Abstract
Objective:
To compare the clinical characteristics and placental histopathology between pregnancies complicated by placenta previa and controls.
Study Design:
Between 2009 and 2015, cesarean deliveries (CDs) of 119 pregnancies with placenta previa were identified from which maternal outcomes, neonatal outcomes and placental pathology were reviewed. Results were compared with CDs matched for maternal age and pregnancy complications (control group, n=119). Placental lesions were classified into maternal and fetal vascular supply lesions and inflammatory response. Composite neonatal outcome was defined as one or more of early neonatal complications. Small-for-gestational age (SGA) was defined as birth weight ⩽10th percentile.
Results:
Placentas from the previa group had higher rates of weights <10th percentile (P<0.001) and of maternal and fetal vascular supply lesions (P<0.001, for both). Higher rate of SGA (P=0.003) and worse composite neonatal outcome (P<0.001) were also observed in the previa group as compared with controls. After controlling for potential confounding bias using multivariable logistic regression models, placenta previa remained statistically significantly associated with placental maternal (adjusted odds ratio (aOR) 2.48, 95% confidence interval (CI) 1.2–4.9, P=0.009) and fetal (aOR 7.05, 95% CI 2.4–20.2, P<0.001) vascular supply lesions, SGA (aOR 10, 95% CI 2.3–44.2, P=0.002) and adverse neonatal outcome (aOR 6.87, 95% CI 2.9–11.8, P<0.001).
Conclusions:
More placental vascular supply lesions, higher rate of SGA and worse neonatal outcome characterized pregnancies with placenta previa in the current study. These findings may suggest that abnormal placentation is accompanied by suboptimal implantation that interferes with fetal growth.
Similar content being viewed by others
Introduction
Placenta previa is described as suboptimal placental implantation over or very near the internal cervical os. Most of the placenta previas that are observed by transvaginal ultrasound scans before 20 weeks of gestation will no longer be present near term.1, 2 Only 1 in 200 pregnancies are complicated by persistent placenta previa at delivery.3 The incidence of placenta previa appears to increase in a dose-dependent manner such that increasing number of prior cesarean deliveries (CDs) is associated with increasing incidence rates of placenta previa in subsequent pregnancies.4 Other risk factors for placenta previa include previous spontaneous and elective pregnancy terminations, previous uterine surgeries,5 parity, advanced maternal age, smoking, cocaine use, multiple gestations, in vitro fertilization and prior placenta previa.6, 7, 8
Pregnancies complicated by placenta previa have been associated with adverse maternal and neonatal outcomes. Preterm and early-term deliveries, prematurity, low Apgar scores, fetal and neonatal death,9, 10, 11 maternal intrapartum and postpartum hemorrhage, the need for blood transfusion, sepsis and hysterectomy3, 9, 12, 13, 14 were observed at increased rates in pregnancies complicated by placenta previa.
The pathophysiology of placenta previa is still unclear. It appears to be associated with endometrial damage and uterine wall scarring, which may interfere with the normal process of placental implantation and development. Moreover, the possible effect of placenta previa, on placental function and consequently on the growing fetus, is controversial.9, 15, 16, 17, 18, 19, 20, 21, 22 Notably, the effect of this abnormal placentation on placental histopathological lesions has not been addressed adequately.
The aim of the present study was to fill this gap and to compare the clinical characteristics, neonatal and maternal outcomes and the placental histopathology between pregnancies complicated by placenta previa and controls. Placental lesions were compared using the classification to three major categories: placental maternal vascular supply lesions, placental fetal vascular supply lesions, and lesions consistent with maternal and fetal inflammatory response.23, 24
MATERIALS AND METHODS
The medical records of all women who underwent CDs for placenta previa between 24 and 42 weeks of gestation from January 2009 to April 2015 were reviewed. The diagnosis of placenta previa was confirmed in all women by third trimester transvaginal ultrasound scans.25 In all cases, the placentas were sent to histopathology for evaluation, in accordance with the departmental policy that routinely performs placental analyses in all complicated pregnancies, and randomly also in women with an uncomplicated pregnancy for research purposes.
Excluded from the study were multiple gestations, deliveries <24 weeks of gestation, known fetal or neonatal malformation, cases with concurrent placenta accrete and cases with missing data.
