Abstract
Attention-deficit/hyperactivity disorder (ADHD) is a common, highly heritable neurodevelopmental syndrome characterized by hyperactivity, inattention and increased impulsivity. To detect micro-deletions and micro-duplications that may have a role in the pathogenesis of ADHD, we carried out a genome-wide screen for copy number variations (CNVs) in a cohort of 99 children and adolescents with severe ADHD. Using high-resolution array comparative genomic hybridization (aCGH), a total of 17 potentially syndrome-associated CNVs were identified. The aberrations comprise 4 deletions and 13 duplications with approximate sizes ranging from 110 kb to 3 Mb. Two CNVs occurred de novo and nine were inherited from a parent with ADHD, whereas five are transmitted by an unaffected parent. Candidates include genes expressing acetylcholine-metabolizing butyrylcholinesterase (BCHE), contained in a de novo chromosome 3q26.1 deletion, and a brain-specific pleckstrin homology domain-containing protein (PLEKHB1), with an established function in primary sensory neurons, in two siblings carrying a 11q13.4 duplication inherited from their affected mother. Other genes potentially influencing ADHD-related psychopathology and involved in aberrations inherited from affected parents are the genes for the mitochondrial NADH dehydrogenase 1 α subcomplex assembly factor 2 (NDUFAF2), the brain-specific phosphodiesterase 4D isoform 6 (PDE4D6) and the neuronal glucose transporter 3 (SLC2A3). The gene encoding neuropeptide Y (NPY) was included in a ∼3 Mb duplication on chromosome 7p15.2-15.3, and investigation of additional family members showed a nominally significant association of this 7p15 duplication with increased NPY plasma concentrations (empirical family-based association test, P=0.023). Lower activation of the left ventral striatum and left posterior insula during anticipation of large rewards or losses elicited by functional magnetic resonance imaging links gene dose-dependent increases in NPY to reward and emotion processing in duplication carriers. These findings implicate CNVs of behaviour-related genes in the pathogenesis of ADHD and are consistent with the notion that both frequent and rare variants influence the development of this common multifactorial syndrome.
Similar content being viewed by others
Introduction
Attention-deficit/hyperactivity disorder (ADHD; OMIM no. 143465) is defined as a clinically heterogeneous neurodevelopmental syndrome comprising the triad of inattention, hyperactivity and increased impulsivity. ADHD represents the most common psychiatric disorder in childhood and adolescence with similar prevalence rates throughout different cultural settings.1 Moreover, the syndromal dimensions of hyperactivity and increased impulsivity are increasingly being recognized as highly persistent into adulthood and are associated with considerable risk for psychiatric comorbidity such as depression and substance use disorder as well as failure in psychosocial adaptation.2
Although the substantial heritability of ADHD is documented in numerous family, twin and adoption studies, with estimates up to 80%, genome-wide linkage scans and candidate gene studies have failed to reliably identify ADHD-associated genes.3 Hebebrand and co-workers4 reported evidence for a risk haplotype at the dopamine transporter (DAT/SLC6A3) locus based on a linkage scan and subsequent fine-mapping of chromosome 5p13. A linkage analysis of eight extended families with high density of ADHD using a ∼50 K single-nucleotide polymorphism (SNP) array-based genotyping assay by our group validated previously reported findings and also revealed several novel susceptibility loci.5 One of these, the chromosome 16q locus, contributes to the genome-wide significant finding revealed by a meta-analysis comprising data from seven ADHD linkage scans.6 However, the identified linkage regions for ADHD are generally large and not easily delimitable, even when the data are combined.
Insight from pharmacological approaches and animal models consistently implicate altered neurotransmission in the neurobiology underlying ADHD. Effectiveness of ADHD treatment with stimulants (for example, methylphenidate) and norepinephrine reuptake inhibitors (for example, atomoxetine), influencing dopaminergic and noradrenergic systems, and the capacity of antidepressants to moderate ADHD symptoms directed the focus to catecholaminergic and serotonergic signalling. The hypothesis that monoaminergic dysfunction has a role in ADHD is further supported by genetic association studies. Polymorphisms in the dopamine receptor genes DRD4 and DRD5 (for review see Thapar et al.7) were found to be associated with ADHD. Although the findings are inconsistent, DAT/SLC6A3 is one of the most studied candidates for ADHD. Therefore, meta-analyses and well-designed subsequent confirmation studies with elaborate recruitment strategies for the establishment of large cohorts are essential for increasing power to validate a potential ADHD risk gene.
Alternative genome-wide molecular genetic approaches, such as array-based association and copy number variation (CNV) analyses,8 have recently been used to identify genomic aberrations underlying several neuropsychiatric disorders, including mental retardation (for review see Stankiewicz and Beaudet9), autism,10, 11, 12 schizophrenia13, 14, 15, 16, 17, 18, 19 and ADHD.20 These CNV analyses have inherent drawbacks and novel technical, statistical and epidemiological methods are required to identify disease risk genes in a reliable way.21 Nevertheless, genes affected by CNVs are especially interesting candidate causative factors for syndromes such as ADHD, where the disorder is defined by a specific constellation of common but extreme personality traits.
Here, we present data from a CNV analysis in a cohort of patients with severe ADHD using array comparative genomic hybridization (aCGH), which reliably detects micro-duplications and micro-deletions spanning up to several megabases. Four deletions and 13 duplications were identified in this ADHD cohort. The (endo)phenotypic consequences including functional magnetic resonance imaging (fMRI)-elicited brain activation of a ∼3 Mb duplication located on chromosome 7p15.2–15.3 and containing the neuropeptide Y (NPY) gene, which is known to influence both behavioural traits related to reward and emotion processing as well as energy homeostasis, were further investigated in an extended multigenerational pedigree with a high density of ADHD.
Materials and methods
Samples
A cohort of children and adolescents with ADHD (n=99; 78 male, 21 female) were included in the CNV scan. Sixty-seven patients were from nuclear families with at least 2 members affected with ADHD, 8 patients were from extended multigenerational families with high density of ADHD and 24 patients had sporadic ADHD. Patients and their families were recruited and phenotypically characterized by a team of experienced psychiatrists in the outpatient units of the Department of Child and Adolescent Psychiatry, Psychosomatics and Psychotherapy and the Department of Psychiatry, Psychosomatics and Psychotherapy, University of Wuerzburg, Germany, according to Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV-TR) criteria. As reference DNA for the aCGH experiments, we used a sex-matched pool of unscreened blood donors (n=100, 50 females) of European ancestry and originating from the same catchment area as the patients. All individuals agreed to participate in the study and written informed consent was obtained from either the participants themselves or the appropriate legal guardian. The study was approved by the ethics committee of the University of Wuerzburg.
