Abstract
Cytotoxic T lymphocytes and natural killer cells kill their targets by secreting specialized granules that contain potent cytotoxic molecules. Through the study of rare immunodeficiency diseases in which this granule pathway of killing is impaired, proteins such as Rab27a have been identified as components of the secretory machinery of these killer cells. Recent evidence suggests that the destruction of activated lymphocytes through granule-mediated killing may be an important mechanism of immunological homeostasis. Although the process by which this occurs is not yet known, it is possible that events taking place at the immunological synapse may render the killer cell susceptible to fratricidal attack by other killer cells.
Similar content being viewed by others
Main
Cytotoxic T lymphocytes (CTLs) and natural killer (NK) cells are highly effective killers of virally infected and tumorigenic cells. Although the receptors involved in recognition of targets by these cells differ, the mechanisms by which they kill are essentially the same. The lytic activity of CTLs and NK cells is localized in specialized granules in their cytoplasm and, through the regulated secretion of these granules, killer cells can selectively induce target cell death.
Killer components of granules
In the 1980s, several groups identified the active proteins present in CTL and NK cell granules1,2. The key soluble protein was called perforin (or cytolysin by Henkart and colleagues1). This protein was recognized by antibodies to the pore-forming C9 component of complement, and amino acid sequencing identified a strong region of homology between perforin and C9 (refs. 3,4). This homology was also reflected functionally, as perforin was found to form pores of 15–16 nm in the membranes of red blood cells similar to those formed by C9 (ref. 5). This led to the proposal that perforin secretion from the lytic granules caused cell death by disrupting the plasma membrane through pore formation6.
Plasma membrane disruption, however, is not the only feature of cell death inflicted by CTLs and NK cells. Unlike complement-mediated lysis, killer cell lysis was found to be accompanied by extensive cellular deterioration beyond damage to the plasma membrane, in particular nuclear disintegration, which suggested that additional factors in the lytic granules were contributing to cytolysis. Other components of the lytic granules were subsequently identified as serine proteases, called granzymes7. These proteases triggers rapid apoptosis in the target cells8,9.
Granzyme function is totally dependent on the activity of perforin, as shown by a series of clever experiments in which perforin either alone or with granzyme A and/or granzyme B was expressed after transfection in the mast cell line RBL. These cells do not express endogenous perforin or granzymes but normally secrete histamine from their own secretory granules in response to degranulation mediated by immunoglobulin-ε (IgE). By crosslinking IgE to target cells, degranulation of the RBL transfectants was triggered and target cell lysis could be detected by the release of either 51Cr (a measure of membrane permeability) or 125I-labeled UdR (a measure of nuclear breakdown). The results of these experiments showed that both perforin and granzymes were required for the release of 51Cr and 125I-labeled UdR. Perforin alone resulted in only 51Cr release, whereas granzymes alone did not kill the target cells10,11,12. These data suggested that the granzymes entered the target cell through a perforin membrane pore.
It was later shown that granzyme B triggers apoptosis by caspase cleavage, leading to rapid death of the target cell13. Granzyme A initiates a caspase-independent cell death pathway, causing nicks in single-stranded DNA and preventing cellular repair, thereby forcing the cell into apoptosis14,15. The idea that perforin-mediated pores are necessary to facilitate granzyme uptake has been challenged by the demonstration of perforin-independent granzyme uptake into target cells16 and the subsequent finding that granzymes A and B can be internalized by endocytosis after binding the mannose-6-phosphate receptor (MPR)17.
Notably, cell death can be triggered in target cells preloaded with granzymes by endocytosis when the endosome is disrupted by adenovirus or pore-forming toxins that disrupt the endosomal membrane16,17,18,19. Curiously, target cell death can also be seen when 'sublytic' amounts of perforin (defined as those resulting in release of <10% of 51Cr) are added to targets preloaded with endocytosed granzymes, leading to the suggestion that perforin may act in the endosomes. Alternatively, because the MPR not only undergoes internalization from the plasma membrane but also recycles rapidly20, it is possible that granzyme B may return to the cell surface without dissociating from the MPR (because dissociation only occurs below pH 6; ref. 21) and enter through a perforin pore at this point.
There are a few reasons why perforin is unlikely to disrupt the endosomal membrane per se. First, the endosomes undergo rapid acidification after endocytosis, reaching a pH of about 4.5 in the lysosome. Because the activity of the perforin is acutely dependent on pH and drops very rapidly below pH 7, it is difficult to see how it could functionally disrupt an endosome membrane22. Second, perforin is stored in its active form in an endosomal compartment of CTLs and NK cells and does not disrupt the membrane of its storage compartment1,23. Last, many studies have shown that purified perforin loses its activity very rapidly, suggesting that the stable preparations of perforin, which can be used in these studies, may also contain other lytic granule proteins24. Any interpretation of these results will be aided by a precise knowledge of pH and calcium concentrations in the synaptic cleft, which influence how perforin works as it meets the target cell.
