Abstract
Calcium (Ca) channel blockers (CCBs) inhibit Ca2+ channels in the myocardium or vascular smooth muscle cells, inhibit myocardium contraction, inhibit the impulse conduction system (anti-arrhythmias) and cause vasodilation. New classifications based on subtypes of Ca channels and α1 subunits have been proposed. Moreover, CCBs have pleiotropic effects on coronary spastic angina (CSA), including variant angina, myocardial infarction (MI) and stent thrombosis (ST). Although the roles of CCBs in clinical situations remain unknown, further studies in this field are expected to broaden our understanding. In this article, we explain the clinical roles of CCBs in ischemic heart diseases, such as CSA, MI and ST, based on previous knowledge and as demonstrated in representative clinical trials.
Similar content being viewed by others
Introduction
Calcium (Ca) channel blockers (CCBs) were first reported in 1969, when Fleckenstein et al.1 in Germany described prenylamine, verapamil and D600 (methoxyverapamil) as coronary vasodilators. Fleckenstein named these agents Ca antagonists, not CCBs, on the basis of their pharmacological effects involving vascular and myocardial stretch activation. These drugs also exert powerful actions on coronary vessels and other smooth muscles, relaxing vascular smooth muscle, uterine smooth muscle and intestinal smooth muscle. The concept of the CCB arose from the advent of the 1,4-dihydropyridine derivative nifedipine (Adalat), which was developed by Vater et al.2 in Germany in 1972, and from basic and clinical studies performed by Fleckenstein et al.3 in Germany and by Hashimoto et al.4 in Japan. Nifedipine is effective for the treatment of ischemic heart disease because it increases coronary blood flow5 and also has a hypotensive effect.6 Diltiazem (Herbesser) was developed in Japan,7 and its effectiveness in variant angina has been demonstrated.8 Many pharmaceutical companies have shown interest in CCBs; hence, many CCBs have been developed.
CCBs are drugs that target voltage-dependent Ca channels, and new classifications based on subtypes of Ca channels and α1 subunits have been proposed.9 In this article, we explain the clinical roles of CCBs in coronary spastic angina (CSA), myocardial infarction (MI) and stent thrombosis (ST) on the basis of previous knowledge and as demonstrated in representative clinical trials.
General background
CCBs bind to voltage-dependent Ca channels in the cell membrane and inhibit the influx of Ca ions into cells. The voltage-dependent Ca channel family members show differences in the potential threshold of depolarization and are classified as high-voltage-activated or low-voltage-activated forms based on their membrane potential dependence. The high-voltage-activated forms include the slow L (long-lasting) type with inert speed, N (neural) types, which are present in regions such as the nerve terminals and P/Q types, which are classified as subtypes of the R type. The low-voltage-activated form includes only the T (transient) type, which has a fast transient inactivation rate, is mainly L-shaped in the myocardium and vascular smooth muscle, and is associated with the T-type pacemaker activity of the sinoatrial node and nerve cells. The Ca channel consists of five subunits (α1, α2, β, γ and δ), each encoded by a separate gene9 The α1 subunit is the most important; it forms the Ca2+ permeation pore and contains a membrane potential detection sensor and the phosphorylation site, which is modified during intracellular signal transduction.
CCBs are classified into the dihydropyridine (DHP) type, the phenylalkylamine (PAA) type or the benzodiazepine (BTZ) type. They have also been classified into three generations based on the timing of their discovery and duration of their action. The first-generation CCBs have a short duration of action and lead to a tachycardia reflex, which is problematic. In the second generation, a sustained-release formulation was developed with long-lasting, stable activity and long-acting antihypertensive effects. The third-generation CCBs, such as amlodipine (Amlodine) and azelnidipine (Calblock), have a long duration of action, produce a small tachycardia reflex, and have high vascular selectivity. The DHP-type CCBs have a high affinity for Ca channels in vascular smooth muscle cells with low membrane potential and have higher activity in vessels than in cardiac muscle cells. They act strongly on vascular smooth muscle, exerting a strong hypotensive effect through peripheral vasodilatation. By contrast, the PAA type CCBs, such as verapamil (Vasolan), act on the impulse conduction system (ICS) with high membrane potential and on Ca channels in ventricular muscle, and have negative inotropic, chronotropic and dromotropic effects. The BTZ type, diltiazem, exerts an intermediate effect between the DHP type and PAA type, acting on the myocardium and ICS, particularly in atrioventricular node conduction. Most recently, the diarylaminopropylamine drug bepridil (Bepricor) has been developed (Table 1).10
CCBs have pleiotropic effects, such as anti-inflammatory effects, antioxidant effects, inhibition of the migration and proliferation of vascular smooth muscle cells, enhanced nitric oxide (NO) production,11 plaque stabilization, inhibition of blood vessel aggregation, vasodilation, decreased cardiac contraction and heart rate, and suppressed atrioventricular conduction. Nifedipine is known to increase the levels of adiponectin12 and peroxisome proliferator-activated receptor-γ,13 which increase the expression of transcription factors involved in adipocyte differentiation. Moreover, nifedipine has an antioxidant effect,14, 15, 16 improves NO bioavailability12, 17, 18 and inhibits vascular smooth muscle migration.19, 20, 21 In addition, it inhibits monocyte chemotactic protein-1 expression,22, 23, 24 thus resulting in anti-inflammatory activity, and is also known to improve vascular remodeling. Amlodipine has a possible inhibitory effect on the onset and progression of atherosclerosis through NO production,25 has anti-inflammatory26, 27 and antioxidant effects,28 inhibits the migration and proliferation of vascular smooth muscle cells, stabilizes plaques29, 30 and inhibits platelet aggregation, as shown by basic science and clinical experiments.