Nuclear families, if they had one or more children affected with ADHD, were recruited for family-based segregation and association studies. The index patient was required to be older than 8 years and to fulfil DSM-IV criteria for the ADHD combined subtype, and other affected siblings in a family had to be older than 6 years. This lower limit was chosen to ensure relative persistence of ADHD symptoms and to exclude children who may show phenocopies of the disorder during preschool age but fail to meet the diagnostic criteria for ADHD during subsequent developmental stages.22, 23 Exclusion criteria were the following: (1) general IQ⩽80; (2) potentially confounding psychiatric diagnoses such as schizophrenia, any pervasive developmental disorder, Tourette's disorder, or primary affective or anxiety disorder; (3) neurological disorders such as epilepsy; (4) history of any acquired brain damage or evidence of fetal alcohol syndrome; (5) premature deliveries and/or (6) maternal reports of severe prenatal, perinatal or postnatal complications. Psychiatric classification was based on the Schedule for Affective Disorders and Schizophrenia for School-Age Children Present and Lifetime version (K-SADS-PL). Mothers completed (1) the unstructured Introductory Interview, (2) the Diagnostic Screening Interview and (3) the Supplement Completion Checklist, and upon fulfilment of screening criteria the appropriate Diagnostic Supplements. Children were interviewed with the screening interview of the K-SADS and in case of positive screening for affective or anxiety disorders, with the respective supplements of the K-SADS-PL. In addition, we used the Child Behaviour Checklist and a German Teachers’ Report on ADHD symptoms according to DSM-IV.
When parents reported individuals with presumable or definite ADHD symptomatology in the extended family, pedigrees were established to determine family size and structure. Reported ADHD symptoms in more than two generations resulted in intensified recruitment of additional family members. Bilineality was not an exclusion criterium for recruitment, because it was presumably present in most recruited families due to assortative mating, and intra-familiar heterogeneity cannot be completely ruled out in complex traits such as ADHD. All members of extended pedigrees were assessed by at least two clinicians experienced in the diagnosis of childhood and adult ADHD (CJ, TR, JR, MR). Due to a tendency towards severe obesity with evidence for co-segregation of this trait with ADHD in an extended family, additional data on body mass index (BMI) and endocrine functions were obtained for further analysis.
Array comparative genomic hybridization
aCGH24, 25 was performed as described previously.26 In brief, samples of sonicated patient and pooled male or female reference DNA were labelled by random priming (BioPrime Array CGH; Invitrogen, Carlsbad, CA, USA) with Cy3 and Cy5 (Amersham Biosciences, Piscataway, NJ, USA), respectively, and hybridized to a tiling path BAC array consisting of the human 32k BAC Re-Array Set (BACPAC Resources Center; http://bacpac.chori.org/pHumanMinSet.htm; DNA kindly provided by Pieter de Jong,27, 28 a 1 Mb resolution BAC set (clones kindly provided by Nigel Carter, Wellcome Trust Sanger Centre,29 and a set of sub-telomeric clones (assembled by members of the COSTB19 Action: molecular cytogenetics of solid tumours). Further information and protocols are available online (http://www.molgen.mpg.de/_abt_rop/molecular_cytogenetics/) and details concerning this platform have been submitted to the Gene Expression Omnibus (GEO; http://www.ncbi.nlm.nih.gov/geo/; GLP: 4645). For the analysis and visualization of aCGH data, our software package CGHPRO30 was used. No background subtraction was applied, and raw data were normalized by ‘Subgrid LOWESS’. For identifying potentially disease-related DNA copy number gains and losses, we initially called those genomic variants that were composed of three or more consecutive clones with log2 signal intensity ratios beyond 0.3 and −0.3, respectively. To increase sensitivity of the read-out, we then modified the selection criteria to enable the identification of CNVs in which as few as two consecutive clones scored above threshold. As this approach entails the risk of an increased false-positive rate, only selected CNVs with highest quality scores (defined by the coefficient of median average deviation and ratio shift) were added to the list obtained using the previous, more stringent selection criteria. CNVs were then prioritized and categorized by mirroring them against two CNV data sets derived from individuals not affected by clinically relevant ADHD. One data set was composed of CNVs from 700 healthy individuals and patients suffering from diseases other than ADHD. These samples have been analysed in our laboratory using the same BAC array platform and data interpretation parameters as those for the ADHD samples in this study.
The second data set, which had also been used to assess potential disease association in a recent SNP-based CNV study of ADHD patients,20 was obtained from the Database of Genomic Variants (DoGV). The DoGV is a public domain depository for CNVs identified in the healthy population (http://projects.tcag.ca/variation/, release August 2009).31 The dataset of Shaikh et al.32 includes all CNVs that were identified in a cohort of 2026 clinically well-characterized individuals free of serious medical disorder, including but not limited to neurodevelopmental disorders (including severe ADHD), cancer, chromosomal abnormalities and known metabolic or genetic disorders.32 On the basis of this comparison, we first identified those CNVs that were not present in either of these two reference data sets and refer to them as those above our high-stringency thresholds. Given the fact that, compared to SNP data, BAC array data are known to exaggerate the real size of a CNV, in our inter-platform comparison, we considered CNVs identical if the size differed no more than 100 kb at both ends or, for CNVs smaller than 300 kb, if they shared at least 50% of the genomic sequence. In a separate, less-stringent category we have summarized the CNVs that have been previously reported in the healthy population but are rare, or where independent evidence exists that genes within these intervals could be associated with ADHD. All CNVs discussed in this paper were either verified by confirmation of inheritance using the same method, or by CGH on 244K oligo arrays, performed according to the protocol provided by the manufacturer and analysed using the company's software CGH Analytics (Agilent, Santa Clara, CA, USA).
