Abstract
Our objectives were to evaluate whether polymorphisms in the α1A- and β2-adrenoceptor genes influence blood pressure response to nifedipine gastrointestinal therapeutic system (GITS). Hypertensive patients received daily treatment with an oral dosage of 30 mg nifedipine GITS for 16 days. Genotypes of the Arg347Cys polymorphism in the α1A-adrenoceptor gene and the Arg16Gly and Gln27Glu polymorphisms in the β2-adrenoceptor gene were determined by TaqMan single-nucleotide polymorphism genotyping assay. The sixteenth-day steady-state plasma concentration of nifedipine was measured using HPLC with UV detection. Multivariate linear regression was performed in a total of 447 patients to evaluate the effects of these polymorphisms on blood pressure response to nifedipine GITS. Patients carrying the Cys347 allele of the α1A-adrenoceptor gene had a greater systolic blood pressure reduction than did those carrying two Arg347 alleles of the α1A-adrenoceptor gene (32.5±14.0 versus 27.3±15.5 mm Hg, respectively, P=0.006). However, diastolic blood pressure reduction was not associated with the Arg347Cys polymorphism in the α1A-adrenoceptor gene. In addition, no significant associations were observed between blood pressure reduction and two polymorphisms in the β2-adrenoceptor gene. Our data suggest that the Arg347Cys polymorphism in the α1A-adrenoceptor gene may be used to predict blood pressure response to nifedipine GITS in Chinese hypertensive patients.
Similar content being viewed by others
Introduction
Essential hypertension, a major independent risk factor of cardiovascular and cerebrovascular diseases, is a worldwide health issue. Given the major role of elevated blood pressure level in the pathogenesis of cerebrovascular and cardiovascular events, such as stroke and myocardial infarction, it is important for hypertensive patients to get their blood pressure well controlled. The nifedipine gastrointestinal therapeutic system (GITS), an extended-release formulation of dihydropyridine calcium channel blocker (CCB), has been proved to be effective in reducing blood pressure.1 However, a considerable interindividual variation was observed in blood pressure response to nifedipine GITS. The Modern Approach to the Treatment of Hypertension Trial showed that about 76% hypertensive patients responded to nifedipine GITS monotherapy.2 The causes of interindividual variation in response to medication have not been conclusively determined, and it is considered to have a genetic basis. Except the genes encoding the drug target and the major metabolic enzyme, several studies have shown that those candidate genes involved in the regulation of blood pressure may also contribute to interindividual variation in response to antihypertensive medications.3, 4
The sympathetic nervous system plays an important role in the pathogenesis of essential hypertension, mainly through the catecholamines acting on G-protein-coupled α- and β-adrenoceptors. A chronic increase in the sympathetic functions, as well as alterations in the balance of adrenoceptors in cardiovascular tissues, is found in many hypertensive patients. α1A-Adrenoceptors play a crucial role in the regulation of vascular tone. Stimulation of α1A-adrenoceptors in the vessels leads to vasoconstriction. One non-synonymous polymorphism (Arg347Cys, formerly named as Arg492Cys) in the α1A-adrenoceptor gene (ADRA1A), which replaces arginine with cysteine at codon 347, has been identified. Earlier studies revealed that this kind of polymorphism located in the carboxy-terminal segment of G-protein-coupled receptors could result in an extra palmitoylation site and affect receptor localization and function.5, 6 β2-Adrenoceptors are well known for the vasodilatation effect on both arteries and veins. There are two common missense polymorphisms, named Arg16Gly and Gln27Glu, in the β2-adrenoceptor gene (ADRB2), which consist of substitutions of glycine for arginine at amino-acid position 16 and glutamine for glutamic acid at amino-acid position 27, respectively. Previous study showed that the Gly16 variants of β2-adrenoceptors had enhanced agonist-promoted downregulation in human lung mast cells, whereas the Glu27 variants of β2-adrenoceptors were resistant to agonist-promoted downregulation.7
These functional implications lead us to question whether these polymorphisms can explain part of the interindividual variation in blood pressure response to nifedipine GITS. In this report, we followed up hypertensive patients from Anhui province, China, to evaluate the associations between blood pressure reduction after a 15-day nifedipine GITS treatment and these polymorphisms in the ADRA1A and ADRB2 genes.