CTL and NK cell resistance to self lysis
Given the effectiveness of the lytic mechanisms stored by CTLs and NK cells, a key question has been how CTLs and NK cells avoid killing themselves while they are destroying their target. Both CTLs and NK cells can kill several target cells in succession without killing themselves25. But killer cells can themselves be targets. Experiments have shown that a anti–b CTLs can polarize their granules towards and kill b anti–c CTLs, which do not polarize their granules towards the a anti–b CTLs. The a anti–b CTLs kill the b anti–c CTLs but are not killed themselves26, suggesting that it is the area of contact between the killer and target (now referred to as the 'immunological synapse') that provides the killer protection during destruction of the target.
Recently, a membrane-bound form of cathepsin B has been implicated in protection from perforin-mediated pore formation at the synapse. Cathepsin B is normally found on the granule membranes of CTLs and NK cells but is translocated to the cell surface on degranulation, when the granule membranes fuse with the plasma membrane. Cathepsin B can cleave perforin, and it has been proposed that granule-derived cathepsin B present at the killer cell surface cleaves perforin and prevents pore formation, thereby protecting the killer cell from perforin-mediated damage during target cell destruction27. It is not clear whether this membrane-bound form of cathepsin B is present in all cells or what happens in its absence.
Other mechanisms can prevent cell death in CTLs. For example, cellular Fas-associated death domain–like interleukin-1β–converting enzyme-inhibitory protein (FLIP) prevents cell death through death receptors such as Fas ligand, although it is ineffective in protecting the killer lymphocytes against the perforin pathway28. A series of proteinase inhibitors, called serpins, are also expressed in CTLs and NK cells, and some of these can protect against killing mediated by granzyme B29.
Formation of the secretory synapse
The above outline of how CTLs and NK cells kill targets and protect themselves indicates that delivering the lytic granules is of central importance in both effecting and protecting from killing. The secretory machinery of killer cells must be able to direct lytic granule secretion with exquisite precision to the immunological synapse.
The secretory granules of CTLs and NK cells are unusual in that they are lysosomes and thus have both the degradative functions of the lysosome and the functions of a regulated secretory granule30,31. In the cell, these 'secretory lysosomes' can move along microtubules both in a plus direction away from the microtubule-organizing center (MTOC) and in a minus direction towards the MTOC. Recognition of a target by either CTLs or NK cells triggers rapid polarization of the MTOC towards the immunological synapse32,33,34.
The Golgi apparatus uses different microtubule motors to associate with the microtubules around the MTOC35 and also polarizes with the MTOC towards the immunological synapse. Initially granules polarize and seem to cluster behind the MTOC before moving around the Golgi and docking at the plasma membrane36 (Fig. 1). Secretion then occurs in the outer adhesion ring and adjacent to the area in which T cell receptor proteins are clustered. The synapse formed between killer and targets differs in at least one important way from the synapse characterized between CD4+ cells and antigen-presenting cells (APCs): both the CTL and NK interactions are rapid (minutes) and transient and lead to destruction of the targets, whereas CD4+ synapses are maintained for hours37.
(a) Polarization of secretory granules at the immunological synapse formed by CTLs and target cells. The granules are labeled with electron-dense horseradish peroxidase and are dark. They cluster in the region of the MTOC and move around the MTOC and Golgi apparatus to dock at the plasma membrane for secretion. (b) Confocal section of two CTLs, both polarized towards the same target cell. Granules are stained with antibodies to cathepsin (green), actin (blue) and the T cell receptor–associated protein Lck (red). (c) Section through the interface between the upper CTL in b and the target cell shown face on to reveal the secretory domain in the immunological synapse formed between CTLs and target cells.
Studies using labeled secretory granules of CTLs have shown that very few granules need to be released to destroy a target36,38, and that the MTOC can polarize rapidly from one target to another39. This suggests that these synapses are made and destroyed rapidly, making the whole process highly efficient.
Genetic defects in killing
Many human diseases and their mouse counterparts are caused by defects in the secretory pathway required for cytotoxicity40,41,42,43,44 (Table 1). Several of these diseases show an unusual combination of immunodeficiency and albinism, reflecting similarities in the cell biology of the secretory machinery used by cells of the immune system and that used by melanocytes, which secrete the melanin needed for pigmentation45,46. Many of these genetic defects impair melanocyte secretion but have no effect on CTL secretion, however, suggesting that some components of the secretory machinery differ between these two types of cells.