The adverse effects of CCBs include palpitations, headache, hot flashes, edema, gingival growth and constipation. Non-DHP CCBs must not be used in patients with heart failure or marked bradycardia because of their cardioinhibitory actions, and careful consideration is necessary regarding their use in elderly patients with latent cardiac disorders or their concomitant use with digitalis or a β-blocker.31
The mechanism of action of CCBs is shown in Figure 1. The cardiovascular pharmacological actions of representative CCBs are shown in Table 2, and are based on the literature.32, 33
Coronary spastic angina
CCBs, which inhibit the intracellular Ca2+ influx in vascular smooth muscle cells, are highly effective for the prevention of coronary spasms and are a first-line treatment for coronary vasospasm.34, 35 In a comparative study of tens of trials, CCBs, regardless of type and time of action, have been shown to be effective at preventing angina attacks.36, 37, 38, 39, 40, 41 In addition, at normal doses, few adverse effects have been reported, thus suggesting that this treatment is safe. A CCB has been reported to inhibit Rho kinase.42 The possibility that there is a difference in prognosis improvement among patients receiving different CCBs has been suggested.43, 44 However, the combined administration of several CCBs and nitrate drugs has not yielded objective evidence regarding the therapeutic effect. Furthermore, if CCBs are discontinued after a long period, a worsening of symptoms (rebound phenomenon) has been reported.45, 46, 47 In cases of dose increases or discontinuation, dose changes must occur in stages, and with each change, it is necessary to confirm that there is no deterioration or coronary spasm by using methods such as Holter monitoring.38 In some cases of CSA, no attacks occur even after discontinuation of CCBs after a certain period of administration; however, so-called spontaneous remission has been reported.48, 49 Substantial data exist indicating that benidipine (Coniel) significantly improves the prognosis of CSA, particularly the medium- and long-term prognoses.44 The mechanisms involved in the cardiovascular protective effect include enhanced expression of vascular endothelial NO synthase, amelioration of vascular remodeling and an antioxidant effect, as mentioned above. In Asian countries, including Japan, the incidence of CSA is higher than in Western countries.50, 51 We have recently reported that a variant of aldehyde dehydrogenase 2 is associated with CSA in east Asian patients52 and that aspirin53 and statin54 were promising therapeutic strategies to improve the prognosis of CSA patients.
Myocardial infarction
The short-acting DHP-type CCB, which was widely used in a high percentage of MI patients until the first half of 1990, was then reported to potentially lead to myocardial ischemia, owing to activation of the sympathetic nerve reflex and the prevalence of tachycardia and hypotension, thereby worsening the prognosis of MI patients, as supported by meta-analysis.55, 56, 57 The contraindication for the administration of this drug to MI patients became dogma in the absence of proof to the contrary.58, 59, 60 However, clinical trials testing the efficacy of the long-acting DHP type of CCBs increasingly confirm the efficacy of this group of drugs alone and in combination with other drugs.61, 62, 63, 64 The Avoiding Cardiovascular Events Through COMbination Therapy in Patients Living With Systolic Hypertension (ACCOMPLISH) study in 2008 has examined, through a double-blind design, in 11 506 hypertension patients with high cardiovascular risk, whether the combination of benazepril (Cibacen) and amlodipine is beneficial for preventing cardiovascular events (such as cardiovascular death, non-fatal MI, non-fatal stroke, hospitalization for angina, resuscitation from sudden cardiac arrest and coronary revascularization), compared with the combination of benazepril and hydrochlorothiazide (Dichlotride).65 In the 36-month follow-up period, the total incidence of cardiac events in the amlodipine combination group was significantly lower than in the hydrochlorothiazide combination group, and there was a significant difference in the non-fatal MI recurrence rate when comparing the individual cardiac events.65 The study did not examine MI secondary prevention directly because MI history patients constituted ~24% of the group; the other participants had angina or coronary risk factors. However, the data demonstrate the superiority of the combination of angiotensin-converting enzyme inhibitors and long-acting DHP-type CCBs for high-risk hypertensive patients, including those with a history of MI.65
In patients with MI definitively due to coronary spasm or coronary spastic ischemia attack, prevention by CCBs is presumed to be superior to secondary prevention because such patients are thought to progress to MI as an extension of angina attacks. This type of MI is in contrast to MI due to coronary plaque rupture, which cannot be prevented by suppression of angina attacks. Notably, the relevant patients are those who are clinically diagnosed with CSA or MI derived from coronary spasms. In past reports, coronary spasms have been shown to occur easily by drug provocation testing in the recovery phase after acute MI in Japanese patients.50, 66 At present, it is not certain whether any CCB is effective for patients in whom coronary spasms are easy to provoke. Regarding the effectiveness of heart rate-lowering CCBs (verapamil and diltiazem) as a secondary form of prevention when β-blockers are contraindicated or poorly tolerated, subanalysis of the INVEST (International Verapamil SR-Trandolapril Study) trial,67 which examined the utility of verapamil for hypertensive patients with coronary artery disease, has demonstrated that verapamil has equal preventive efficacy to that of atenolol (Tenormin).68
Stent thrombosis
ST is a phenomenon in which thrombosis occurs in a deployed stent segment and occludes the coronary artery. When ST occurs, severe outcomes such as acute MI or death are frequent; hence, it is well known as a disease state with poor prognosis. Regarding the time of emergence, ST most commonly occurs within 1 week after stent deployment, often in the late phase. During the drug-eluting stent (DES) era, very late ST was often observed. ST is classified according to the time of emergence. In the past, ST was classified as acute ST (within 24 h after the procedures) or subacute ST (within 30 days after the procedures). However, after the appearance of the DES, very late ST became a clinical issue, and a new definition was adopted. ST is now classified as early ST (within 30 days after the procedures), late ST (from 31 to 365 days after the procedures) or very late ST (>1 year after the procedures).69, 70 Furthermore, as the use of a common international definition to discuss ST became more necessary, the definition from the Academic Research Consortium (ARC) became more widely used.