Materials and methods
Subjects
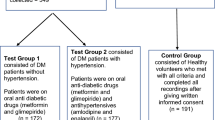
The study was conducted in Wangjiang county of Anhui province, China, from March 2004 to May 2004. Hypertensive patients, defined as having systolic blood pressure (SBP) ⩾140 mm Hg and/or diastolic blood pressure (DBP) ⩾90 mm Hg, were enrolled using the following criteria: (1) 35–60 years old; (2) not taking antihypertensive medications for 4 weeks before this study; (3) no current daily medications that may have interactions with nifedipine; (4) no habit of drinking grapefruit juice; (5) having an SBP not higher than 200 mm Hg and DBP not higher than 115 mm Hg; (6) not diagnosed as having secondary hypertension; (7) not diagnosed as having acute coronary syndrome or transient ischemia attack in the last 3 months; (8) not diagnosed as having myocardial infarction, stroke, heart failure, severe liver dysfunction, severe kidney dysfunction or other diseases that may affect the drug's efficacy or the patient's safety; and (9) not pregnant or lactating. All patients signed their informed consents before they took part in the study. The study procedure was approved by the Institutional Review Board of Anhui Medical University, China.
Procedures
Participants were invited to our research center 1 day before the treatment and were enrolled in the study after a screening examination including questionnaire inquiry, physical examination, biochemical measurements, electrocardiogram and abdominal B ultrasound. After an overnight fast, patients had their baseline blood pressure measured at 0800 hours, after which they took 30 mg nifedipine GITS (Adalat, Bayer Healthcare Pharmaceutical Division, Beijing, China) orally. Their blood pressure was monitored at 1, 2, 4 and 6 h after the administration. Patients then left and began to take nifedipine GITS 30 mg once daily around 0800 hours in the morning. They were asked to record information regarding their response and lifestyle changes everyday. Patients returned to the research center in the afternoon on the fifteenth day and the same procedures as those of the first day were repeated on the sixteenth day.
Blood pressure measurement
After resting for 30 min, patient's seated blood pressure was measured on the right arm by two trained nurses simultaneously, using a mercury sphygmomanometer with an appropriate-sized cuff and a special stethoscope with two sets of headsets. SBP was defined as the appearance of the sound (Korotkoff phase I) and DBP was defined as the disappearance of the sound (Korotkoff phase V). Blood pressure was measured thrice consecutively by each nurse, and the average of these values was used for data analysis.
Plasma drug concentration measurement
As nifedipine is susceptible to photodegradation, plasma concentration of nifedipine was measured under red light in a dark room using HPLC with UV detection. In brief, 500 μl of a heparin anticoagulant plasma sample, together with 100 μl of internal standard diazepam (200 ng ml−1, dissolved with methanol; The State Narcotic Laboratory, Beijing, China) and 100 μl of sodium hydroxide, was put into a 10-ml polypropylene tube. The mixture was first vortexed for 1 min, and then mixed with 3 ml another mixture (3:1, v/v) of diethyl ether and n-hexane. After vortexing for 1 min, the mixture was centrifuged at 4500 r.p.m. for 15 min. The supernatant was then transferred to a 2-ml microcentrifuge tube and dried using nitrogen flow. The residuals were dissolved with 200 μl methanol and centrifuged at 6500 r.p.m. for 10 min. A total volume of 20 μl supernatant was injected into the Agilent 1100 series HPLC system (Agilent, Santa Clara, CA, USA). The wavelength of the UV detector was set at 238 nm. A Diamosil C18 column (5 μm, 150 × 4.6 mm; Beijing Dikma Technology Co. Ltd, Beijing, China) was used for the analysis, and its temperature was set at 30 °C. The mobile phase consisted of acetonitrile and water (45:55, v/v), and its flow rate was 1.0 ml min−1. A calibration curve of nifedipine (National Institute for the Control of Pharmaceutical and Biological Products, Beijing, China) was drawn using a series of standard working solutions dissolved with methanol. The concentrations were 5, 10, 30, 50, 100 and 200 ng ml−1. A linear relationship was observed between the peak area of nifedipine and the corresponding concentration in this range. Quantification of plasma nifedipine concentration was calculated by comparing its peak area with that of the internal standard.