Griscelli syndrome is characterized by albinism and loss of CTL activity. The defective gene encodes a small GTP-binding protein, Rab27a41. A similar loss of Rab27a expression has been identified in ashen mice42. Notably, CTLs and NK cells from ashen mice cannot kill their targets through the granule pathway. Although possessing normal numbers of granules with normal morphology, ashen killer cells are unable to secrete them47,48. Live cell imaging and electron microscopy studies have shown that the granules polarize to the target cell interface but do not reach the plasma membrane and therefore do not complete the secretory process48. This shows that Rab27a has a crucial role in transporting the lysosomes from the MTOC to the plasma membrane.
Although loss of Rab27a also results in loss of melanosome secretion and consequent albinism, it seems that the similarity ends there. In melanocytes, Rab27a interacts with the cytosolic protein melanophilin, which in turn interacts with myosin Va, allowing melanosomes to be 'captured' onto the actin cytoskeleton as they move back and forth along the microtubules49,50. In this way the melanosomes are tethered at the plasma membrane and thus can be secreted. Loss of melanophilin, which occurs in leaden mice, or loss of myosin Va, which occurs in dilute mice or individuals with Elejalde syndrome (also referred to as Griscelli syndrome51), does not impair CTL function52, showing that the same complex of proteins is not involved in lytic granule secretion. In a sense this is not surprising, because the lytic granules move in a minus direction to polarize at the MTOC during secretion from CTLs, whereas melanosomes need to be captured from the plus end of microtubules for secretion from melanocytes.
But if Rab27a is not interacting with melanophilin in CTLs, then what is it doing? Numerous Rab27a-interacting proteins have been identified. A family of synaptotagmin-like proteins (Slp) have been shown to interact with Rab27a53,54,55, although it is not yet clear which ones are expressed in CTLs and whether they are involved in secretion.
Other Rab proteins also seem to be involved in the secretory process. The gunmetal mouse carries a mutation in the gene encoding Rab geranylgeranyl transferase (RGGT)43. Rab 27a, as well as other Rab proteins, requires RGGT activity to add the geranylgeranyl moiety required for attachment to their target membranes. Without this modification the Rabs are nonfunctional. Consequently, Rab27a and other unidentified Rab proteins have greatly reduced activity in gunmetal mice. The marked difference between CTLs derived from gunmetal mice and those derived from ashen mice is that on target cell recognition, many of the granules in the gunmetal CTLs are left around the periphery of the cell48, indicating that other Rab proteins are probably involved in microtubule attachment or movement. Both Rab6 (ref. 56) and Rab7 (refs. 57,58) are involved in microtubule movement in other types of cells, and it is possible that other Rabs have similar roles.
Insight into the proteins required at the plasma membrane has come from studies on Chediak-Higashi syndrome (CHS), a rare autosomal recessive disorder characterized by partial albinism and a defect in NK and CTL activity59. The most prominent morphological feature of this disease is the occurrence of giant lysosomes in all types of cells; however, only cells relying on the secretion of these lysosomes manifest pathological defects. CTLs from individuals affected with CHS possess giant cytotoxic granules that are not secreted60.
The gene that is mutated in CHS predicts protein of more than 400 kDa, known as CHS1 or LYST40,61. During early development, granule biogenesis is normal, and perforin and granzymes are synthesized and routed correctly to the granules60. Once formed, however, the granules seem to fuse to form giant organelles62. Several studies have led to the suggestion that the enlarged lysosomes found in CHS cells are the result of defects in membrane fusion or fission, which occur during the biogenesis of this organelle59. Curiously, in CTLs the enlarged granules can both polarize and dock at the immunological synapse (G.M.G. et al., unpublished data). The simplest explanation for the seemingly conflicting observations of the enlarged granules is that CHS1 may regulate membrane fusion and/or membrane fission events, one of which is crucial for degranulation at the immunological synapse. Recent data indicate that the CHS1 protein interacts with soluble N-ethylmaleimide-sensitive factor (NSF) attachment protein receptors (SNAREs)63, consistent with a role in membrane fusion or fission.
Granule cytotoxicity and immunological down-regulation
A feature common to both CHS and Griscelli syndrome is the onset of an acute phase leading to hemophagocytic lymphohistiocytosis (HLH), a disorder characterized by excessive lymphocyte expansion. HLH is also seen in individuals affected with familial hemophagocytic lymphohistiocytosis (FHL), a devastating childhood disease in which lymphocytes (in particular CD8+ T cells) expand uncontrollably and infiltrate into tissues. The ensuing production of excessive cytokines and their infiltration into tissues leads to massive tissue necrosis and organ failure64. Without bone marrow transplantation, FHL is usually fatal in the first year of life.
The molecular defect associated with about a third of FHL cases is caused by mutations in the gene encoding perforin44. Several different perforin mutations can give rise to FHL65,66,67,68. Intriguingly, mice that lack the transcriptional activator myeloid elf-1–like factor (MEF), which is involved in activating perforin in NK and NKT cells, also show polyclonal lymphocytic infiltrations into various organs, suggesting that they have immune dysregulation69.