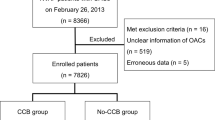
It is sometimes impossible to determine whether cardiac events or sudden death occurring in the late phase after stent deployment are due to ST. Therefore, ST has been classified according to the degree of reliability of the confirmation. Definitive ST classification requires angiographic71 or autopsy confirmation of thrombosis or occlusion as an acute coronary syndrome. Probable ST is defined as unaccountable death within 30 days or a lack of confirmed MI in the perfusion area of the target lesion, whereas possible ST is defined as unaccountable death over 30 days after stent deployment.69, 70 ST has emerged as a severe complication of percutaneous coronary intervention.72 Because the occurrence of ST is lower in Japan than in Western countries,73, 74 there are limited data from which to predict ST after DES implantation in Japan.75, 76 We have examined the independent predictors of ST incidence after DES implantation in Japanese patients, including the use of CCBs, using data from the Kumamoto Intervention Conference Study registry.77, 78, 79, 80 In this registry, CCB use was found to be associated with a decreased risk of ST after DES implantation within 1 year in Japanese patients.81 The underlying mechanism of the decreased risk of ST in CCB users is thought to be related to the prevalence of coronary spasms. Although the relation between coronary spasms and ST is unclear, given the decreased risk of ST with CCB use, it is possible that coronary spasms may be associated with the pathogenesis of ST as well as the pathophysiology of ischemic heart diseases.
Major clinical trials
Although in the Prospective Randomized Amlodipine Survival Evaluation (PRAISE) II study in 2000 (Annual Scientific Session of American College of Cardiology), amlodipine did not seem to have the ability to prevent heart failure or exert therapeutic effects, the A Coronary Disease Trial Investigating Outcome with Nifedipine (ACTION) study in 200461 showed that sustained-release nifedipine significantly suppresses the onset of ischemic heart failure, demonstrating that CCBs can offer proactive adaptation in cases of ischemic heart disease.
The status of CCBs as the most reliable type of hypotensive agent is already established. Based on the maintenance of a stricter hypotensive effect and organ protection, the clinical significance of combination therapy has been demonstrated. In The Anglo-Scandinavian Cardiac Outcomes Trial-Conduit Artery Function Evaluation (ASCOT-CAFÉ) trial,82 the combination of amlodipine and perindopril (Coversyl) was found to ameliorate aortic pulse pressure, which is not detected in peripheral blood pressure, thus highlighting a novel organ protective effect for CCBs.83 The combination of a CCB and a renin–angiotensin system (RAS) blocker is a focus in recent literature.84, 85 In the nifedipine and candesartan combination (NICE-Combi) trial,86 low-dose combination therapy with controlled-released nifedipine and candesartan (Blopress) was shown to be superior to up-titrated monotherapy with candesartan in terms of blood pressure control and renal protection in patients with essential hypertension. The ACCOMPLISH trial,65 comparing benazepril combined with an amlodipine or a hydrochlorothiazide in the prevention of cardiovascular events in high-risk hypertensive patients, demonstrated that the combination of a RAS blocker with a CCB is superior to the combination of a RAS blocker with a diuretic in preventing cardiovascular events in high-risk hypertensive patients. Furthermore, subgroup analysis of the ACCOMPLISH trial showed that the combination of a RAS blocker with a CCB is also superior to the combination of a RAS blocker with a diuretic in diabetic hypertensive patients87 and that the combination suppresses the risk of renal failure progression.88 In the OlmeSartan and Calcium Antagonists Randomized (OSCAR) trial,89 the combination of olmesartan (Benicar, Olmetec) and CCB was found to lower blood pressure and to reduce the incidence of primary end points more effectively than high-dose olmesartan in patients with cardiovascular disease. The addition of a second antihypertensive agent is more effective at lowering blood pressure than simply doubling the dose of an existing agent.
