Abstract
Episodes of transient loss of consciousness (TLOC) events pose diagnostic difficulties, as the causes are diverse, carry vastly different risks, and span various specialties. An inconsistent terminology contributes to the confusion. Here, we present a classification scheme for TLOC, based on ongoing multidisciplinary efforts including those of the Task Force on Syncope of the European Society of Cardiology. We also discuss the pathophysiology of TLOC and the key clinical features that aid diagnosis. TLOC is defined as an apparent loss of consciousness with an abrupt onset, a short duration, and a spontaneous and complete recovery. Syncope is defined as TLOC due to cerebral hypoperfusion, and is divided into reflex syncope (synonymous with neurally mediated syncope), syncope due to orthostatic hypotension, and cardiac syncope (arrhythmic or associated with structural cardiac disease). The other major groups of TLOC are generalized epileptic seizures, functional TLOC (psychogenic TLOC mimicking either epilepsy or syncope), and a further group of miscellaneous disorders. The management of patients who experience TLOC requires the recognition of the defining features of each of the major groups, and cooperation between different clinical specialties.
Key Points
-
Transient loss of consciousness (TLOC) is an apparent loss of consciousness with an abrupt onset, short duration, and spontaneous and complete recovery
-
TLOC is a distinct diagnostic group comprising syncope, generalized epileptic seizures, functional TLOC and a group of rare causes
-
Syncope is divided into reflex syncope, syncope due to orthostatic hypotension and cardiac syncope
-
Reflex syncope is by far the most common form of TLOC and might affect up to 40% of the population
-
Diagnosis of TLOC requires an understanding of key clues, pathophysiology and underlying epidemiological patterns, and entails a multidisciplinary approach
Similar content being viewed by others
Introduction
The diagnosis of spells of unconsciousness can be problematic for various reasons. As the spell has typically ended by the time that the patient sees a physician, the cause must be established after the event, sometimes on shaky grounds. Causes of brief episodes of unconsciousness span a range of clinical specialties, and include cardiac arrhythmia, the 'common faint', epileptic seizures, functional (psychogenic) disorders, and concussion. Diagnostic insecurity can either induce a 'shotgun' approach aimed at all possible causes,1 or, conversely, an approach purely restricted to one's own specialty. The latter approach could be responsible for many mistaken diagnoses of epilepsy.2,3,4
The most common cause of spells of unconsciousness, reflex syncope, affects up to 40% of the population,5,6,7 but seems to receive little attention in medical teaching. The medical literature can be confusing: some authors use 'syncope' widely for many causes, whereas others, often implicitly, narrow it down to one cause, namely cerebral hypoperfusion.8,9,10 A review of the top-impact journals revealed that syncope and related concepts were left undefined in over 50% of papers.11
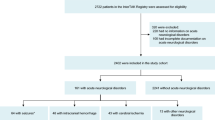
The multidisciplinary Task Force on Syncope introduced the term 'transient loss of consciousness' (TLOC) to describe the wider concept of brief episodes of unconsciousness,12,13 rendering syncope as just one form of TLOC under the resulting classification scheme.13,14,15 The TLOC concept was designed to bundle together a group of disorders that feature in one another's differential diagnosis (Figure 1). This Review aims to improve diagnostic skills by providing an overview of the various forms of TLOC—with a particular emphasis on reflex syncope—and highlighting key clues to their diagnosis.
Definitions
The word 'unconscious' is sometimes used to describe states such as absence seizures and complex partial seizures, in which people seem to be awake but are unaware of themselves or their surroundings. This usage corresponds to Plum and Posner's content aspect of consciousness.16 The term 'unconscious' is, however, more commonly used to describe a loss of the arousal aspect of consciousness, which describes a state ranging from complete alertness through sleepiness and stupor to coma. 'Unconsiousness' will be used exclusively in the latter sense in our definition of TLOC, meaning that it is necessarily associated with a loss of postural control (falling). Hence, absence seizures and complex partial seizures are not considered to be forms of TLOC, as patients typically remain upright during attacks. Loss of consciousness in TLOC is usually determined through history taking, and its occurrence can be established using three historical features. First, a loss of normal motor control is evident as flaccidity or stiffness, either of which can be accompanied by jerking movements, and postural control is lost so that patients fall if they are in an upright position. Second, normal responsiveness is lost. Third, the patient experiences amnesia for the event.
TLOC is defined as an apparent loss of consciousness, as defined above, with a rapid onset, a short duration, and a spontaneous and complete recovery. This definition includes disorders in which consciousness seems to be lost, such as functional—or psychogenic—TLOC (see below). The fact that these attacks can be mistaken for either syncope or epilepsy warrants their inclusion in the TLOC classification. Deviation from any of the defining features of TLOC changes the differential diagnosis; for example, lack of unconsciousness means that all causes of falling need to be considered,17 and a longer duration of unconsciousness would exclude syncope but include intoxications and metabolic disorders (Figure 1).