The control group included women who underwent an elective CD during the same time period, owing to malpresentation or previous CD, and their placentas were sent for histopathological evaluation. The controls were matched, on a 1:1 basis, to the study group (previa group) for maternal age (±1 year) and pregnancy complications, including the presence of preeclampsia, diabetes mellitus and thrombophilias. For the purpose of the study, data were compared between the previa and control groups.
Approval was obtained from the Local Ethics Committee.
Data collection
The following data were collected from the admission file of each woman: age, gravidity, parity, previous CDs, gestational age (confirmed by first-trimester ultrasonography), prepregnancy body mass index (BMI, kg m−2), cigarette smoking, pregnancies achieved by assisted reproductive techniques (ovulation induction or in vitro fertilization), and pregnancy complications such as: preeclampsia, chronic hypertension, gestational diabetes mellitus (A1 and A2), pregestational diabetes mellitus, and thrombophilia (defined as any thrombophilia inherited or acquired that necessitated thromboprophylaxis).26, 27
The following data were collected from the surgical report and postpartum file of each woman: hospitalization (days), preoperative hemoglobin concentrations, 24 h postpartum hemoglobin concentration, postpartum hemorrhage that necessitated the use of uterotonic medications, hysterectomy, uterine/hypogastric artery ligation, the need for re-laparotomy, intensive care unit (ICU) admission, and the need for blood product transfusion. Significant blood loss was defined as a difference in hemoglobin concentration ⩾3 g dl−1 between the preoperative and postpartum hemoglobin levels.
Immediately after birth, all neonates were examined by pediatricians. Birth weight percentile for gestational age was assigned using the updated Israeli growth charts.28 Small-for-gestational age (SGA) was defined as actual birth weight ⩽10th percentile or ⩽5th percentile for gestational age. The following information was collected from the neonatal records: Apgar scores, cord blood pH, neonatal hospitalization, neonatal ICU (NICU) admissions, sepsis (positive blood or cerebrospinal fluid culture), need for blood transfusion, need for phototherapy, respiratory distress syndrome, need for mechanical ventilation or support, necrotizing enterocolitis, intraventricular hemorrhage (all grades), hypoxic ischemic encephalopathy, seizures, and death.
Placental examination
Placental histopathology examinations were performed using our standard protocol by a single pathologist (LS). Placental lesions were classified by maternal or fetal origin, according to the criteria adopted by the Society for Pediatric Pathology24 and as we previously reported.29 Briefly, placental weight was determined 24 h after delivery, and the percentile was determined according to placental weight charts.30 Each placenta was fixed in formalin, and at least five samples were embedded in paraffin blocks for microscopic assessment.
Placental lesions
Lesions of maternal vascular supply included: placental hemorrhages (marginal and retro-placental), vascular changes associated with maternal malperfusion (acute atherosis and mural hypertrophy), and villous changes associated with maternal malperfusion (increased syncytial knots, villous agglutination, increased intervillous fibrin deposition, distal villous hypoplasia and villous infarcts).
Lesions of fetal vascular supply were defined as findings consistent with fetal thrombo-occlusive disease: vascular lesions (thrombosis of the chorionic plate and stem villous vessels) and villous changes (hypovascular, fibrotic and avascular villi).
Findings consistent with chorioamnionitis were defined by the presence of an inflammatory neutrophil infiltrate at two or more sites on the chorionic plate and extraplacental membrane. Maternal inflammatory response was divided into three stages: stage 1—characterized by the presence of a few scattered neutrophils in the subchorionic space; stage 2—characterized by many neutrophils (11–30 per high-power field) in the lower half of the chorionic plate; and stage 3—characterized by dense infiltrates of neutrophils (>30 per high-power field) throughout the chorionic plate. Fetal inflammatory response was also divided into 3 stages: stage 1—early, umbilical phlebitis; stage 2—intermediate, umbilical arteritis; and stage 3—concentric umbilical perivasculitis (necrotizing funisitis).
The umbilical cord was examined for the detection of hypercoiling and abnormal cord insertion. Umbilical coiling index was calculated by dividing the total number of coils by the length of the cord in centimeters. Hypercoiling was diagnosed in cases of umbilical coiling index ⩾0.3 coils cm−1, and hypocoiling was diagnosed in cases of umbilical coiling index ⩽0.1 coils cm−1.31 Abnormal cord insertion was defined as either velamentous or marginal insertion.