Because defects in perforin activity and defects that prevent granule secretion both cause uncontrollable lymphocyte expansion, it has been suggested that the granule pathway of cytotoxicity has an essential role in homeostasis in the immune system64,70. The exact mechanism involved is not clear, and the proposal that perforin-mediated killing may be involved in immunoregulation70 has generated debate about how perforin might down-regulate the functions of CTLs71.
Perforin-deficient killer cells show profoundly impaired cytotoxic activity and are unable to kill many targets, as assessed by in vitro and in vivo assays72,73,74. This raises the issue of whether the lymphocyte expansion seen in FHL could be due to an inability to clear an infectious agent, which would result in antigenic persistence and thus the sustained stimulation and expansion of lymphocytes. The association of hemophagocytic syndromes with a viral trigger is well documented64; however, the issue of antigenic clearance has been addressed by studying perforin-deficient mice and it seems that the lymphoproliferation observed in these models is not simply a function of increased antigenic exposure. For example, even when viral burdens are equivalent, perforin-deficient mice show enhanced lymphocyte expansion after infection with lymphocytic choriomeningitis virus as compared with wild-type mice75. In addition, the synergistic effect of perforin mutation on Fas deficiency (whereby perforin deficiency markedly accelerates the lymphoproliferative disease and death seen in mice lacking Fas) supports a contribution of perforin-mediated killing to lymphocyte homeostasis76,75.
Multifunctional synapses
How might perforin-mediated killing down-regulate the T cell response? One possibility is that CTLs can kill each other—a process that has been called 'fratricide'. Work has shown that cloned CTLs can be killed by exposure to their cognate peptides in a dose-dependent manner77. More recently, it has been shown that CTLs can acquire major histocompatibility (MHC) class I molecules from their targets in an antigen dose–dependent manner. Notably, these MHC class I molecules are internalized by the CTLs and presented on the cell surface with peptide, rendering the CTLs susceptible to lysis by neighboring CTLs of the same clone78,79. Thus, the size of the CTL population might be regulated by CTL-mediated fratricide as CTLs acquire MHC class I from their targets and destroy each other. But how do CTLs acquire target membranes?
Studies of the immunological synapse suggest that the formation of this structure itself may lead to membrane transfer from target cells to CTLs36. The polarization of intracellular organelles towards the contact site is so distinctive that it is relatively straightforward to distinguish synapses that are dissociating from those that are tightly focused for secretion. At these 'dissociating synapses', which are characterized by the jumbled appearance of the intracellular organelles, areas of membrane fusion form 'bridges' between the target and effector cells.
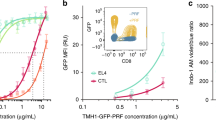
The transfer of membrane can be clearly seen when target cell membranes are labeled with fluorescently tagged proteins (Fig. 2 and Supplementary Video 1 online). When CTLs are conjugated to the target cell, some granules are clustered behind the MTOC and some are docked at the membrane, ready to release their contents and destroy the target. The organelles have a characteristic highly ordered appearance as they polarize toward this synapse (Fig. 2a–c). In live cells, the target cell membrane envelops the area surrounding the synapse on the CTL side. Electron microscopy images show that the granules retract (Fig. 2e), and that the MTOC and Golgi are less tightly polarized towards the contact site (Fig. 2d,e), as the cells part. Both electron microscopy and live cell studies show that strands of membranes from the dying targets are left tightly attached to the CTL as the two cells part36.
(a–e) A series of still frames from a movie (see Supplementary Video 1 online) showing CTLs killing a target cell, the membrane of which has been labeled with a fluorescent protein marker, and electron micrographs showing roughly equivalent stages of synapse formation. Granules polarize towards the immunological synapse as the CTL engages its target (a–c); as the CTL disengages, the granules withdraw from the synapse (d), where membrane from the target has accumulated. As the CTL detaches, target membrane is ripped off the dying target (e), and the CTL can engage a new target (color panel of e).
Transfer of membrane proteins has been noticed between other lymphocytes and their APCs. B cells can acquire antigenic integral membrane proteins from APCs80. Similarly, NK cells can acquire MHC class I molecules from their targets81,82,83. γδ T cells also acquire membrane proteins from their targets84. For all cell types, the transfer is dependent on antigen recognition and presumably on formation of the immunological synapse. When studied in detail, the transfer seems to be unidirectional and nonspecific36,85, suggesting that T, NK and possibly also B cells acquire and incorporate membrane proteins from their targets. These proteins are sometimes internalized and sorted as endogenous proteins in the lymphocytes.