Plasma neuropeptide Y
NPY plasma concentrations were determined in 12 individuals from the extended multigenerational family. Plasma was immediately separated from venous blood samples by centrifugation, kept on dry ice during transport and stored at −80 °C until processing. For measurement of plasma NPY, we performed a commercial radioimmunoassay (IBL Hamburg, http://www.ibl-hamburg.com) according to the protocol provided by the manufacturer.
fMRI analysis of 7p15 duplication carriers
The impact of the 7p15 duplication and associated increase in NPY plasma concentrations on brain function was explored by fMRI. Imaging was performed during two paradigms: Both were modified versions of the monetary incentive delay task that has been shown to reliably elicit neural responses related to the anticipation of rewards and losses, respectively.33 Data were pre-processed and analysed using Statistical Parametric Mapping software (SPM5; Wellcome Department of Cognitive Neurology, UK) as described previously.34 To show potential alterations in reward- and loss-related neural responses, we compared four ADHD patients carrying the 7p15 duplication (F2-1, F2-4, F2-6, F2-8; Figure 2a and b) to an age-matched sample of healthy control subjects (n=21; mean=42.0, s.d.=6.7; all within 10 years of the median of the patient group) using a voxel-wise non-parametric procedure. P-values represent the probability of the median neural activation during the anticipation of rewards/losses of the patient group to be smaller than the median distribution obtained from all possible sets of four subjects (k=4) that can be drawn from the control sample (5985 combinations). Subsequent statistical analyses focused on the ventral striatum and the posterior insula as defined by voxel masks from a publication-based probabilistic MNI atlas at a probability threshold of 0.9.35 Correction for multiple comparisons was realized using AlphaSim (provided with AFNI software; http://afni.nimh.nih.gov/afni/) with a single voxel P-value of 0.05. With this procedure, we assured an overall corrected alpha threshold of P<0.05.
Statistics
The family-based association test (FBAT, http://biosun1.harvard.edu/~fbat/fbat.htm)36, 37 was used to investigate whether the 7p15.2-15.3 duplication is associated with ADHD, sex, BMI (kg m−2), binge eating (no/yes) and NPY plasma concentrations (pmol l−) within a multigenerational pedigree comprising 20 individuals. By means of 10 000 simulations, empirical two-sided P-values were obtained, which are more reliable than the respective asymptotic P-values in the case of small sample size. The offset parameter was set to null for residuals of BMI and NPY that were adjusted for sex and age, whereas for binge eating, an offset minimizing variance of the test statistic was chosen. The reported P-values are nominal, that is, not adjusted for multiple testing, at the significance level of 0.05.
Results
Array comparative genomic hybridization
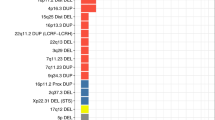
Using sub-megabase resolution aCGH, we screened a cohort of 99 children and adolescents diagnosed with ADHD for the presence of non-polymorphic CNVs. Approximately 75% of the patients were characterized by a family history of ADHD. Using stringent criteria for data analysis as outlined in the methods section, we identified a total of 11 duplications and 2 deletions. These aberrations are likely ADHD-associated, based on the fact that they are not documented in the reference data sets. One of these variations was confirmed to be de novo, whereas seven were inherited from an affected parent (Table 1a, Supplementary Figure S1). Except for one patient in whom inheritance could not be determined, the remaining variations falling into this category were inherited from an unaffected parent (Table 1b, Supplementary Figure S1). The tables include the CNV boundaries, and implicated genes are listed. For additional comparison, we indicate the number of times a similar CNV has been described in the DoGV. Finally, we detected an additional two duplications and two deletions that we consider potentially syndrome-associated despite the fact that they did not reach our high-stringency threshold scores because they were also observed at low frequency in one or both of the reference data sets (Table 2, Supplementary Figure S1). All aberrations were definite, as all have been verified either directly by oligo array or indirectly by analysis of parental DNA. None were observed at high frequencies in other patient cohorts in our hands, suggesting that they are potential risk factors for ADHD. One of these CNVs was de novo, two were inherited from affected parents, and one was inherited from a healthy parent.
Among apparent candidates is the gene encoding neuropeptide Y (NPY) contained in a duplication on chromosome 7p15.2-15.3 (described in detail in the next section). Further candidates included genes expressing acetylcholine-metabolizing butyrylcholinesterase (BCHE) involved in a de novo chromosome 3q26.1 deletion in an individual severely affected with ADHD and a brain-specific pleckstrin homology domain-containing protein (PLEKHB1), with an established function in primary sensory neurons, in two siblings with severe ADHD carrying a 11q13.4 duplication inherited from their affected mother. Other potentially disorder-causing genes involved in confirmed aberrations and inherited from affected parents include the genes for the mitochondrial NADH dehydrogenase 1 α subcomplex, assembly factor 2 (NDUFAF2), the brain-specific phosphodiesterase 4D isoform 6 (PDE4D6) (Figure 1) and the neuronal glucose transporter 3 (SLC2A3).
Duplication of 5q11.2 in patient 201. (a) Schematic view of chromosome 5, with mapped genomic clones depicted to the right. For each BAC clone, Cy3/Cy5 signal intensity ratios are plotted alongside the chromosome. Red and green lines correspond to log2 ratios −0.3 (loss) and 0.3 (gain), respectively. The region encompassing the aberration is highlighted by a red rectangle. (b) Closer view of the relevant region. (c) Ratio plot of the corresponding verification experiment using a 244K oligonucleotide array. (d) UCSC screenshot depicting genomic region chr5:57,791,039-58,811,926 (HG17). The red bar indicates the location of the duplication identified in patient 201. Grey bars in the custom track below represent copy number variations (CNVs) detected in 2026 control individuals by Shaikh et al.32 The specific identifying number is given on the left. Genes and their positions are indicated below these. Finally, all variations observed in the Database of Genomic Variants (DoGV) are included at the bottom of each panel for reference. These variations are colour-coded according to DoGV convention to reflect gain (red), loss (blue) or gain/loss (green). Noteworthy, the CNV identified in patient 201 includes the complete brain-specific PDE4D6 isoform described by Wang et al.,59 whereas all other CNVs are located within intronic regions.