Statistical analysis
Data were analyzed with the SPSS software, version 21.0 (SPSS, Chicago, IL, USA). Continuous variables are presented as mean±s.d. or median and range, as appropriate. Categorical variables are presented as rate (%). Continuous parameters were compared by Student’s t-test and categorical variables by chi-square test or by Fisher’s exact test, as appropriate. P-value of <0.05 was considered statistically significant.
Composite placental maternal vascular supply lesions was defined as the presence of one or more maternal vascular supply abnormalities, and composite placental fetal vascular supply lesions was defined as the presence of one or more fetal vascular supply abnormalities.
Composite adverse neonatal outcome was defined as one or more of the following complications: neonatal sepsis, blood transfusion, phototherapy, respiratory morbidity (presence of respiratory distress syndrome, transient tachypnea of the newborn, mechanical ventilation or need for respiratory support), cerebral morbidity (presence of intraventricular hemorrhage, seizures or hypoxic–ischemic encephalopathy), necrotizing enterocolitis, or death.
Composite maternal hemorrhagic morbidity included one or more of the following maternal surgical and postpartum complications: hysterectomy, uterine/hypogastric artery ligation, and the need for re-laparotomy, ICU admission, or the need for blood product transfusion.
To identify independent risk factors for the presence of placental weight ⩽10th percentile, placental maternal vascular supply lesions (composite) and for placental fetal vascular supply lesions (composite), multivariate logistic regression analyses were performed. Placental weight ⩽10th percentile, composite placental maternal vascular supply lesions and composite placental fetal vascular lesions served as the dependent variables, whereas placenta previa, maternal age, gestational age, parity, smoking, thrombophilia and BMI served as independent variables.
To identify independent risk factors for SGA (birth-weight ⩽10th percentile) and for adverse neonatal outcome, multivariate logistic regression analyses were performed. SGA and composite adverse neonatal outcome served as the dependent variables, whereas placenta previa, maternal age, gestational age, parity, smoking, thrombophilia and BMI served as independent variables.
Results
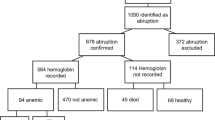
During the study period, 158 women with placenta previa, out of 28 376 deliveries (0.56%), underwent CD. The study group included 119 women after excluding 39 cases, owing to multiple pregnancy,15 concurrent placenta accrete14 and incomplete data.10
Table 1 presents maternal and pregnancy characteristics of the study groups.
Women in the previa group were less likely to be nulliparous (P<0.001), had a higher rate of cigarette smoking (P=0.038) and gave birth at earlier gestational ages (35.8±4.4 vs 38.8±2.9 weeks, P<0.001) as compared with controls. There were no differences in maternal age, maternal BMI and the rate of pregnancies achieved by assisted reproductive techniques between the groups. As expected from the study design, both groups had similar rates of gestational or pregestational diabetes mellitus (10%), preeclampsia (0.8%) and thrombophilia (2.5%).
Table 2 presents the placental characteristics of the previa group as compared with controls. Mean placental weight was significantly lower in the previa group as compared with the controls (432±126 vs 498±108 g, P<0.001, respectively). In addition, the previa group had a higher rate of placental weight below the 10th percentile, (P<0.001). Higher rates of maternal placental vascular lesions related to maternal malperfusion, placental hemorrhages and composite placental maternal vascular supply lesions were also detected in the previa group as compared with the control group (P=0.019, P<0.001, P<0.001, respectively). Additionally, higher rates of placental lesions consistent with fetal thrombo-occlusive disease, (vascular and villous), as well as higher rates of composite fetal vascular lesions, were observed in the previa group as compared with the controls (P=0.024, P=0.049, P<0.001, respectively). Moreover, placentas in the previa group had more abnormal cord insertion as compared with the control group (16.5% vs 5.9%, P=0.013). There were no significant between-group differences in rates of placental inflammatory lesions and abnormal coiling of the cord. Using multivariate logistic regression analyses, composite placental maternal vascular supply lesions and composite placental fetal vascular supply lesions were independently associated with placenta previa (adjusted odds ratio (aOR)=2.48, 95% confidence interval (CI) 1.2–4.9, P=0.009 and aOR 7.05, 95% CI 2.4–20.2, P<0.001, respectively). In addition, placental weight <10th percentile was also independently associated with placenta previa (aOR=6.58, 95% CI 2.6–16.7, P<0.001) after controlling for background maternal confounders (maternal age, gestational age, parity, smoking, thrombophilia and BMI).