Taken together, these examples suggest that membrane transfer may be driven, in part, by the formation of the immunological synapse. Although the physiological roles of membrane acquisition may differ between cell types, current data suggest that the acquisition of MHC class I molecules by T cells may promote self-recognition by CTLs and may be involved in down-regulating the immune response. In fact, MHC class I molecules can be visualized at a contact site between two CTLs with the granules of one cell polarized towards the other cell, consistent with the interaction leading to granule-mediated fratricide (Fig. 3). In diseases such as HLH, in which either perforin itself is nonfunctional or the granule exocytosis pathway is blocked, such down-regulation of the immune response also might be blocked.
Conclusion
Recent advances in immunology and cell biology have provided great insight into the way in which a killer cell delivers the lethal hit to its target. The events occurring at the immunological synapse may ultimately change the fate of a killer cell to that of a target cell. The study of rare immunodeficiency diseases has proved extremely valuable not only in deciphering the molecules involved in granule exocytosis, but also in highlighting the role of the granule pathway in immunological homeostasis. The fatal nature of a disease such as FHL is a powerful example of what happens when granule-mediated killing is impaired, and suggests that delivery of the kiss of death also provides the kiss of life.
Note: Supplementary information is available on the Nature Immunology website.
References
Millard, P.J., Henkart, M.P., Reynolds, C.W. & Henkart, P.A. Purification and properties of cytoplasmic granules from cytotoxic rat LGL tumors. J. Immunol. 132, 3197–3204 (1984).
Podack, E.R., Young, J.D. & Cohn, Z.A. Isolation and biochemical and functional characterization of perforin from cytolytic T cell granules. Proc. Natl. Acad. Sci. USA 82, 8629–8633 (1985).
Shinkai, Y., Takio, K. & Okumura, K. Homology of perforin to the ninth component of complement (C9). Nature 334, 525–527 (1998).
Tschopp, J., Massom, D. & Stanley, K.K. Structural-functional similarity between proteins involved in complement- and cytotoxic T-lymphocyte-mediated cytolysis. Nature 322, 831–834 (1986).
Sauer, H., Pratsch, L., Tschopp, J., Bhakdi, S. & Peters, R. Functional size of complement and perforin pores compared by confocal laser scanning microscopy and fluorescent microphotolysis. Biochim. Biophys. Acta 1063, 137–146 (1991).
Henkart, M.P. & Henkart, P.A. Lymphocyte mediated cytolysis as a secretory phenomenon. Adv. Exp. Med. Biol. 146, 227–247 (1982).
Lowin, B., Peitsch, M.C. & Tschopp, J. Perforin and granzymes: crucial effector molecules in cytolytic T lymphocyte and natural killer cell-mediated cytotoxicity. Curr. Top. Microbiol. Immunol. 198, 1–24 (1995).
Shi, L., Kraut, R.P., Aebersold, R. & Greenberg, A.H. A natural killer cell granule protein that induces DNA fragmentation and apoptosis. J. Exp. Med. 175, 553–566 (1992).
Heusel, J.W., Wesselschmidt, R.L., Shresta, S., Russell, J.H. & Ley, T.J. Cytotoxic lymphocytes require granzyme B for the rapid induction of DNA fragmentation and apoptosis in allogeneic target cells. Cell 76, 977–987 (1994).
Nakajima, H., Park, H.L. & Henkart, P.A. Synergistic roles of granzymes A and B in mediating target cell death by rat basophilic leukemia mast cell tumours also expressing cytolysin/perforin. J. Exp. Med. 181, 1037–1046 (1995).
Shiver, J.W. & Henkart, P.A. A noncytotoxic mast cell tumor line exhibits potent IgE-dependent cytotoxicity after transfection with the cytolysin/perforin gene. Cell 64, 1175–1181 (1991).
Shiver, J.W., Su, L. & Henkart, P.A. Cytotoxicity with target DNA breakdown by rat basophilic leukemia cells expressing both cytolysin and granzyme A. Cell 71, 315–322 (1992).
Barry, M. & Bleackley, R.C. Cytotoxic T lymphocytes: all roads lead to death. Nat. Rev. Immunol. 2, 401–409 (2002).
Beresford, P.J. et al. Granzyme A activates an endoplasmic reticulum-associated caspase-independent nuclease to induce single-stranded DNA nicks. J. Biol. Chem. 276, 43285–43293 (2001).
Fan, Z. et al. Cleaving the oxidative repair protein Ape1 enhances cell death mediated by granzyme A. Nat. Immunol. 4, 145–153 (2003).
Froelich, C.J. et al. New paradigm for lymphocyte granule mediated cytotoxicity. Targets bind and internalize granzyme B, but an endosomolytic agent is necessary for cytosolic delivery and subsequent apoptosis. J. Biol. Chem. 271, 29073–29079 (1996).
Motyka, B. et al. Mannose 6-phosphate/insulin-like growth factor II receptor is a death receptor for granzyme B during cytotoxic T cell-induced apoptosis. Cell 103, 491–500 (2000).