Phenotype associated with the 7p15 duplication in a multigenerational pedigree
On the basis of the findings in the initial patient cohort resulting in the identification of a ∼3 Mb duplication located on chromosome 7p15.2-15.3, we ascertained the extended multigenerational pedigree (displaying a high density of ADHD) of the index patient to further investigate the phenotypic consequences of an additional copy of the NPY gene. Using aCGH, the 7p15.2-15.3 duplication was detected in several additional family members across three generations (Figure 2a). It is inherited from individual F1-2 of the first generation and 8 out of 12 affected family members of the F2 and F3 generations are also carriers. All individuals with the duplication are affected by ADHD, whereas in four affected descendants of the F1 generation no chromosomal rearrangement was detected at 7p15 suggesting a bilineal transmission of the syndrome in this family, as non-carrier F1/1 also suffers from ADHD. Assuming that the 7p15 duplication may influence the development of ADHD and further phenotypes such as BMI, binge eating behaviour and NPY plasma concentration, we additionally conducted FBATs for these phenotypes.
(a) Segregation of the chromosome 7p15.2-15.3 duplication (D) in a multigenerational family with diagnosed attention-deficit/hyperactivity disorder (ADHD). Affected members are symbolized by solid black symbols when the duplication is present and by solid grey when absent; unaffected members are identified by open symbols. Unknown clinical status is indicated by a circle. DNA of individuals F2-2, F2-3a and F2-5 was not available for analyses. (b) Neuropeptide Y (NPY) plasma concentrations blotted against the body mass index (BMI) in 7p15.2-15.3 duplication carriers with ADHD, non-carriers with ADHD and healthy family members. F numbers allow allocation to the pedigree.
Table 3a displays the clinical phenotype in carriers and non-carriers with respect to ADHD, food intake and obesity-related parameters as well as NPY plasma concentrations. Table 3b describes these phenotypes in relation to the transmission pattern of the 7p15 duplication. NPY plasma concentrations were significantly higher in offsprings having inherited the 7p15 duplication than in non-carriers (empirical FBAT, P=0.023; median NPY level 78.5 versus 46.6 pmol l−; Table 3b, Figure 2b). There was a trend towards a preferable transmission of the 7p15 duplication to affected family members (empirical FBAT, P=0.138, eight transmissions versus three non-transmissions) and binge eating (empirical FBAT, P=0.117, six transmissions versus one non-transmissions). However, these results did not reach an overall significance level if corrected by Bonferroni's approach. Finally, the empirical FBAT for BMI indicated no association with this trait (P=0.192).
The effect of the 7p15 duplication and gene dose-dependent increase in NPY plasma concentrations on brain function was explored by fMRI in four carriers with ADHD compared to healthy controls. Region of interest analyses revealed a significantly lower activation of the left ventral striatum during the anticipation of large rewards for duplication carriers than for controls (P<0.05, corrected; Figure 3, upper panels). A significantly lower activation of the left posterior insula during the anticipation of large losses was also observed in carriers compared to controls (P<0.05, corrected; Figure 3, lower panels). In none of the two regions, a significant difference between carriers and controls was observed for no or small rewards or losses. Furthermore, activation for the carriers never exceeded the controls’ responses in those two structures.
Neural activation in the ventral striatum during the anticipation of large rewards (upper panel) and in the posterior insula during the anticipation of large losses (lower panel) for 7p15.2-15.3 duplication carriers with attention-deficit/hyperactivity disorder (ADHD) (n=4) and healthy controls (n=21). Brain maps show significant –log10-transformed P-values (P<0.05 corrected) in the left ventral striatum (upper right panel) and in the left posterior insula (lower right panel). Box plots show medians, 25th and 75th percentiles and most extreme signal changes (whiskers extend to the most extreme subject values) corresponding to the brain maps of the ventral striatum (upper left panel) and the posterior insula (lower left panel).
Discussion
Sub-megabase resolution aCGH identified a total of 17 potentially disease-associated CNVs in a cohort of 99 children severely affected with ADHD. The aberrations comprise 4 deletions and 13 duplications with approximate sizes ranging from 130 kb to 3 Mb. Two CNVs occurred de novo and nine were inherited from a parent with ADHD, whereas five were transmitted by an unaffected parent. For one case, inheritance was not determined. These CNVs showed no overlap between individual patients, that is, they are not recurrent, but several of the genes involved may be integrated into behaviourally relevant functional pathways, including neurodevelopment, neurotransmission and synaptic plasticity.
The de novo CNVs are deletions on chromosomes 3q26 and 6q16.1. The 3q26 deletion, which overlaps with a recently described potentially disease-associated CNV,20 comprises an interval of 2 Mb and involves at least five genes, BCHE (butyrylcholinesterase, OMIM no. 177400), ZBBX (B-box domain containing zinc-finger protein), WDR49, SERPINI2 (serpin peptidase inhibitor) and PDCD10 (programmed cell death protein 10, disrupted by deletion of 4 exons at the 3′ end). Among these, BCHE is particularly of interest. BCHE is a glycoprotein enzyme within the family of serine esterases, expressed in the brain and periphery and involved in the metabolism of endogenous choline esters, such as acetylcholine. In brain, BCHE is strongly expressed in cholinergic neurons of the pedunculopontine tegmentum that, in interaction with dopaminergic, noradrenergic and serotonergic networks, regulate sleep–wake behaviour and vigilance,38 suggesting that this gene may also directly influence locomotor activity, attention and reward-related behaviour. BCHE also inactivates exogenous neurotoxic compounds.39 For example, BCHE administration inhibits cocaine-induced behavioural changes in mice, by converting cocaine into non-toxic metabolites.40 Variation in BCHE concentration has been recently associated with specific differences in cognitive function.41 Haplotype insufficiency with reduced BCHE activity in the patient carrying the deletion, in conjunction with an as yet unknown environmental factor during brain development, may moderate the risk for the development of ADHD symptoms including cognitive dysfunction. The other genes within the 3q26 deletion are not obvious candidate genes for behavioural disorders, or they display moderate (WDR49) to low (PDCD10) or no (ZBBX, SERPINI2) brain expression, but given the overlap with the CNV reported by Elia et al.20 a contribution to the phenotype cannot be excluded.
Given the remarkable heritability of ADHD, CNVs inherited from an affected parent are also likely to contain genes influencing disease risk. We identified a ∼3 Mb duplication containing the gene encoding NPY on chromosome 7p15.2-15.3 in a patient with a unique syndrome comprising severe ADHD and obesity. Subsequent investigation of the extended multigenerational pedigree with high density of ADHD patients revealed nominally significant evidence for an association of this duplication with ADHD, increased BMI and binge eating, suggesting that the duplication contributes to the syndrome in this family. However, in four descendants of the F1 generation affected with ADHD, no chromosomal rearrangement was detected. Due to assortative mating, which is common in ADHD, bilineal transmission of at least two causative gene variants (one of which is the NPY-containing duplication) passed by two affected F1 founders can be assumed.