Neonatal outcome parameters are summarized in Table 3. Increased rates of SGA neonates, below the 10th percentile and below the 5th percentile, were observed in the previa group as compared with controls (15.1% vs 3.4%, P=0.003 and 6.7% vs 0%, P=0.005, respectively). Neonates in the previa group had a longer hospitalization (12.7±15.1 vs 4.8±3.9 days, P<0.001) and higher rate of NICU admission (38.7% vs 14.3%, P<0.001), as compared with neonates in the control group. Composite neonatal outcome was worse in the previa group as compared with the control group (45.3 vs 11.8%, P<0.001). Using multivariate logistic regression analysis, SGA ⩽10th percentile (aOR 10.09, 95% CI 2.3–44.2, P=0.002), NICU admission (aOR 3.87, 95% CI 2.5–12.3, P<0.001) and composite adverse neonatal outcome (aOR 6.87, 95% CI 2.9–11.8, P<0.001) remained independently associated with placenta previa after controlling for background maternal confounders (maternal age, gestational age, parity, smoking, thrombophilia and BMI).
Table 4 presents the maternal postpartum outcome. As compared with the controls, women in the previa group had longer hospitalization (7.0±2.1 vs 4.3±1.7 days, P<0.001) and higher rate of composite maternal hemorrhagic morbidity (26.9% vs 5.9%, P<0.001). Using a multivariate logistic regression analysis, composite maternal hemorrhagic morbidity (aOR=5.32, 95% CI 2.4–15.3, P<0.001) and significant blood loss (aOR 4.36, 95% CI 2.6–17.3, P<0.001) remained independently associated with placenta previa after controlling for background maternal confounders (maternal age, gestational age, parity, smoking, thrombophilia and BMI).
Discussion
In the present study, differences in the morphological appearance of placentas from pregnancies complicated by placenta previa as compared with normal placental implantation were observed. Moreover, pregnancies with placenta previa were characterized by SGA neonates and worse maternal and neonatal outcomes.
Placental pathology is a valuable link that may explain how underlying pathology results in adverse pregnancy outcomes. Yet, the effect of an abnormal implantation site, as in placenta previa, on placental histopathology lesions is unknown. In the current study, we observed that placentas from pregnancies complicated by placenta previa were smaller with higher rate of placental weight below the 10th percentile. Additionally, these placentas had significantly more of the characteristic vascular lesions associated with placental hemorrhages, maternal malperfusion and fetal thrombo-occlusive disease, known to occur in preeclampsia and fetal growth restriction.32 By multivariate regression analyses, placental weight <10th percentile and placental vascular lesions (maternal and fetal) were independently associated with placenta previa. In a recent review,33 it has been pointed out that developmental abnormalities of the maternal stromal-vascular compartment of the placenta contribute to placental dysfunction via malperfusion and loss of integrity. In concordance with it, the current findings suggest that abnormal site of implantation may result in abnormal placental development that may compromise fetal development. Notably, the higher rate of abnormal cord insertion observed in placenta previa as compared with controls is in concordance with others,34 and it correlates with increased rate of placental vascular lesions.35 Heidari et al.36 performed a stereological analysis of 10 placentas from pregnancies complicated by placenta previa and observed significant changes in the structure of the placenta as compared with controls. Yet, compared with our findings, placental bed biopsies in cases of placenta previa demonstrated a significantly higher trophoblastic giant cell infiltration in decidua and myometrial blood vessels,37 suggesting that placenta previa is associated with normal physiological changes of the spiral arteries.
In the current study, we demonstrate that pregnancies complicated by placenta previa were associated with SGA neonates. SGA below the 10th percentile was independently associated with placenta previa, aOR 10.09, 95% CI 2.3–44.2, P=0.002. Indeed, the association between placenta previa and SGA has been studied with differing results, between no correlations,18, 19, 20, 21, 22 to increased risk.9, 15, 16, 17 Our findings suggest an etiopathogenesis for the development of SGA in pregnancies complicated with placenta previa, probably via the vascular compromise that is a result from abnormal placentation and is expressed by placental maternal and fetal vascular supply lesions.