Browne, K.A. et al. Cytosolic delivery of granzyme B by bacterial toxins: evidence that endosomal disruption, in addition to transmembrane pore formation, is an important function of perforin. Mol. Cell. Biol. 19, 8604–8615 (1999).
Metkar, S.S. et al. Cytotoxic cell granule-mediated apoptosis: perforin delivers granzyme B–serglycin complexes into target cells without plasma membrane pore formation. Immunity 16, 417–428 (2002).
Gartung, C., Braulke, T., Hasilik, A. & von Figura, K. Internalization of blocking antibodies against mannose-6-phosphate specific receptors. EMBO J. 4, 1725–1730 (1985).
Gonzalez-Noriega, A., Grubb, J.H., Talkad, V. & Sly, W.S. Chloroquine inhibits lysosomal enzyme pinocytosis and enhances lysosomal enzyme secretion by impairing receptor recycling. J. Cell Biol. 85, 839–852 (1980).
Kuta, A.E., Reynolds, C.R. & Henkart, P.A. Mechanisms of lysis by large granular lymphocyte granule cytolysin: generation of a stable cytolysin-RBC intermediate. J. Immunol. 142, 4378–4384 (1989).
Uellner, R. et al. Perforin is activated by proteolytic cleavage during biosynthesis which reveals a phospholipid-binding C2 domain. EMBO J. 16, 7287–7296 (1997).
Winkler, U., Fraser, S.A. & Hudig, D. Perforin-enhancing protein, a low molecular weight protein of cytotoxic lymphocyte granules, enhances perforin lysis. Biochem. Biophys. Res. Commun. 236, 34–39 (1997).
Sanderson, C.J. The mechanism of T cell mediated cytotoxicity. I. The release of different cell components. Proc. R. Soc. Lond. B 192, 221–239 (1976).
Kupfer, A., Singer, S.J. & Dennert, G. On the mechanism of unidirectional killing in mixtures of two cytotoxic T lymphocytes. Unidirectional polarization of cytoplasmic organelles and the membrane-associated cytoskeleton in the effector cell. J. Exp. Med. 163, 489–498 (1986).
Balaji, K.N., Schaschke, N., Machleidt, W., Catalfamo, M. & Henkart, P.A. Surface cathepsin B protects cytotoxic lymphocytes from self-destruction after degranulation. J. Exp. Med. 196, 493–503 (2002).
Kataoka, T. et al. FLIP prevents apoptosis induced by death receptors but not by perforin/granzyme B, chemotherapeutic drugs, and γ-irradiation. J. Immunol. 161, 3936–3942 (1998).
Hirst, C.E. et al. The intracellular Granzyme B inhibitor, proteinase inhibitor 9, is up-regulated during accessory cell maturation and effector cell degranulation, and its overexpression enhances CTL potency. J. Immunol. 170, 805–815 (2003).
Burkhardt, J.K., Hester, S., Lapham, C.K. & Argon, Y. The lytic granules of natural killer cells are dual-function organelles combining secretory and pre-lysosomal compartments. J. Cell Biol. 111, 2327–2340 (1990).
Peters, P.J. et al. Cytotoxic T lymphocyte granules are secretory lysosomes, containing both perforin and granzymes. J. Exp. Med. 173, 1099–1109 (1991).
Geiger, B., Rosen, D. & Berke, G. Spatial relationships of microtubule organizing centers and the contact area of cytotoxic T lymphocytes and target cells. J. Cell Biol. 95, 137–143 (1982).
Kupfer, A. & Dennert, G. Reorientation of the microtubule-organizing center and the Golgi apparatus in cloned cytotoxic lymphocytes triggered by binding to lysable target cells. J. Immunol. 133, 2762–2766 (1984).
Kupfer, A., Dennert, G. & Singer, S.J. The reorientation of the Golgi apparatus and the microtubule-organizing center in the cytotoxic effector cell is a prerequisite in the lysis of bound target cells. J. Mol. Cell. Immunol. 2, 37–49 (1985).
Allan, V.J., Thompson, H.N. & McNiven, M.A. Motoring around the Golgi. Nat. Cell Biol. 4, E236–E242 (2002).
Stinchcombe, J.C., Bossi, G., Booth, S. & Griffiths, G.M. The immunological synapse of CTL contains a secretory domain and membrane bridges. Immunity 15, 751–761 (2001).
van der Merwe, P.A. Formation and function of the immunological synapse. Curr. Opin. Immunol. 14, 293–298 (2002).
Lyubchenko, T.A., Wurth, G.A. & Zweifach, A. Role of calcium influx in cytotoxic T lymphocyte lytic granule exocytosis during target cell killing. Immunity. 15, 847–859 (2001).
Kuhn, J.R. & Poenie, M. Dynamic polarization of the microtubule cytoskeleton during CTL-mediated killing. Immunity 16, 111–121 (2002).