NPY is a highly conserved 36-amino-acid peptide that is abundant throughout the peripheral and central nervous system. This neuropeptide has numerous physiological effects in the cardiovascular, gastrointestinal and pituitary-adrenocortical systems. Moreover, NPY participates in the regulation of feeding, circadian rhythms, reproduction and thermoregulation.42, 43 Although it has been widely investigated in the context of energy balance and body weight regulation, NPY has recently not only been implicated in behavioural traits, particularly negative emotionality and aggression,44 but also in several neuropsychiatric disorders including depression, panic disorder, bipolar disorder and schizophrenia.45 A functional polymorphism in the human NPY (Leu7Pro) resulting in increased NPY release from sympathetic nerves is associated with characteristics of metabolic syndrome and it has been suggested that the Pro7 allele is associated with an increased risk for alcohol dependence, a common comorbid disorder of ADHD.46
In the rodent model, central administration or overexpression of NPY produces a profound increase in food intake, whereas a reduction of NPY results in a decrease (for review see Karl and Herzog45). Food deprivation upregulates NPY in the arcuate nucleus of the hypothalamus, and repeated administration of NPY induces obesity. Transgenic mice overexpressing NPY in noradrenergic neurons were reported to display disturbances in glucose and lipid metabolism, key components of the cluster of abnormalities comprising the metabolic syndrome.47 NPY-deficient mice show reduced food intake in response to fasting and an anxiety-like phenotype with increased startle response.48 Several receptors mediate the physiological effects of NPY, and data suggest that the energy balance effects of NPY are mediated by both the NPY Y1 and Y5 receptors. NPY Y4 knockout mice display increased locomotor activity, less anxiety-like behaviour and behavioural despair, whereas behavioural characterization of NPY Y2 knockout mice revealed reduced attention and increased impulsivity.49, 50 Because we observed increased plasma NPY concentrations in the presence of an additional copy of NPY within the investigated extended family as a peripheral biomarker, receptor subtype-dependent signalling in the brain, with consequences on the regulation of metabolic homeostasis, as well as cognition, reward-related behaviour and emotion regulation are likely to be altered in duplication carriers.
In support of an impact of gene dosage-dependent increases in NPY expression on brain function, fMRI of reward and emotion processing detected lower activation of the left ventral striatum and left posterior insula during anticipation of large rewards/losses in duplication carriers, respectively. As left ventral striatal hyporesponsiveness during reward anticipation has been repeatedly shown in patients with adult ADHD,51, 52 NPY overexpression may result in deviant reward-related neural processing in duplication carriers. Moreover, the relative hypoactivity within the left posterior insula during the anticipation of monetary loss in carriers could reflect anxiolytic effects of NPY.48, 49, 50 Higher genotype-driven NPY expression has been recently shown to be associated with reduced pain/stress-induced activations of endogenous opioid neurotransmission and accounted for 37% variance in left posterior insular cortex activation.44 Hence, our fMRI findings replicate previously reported NPY-related alterations in the processing of aversive stimuli while extending evidence for an interaction of NPY with reward circuits. Taken together, our findings provide evidence that increased NPY dosage is not only reflected by the peripheral biomarker of increased NPY plasma concentration but also by fMRI-elicited alteration in brain function related to reward and emotion processing.
Although increased plasma NPY concentrations were previously observed in children with ADHD,53 the general role of this neuropeptide in the pathophysiology of ADHD remains to be determined. The potential link between ADHD, metabolic dysregulation and NPY is underscored by studies revealing that ADHD is highly prevalent among obese patients and highest in those with extreme obesity. Mechanisms for the comorbidity are unknown, but they may involve brain dopamine function, glucose utilization and insulin receptor activity.54 Alterations in the brain dopamine system affect a spectrum of behavioural phenotypes ranging from ADHD-associated behaviour to food intake, and from an evolutionary perspective, gene variations selected to increase cognitive and behavioural flexibility may presently be associated with attention deficits and increased food consumption in an obesogenic environment. Taken together, there is substantial evidence supporting a role for NPY in the ADHD-related behavioural phenotype and dysregulation of energy balance in carriers of the 7p15.2-15.3 duplication. Although increased NPY concentrations in brain are likely to have a causative role in the ADHD and obesity-related phenotype of NPY duplication carriers, it should be noted that the duplication is large and also harbours other brain-expressed genes that may influence behaviour.
The 5q12.1 deletion in patient 241 (inherited from his affected mother) affects four genes, of which the partially deleted NDUFAF2 is a plausible candidate. NDUFAF2 is a Myc-induced mitochondrial NADH dehydrogenase and complex I assembly factor. Complex I catalyses the first step in the mitochondrial respiratory chain, and a homozygous mutation in this gene was found in a child with severe progressive leukoencephalopathy.55 Disruption and functional loss or a dominant interfering effect of a mutant copy of NDUFAF2 may cause neurometabolic deficiency resulting in an allelic disorder with an ADHD phenotype. Patient 51 carries a ∼500 kb duplication located at 11q13.4 and inherited from the affected mother. The deletion, which was also detected in an affected brother, harbours the gene for the brain-expressed PLEKHB1, which exerts cellular functions in primary sensory neurons.56 Another candidate from the deleted interval, RAB6A is involved in the regulation of synaptic vesicle function, and the mitochondrial uncoupling protein UCP2, also implicated, has a neuroprotective effect in both the developing and adult brain.57, 58 Whether these two genes contribute to the general genetic risk towards ADHD in the population remains to be established.
Several aberrations inherited from healthy parents, as well as those that were observed at low frequencies in the reference data sets may also represent candidate risk factors for ADHD. Of particular relevance, the calcium/calmodulin-dependent protein kinase IID gene (CAMK2D) is disrupted by the duplication in patient 461. CAMK2D belongs to the family of calcium- and calmodulin-dependent protein kinases. Several isoforms have been described, one of which is expressed exclusively in rodent and human cerebral cortex.