Several studies have reported an increased incidence of placental maternal vascular lesions in pregnancies complicated by SGA neonates, while others have demonstrated a combined maternal and fetal compartment involvement in the development of growth restriction and SGA neonates.38, 39 Importantly, placental fetal vascular supply lesions are also known to be important contributors to adverse pregnancy outcome.40, 41 In the same line, worse neonatal outcome was observed in the current study in cases with placenta previa. Deliveries in pregnancies complicated by placenta previa are more likely to occur preterm. It is well established that late preterm birth is still associated with adverse neonatal outcome, including respiratory morbidity, intraventricular hemorrhage, sepsis work-ups, sepsis, phototherapy for hyperbilirubinemia and neonatal death.42, 43, 44 However, in the current study adverse neonatal outcome was found to be independently associated with placenta previa (aOR 6.87, 95% CI 2.9–11.8, P<0.001), after adjustment for gestational age. These findings also support our hypothesis that suboptimal implantation, as occurs in placenta previa, results in abnormal placentation leading to placental malfunction with decreased placental perfusion.
The increased composite maternal hemorrhagic morbidity (26.9%), observed in pregnancies complicated by placenta previa, was expected, and it is in concordance with previous studies.3, 9, 12, 13, 14 It probably reflects inadequate muscles contractions, at the lower uterine segment, hence bleeding ensues from the placental bed.
Our study has several strengths. It is the first to our knowledge that describes histopathological lesions in pregnancies complicated by placenta previa and applies the placental histopathology strict criteria that were validated and adopted by the Society of Pediatrics Pathology.24 In addition, a single pathologist who was blinded to neonatal and maternal outcomes (but not to the diagnosis of placenta previa) performed all histopathological evaluations. We could find a control group matched to the study previa group by maternal age, pregnancy complications and mode of labor.
We are aware that our study is not without limitations. First, owing to its rare incidence, the placenta previa group is heterogeneous in terms of clinical presentation (with and without bleeding events). Second, this is a retrospective study, and although we observed a higher rate of SGA among the previa group, prenatal studies for growth restriction, such as Doppler flow velocity, were not available to all. Additionally, we designed the control group to match only for mode of delivery and maternal diseases but not for gestational age. It is well established that spontaneous preterm deliveries are associated with high rates of infection and inflammation.45, 46 In order to avoid these effects on the placental pathology and neonatal outcome, we preferred not to match the control group for gestational age. To overcome the issue of the differences in gestational age between the groups, we designed regression analysis models for each one of our findings and found that each of the findings (placental lesions, SGA and adverse neonatal and maternal outcomes) was associated with placenta previa independent of gestational age (and other background factors).
In conclusion, placental implantation over the internal cervical os is associated with abnormal placentation and increased placental maternal and fetal vascular supply lesions. As a consequence of the abnormal placentation, there is a decreased placental perfusion that interferes with fetal growth and development, resulting in a higher rate of SGA neonates and worse neonatal outcome.
References
Taipale P, Hiilesmaa V, Ylostalo P . Diagnosis of placenta previa by transvaginal sonographic screening at 12-16 weeks in a nonselected population. Obstet Gynecol 1997; 89 (3): 364–367.
Oyelese Y . Placenta previa: the evolving role of ultrasound. Ultrasound Obstet Gynecol 2009; 34 (2): 123–126.
Oyelese Y, Smulian JC . Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol 2006; 107 (4): 927–941.
Getahun D, Oyelese Y, Salihu HM, Ananth CV . Previous cesarean delivery and risks of placenta previa and placental abruption. Obstet Gynecol 2006; 107 (4): 771–778.
Ananth CV, Smulian JC, Vintzileos AM . The association of placenta previa with history of cesarean delivery and abortion: a metaanalysis. Am J Obstet Gynecol 1997; 177 (5): 1071–1078.
Ananth CV, Wilcox AJ, Savitz DA, Bowes WA Jr., Luther ER . Effect of maternal age and parity on the risk of uteroplacental bleeding disorders in pregnancy. Obstet Gynecol 1996; 88 (4 Pt 1): 511–516.
Macones GA, Sehdev HM, Parry S, Morgan MA, Berlin JA . The association between maternal cocaine use and placenta previa. Am J Obstet Gynecol 1997; 177 (5): 1097–1100.
