1973) Microtubule assembly in the absence of added nucleotides. Proc Natl Acad Sci USA 70: 765–768.
Stengel C, Newman SP, Leese MP, Potter BVL, Reed MJ, Purohit A (2010) Class III beta-tubulin expression and in vitro resistance to microtubule targeting agents. Br J Cancer 102: 316–324.
Tahir SK, Kovar P, Rosenberg SH, Ng SC (2000) Rapid colchicine competition-binding scintillation proximity assay using biotin-labeled tubulin. Biotechniques 29: 156–160.
Workman P, Aboagye EO, Balkwill F, Balmain A, Bruder G, Chaplin DJ, Double JA, Everitt J, Farningham DA, Glennie MJ, Kelland LR, Robinson V, Stratford IJ, Tozer GM, Watson S, Wedge SR, Eccles SA Committee of the National Cancer Research Institute (2010) Guidelines for the welfare and use of animals in cancer research. Br J Cancer 102: 1555–1557.
Yuan J, Yan R, Kramer A, Eckerdt F, Roller M, Kaufmann M, Strebhardt K (2004) Cyclin B1 depletion inhibits proliferation and induces apoptosis in human tumor cells. Oncogene 23: 5843–5852.
Zhang P, Sun M, Qiu R, Tang L, Dou G, Xu B (2011) Phase I clinical and pharmacokinetic study of UTD1, a genetically engineered epothilone analog in patients with advanced solid tumors. Cancer Chemother Pharmacol 68: 971–978.
Acknowledgements
This research was supported by Sterix Ltd, a member of the Ipsen Group.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
BVLP and MJR were consultants to IPSEN Ltd. AP is a consultant to IPSEN Ltd. The remaining authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Stengel, C., Newman, S., Day, J. et al. In vivo and in vitro properties of STX2484: a novel non-steroidal anti-cancer compound active in taxane-resistant breast cancer. Br J Cancer 111, 300–308 (2014). https://doi.org/10.1038/bjc.2014.188
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.188
Keywords
This article is cited by
-
Molecular Mechanisms of Metal Toxicity in the Pathogenesis of Alzheimer’s Disease
Molecular Neurobiology (2021)
-
Pathogenic Mechanisms of Heavy Metal Induced-Alzheimer’s Disease
Toxicology and Environmental Health Sciences (2018)
-
Targeted NF1 cancer therapeutics with multiple modes of action: small molecule hormone-like agents resembling the natural anticancer metabolite, 2-methoxyoestradiol
British Journal of Cancer (2015)