The gene encoding the supershort brain-specific isoform 6 of the phoshodiesterase 4D (PDE4D6)59 including its presumed transcriptional control region is exclusively duplicated in patient 201. The duplication of PDE4D6 is inherited from the affected mother and located on chromsome 5q11.2, a region adjacent to the 5q13.1 locus of genome-wide significance in a high-resolution linkage study to ADHD (∼2.5 Mb 5′ of rs895381, family P1).5 It is noteworthy that the 5q12.1 deletion in patient 241 (also see preceding section) is only ∼250 kb upstream of a linkage interval flanked by markers D5S1968-D5S629 in an extended pedigree (Lin et al., unpublished results) and nominally significant association of several SNPs (highest ranking SNP rs17780175, P=3.41 × 10−9) in PDE4D, was also revealed by a pooling-based genome-wide association (GWA) study in adult ADHD.60 Of related interest, PDE4D variants that distinguish dependent versus non-dependent individuals abusing methamphetamine, alcohol, nicotine and other substances have been previously identified in several GWA studies of addiction vulnerability.61 Given the high comorbididty of ADHD with substance use disorders, the convergence with genes identified in GWA studies of addiction vulnerability and related phenotypes provides further confidence in our data. Although previous association to ADHD has not been reported for these genes, those identified both by this study and by findings from other related reports appear especially relevant for further detailed evaluation.
At 5q13.3 SV2C encoding the synaptic vesicle protein 2C is partially duplicated in patient 21 with preservation of the 3′ segment and, finally, another common copy number polymorphism in patient 211 results in a duplication of the gene for the SLC2A3 at 12p13.3. Both gene products are associated with synaptic vesicles and participate in the regulation of neurotransmitter release. Interestingly, reduced SLC2A3 expression resulting from a trans-regulation effect of a locus on 4q32.1 was recently implicated in dyslexia.62 Given the remarkable comorbidity of dyslexia and ADHD, and the anecdotal reports of sugar intolerance in ADHD associated with an exacerbation of the symptomatology, systematic investigation of the role of common CNVs in the SLC2A3 region in neuronal glucose utilization is warranted.
Although our findings implicate rare variants in the pathogenesis of ADHD, GWA studies are by and large considered to support the common disease/common variants hypothesis whose validity for psychiatric disorders is currently controversial.60, 63, 64 Although several genes affected by CNVs identified in this study contain SNPs that yield significant signals in GWA studies, there is presently no obvious relationship between the heritability of ADHD and the number or strength of the observed effects. Unlike rare CNVs, common variants for ADHD may be of very small effect and thus require very large samples to be reliably detected. This argues for the requirement of meta-analysis of various whole-genome (including classical and high-resolution) linkage, GWA and CNV scans, as well as larger sample collections. In conclusion, our findings from this aCGH CNV screen in ADHD are consistent with the notion that multiple rare and frequent CNVs involving genes functioning in shared dosage-sensitive neurobiological pathways contribute to ADHD-related pathology.
References
Lesch KP . Attention-deficit/hyperactivity disorder (ADHD). In: Lang F (ed). Encyclopedia of Molecular Mechanisms of Disease. Springer: Heidelberg, New York, 2009 pp 188–191.
Jacob CP, Romanos J, Dempfle A, Heine M, Windemuth-Kieselbach C, Kruse A et al. Co-morbidity of adult attention-deficit/hyperactivity disorder with focus on personality traits and related disorders in a tertiary referral center. Eur Arch Psychiatry Clin Neurosci 2007; 257: 309–317.
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA et al. Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry 2005; 57: 1313–1323.
Friedel S, Saar K, Sauer S, Dempfle A, Walitza S, Renner T et al. Association and linkage of allelic variants of the dopamine transporter gene in ADHD. Mol Psychiatry 2007; 12: 923–933.
Romanos M, Freitag C, Jacob C, Craig DW, Dempfle A, Nguyen TT et al. Genome-wide linkage analysis of ADHD using high-density SNP arrays: novel loci at 5q13.1 and 14q12. Mol Psychiatry 2008; 13: 522–530.
Zhou K, Dempfle A, Arcos-Burgos M, Bakker SC, Banaschewski T, Biederman J et al. Meta-analysis of genome-wide linkage scans of attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 2008; 147B: 1392–1398.
Thapar A, Langley K, Owen MJ, O’Donovan MC . Advances in genetic findings on attention deficit hyperactivity disorder. Psychol Med 2007; 37: 1681–1692.
Lee JA, Lupski JR . Genomic rearrangements and gene copy-number alterations as a cause of nervous system disorders. Neuron 2006; 52: 103–121.
Stankiewicz P, Beaudet AL . Use of array CGH in the evaluation of dysmorphology, malformations, developmental delay, and idiopathic mental retardation. Curr Opin Genet Dev 2007; 17: 182–192.
Szatmari P, Paterson AD, Zwaigenbaum L, Roberts W, Brian J, Liu XQ et al. Mapping autism risk loci using genetic linkage and chromosomal rearrangements. Nat Genet 2007; 39: 319–328.
Sebat J, Lakshmi B, Malhotra D, Troge J, Lese-Martin C, Walsh T et al. Strong association of de novo copy number mutations with autism. Science 2007; 316: 445–449.
Marshall CR, Noor A, Vincent JB, Lionel AC, Feuk L, Skaug J et al. Structural variation of chromosomes in autism spectrum disorder. Am J Hum Genet 2008; 82: 477–488.
Xu B, Roos JL, Levy S, van Rensburg EJ, Gogos JA, Karayiorgou M . Strong association of de novo copy number mutations with sporadic schizophrenia. Nat Genet 2008; 40: 880–885.
Walsh T, McClellan JM, McCarthy SE, Addington AM, Pierce SB, Cooper GM et al. Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science 2008; 320: 539–543.
Friedman JI, Vrijenhoek T, Markx S, Janssen IM, van der Vliet WA, Faas BH et al. CNTNAP2 gene dosage variation is associated with schizophrenia and epilepsy. Mol Psychiatry 2008; 13: 261–266.
Kirov G, Gumus D, Chen W, Norton N, Georgieva L, Sari M et al. Comparative genome hybridization suggests a role for NRXN1 and APBA2 in schizophrenia. Hum Mol Genet 2008; 17: 458–465.
Wilson GM, Flibotte S, Chopra V, Melnyk BL, Honer WG, Holt RA . DNA copy-number analysis in bipolar disorder and schizophrenia reveals aberrations in genes involved in glutamate signaling. Hum Mol Genet 2006; 15: 743–749.