Ananth CV, Demissie K, Smulian JC, Vintzileos AM . Placenta previa in singleton and twin births in the United States, 1989 through 1998: a comparison of risk factor profiles and associated conditions. Am J Obstet Gynecol 2003; 188 (1): 275–281.
Rosenberg T, Pariente G, Sergienko R, Wiznitzer A, Sheiner E . Critical analysis of risk factors and outcome of placenta previa. Arch Gynecol Obstet 2011; 284 (1): 47–51.
Faiz AS, Ananth CV . Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med 2003; 13 (3): 175–190.
Norgaard LN, Pinborg A, Lidegaard O, Bergholt T . A Danish national cohort study on neonatal outcome in singleton pregnancies with placenta previa. Acta Obstet Gynecol Scand 2012; 91 (5): 546–551.
Crane JM, Van den Hof MC, Dodds L, Armson BA, Liston R . Maternal complications with placenta previa. Am J Perinatol 2000; 17 (2): 101–105.
Rao KP, Belogolovkin V, Yankowitz J, Spinnato JA 2nd . Abnormal placentation: evidence-based diagnosis and management of placenta previa, placenta accreta, and vasa previa. Obstet Gynecol Surv 2012; 67 (8): 503–519.
Spong CY, Mercer BM, D'Alton M, Kilpatrick S, Blackwell S, Saade G . Timing of indicated late-preterm and early-term birth. Obstet Gynecol 2011; 118 (2 Pt 1): 323–333.
Raisanen S, Kancherla V, Kramer MR, Gissler M, Heinonen S . Placenta previa and the risk of delivering a small-for-gestational-age newborn. Obstet Gynecol 2014; 124 (2 Pt 1): 285–291.
Neri A, Gorodesky I, Bahary C, Ovadia Y . Impact of placenta previa on intrauterine fetal growth. Isr J Med Sci 1980; 16 (6): 429–432.
Ananth CV, Demissie K, Smulian JC, Vintzileos AM . Relationship among placenta previa, fetal growth restriction, and preterm delivery: a population-based study. Obstet Gynecol 2001; 98 (2): 299–306.
Kassem GA, Alzahrani AK . Maternal and neonatal outcomes of placenta previa and placenta accreta: three years of experience with a two-consultant approach. Int J Womens Health 2013; 5: 803–810.
Yeniel AO, Ergenoglu AM, Itil IM, Askar N, Meseri R . Effect of placenta previa on fetal growth restriction and stillbirth. Arch Gynecol Obstet 2012; 286 (2): 295–298.
Harper LM, Odibo AO, Macones GA, Crane JP, Cahill AG . Effect of placenta previa on fetal growth. Am J Obstet Gynecol 2010; 203 (4): 330 e1–330 e5.
Wolf EJ, Mallozzi A, Rodis JF, Egan JF, Vintzileos AM, Campbell WA . Placenta previa is not an independent risk factor for a small for gestational age infant. Obstet Gynecol 1991; 77 (5): 707–709.
Crane JM, van den Hof MC, Dodds L, Armson BA, Liston R . Neonatal outcomes with placenta previa. Obstet Gynecol 1999; 93 (4): 541–544.
Redline RW . Placental pathology: a systematic approach with clinical correlations. Placenta 2008; 29 (Suppl A): S86–S91.
Redline RW, Heller D, Keating S, Kingdom J . Placental diagnostic criteria and clinical correlation—a workshop report. Placenta 2005; 26 (Suppl A): S114–S117.
Reddy UM, Abuhamad AZ, Levine D, Saade GR, Fetal Imaging Workshop Invited Participants. Fetal imaging: executive summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, American College of Radiology, Society for Pediatric Radiology, and Society of Radiologists in Ultrasound Fetal Imaging Workshop. J Ultrasound Med 2014; 33 (5): 745–757.
American College of Obstetricians and Gynecologists Women's Health Care Physicians. ACOG Practice Bulletin No. 138: inherited thrombophilias in pregnancy. Obstet Gynecol 2013; 122 (3): 706–717.
American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 118: antiphospholipid syndrome. Obstet Gynecol 2011; 117 (1): 192–199.
Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon ES . Birth weight standards in the live-born population in Israel. Isr Med Assoc J 2005; 7 (5): 311–314.