Genotyping
Polymorphisms were genotyped using TaqMan assay, a fluorescence-based PCR method. The primers and probes are summarized in Table 1. A total volume of 5 μl reaction mixture containing 9 ng genomic DNA, 1 × TaqMan universal PCR master mix and 1 × assay mix (Applied Biosystems, Foster City, CA, USA) was carried out on a DTC-225 Themocycler (MJ Research, Watertown, MA, USA) using the following program. The initial denaturation was performed at 95 °C for 10 min, followed by 50 cycles of 15 s at 92 °C and 60 s at 60 °C. The PCR products were then read on a TaqMan 7900 machine (Applied Biosystems). Different genotypes were called by different clusters resulting from dye-specific fluorescent intensity.
Statistical analysis
Data analysis was carried out using the SAS 8.2 software package (SAS Institute, Cary, NC, USA). Blood pressure reduction was calculated by subtracting the blood pressure right before taking nifedipine GITS on the sixteenth day from the baseline blood pressure on the first day. As the distribution of plasma concentrations of nifedipine was skewed with a long tail to the right, the log-transformed value of plasma drug concentration was used to achieve a more normal distribution. Quantitative variables of the basic characteristics, such as age, were compared using t-test or analysis of variance among two or three genotype groups, respectively. Categorical variables of the basic characteristics, such as gender frequency, were compared using a χ2-test. Multivariate linear regression analysis was carried out to estimate the association of different genotypes and blood pressure reduction, adjusting for age, gender, body mass index (BMI), smoking status, drinking status, the sixteenth-day steady state plasma drug concentration (log-transformed value) and baseline blood pressure. P<0.05 was considered statistically significant.
Results
A total of 447 hypertensive patients with complete phenotype data were finally included in our analysis. Among them, six patients had missing genotype data of the Arg347Cys polymorphism in the ADRA1A gene, three patients had missing genotype data of the Arg16Gly polymorphism in the ADRB2 gene and one patient had missing genotype data of the Gln27Glu polymorphism in the ADRB2 gene. The genotype distribution and allele frequency of these polymorphisms are shown in Table 2. The minor allele frequencies of the Arg347Cys, Arg16Gly and Gln27Glu polymorphisms were 10.7, 45.7 and 10.2%, respectively. As only five patients carried the Cys/Cys genotype of the ADRA1A gene and six patients carried the Glu/Glu genotype of the ADRB2 gene, and their BP reduction trends were similar with those of their heterozygotes (data not shown), we combined heterozygote and homozygote mutants together in our further analysis.
The basic characteristics of patients are summarized in Table 3, stratified by different genotypes of the ADRA1A gene. Patients carrying the Cys347 allele of the ADRA1A gene were younger (51.1±5.6 versus 52.5±5.6, P=0.034) and had a higher steady-state plasma drug concentration than those carrying two Arg347 alleles of the ADRA1A gene (log-transformed value, 3.4±0.7 versus 3.2±0.8, P=0.019). There were no significant differences in other covariates between two groups, including BMI, gender, smoking status, drinking status and baseline blood pressure. In addition, no significant differences of basic characteristics were found between those groups stratified by genotypes of Arg16Gly or Gln27Glu polymorphism in the ADRB2 gene (data not shown).
The associations between blood pressure reduction 24 h after the fifteenth administration and three polymorphisms are shown in Table 4. We found that patients carrying the Cys347 allele of the ADRA1A gene had a significantly greater SBP reduction (β=5.2, P=0.004) and a greater DBP reduction (β=2.0, P=0.028) than those carrying two Arg347 alleles of the ADRA1A gene in the crude analysis. Moreover, the difference of SBP reduction in response to nifedipine GITS between the two groups remained statistically significant (β=4.1, P=0.006) after adjustment for major demographic and clinical covariates, including age, gender, BMI, smoking status, drinking status, the sixteenth-day steady-state plasma drug concentration (log-transformed value) and baseline blood pressure. There was also a trend toward a greater DBP reduction in the non-Arg347 homozygote group, although this difference did not achieve statistical significance after adjustment. In addition, no significant results were observed between different genotype groups of either Arg16Gly or Gln27Glu polymorphism in the ADRB2 gene.
Discussion
To our knowledge, a few studies with a small sample size have been conducted to investigate whether genetic factors could predict the antihypertensive effect of CCB therapy.8, 9 In this study, we showed that hypertensive patients carrying the Cys347 allele of the ADRA1A gene had a better SBP reduction in response to short-term nifedipine GITS medication than did those carrying two Arg347 alleles of the ADRA1A gene. No significant association was observed between DBP reduction and the Arg347Cys polymorphism in the ADRA1A gene. In addition, blood pressure response to nifedipine GITS was also not associated with either the Arg16Gly or the Gln27Glu polymorphism in the ADRB2 gene.