Summary
CCBs inhibit Ca2+ channels in the myocardium or vascular smooth muscle cells, resulting in inhibition of myocardium contraction, inhibition of ICS (anti-arrhythmias) and vasodilation. Moreover, CCBs have a pleiotropic effect on CSA including variant angina, MI and ST. Furthermore, new mechanisms of action of Ca2+ channels, such as the aldosterone inhibition effect and mineralocorticoid receptor blockade effect, have been elucidated in the field of endocrinology.90, 91, 92 Although the roles of CCBs in clinical situations remain unknown, further studies in this field are expected to broaden our understanding.
References
Fleckenstein A, Nakayama K, Fleckenstein-Grün G, Byon Y . Interactions of H ions, Ca-antagonistic drugs and cardiac glycosides with excitation-contraction coupling of vascular smooth muscle Ionic actions on vascular smooth muscle. Springer 1976, 117–123.
Vater W, Kroneberg G, Hoffmeister F, Saller H, Meng K, Oberdorf A, Puls W, Schlossmann K, Stoepel K . Pharmacology of 4-(2'-nitrophenyl)-2, 6-dimethyl-1, 4-dihydropyridine-3,5-dicarboxylic acid dimethyl ester (Nifedipine, BAY a 1040). Arzneimittel-Forschung 1972; 22: 1–14.
Fleckenstein A, Tritthart H, Döring H-J, Byron KY . BAY a 1040 — ein hochaktiver Ca++-antagonistischer Inhibitor der elektro-mechanischen Koppelungsprozesse im Warmblüter-Myocard. Arzneimittelforsch 1972; 22: 22–23.
Hashimoto K, Taira N, Sato S, Chiba S, Hashimoto K, Tamura K, Endoh M, Iijima T . Pharmacological action on nitrophenyi-dimethyl-dihydropyridine-deri-vatlve. Heart 1971; 3: 1294–1304.
Murakami M, Murakami E, Takekoshi N, Tsuchiya M, Kin T, Onoe T, Takeuchi N, Funatsu T, Hara S, Ishise S . Antihypertensive effect of 4 (-2'-nitrophenyl)-2, 6-dimethyl-1, 4-dihydropyridine-3, 5-dicarbonic acid dimethylester (nifedipine, bay-a 1040), a new coronary dilator. Jpn Heart J 1972; 13: 128–135.
Aoki K, Yoshida T, Kato S, Tazumi K, Sato I, Takikawa K, Hotta K . Hypotensive action and increased plasma renin activity by Ca2+ antagonist (nifedipine) in hypertensive patients. Jpn Heart J 1976; 17: 479–484.
Sato M, Nagao T, Yamaguchi I, Nakajima H, Kiyomoto A . Pharmacological studies on a new l, 5-benzothiazepine derivative (CRD-401). Arzneimittelforschung 1971; 21: 1338.
Yasue H, Takizawa A, Nagao M, Nishida S, Horie M, Kubota J, Omote S, Takaoka K, Okumura K . Long-term prognosis for patients with variant angina and influential factors. Circulation 1988; 78: 1–9.
Hayashi K, Wakino S, Sugano N, Ozawa Y, Homma K, Saruta T . Ca2+ channel subtypes and pharmacology in the kidney. Circ Res 2007; 100: 342–353.
Cosnier D, Duchenne-Marullaz P, Rispat G, Streichenberger G . Cardiovascular pharmacology of bepridil (1 [3 isobutoxy 2 (benzylphenyl) amino] propyl pyrrolidine hydrochloride) a new potential anti-anginal compound. Arch Int Pharmacodyn Ther 1977; 225: 133–151.
Yamamoto E, Nakamura T, Kataoka K, Tokutomi Y, Dong Y-F, Fukuda M, Nako H, Yasuda O, Ogawa H, Kim-Mitsuyama S . Nifedipine prevents vascular endothelial dysfunction in a mouse model of obesity and type 2 diabetes, by improving eNOS dysfunction and dephosphorylation. Biochem Bbiophys Res Commun 2010; 403: 258–263.
Nomura S, Inami N, Kimura Y, Omoto S, Shouzu A, Nishikawa M, Iwasaka T . Effect of nifedipine on adiponectin in hypertensive patients with type 2 diabetes mellitus. J Hum Hypertens 2007; 21: 38–44.
Matsumori A, Nunokawa Y, Sasayama S . Nifedipine inhibits activation of transcription factor NF-κB. Life Sci 2000; 67: 2655–2661.
Lupo E, Locher R, Weisser B, Vetter W . In vitro antioxidant activity of calcium antagonists against LDL oxidation compared with α-tocopherol. Biochem Biophys Res Commun 1994; 203: 1803–1808.
Hashimoto R, Umemoto S, Guo F, Umeji K, Itoh S, Kishi H, Kobayashi S, Matsuzaki M . Nifedipine activates PPARγ and exerts antioxidative action through Cu/ZnSOD independent of blood-pressure lowering in SHRSP. J Atheroscler Thromb 2010; 17: 785–795.