St Clair D . Copy number variation and schizophrenia. Schizophr Bull 2009; 35: 9–12.
Vrijenhoek T, Buizer-Voskamp JE, van der Stelt I, Strengman E, Sabatti C, Geurts van Kessel A et al. Recurrent CNVs disrupt three candidate genes in schizophrenia patients. Am J Hum Genet 2008; 83: 504–510.
Elia J, Gai X, Xie HM, Perin JC, Geiger E, Glessner JT et al. Rare structural variants found in attention-deficit hyperactivity disorder are preferentially associated with neurodevelopmental genes. Mol Psychiatry 2009, June 23 [e-pub ahead of print].
Ionita-Laza I, Rogers AJ, Lange C, Raby BA, Lee C . Genetic association analysis of copy-number variation (CNV) in human disease pathogenesis. Genomics 2009; 93: 22–26.
Barkley RA, Shelton TL, Crosswait C, Moorehouse M, Fletcher K, Barrett S et al. Preschool children with disruptive behavior: three-year outcome as a function of adaptive disability. Dev Psychopathol 2002; 14: 45–67.
Shelton TL, Barkley RA, Crosswait C, Moorehouse M, Fletcher K, Barrett S et al. Multimethod psychoeducational intervention for preschool children with disruptive behavior: two-year post-treatment follow-up. J Abnorm Child Psychol 2000; 28: 253–266.
Pinkel D, Segraves R, Sudar D, Clark S, Poole I, Kowbel D et al. High resolution analysis of DNA copy number variation using comparative genomic hybridization to microarrays. Nat Genet 1998; 20: 207–211.
Solinas-Toldo S, Lampel S, Stilgenbauer S, Nickolenko J, Benner A, Dohner H et al. Matrix-based comparative genomic hybridization: biochips to screen for genomic imbalances. Genes Chromosomes Cancer 1997; 20: 399–407.
Erdogan F, Chen W, Kirchhoff M, Kalscheuer VM, Hultschig C, Muller I et al. Impact of low copy repeats on the generation of balanced and unbalanced chromosomal aberrations in mental retardation. Cytogenet Genome Res 2006; 115: 247–253.
Ishkanian AS, Malloff CA, Watson SK, DeLeeuw RJ, Chi B, Coe BP et al. A tiling resolution DNA microarray with complete coverage of the human genome. Nat Genet 2004; 36: 299–303.
Krzywinski M, Bosdet I, Smailus D, Chiu R, Mathewson C, Wye N et al. A set of BAC clones spanning the human genome. Nucleic Acids Res 2004; 32: 3651–3660.
Fiegler H, Carr P, Douglas EJ, Burford DC, Hunt S, Scott CE et al. DNA microarrays for comparative genomic hybridization based on DOP-PCR amplification of BAC and PAC clones. Genes Chromosomes Cancer 2003; 36: 361–374.
Chen W, Erdogan F, Ropers HH, Lenzner S, Ullmann R . CGHPRO—a comprehensive data analysis tool for array CGH. BMC Bioinformatics 2005; 6: 85.
Iafrate AJ, Feuk L, Rivera MN, Listewnik ML, Donahoe PK, Qi Y et al. Detection of large-scale variation in the human genome. Nat Genet 2004; 36: 949–951.
Shaikh TH, Gai X, Perin JC, Glessner JT, Xie H, Murphy K et al. High-resolution mapping and analysis of copy number variations in the human genome: a data resource for clinical and research applications. Genome Res 2009; 19: 1682–1690.
Knutson B, Adams CM, Fong GW, Hommer D . Anticipation of increasing monetary reward selectively recruits nucleus accumbens. J Neurosci 2001; 21: RC159.
Hahn T, Dresler T, Ehlis AC, Plichta MM, Heinzel S, Polak T et al. Neural response to reward anticipation is modulated by Gray’s impulsivity. Neuroimage 2009; 46: 1148–1153.
Fox PT, Lancaster JL . Opinion: mapping context and content: the BrainMap model. Nat Rev Neurosci 2002; 3: 319–321.
Laird NM, Horvath S, Xu X . Implementing a unified approach to family-based tests of association. Genet Epidemiol 2000; 19 (Suppl 1): S36–S42.
Rabinowitz D, Laird N . A unified approach to adjusting association tests for population admixture with arbitrary pedigree structure and arbitrary missing marker information. Hum Hered 2000; 50: 211–223.
Darvesh S, Hopkins DA, Geula C . Neurobiology of butyrylcholinesterase. Nat Rev Neurosci 2003; 4: 131–138.
Raveh L, Grunwald J, Marcus D, Papier Y, Cohen E, Ashani Y . Human butyrylcholinesterase as a general prophylactic antidote for nerve agent toxicity. In vitro and in vivo quantitative characterization. Biochem Pharmacol 1993; 45: 2465–2474.
Koetzner L, Woods JH . Characterization of butyrylcholinesterase antagonism of cocaine-induced hyperactivity. Drug Metab Dispos 2002; 30: 716–723.
Manoharan I, Kuznetsova A, Fisk JD, Boopathy R, Lockridge O, Darvesh S . Comparison of cognitive functions between people with silent and wild-type butyrylcholinesterase. J Neural Transm 2007; 114: 939–945.
Hokfelt T, Broberger C, Diez M, Xu ZQ, Shi T, Kopp J et al. Galanin and NPY, two peptides with multiple putative roles in the nervous system. Horm Metab Res 1999; 31: 330–334.
Herzog H . Neuropeptide Y and energy homeostasis: insights from Y receptor knockout models. Eur J Pharmacol 2003; 480: 21–29.
Zhou Z, Zhu G, Hariri AR, Enoch MA, Scott D, Sinha R et al. Genetic variation in human NPY expression affects stress response and emotion. Nature 2008; 452: 997–1001.
Karl T, Herzog H . Behavioral profiling of NPY in aggression and neuropsychiatric diseases. Peptides 2007; 28: 326–333.
Zhu G, Pollak L, Mottagui-Tabar S, Wahlestedt C, Taubman J, Virkkunen M et al. NPY Leu7Pro and alcohol dependence in Finnish and Swedish populations. Alcohol Clin Exp Res 2003; 27: 19–24.
Ruohonen ST, Pesonen U, Moritz N, Kaipio K, Roytta M, Koulu M et al. Transgenic mice overexpressing neuropeptide Y in noradrenergic neurons: a novel model of increased adiposity and impaired glucose tolerance. Diabetes 2008; 57: 1517–1525.