Perou, C.M. et al. Identification of the murine beige gene by YAC complementation and positional cloning. Nat. Genet. 13, 303–308 (1996).
Menasche, G. et al. Mutations in RAB27A cause Griscelli syndrome associated with haemophagocytic syndrome. Nat. Genet. 25, 173–176 (2000).
Wilson, S.M. et al. A mutation in Rab27a causes the vesicle transport defects observed in ashen mice. Proc. Natl. Acad. Sci. USA 97, 7933–7938 (2000).
Detter, J.C. et al. Rab geranylgeranyl transferase α mutation in the gunmetal mouse reduces Rab prenylation and platelet synthesis Proc. Natl. Acad. Sci. USA 97, 4144–4149 (2000).
Stepp, S.E. et al. Perforin gene defects in familial haemophagocytic lymphohistiocytosis. Science 286, 1957–1959 (1999).
Griffiths, G.M. Albinism and immunity: what's the link? Curr. Mol. Med. 2, 479–483 (2002).
Stinchcombe, J.C. & Griffiths, G.M. Regulated secretion from hemopoietic cells. J. Cell Biol. 147, 1–6 (1999).
Haddad, E.K., Wu, X., Hammer, J.A. & Henkart, P.A. Defective granule exocytosis in Rab27a-deficient lymphocytes from Ashen mice. J. Cell Biol. 152, 835–842 (2001).
Stinchcombe, J.C. et al. Rab27a is required for regulated secretion in cytotoxic T lymphocytes. J. Cell Biol. 152, 825–834 (2001).
Hume, A.N. et al. Rab27a regulates the peripheral distribution of melanosomes in melanocytes. J. Cell Biol. 152, 795–808 (2001).
Wu, X., Wang, F., Rao, K., Sellers, J.R. & Hammer, J.A. Rab27a is an essential component of melanosome receptor for myosin Va. Mol. Biol. Cell. 13, 1735–1749 (2002).
Pastural, E. et al. Two genes are responsible for Griscelli syndrome at the same 15q21 locus. Genomics 63, 299–306 (2000).
Hume, A.N. et al. The leaden gene product is required with Rab27a to recruit myosin Va to melanosomes in melanocytes. Traffic 3, 193–202 (2002).
Fukuda, M., Kuroda, T.S. & Mikoshiba, K. Slac2-a/melanophilin, the missing link between Rab27 and myosin Va: implications of a tripartite protein complex for melanosome transport. J. Biol. Chem. 277, 12432–12436 (2002).
Kuroda, T.S., Fukuda, M., Ariga, H. & Mikoshiba, K. Synaptotagmin-like protein 5: a novel Rab27A effector with C-terminal tandem C2 domains. Biochem. Biophys. Res. Commun. 293, 899–906 (2002).
Strom, M., Hume, A.N., Tarafder, A.K., Barkagianni, E. & Seabra, M.C. A family of Rab27-binding proteins. Melanophilin links Rab27a and myosin Va function in melanosome transport. J. Biol. Chem. 277, 25423–25430 (2002).
Echard, A. et al. Interaction of a Golgi-associated kinesin-like protein with Rab6. Science. 279, 580–585 (1998).
Jordens, I. et al. The Rab7 effector protein RILP controls lysosomal transport by inducing the recruitment of dynein-dynactin motors. Curr. Biol. 11, 1680–1685 (2001).
Lebrand, C. et al. Late endosome motility depends on lipids via the small GTPase Rab7. EMBO J. 21, 1289–300 (2002).
Ward, D.M., Griffiths, G.M., Stinchcombe, J.C. & Kaplan, J. Analysis of the lysosomal storage disease Chediak-Higashi syndrome. Traffic 1, 816–822 (2000).
Baetz, K., Isaaz, S. & Griffiths, G.M. Loss of cytotoxic T lymphocyte function in Chediak-Higashi syndrome arises from a secretory defect that prevents lytic granule exocytosis. J. Immunol. 154, 6122–6131 (1995).
Barbosa, M.D. et al. Identification of the homologous beige and Chediak-Higashi syndrome genes. Nature 382, 262–265 (1996).
Stinchcombe, J.C., Page, L.J. & Griffiths, G.M. Secretory lysosome biogenesis in cytotoxic T lymphocytes from normal and Chediak-Higashi syndrome patients. Traffic 1, 435–444 (2000).
Tchernev, V.T. et al. The Chediak-Higashi protein interacts with SNARE complex and signal transduction proteins. Mol. Med. 8, 56–64 (2002).
de Saint Basile, G. & Fischer, A. The role of cytotoxicity in lymphocyte homeostasis. Curr. Opin. Immunol. 13, 549–554 (2001).
Arico, M. et al. Haemophagocytic lymphohistiocytosis: proposal of a diagnostic algorithm based on perforin expression. Br. J. Haematol. 119, 180–188 (2002).