Subudhi BB, Sahoo SP . Synthesis and evaluation of antioxidant, anti-inflammatory and antiulcer activity of conjugates of amino acids with Nifedipine. Chem Pharm Bull 2011; 59: 1153–1156.
Rosenkranz AC, Lob H, Breitenbach T, Be JP . Endothelial antioxidant actions of dihydropyridines and angiotensin converting enzyme inhibitors. Eur J Pharmacol 2006; 529: 55–62.
Berkels R, Egink G, Marsen TA, Bartels H, Roesen R, Klaus W . Nifedipine increases endothelial nitric oxide bioavailability by antioxidative mechanisms. Hypertension 2001; 37: 240–245.
Sakurada T, Ishizawa K, Imanishi M, Izawa-Ishizawa Y, Fujii S, Tominaga E, Tsuneishi T, Horinouchi Y, Kihira Y, Ikeda Y . Nitrosonifedipine ameliorates angiotensin II-induced vascular remodeling via antioxidative effects. Naunyn Schmiedeberg Arch Pharmacol 2013; 386: 29–39.
Soe NN, Ishida T, Miho N, Ishida M, Sawano M, Abe K, Chayama K, Kihara Y, Yoshizumi M . Nifedipine interferes with migration of vascular smooth muscle cells via inhibition of Pyk2-Src axis. J Atheroscler Thromb 2009; 16: 230–238.
Motro M, Shemesh J . Calcium channel blocker nifedipine slows down progression of coronary calcification in hypertensive patients compared with diuretics. Hypertension 2001; 37: 1410–1413.
Matsui T, Takeuchi M, Yamagishi S-i . Nifedipine, a calcium channel blocker, inhibits inflammatory and fibrogenic gene expressions in advanced glycation end product (AGE)-exposed fibroblasts via mineralocorticoid receptor antagonistic activity. Biochem Biophys Res Commun 2010; 396: 566–570.
Matsui T, Yamagishi S-i, Takeuchi M, Ueda S, Fukami K, Okuda S . Nifedipine, a calcium channel blocker, inhibits advanced glycation end product (AGE)-elicited mesangial cell damage by suppressing AGE receptor (RAGE) expression via peroxisome proliferator-activated receptor-gamma activation. Biochem Biophys Res Commun 2009; 385: 269–272.
Gao X, Iwai M, Inaba S, Tomono Y, Kanno H, Mogi M, Horiuchi M . Attenuation of monocyte chemoattractant protein-1 expression via inhibition of nuclear factor-κB activity in inflammatory vascular injury. Am J Hypertens 2007; 20: 1170–1175.
Berkels R, Taubert D, Bartels H, Breitenbach T, Klaus W, Roesen R . Amlodipine increases endothelial nitric oxide by dual mechanisms. Pharmacology 2004; 70: 39–45.
Matsumori A, Nishio R, Nose Y . Calcium channel blockers differentially modulate cytokine production by peripheral blood mononuclear cells. Circ J 2010; 74: 567–571.
Kataoka C, Egashira K, Ishibashi M, Inoue S, Ni W, Hiasa K-i, Kitamoto S, Usui M, Takeshita A . Novel anti-inflammatory actions of amlodipine in a rat model of arteriosclerosis induced by long-term inhibition of nitric oxide synthesis. Am J Physiol Heart Circ Physiol 2004; 286: H768–H774.
Sueta D, Nakamura T, Dong Y-F, Kataoka K, Koibuchi N, Yamamoto E, Toyama K, Yasuda O, Ogawa H, Kim-Mitsuyama S . Amlodipine enhances amelioration of vascular insulin resistance, oxidative stress, and metabolic disorders by candesartan in metabolic syndrome rats. Am J Hypertens 2012; 25: 704–710.
Tulenko T, Sumner A, Chen M, Huang Y, Laury-Kleintop L, Ferdinand F . The smooth muscle cell membrane during atherogenesis: a potential target for amlodipine in atheroprotection. Am Heart J 2001; 141: S1–S11.
Mason RP . Mechanisms of atherosclerotic plaque stabilization for a lipophilic calcium antagonist amlodipine. Am Cardiol 2001; 88: 2–6.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M . The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res 2014; 37: 253–390.
Taira N . Differences in cardiovascular profile among calcium antagonists. Am J Cardiol 1987; 59: B24–B29.
Abernethy DR, Schwartz JB . Calcium-antagonist drugs. N Engl J Med 1999; 341: 1447–1457.
Antman E, Muller J, Goldberg S, MacAlpin R, Rubenfire M, Tabatznik B, Liang C-s, Heupler F, Achuff S, Reicher N . Nifedipine therapy for coronary-artery spasm: experience in 127 patients. N Engl J Med 1980; 302: 1269–1273.
Kimura E, Kishida H . Treatment of variant angina with drugs: a survey of 11 cardiology institutes in Japan. Circulation 1981; 63: 844–848.
Ginsburg R, Lamb IH, Schroeder JS, Hu M, Harrison DC . Randomized double-blind comparison of nifedipine and isosorbide dinitrate therapy in variant angina pectoris due to coronary artery spasm. Am Heart J 1982; 103: 44–48.