Bannon AW, Seda J, Carmouche M, Francis JM, Norman MH, Karbon B et al. Behavioral characterization of neuropeptide Y knockout mice. Brain Res 2000; 868: 79–87.
Painsipp E, Wultsch T, Edelsbrunner ME, Tasan RO, Singewald N, Herzog H et al. Reduced anxiety-like and depression-related behavior in neuropeptide Y Y4 receptor knockout mice. Genes Brain Behav 2008; 7: 532–542.
Greco B, Carli M . Reduced attention and increased impulsivity in mice lacking NPY Y2 receptors: relation to anxiolytic-like phenotype. Behav Brain Res 2006; 169: 325–334.
Scheres A, Milham MP, Knutson B, Castellanos FX . Ventral striatal hyporesponsiveness during reward anticipation in attention-deficit/hyperactivity disorder. Biol Psychiatry 2007; 61: 720–724.
Strohle A, Stoy M, Wrase J, Schwarzer S, Schlagenhauf F, Huss M et al. Reward anticipation and outcomes in adult males with attention-deficit/hyperactivity disorder. Neuroimage 2008; 39: 966–972.
Oades RD, Daniels R, Rascher W . Plasma neuropeptide-Y levels, monoamine metabolism, electrolyte excretion and drinking behavior in children with attention-deficit hyperactivity disorder. Psychiatry Res 1998; 80: 177–186.
Agranat-Meged AN, Deitcher C, Goldzweig G, Leibenson L, Stein M, Galili-Weisstub E . Childhood obesity and attention deficit/hyperactivity disorder: a newly described comorbidity in obese hospitalized children. Int J Eat Disord 2005; 37: 357–359.
Ogilvie I, Kennaway NG, Shoubridge EA . A molecular chaperone for mitochondrial complex I assembly is mutated in a progressive encephalopathy. J Clin Invest 2005; 115: 2784–2792.
Xu S, Wang Y, Zhao H, Zhang L, Xiong W, Yau KW et al. PHR1, a PH domain-containing protein expressed in primary sensory neurons. Mol Cell Biol 2004; 24: 9137–9151.
Sullivan PG, Dube C, Dorenbos K, Steward O, Baram TZ . Mitochondrial uncoupling protein-2 protects the immature brain from excitotoxic neuronal death. Ann Neurol 2003; 53: 711–717.
Mattiasson G, Shamloo M, Gido G, Mathi K, Tomasevic G, Yi S et al. Uncoupling protein-2 prevents neuronal death and diminishes brain dysfunction after stroke and brain trauma. Nat Med 2003; 9: 1062–1068.
Wang D, Deng C, Bugaj-Gaweda B, Kwan M, Gunwaldsen C, Leonard C et al. Cloning and characterization of novel PDE4D isoforms PDE4D6 and PDE4D7. Cell Signal 2003; 15: 883–891.
Lesch KP, Timmesfeld N, Renner TJ, Halperin R, Roser C, Nguyen TT et al. Molecular genetics of adult ADHD: converging evidence from genome-wide association and extended pedigree linkage studies. J Neural Transm 2008; 115: 1573–1585.
Uhl GR, Drgon T, Johnson C, Fatusin OO, Liu QR, Contoreggi C et al. ‘Higher order’ addiction molecular genetics: convergent data from genome-wide association in humans and mice. Biochem Pharmacol 2008; 75: 98–111.
Roeske D, Ludwig KU, Neuhoff N, Becker J, Bartling J, Bruder J et al. First genome-wide association scan on neurophysiological endophenotypes points to trans-regulation effects on SLC2A3 in dyslexic children. Mol Psychiatry 2009, September 29 [e-pub ahead of print].
Mitchell KJ, Porteous DJ . GWAS for psychiatric disease: is the framework built on a solid foundation? Mol Psychiatry 2009; 14: 740–741.
Franke B, Neale BM, Faraone SV . Genome-wide association studies in ADHD. Hum Genet 2009; 126: 13–50.
Acknowledgements
We thank the patients and their families for their participation and support. We greatly appreciate the input from co-workers, who contributed to organization of the study, data management and technical assistance: Annette Nowak, Gabriele Ortega, Nicole Steigerwald, Nicole Döring and Theresia Töpner. This study was supported by the Deutsche Forschungsgemeinschaft (KFO 125, SFB 581, SFB TRR 58, GRK 1156, GRK 1253) and the Bundesministerium für Bildung und Forschung (BMBF 01GV0605).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions: The study was conceptualized and supervised by KPL, AW, HHR and RU. MR, JR and CJ ascertained and clinically characterized the patients. SW, TR, MH, AB-H and CJ contributed to clinical characterization of family members. SS, SS and RU carried out the genetic analysis. KPL, SS, RU and TR evaluated the genomic data. MF and BA determined NPY plasma concentrations. TH, SH and AF conducted and analysed the fMRI. TW and AR contributed expertise on genetic analyses and NPY animal models. TN, AD, HZ, and HS performed statistical analyses. KPL, TR, SS, AR and RU wrote and revised the paper.
Supplementary Information accompanies the paper on the Molecular Psychiatry website (http://www.nature.com/mp)
Supplementary information
Rights and permissions
About this article
Cite this article
Lesch, KP., Selch, S., Renner, T. et al. Genome-wide copy number variation analysis in attention-deficit/hyperactivity disorder: association with neuropeptide Y gene dosage in an extended pedigree. Mol Psychiatry 16, 491–503 (2011). https://doi.org/10.1038/mp.2010.29
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2010.29
Keywords
This article is cited by
-
Systematic review of mitochondrial genetic variation in attention-deficit/hyperactivity disorder
European Child & Adolescent Psychiatry (2022)
-
Genetic variations influence brain changes in patients with attention-deficit hyperactivity disorder
Translational Psychiatry (2021)
-
Copy Number Variants and Polygenic Risk Scores Predict Need of Care in Autism and/or ADHD Families
Journal of Autism and Developmental Disorders (2021)
-
Serotonin-specific neurons differentiated from human iPSCs form distinct subtypes with synaptic protein assembly
Journal of Neural Transmission (2021)
-
Genetics of ADHD: What Should the Clinician Know?
Current Psychiatry Reports (2020)