Weiner E, Bar J, Fainstein N, Schreiber L, Ben-Haroush A, Kovo M . Intraoperative findings, placental assessment and neonatal outcome in emergent cesarean deliveries for non-reassuring fetal heart rate. Eur J Obstet Gynecol Reprod Biol 2015; 185: 103–107.
Pinar H, Sung CJ, Oyer CE, Singer DB . Reference values for singleton and twin placental weights. Pediatr Pathol Lab Med 1996; 16 (6): 901–907.
Strong TH Jr., Jarles DL, Vega JS, Feldman DB . The umbilical coiling index. Am J Obstet Gynecol 1994; 170 (1 Pt 1): 29–32.
Redline RW . The clinical implications of placental diagnoses. Semin Perinatol 2015; 39 (1): 2–8.
Redline RW . Classification of placental lesions. Am J Obstet Gynecol 2015; 213 (4 Suppl): S21–S28.
Papinniemi M, Keski-Nisula L, Heinonen S . Placental ratio and risk of velamentous umbilical cord insertion are increased in women with placenta previa. Am J Perinatol 2007; 24 (6): 353–357.
Chan JS, Baergen RN . Gross umbilical cord complications are associated with placental lesions of circulatory stasis and fetal hypoxia. Pediatr Dev Pathol 2012; 15 (6): 487–494.
Heidari Z, Sakhavar N, Mahmoudzadeh-Sagheb H, Ezazi-Bojnourdi T . Stereological analysis of human placenta in cases of placenta previa in comparison with normally implanted controls. J Reprod Infertil 2015; 16 (2): 90–95.
Biswas R, Sawhney H, Dass R, Saran RK, Vasishta K . Histopathological study of placental bed biopsy in placenta previa. Acta Obstet Gynecol Scand 1999; 78 (3): 173–179.
Salafia CM, Vintzileos AM, Silberman L, Bantham KF, Vogel CA . Placental pathology of idiopathic intrauterine growth retardation at term. Am J Perinatol 1992; 9 (3): 179–184.
Kovo M, Schreiber L, Ben-Haroush A, Cohen G, Weiner E, Golan A et al. The placental factor in early- and late-onset normotensive fetal growth restriction. Placenta 2013; 34 (4): 320–324.
Sander CH, Kinnane L, Stevens NG . Hemorrhagic endovasculitis of the placenta: a clinicopathologic entity associated with adverse pregnancy outcome. Compr Ther 1985; 11 (5): 66–74.
Redline RW . Severe fetal placental vascular lesions in term infants with neurologic impairment. Am J Obstet Gynecol. 2005; 192 (2): 452–457.
McIntire DD, Leveno KJ . Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol 2008; 111 (1): 35–41.
Yoder BA, Gordon MC, Barth WH Jr . Late-preterm birth: does the changing obstetric paradigm alter the epidemiology of respiratory complications? Obstet Gynecol 2008; 111 (4): 814–822.
Consortium on Safe Labor, Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S et al. Respiratory morbidity in late preterm births. JAMA 2010; 304 (4): 419–425.
Romero R, Dey SK, Fisher SJ . Preterm labor: one syndrome, many causes. Science 2014; 345 (6198): 760–765.
Ghidini A, Salafia CM . Histologic placental lesions in women with recurrent preterm delivery. Acta Obstet Gynecol Scand 2005; 84 (6): 547–550.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Weiner, E., Miremberg, H., Grinstein, E. et al. The effect of placenta previa on fetal growth and pregnancy outcome, in correlation with placental pathology. J Perinatol 36, 1073–1078 (2016). https://doi.org/10.1038/jp.2016.140
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.140
This article is cited by
-
Risk Factors and Pregnancy Outcomes of Antepartum Hemorrhage in Women with Placenta Previa
Reproductive Sciences (2023)
-
Effect of previous placenta previa on outcome of next pregnancy: a 10-year retrospective cohort study
BMC Pregnancy and Childbirth (2020)
-
Cumulative Antenatal Risk and Kindergarten Readiness in Preterm-Born Preschoolers
Research on Child and Adolescent Psychopathology (2020)
-
Amniotic fluid transitioning from clear to meconium stained during labor—prevalence and association with adverse maternal and neonatal outcomes
Journal of Perinatology (2019)