Mauritson DR, Johnson SM, Winniford MD, Cary JR, Willerson JT, Hillis LD . Verapamil for unstable angina at rest: A short-term randomized, double-blind study. Am Heart J 1983; 106: 652–658.
Pesola A, Lauro A, Gallo R, Madeo A, Cosentino G . Efficacy of diltiazem in variant angina. Results of a double-blind crossover study in CCU by Holter monitoring. The possible occurrence of a withdrawal syndrome. G Ital Cardiol 1987; 17: 329–339.
Chahine RA, Feldman RL, Giles TD, Nicod P, Raizner AE, Weiss RJ, Vanov SK . Randomized placebo-controlled trial of amlodipine in vasospastic angina. J Am Coll Cardiol 1993; 21: 1365–1370.
Oikawa Y, Matsuno S, Yajima J, Nakamura M, Ono T, Ishiwata S, Fujimoto Y, Aizawa T . Effects of treatment with once-daily nifedipine CR and twice-daily benidipine on prevention of symptomatic attacks in patients with coronary spastic angina pectoris—Adalat Trial vs. Coniel in Tokyo against Coronary Spastic Angina (ATTACK CSA). J Cardiol 2010; 55: 238–247.
Higuma T, Oikawa K, Kato T, Mori Y, Kudo T, Yamamoto T, Hoshi Y, Kameda K, Suto N, Fujita N . Comparison of the effects of long-acting nifedipine CR and diltiazem R in patients with vasospastic angina: Aomori coronary spastic angina study. J Cardiol 2010; 56: 354–360.
Hata T, Soga J, Hidaka T, Idei N, Fujii Y, Fujimura N, Mikami S, Maruhashi T, Kihara Y, Chayama K . Calcium channel blocker and Rho-associated kinase activity in patients with hypertension. J Hypertens 2011; 29: 373.
Ito A, Fukumoto Y, Shimokawa H . Changing characteristics of patients with vasospastic angina in the era of new calcium channel blockers. J Cardiovasc Pharmacol 2004; 44: 480–485.
Nishigaki K, Inoue Y, Yamanouchi Y, Fukumoto Y, Yasuda S, Sueda S, Urata H, Shimokawa H, Minatoguchi S . Prognostic effects of calcium channel blockers in patients with vasospastic angina-a meta-analysis. Circ J 2010; 74: 1943–1950.
Lette J, Gagnon R-M, Lemire JG, Morissette M . Rebound of vasospastic angina after cessation of long-term treatment with nifedipine. Can Med Assoc J 1984; 130: 1169.
Kozeny G, Ragona B, Bansal V, Hurley R, Dixon DW, Vertuno L, Hano J . Myocardial infarction with normal results of coronary angiography following diltiazem withdrawal. Am J Med 1986; 80: 1184–1186.
Kostis WJ, Suh WM, Palacios IF . Acute myocardial infarction caused by multivessel coronary spasm due to calcium channel blocker withdrawal. Catheter Cardiovasc Interv 2011; 78: 229–233.
tashiro H, Shimokawa H, Koyanagi S, Takeshita A . Clinical characteristics of patients with spontaneous remission of variant angina. Jpn Circ J 1993; 57: 117–122.
Waters DD, Bouchard A, ThÉroux P . Spontaneous remission is a frequent outcome of variant angina. J Am Coll Cardiol 1983; 2: 195–199.
Pristipino C, Beltrame JF, Finocchiaro ML, Hattori R, Fujita M, Mongiardo R, Cianflone D, Sanna T, Sasayama S, Maseri A . Major racial differences in coronary constrictor response between Japanese and Caucasians with recent myocardial infarction. Circulation 2000; 101: 1102–1108.
Group JJW. Guidelines for diagnosis and treatment of patients with vasospastic angina (Coronary Spastic Angina)(JCS 2013). Circ J 2014; 78: 2779.
Mizuno Y, Harada E, Morita S, Kinoshita K, Hayashida M, Shono M, Morikawa Y, Murohara T, Nakayama M, Yoshimura M . East Asian variant of aldehyde dehydrogenase 2 (ALDH2* 2) is associated with coronary spastic angina: possible roles of reactive aldehydes and implications of alcohol flushing syndrome. Circulation 2015; 114: 013120.
Ishii M, Kaikita K, Sato K, Yamanaga K, Miyazaki T, Akasaka T, Tabata N, Arima Y, Sueta D, Sakamoto K . Impact of aspirin on the prognosis in patients with coronary spasm without significant atherosclerotic stenosis. Int J Cardiol 2016; 220: 328–332.
Ishii M, Kaikita K, Sato K, Yamanaga K, Miyazaki T, Akasaka T, Tabata N, Arima Y, Sueta D, Sakamoto K . Impact of statin therapy on clinical outcome in patients with coronary spasm. J Am Heart Assoc 2016; 5: e003426.
Furberg CD, Psaty BM, Meyer JV . Nifedipine dose-related increase in mortality in patients with coronary heart disease. Circulation 1995; 92: 1326–1331.
Opie LH, Messerli FH . Nifedipine and mortality grave defects in the dossier. Circulation 1995; 92: 1068–1073.