Feldmann, J. et al. Functional consequences of perforin gene mutations in 22 patients with familial haemophagocytic lymphohistiocytosis. Br. J. Haematol. 111, 965–972 (2002).
Goransdotter Ericson, K. et al. Spectrum of perforin gene mutations in familial hemophagocytic lymphohistiocytosis. Am J. Hum. Genet. 68, 590–597 (2001).
Suga, N. et al. Perforin defects of primary haemophagocytic lymphohistiocytosis in Japan. Br. J. Haematol. 116, 346–349 (2002).
Lacorazza, H.D. et al. The ETS protein MEF plays a critical role in perforin gene expression and the development of natural killer and NK-T cells. Immunity 17, 437–449 (2002).
Stepp, S.E., Mathew, P.A., Bennett, M., de Saint-Basile, G. & Kumar, V. Perforin: more than just an effector molecule. Immunol. Today 21, 254–256 (2000).
Moretta, L., Moretta, A., Hengartner, H. & Zinkernagel, R.M. On the pathogenesis of perforin defects and related immunodeficiencies. Immunol. Today 21, 593–594 (2000).
Kagi, D., Ledermann, B., Burki, K., Zinkernagel, R.M. & Hengartner, H. Molecular mechanisms of lymphocyte-mediated cytotoxicity and their role in immunological protection and pathogenesis in vivo. Annu. Rev. Immunol. 14, 207–232 (1996).
Lowin, B., Hahne, M., Mattman, C. & Tschopp, J. Cytolytic T cell cytotoxicity is mediated through perforin and Fas lytic pathways. Nature 370, 650–652 (1994).
Walsh, C.M. et al. Immune function in mice lacking the perforin gene. Proc. Natl. Acad. Sci. USA 91, 10854–10858 (1994).
Matloubian, M. et al. A role for perforin in downregulating T-cell responses during chronic viral infection. J. Virol. 73, 2527–2536 (1999).
Kagi, D., Odermatt, B. & Mak T.W. Homeostatic regulation of CD8+ T cells by perforin. Eur. J. Immunol. 29, 3262–3272 (1999).
Walden, P.R. & Eisen, H.N. Cognate peptides induce self-destruction of CD8+ cytolytic T lymphocytes. Proc. Natl. Acad. Sci. USA 87, 9015–9019 (1990).
Huang, J.F. et al. TCR-mediated internalization of peptide-MHC complexes acquired by T cells. Science 286, 952–954 (1999).
Hwang, I. et al. T cells can use either T cell receptor or CD28 receptors to absorb and internalise cell surface molecules derived from antigen-presenting cells. J. Exp. Med. 191, 1137–1148 (2000).
Batista, F.D., Iber, D. & Neuberger, M.S. B cells acquire antigen from target cells after synapse formation. Nature 411, 489–494 (2001).
Carlin, L.M., Eleme, K., McCann, F.E. & Davis, D.M. Intercellular transfer and supramolecular organization of human leucocyte antigen C at inhibitory natural killer cell immune synapses. J. Exp. Med. 194, 1507–17 (2001).
Sjostrom, A. et al. Acquisition of external major histocompatibility complex class I molecules by natural killer cells expressing inhibitory Ly49 receptors. J. Exp Med. 194, 1519–1530 (2001).
Tabiasco, J. et al. Active trans-synaptic capture of membrane fragments by natural killer cells. Eur. J. Immunol. 32, 1502–1508 (2002).
Espinosa, E., Tabiasco, J., Hudrisier, D. & Fournie, J.J. Synaptic transfer by human gamma delta T cells stimulated with soluble or cellular antigens. J. Immunol. 168, 6336–6343 (2002).
Hudrisier, D., Riond, J., Mazarguil, H., Gairin, J.E. & Jolly, E. Cutting edge: CTLs rapidly capture membrane fragments from target cells in a TCR-signaling dependent manner. J. Immunol. 166, 3645–3649 (2001).
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Rights and permissions
About this article
Cite this article
Trambas, C., Griffiths, G. Delivering the kiss of death. Nat Immunol 4, 399–403 (2003). https://doi.org/10.1038/ni0503-399
Issue Date:
DOI: https://doi.org/10.1038/ni0503-399
This article is cited by
-
Outsmarting trogocytosis to boost CAR NK/T cell therapy
Molecular Cancer (2023)
-
A transistor-like pH-sensitive nanodetergent for selective cancer therapy
Nature Nanotechnology (2022)
-
Rapid, label-free classification of tumor-reactive T cell killing with quantitative phase microscopy and machine learning
Scientific Reports (2021)
-
The immune system of jawless vertebrates: insights into the prototype of the adaptive immune system
Immunogenetics (2021)
-
PD-L1/L2 protein levels rapidly increase on monocytes via trogocytosis from tumor cells in classical Hodgkin lymphoma
Leukemia (2020)