The sympathetic nervous system plays a major role in blood pressure regulation by modulating cardiac and vascular contractility. Vascular contraction is controlled primarily by α1-adrenoceptors through their responses to endogenous noradrenaline and adrenaline. Its importance in blood pressure regulation is emphasized by the efficacy of α1-adrenoceptor antagonists in the treatment of human hypertension. Currently, three α1-adrenoceptor subtypes have been characterized as follows: α1A-adrenoceptor (including the former α1C-adrenoceptor), α1B-adrenoceptor and α1D-adrenoceptor. Of the three subtypes, the α1A-adrenoceptor has been implicated in regulating vascular resistance in many species. Studies showed that α1A-adrenoceptors mediated the contractions of both animal and human blood vessels.10, 11, 12, 13 Animal studies also indicated that the α1A-adrenoceptor subtype was required for normal arterial blood pressure regulation. ADRA1A gene knockout (KO) mice exhibited an 8–12% reduction in blood pressure depending on gene copy numbers. Phenylephrine, a subtype-nonselective agonist, raised blood pressure in KO mice, but the final arterial pressure was only 85% of that of the wild type.14 Taken together, it suggests that α1A-adrenoceptors play a key role in the regulation of peripheral vascular resistance and blood pressure in mammals.
An increase in intracellular calcium plays a primary role in triggering the contraction of vascular smooth muscles. Both Ca2+, released from intracellular stores and influx through membrane calcium channels, are involved in the activation of α1A-adrenoceptors. Vasodilation induced by the inhibition of Ca2+ influx into vascular smooth muscle cells represents the main mechanism for the antihypertensive effect of nifedipine. It has been suggested that α1A-adrenoceptors can selectively activate Ca2+ influx through dihydropyridine-sensitive channels in smooth muscle.15, 16 Consistent with these findings, α1A-adrenoceptor-mediated constriction of the swine renal artery smooth muscle ring was found to be inhibited by 85% by nifedipine.17
Substitution of C for T in the ADRA1A gene caused an amino-acid alteration from Arg347 to Cys347. The Cys347 residue, located at the intracellular carboxyl terminus, might serve as an additional putative palmitoylation site of the α1A-adrenoceptor. In transfected Chinese hamster ovary cells, two polymorphic α1A-adrenoceptors (Arg347 and Cys347) exhibited similar characteristics in antagonist- and agonist-binding affinities.18 However, whether this polymorphism can affect Ca2+ influx through L-type calcium channels is still unknown. An alternative explanation for our finding is that the Arg347Cys polymorphism is in linkage disequilibrium with real functional genetic variants, which are actually responsible for the interindividual variation of blood pressure reduction in response to nifedipine GITS. Further studies are necessary to functionally characterize the ADRA1A variants and to identify other functional polymorphisms in this region.
β2-Adrenoceptors are well known to regulate vasodilatation. As the functional implications of the Arg16Gly and Gln27Glu polymorphisms were revealed in vitro, their effects on the agonist-induced vasodilator response have also been investigated in vivo, and the results were controversial.19, 20, 21, 22, 23 Moreover, there was also no significant association detected between the blood pressure response to hydrochlorothiazide or atenolol and the Arg16Gly polymorphism in several studies.24, 25
An attenuation of β-adrenergic function and a potentiation of α-adrenergic function in cardiovascular tissues have been shown in hypertensive patients, suggesting the development of a postsynaptic α1 function dominance during the development and evolution of hypertension. The higher baseline activity of α1A-adrenoceptors could result in greater functional differences between different genotypes of the ADRA1A gene, and thus affect the interindividual variation in response to nifedipine GITS.
It is known that pharmacokinetic characteristics can contribute to the interindividual variation in response to medications. Several studies have suggested that changes in nifedipine concentrations significantly correlated with changes in blood pressure.26, 27 GITS formulation provides a continuous and slow zero-order drug release, resulting in a smooth plasma concentration/time profile. The plasma concentration of nifedipine can reach a plateau within 6 h and continue at that concentration for at least 24 h after administration.28 The major advantage of our study is the measurement of steady-state plasma drug concentration on the sixteenth day. The fact that the positive findings remained after adjustment for plasma nifedipine concentration made our results much more convincing. In addition, the patients were relatively homogenous as they were from the same county. However, we still cannot exclude the possibility that the significant result was because of population admixture, which is the major limitation of population-based association studies.