Psaty BM, Heckbert SR, Koepsell TD, Siscovick DS, Raghunathan TE, Weiss NS, Rosendaal FR, Lemaitre RN, Smith NL, Wahl PW . The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA 1995; 274: 620–625.
Ishikawa K, Nakai S, Takenaka T, Kanamasa K, Hama J, Ogawa I, Yamamoto T, Oyaizu M, Kimura A, Yamamoto K . Short-acting nifedipine and diltiazem do not reduce the incidence of cardiac events in patients with healed myocardial infarction. Circulation 1997; 95: 2368–2373.
Yusuf S . Calciumantagonists in coronary artery disease and hypertension time for reevaluation? Circulation 1995; 92: 1079–1082.
Eisenberg MJ, Brox A, Bestawros AN . Calcium channel blockers: an update. Am J Med 2004; 116: 35–43.
Poole-Wilson PA, Lubsen J, Kirwan B-A, van Dalen FJ, Wagener G, Danchin N, Just H, Fox KA, Pocock SJ, Clayton TC . Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with stable angina requiring treatment (ACTION trial): randomised controlled trial. Lancet 2004; 364: 849–857.
Nissen SE, Tuzcu EM, Libby P, Thompson PD, Ghali M, Garza D, Berman L, Shi H, Buebendorf E, Topol EJ . Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trial. JAMA 2004; 292: 2217–2225.
Pepine CJ, Handberg EM, Cooper-DeHoff RM, Marks RG, Kowey P, Messerli FH, Mancia G, Cangiano JL, Garcia-Barreto D, Keltai M . A calcium antagonist vs. a non–calcium antagonist hypertension treatment strategy for patients with coronary artery disease: the International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. JAMA 2003; 290: 2805–2816.
Black HR, Elliott WJ, Grandits G, Grambsch P, Lucente T, White WB, Neaton JD, Grimm RH Jr, Hansson L, Lacourcière Y . Principal results of the controlled onset verapamil investigation of cardiovascular end points (CONVINCE) trial. JAMA 2003; 289: 2073–2082.
Jamerson K, Weber MA, Bakris GL, Dahlöf B, Pitt B, Shi V, Hester A, Gupte J, Gatlin M, Velazquez EJ . Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359: 2417–2428.
Wakabayashi K, Suzuki H, Honda Y, Wakatsuki D, Kawachi K, Ota K, Koba S, Shimizu N, Asano F, Sato T . Provoked coronary spasm predicts adverse outcome in patients with acute myocardial infarction: a novel predictor of prognosis after acute myocardial infarction. J Am Coll Cardiol 2008; 52: 518–522.
Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, Pepine CJ . Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA 2010; 304: 61–68.
Bangalore S, Messerli FH, Cohen JD, Bacher PH, Sleight P, Mancia G, Kowey P, Zhou Q, Champion A, Pepine CJ . Verapamil-sustained release–based treatment strategy is equivalent to atenolol-based treatment strategy at reducing cardiovascular events in patients with prior myocardial infarction: an INternational VErapamil SR-Trandolapril (INVEST) substudy. Am Heart J 2008; 156: 241–247.
Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es G-A, Steg PG, Morel M-a, Mauri L, Vranckx P . Clinical end points in coronary stent trials a case for standardized definitions. Circulation 2007; 115: 2344–2351.
Mauri L, Hsieh W-h, Massaro JM, Ho KK, D'Agostino R, Cutlip DE . Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med 2007; 356: 1020–1029.
Capone G, Wolf NM, Meyer B, Meister SG . Frequency of intracoronary filling defects by angiography in angina pectoris at rest. Am J Cardiol 1985; 56: 403–406.
Al Suwaidi J, Holmes DR, Salam AM, Lennon R, Berger PB . Impact of coronary artery stents on mortality and nonfatal myocardial infarction: meta-analysis of randomized trials comparing a strategy of routine stenting with that of balloon angioplasty. Am Heart J 2004; 147: 815–822.
Kimura T, Morimoto T, Nakagawa Y, Tamura T, Kadota K, Yasumoto H, Nishikawa H, Hiasa Y, Muramatsu T, Meguro T . Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation 2009; 119: 987–995.
Dangas GD, Caixeta A, Mehran R, Parise H, Lansky AJ, Cristea E, Brodie BR, Witzenbichler B, Guagliumi G, Peruga JZ . Frequency and predictors of stent thrombosis after percutaneous coronary intervention in acute myocardial infarction. Circulation 2011; 123: 1745–1756.
King SB, Smith SC, Hirshfeld JW, Jacobs AK, Morrison DA, Williams DO, Feldman TE, Kern MJ, O’Neill WW, Schaff HV . 2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention a Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention Writing on Behalf of the 2005 Writing Committee. Circulation 2008; 117: 261–295.
Kushner FG, Hand M, Smith SC, King SB, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE . 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2009; 54: 2205–2241.
Chitose T, Hokimoto S, Oshima S, Nakao K, Fujimoto K, Miyao Y, Shimomura H, Tsunoda R, Maruyama H, Hirose T . Clinical outcomes following coronary stenting in Japanese patients treated with and without proton pump inhibitor. Circ J 2012; 76: 71–78.
Akasaka T, Hokimoto S, Oshima S, Nakao K, Fujimoto K, Miyao Y, Shimomura H, Tsunoda R, Hirose T, Kajiwara I . Clinical outcomes of percutaneous coronary intervention (PCI) at hospital with or without onsite cardiac surgery backup. Int J Cardiol 2014; 176: 1385.
Ishii M, Hokimoto S, Akasaka T, Fujimoto K, Miyao Y, Kaikita K, Oshima S, Nakao K, Shimomura H, Tsunoda R . Differential effects of strong and regular statins on the clinical outcome of patients with chronic kidney disease following coronary stent implantation. Circ J 2015; 79: 1115–1124.
Akasaka T, Hokimoto S, Sueta D, Tabata N, Oshima S, Nakao K, Fujimoto K, Miyao Y, Shimomura H, Tsunoda R . Clinical outcomes of percutaneous coronary intervention for acute coronary syndrome between hospitals with and without onsite cardiac surgery backup. J Cardiol 2016; 69: 103–109.
Nagano M, Hokimoto S, Nakao K, Kaikita K, Akasaka T, Ogawa H . Relation between stent thrombosis and calcium channel blocker after drug-eluting stent implantation: Kumamoto Intervention Conference Study (KICS) registry. J Cardiol 2015; 66: 333–340.
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, Hughes AD, Thurston H, O’Rourke M, Investigators C. Differential impact of blood pressure–lowering drugs on central aortic pressure and clinical outcomes principal results of the Conduit Artery Function Evaluation (CAFE) Study. Circulation 2006; 113: 1213–1225.
Tokitsu T, Yamamoto E, Hirata Y, Fujisue K, Sugamura K, Maeda H, Tsujita K, Kaikita K, Hokimoto S, Sugiyama S . Relationship between inter-arm blood pressure differences and future cardiovascular events in coronary artery disease. J Hypertens 2015; 33: 1780–1790.
Thamcharoen N, Susantitaphong P, Wongrakpanich S, Chongsathidkiat P, Tantrachoti P, Pitukweerakul S, Avihingsanon Y, Praditpornsilpa K, Jaber BL, Eiam-Ong S . Effect of N-and T-type calcium channel blocker on proteinuria, blood pressure and kidney function in hypertensive patients: a meta-analysis. Hypertens Res 2015; 38: 847–855.
Nagasawa K, Takahashi K, Matsuura N, Takatsu M, Hattori T, Watanabe S, Harada E, Niinuma K, Murohara T, Nagata K . Comparative effects of valsartan in combination with cilnidipine or amlodipine on cardiac remodeling and diastolic dysfunction in Dahl salt-sensitive rats. Hypertens Res 2015; 38: 39–47.
Hasebe N, Kikuchi K, Group NCS. Controlled-release nifedipine and candesartan low-dose combination therapy in patients with essential hypertension: the NICE Combi (Nifedipine and Candesartan Combination) Study. J Hypertens 2005; 23: 445–453.
Weber MA, Bakris GL, Jamerson K, Weir M, Kjeldsen SE, Devereux RB, Velazquez EJ, Dahlöf B, Kelly RY, Hua TA . Cardiovascular events during differing hypertension therapies in patients with diabetes. J Am Coll Cardiol 2010; 56: 77–85.
Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, Velazquez EJ, Staikos-Byrne L, Kelly RY, Shi V . Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet 2010; 375: 1173–1181.
Ogawa H, Kim-Mitsuyama S, Matsui K, Jinnouchi T, Jinnouchi H, Arakawa K . Angiotensin II receptor blocker-based therapy in Japanese elderly, high-risk, hypertensive patients. Am J Med 2012; 125: 981–990.
Ishimitsu T, Kameda T, Akashiba A, Takahashi T, Ohta S, Yoshii M, Minami J, Ono H, Numabe A, Matsuoka H . Efonidipine reduces proteinuria and plasma aldosterone in patients with chronic glomerulonephritis. Hypertens Res 2007; 30: 621–626.
Isaka T, Ikeda K, Takada Y, Inada Y, Tojo K, Tajima N . Azelnidipine inhibits aldosterone synthesis and secretion in human adrenocortical cell line NCI-H295R. Eur J Pharmacol 2009; 605: 49–52.
Dietz JD, Du S, Bolten CW, Payne MA, Xia C, Blinn JR, Funder JW, Hu X . A number of marketed dihydropyridine calcium channel blockers have mineralocorticoid receptor antagonist activity. Hypertension 2008; 51: 742–748.
Acknowledgements
We thank all the paramedical staff and clinical secretaries for their kind support during the course of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sueta, D., Tabata, N. & Hokimoto, S. Clinical roles of calcium channel blockers in ischemic heart diseases. Hypertens Res 40, 423–428 (2017). https://doi.org/10.1038/hr.2016.183
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.183
This article is cited by
-
Histopathological and proteomic analyses identify integrin-β1 as a potential mediator of phlebosclerosis in uremic patients
Clinical and Experimental Nephrology (2019)
-
Pleiotropic effects of calcium channel blockers
Hypertension Research (2018)