In conclusion, our study suggests that the Arg347Cys polymorphism in the ADRA1A gene may predict the short-term antihypertensive effect of nifedipine GITS 30 mg, administered once daily in hypertensive patients of Anhui Province, China. Our study represents the very first step in understanding the genetic mechanisms of interindividual variation in response to nifedipine GITS in hypertensive patients. In the future, it would be interesting to confirm our results in other independent populations.
References
Brown, M. J., Palmer, C. R., Castaigne, A., de Leeuw, P. W., Mancia, G. & Rosenthalm, T. et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT). Lancet 356, 366–372 (2000).
Krakoff, L. R. Effectiveness of nifedipine gastrointestinal therapeutic system for treatment of hypertension: results of the MATH Trial. J. Cardiovasc. Pharmacol. 21, S14–S17 (1993).
Hingorani, A. D., Jia, H., Stevens, P. A., Hopper, R., Dickerson, J. E. & Brown, M. J. Renin–angiotensin system gene polymorphisms influence blood pressure and the response to angiotensin converting enzyme inhibition. J. Hypertens. 13, 1602–1609 (1995).
Psaty, B. M., Smith, N. L., Heckbert, S. R., Vos, H. L., Lemaitre, R. N., Reiner, A. P. et al. Diuretic therapy, the alpha-adducin gene variant, and the risk of myocardial infarction or stroke in persons with treated hypertension. JAMA 287, 1680–1689 (2002).
Moffett, S., Mouillac, B., Bonin, H. & Bouvier, M. Altered phosphorylation and desensitization patterns of a human beta 2-adrenergic receptor lacking the palmitoylated Cys341. EMBO J. 12, 349–356 (1993).
O'Dowd, B. F., Hnatowich, M., Regan, J. W., Leader, W. M., Caron, M. G. & Lefkowitz, R. J. Site-directed mutagenesis of the cytoplasmic domains of the human beta 2-adrenergic receptor. Localization of regions involved in G protein-receptor coupling. J. Biol. Chem. 263, 15985–15992 (1988).
Green, S. A., Turki, J., Innis, M. & Liggett, S. B. Amino-terminal polymorphisms of the human beta 2-adrenergic receptor impart distinct agonist-promoted regulatory properties. Biochemistry 33, 9414–9419 (1994).
Benetos, A., Cambien, F., Gautier, S., Ricard, S., Safar, M., Laurent, S. et al. Influence of the angiotensin II type 1 receptor gene polymorphism on the effects of perindopril and nitrendipine on arterial stiffness in hypertensive individuals. Hypertension 28, 1081–1084 (1996).
Dudley, C., Keavney, B., Casadei, B., Conway, J., Bird, R. & Ratcliffe, P. Prediction of patient responses to antihypertensive drugs using genetic polymorphisms: investigation of renin–angiotensin system genes. J. Hypertens. 14, 259–262 (1996).
Nair, R. & Dyer, D. C. Pharmacological characterization of alpha 1-adrenoceptors in porcine uterine artery. Eur. J. Pharmacol. 312, 45–51 (1996).
Rudner, X. L., Berkowitz, D. E., Booth, J. V., Funk, B. L., Cozart, K. L., D'Amico, E. B. et al. Subtype specific regulation of human vascular alpha(1)-adrenergic receptors by vessel bed and age. Circulation 100, 2336–2343 (1999).
Testa, R., Guarneri, L., Taddei, C., Poggesi, E., Angelico, P., Sartani, A. et al. Functional antagonistic activity of Rec 15/2739, a novel alpha-1 antagonist selective for the lower urinary tract, on noradrenaline-induced contraction of human prostate and mesenteric artery. J. Pharmacol. Exp. Ther. 277, 1237–1246 (1996).
Villalobos-Molina, R., Lopez-Guerrero, J. J. & Ibarra, M. Alpha 1D- and alpha 1A-adrenoceptors mediate contraction in rat renal artery. Eur. J. Pharmacol. 322, 225–227 (1997).
Rokosh, D. G. & Simpson, P. C. Knockout of the alpha 1A/C-adrenergic receptor subtype: the alpha 1A/C is expressed in resistance arteries and is required to maintain arterial blood pressure. Proc. Natl Acad. Sci. USA 99, 9474–9479 (2002).
Han, C., Abel, P. W. & Minneman, K. P. Alpha 1-adrenoceptor subtypes linked to different mechanisms for increasing intracellular Ca2+ in smooth muscle. Nature 329, 333–335 (1987).
Han, C., Li, J. & Minneman, K. P. Subtypes of alpha 1-adrenoceptors in rat blood vessels. Eur. J. Pharmacol. 190, 97–104 (1990).
Eckert, R. E., Karsten, A. J., Utz, J. & Ziegler, M. Regulation of renal artery smooth muscle tone by alpha1-adrenoceptors: role of voltage-gated calcium channels and intracellular calcium stores. Urol. Res. 28, 122–127 (2000).
Shibata, K., Hirasawa, A., Moriyama, N., Kawabe, K., Ogawa, S. & Tsujimoto, G. Alpha 1a-adrenoceptor polymorphism: pharmacological characterization and association with benign prostatic hypertrophy. Br. J. Pharmacol. 118, 1403–1408 (1996).
Cockroft, J. R., Gazis, A. G., Cross, D. J., Wheatley, A., Dewar, J., Hall, I. P. et al. β2-Adrenoceptor polymorphism determines vascular reactivity in humans. Hypertension 36, 371–375 (2000).
Dishy, V., Sofowora, G. G., Xie, H. G., Kim, R. B., Byrne, D. W., Stein, C. M. et al. The effect of common polymorphisms of the beta2-adrenergic receptor on agonist-mediated vascular desensitization. N. Engl. J. Med. 345, 1030–1035 (2001).
Garovic, V. D., Joyner, M. J., Dietz, N. M., Boerwinkle, E. & Turner, S. T. β2-Adrenergic receptor polymorphism and nitric oxide-dependent forearm blood flow responses to isoproterenol in humans. J. Physiol. 546, 583–589 (2003).
Gratze, G., Fortin, J., Labugger, R., Binder, A., Kotanko, P., Timmermann, B. et al. Beta-2 adrenergic receptor variants affect resting blood pressure and agonist-induced vasodilation in young adult Caucasians. Hypertension 33, 1425–1430 (1999).
Hoit, B. D., Suresh, D. P., Craft, L., Walsh, R. A. & Liggett, S. B. Beta2-adrenergic receptor polymorphisms at amino acid 16 differentially influence agonist-stimulated blood pressure and peripheral blood flow in normal individuals. Am. Heart J. 139, 537–542 (2000).
Liljedahl, U., Karlsson, J., Melhus, H., Kurland, L., Lindersson, M., Kahan, T. et al. A microarray minisequencing system for pharmacogenetic profiling of antihypertensive drug response. Pharmacogenetics 13, 7–17 (2003).
Turner, S. T., Chapman, A. B., Schwartz, G. L. & Boerwinkle, E. Effects of endothelial nitric oxide synthase, alpha-adducin, and other candidate gene polymorphisms on blood pressure response to hydrochlorothiazide. Am. J. Hypertens. 16, 834–839 (2003).
Banzet, O., Colin, J. N., Thibonnier, M., Singlas, E., Alexandre, J. M. & Corvol, P. Acute antihypertensive effect and pharmacokinetics of a tablet preparation of nifedipine. Eur. J. Clin. Pharmacol. 24, 145–150 (1983).
Taburet, A. M., Singlas, E., Colin, J. N., Banzet, O., Thibonnier, M. & Corvol, P. Pharmacokinetic studies of nifedipine tablet. Correlation with antihypertensive effects. Hypertension 5, II 29–33 (1983).
Chung, M., Reitberg, D. P., Gaffney, M. & Singleton, W. Clinical pharmacokinetics of nifedipine gastrointestinal therapeutic system. A controlled-release formulation of nifedipine. Am. J. Med. 83, 10–14 (1987).
Acknowledgements
This study was supported in part by the Anhui Provincial Ministry of Education, Anhui Medical University Biomedical Institute. We thank the faculties and staffs of both Anhui Medical University and Peking University First Hospital. We are also grateful to all study participants and their families for their assistance and cooperation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Y., Hong, X., Liu, H. et al. Arg347Cys polymorphism of α1A-adrenoceptor gene is associated with blood pressure response to nifedipine GITS in Chinese hypertensive patients. J Hum Genet 54, 360–364 (2009). https://doi.org/10.1038/jhg.2009.42
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2009.42
Keywords
This article is cited by
-
Pharmacogenetics of the response to antihypertensive drugs
Current Cardiovascular Risk Reports (2009)