Figure 2 summarizes the main forms of TLOC, and Box 1 provides a more detailed classification. TLOC due to cerebral concussion will not be discussed in detail, as the cause is usually obvious. Problems arise when TLOC causes falls that in turn cause concussion, as concussional amnesia can obscure the fact that TLOC caused the fall. Syncope, epileptic seizures and functional TLOC receive separate headings because they are common and/or carry appreciable risks. The various rare causes do not share a common pathophysiology or presentation, and are grouped together to underline their minor importance in terms of prevalence.
Traumatic TLOC (concussion) can usually be recognized easily, as the cause tends to be obvious. Nontraumatic TLOC is divided into four groups: syncope, epileptic seizures, functional TLOC, and a miscellaneous group encompassing rare disorders that cause TLOC and conditions that can be mistaken for TLOC; the disorders in the latter group do not share a common pathophysiology. See Table 1 for a more detailed classification of TLOC. Abbreviation: TLOC, transient loss of consciousness.
Syncope
Syncope is defined as TLOC due to cerebral hypoperfusion. The signs and symptoms of syncope fall into two groups, the first relating to the consequences of cerebral hypoperfusion and the second being linked to the cause of syncope.
Consequences of cerebral hypoperfusion
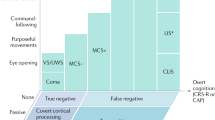
Expressions of cerebral hypoperfusion are common to all forms of syncope, but not all features associated with this state occur in all attacks, partly owing to differences in the rapidity of onset. In very rapid syncope, such as with sudden cardiac asystole, individuals can notice few features before losing consciousness. In slowly developing forms, as might occur in autonomic failure, more features might be noticed by the patient. Difficulty in thinking and light-headedness occur early, followed by loss of color vision and blurring or darkening of vision. Sounds can seem to come from far away. Just before becoming unconscious, individuals can lose the ability to act purposely while still remaining aware.18
The onset of unconsciousness is accompanied by a loss of voluntary motor control. Patients are often flaccid during falls, but stiffness can sometimes occur.19 The eyes are usually open, even if they were closed before the attack began, and are directed upwards or straight ahead.18,20,21 Jerks of the limbs, lasting only a few seconds, can occur. These jerks are usually small in amplitude, do not cause pronounced bending of the knees or elbows, and are not rhythmic or synchronous. The incidence of myoclonic jerks varies: estimates in fainting blood donors were 12% in a retrospective series22 but ∼45% in a prospective series.23 Among individuals performing the 'mess trick', a self-induced form of syncope marked by an almost instantaneous fall in blood pressure, up to 90% exhibited jerks.19 The nature of the jerks aids the differentiation of syncope from epileptic seizures (see below). Urinary incontinence occurs in about one-quarter of syncope cases,21,24,25 and does not reliably differentiate between syncope and epilepsy. Tongue biting, however, is extremely rare in syncope,21,25 and if it does occur it usually involves the tip of the tongue, rather than the side as in epilepsy.26 Unconsciousness usually lasts less than 20 s in syncope,19,21 but can be longer in duration if patients are kept upright. Some patients lie still while taking time to collect themselves, and this might be interpreted as prolongation of unconsciousness.
Falling or lying down usually helps to restore consciousness in syncope by increasing venous return and cardiac output, leading to a rise in blood pressure. Cerebral blood pressure is also increased by lying down: in people who are upright the brain is 25–30 cm higher than the heart, so arterial pressure at brain height is about 20 mmHg less than while lying down. Resumption of cerebral perfusion restores consciousness very quickly, and patients can subsequently think clearly and remember events. Fatigue and sleepiness can persist for several hours after syncope, particularly in children.
Causes of syncope
Reflex syncope
Reflex syncope—also known as neurally mediated syncope—is often both preceded and followed by autonomic activation, which is characterized by nausea, a deathly white pallor and sweating. These symptoms are less pronounced in the elderly than in younger individuals. A key feature of reflex syncope is that it is usually triggered, and several variants of this condition are named according to their triggers.
In vasovagal syncope, the most common triggers are acute pain and fear, usually in combination, and prolonged standing.6 In the former case, neither the fear nor the pain needs be excessive. Vasovagal syncope occurs at some point in up to 40% of the population, and has a pronounced familial occurrence27 but an unclear genetic background.28 The incidence of vasovagal syncope peaks initially at 13–16 years of age,5,7,29 is relatively rare during most of adult life, but often re-emerges in old age.7 First episodes of vasovagal syncope are rarely observed beyond the age of 35 years,7,29 so other causes must be considered in cases of syncope beginning after that age. The issue of whether this condition has any evolutionary purpose has been the subject of some debate.30,31,32
The pathophysiology of vasovagal syncope is poorly understood,33 particularly in the case of pure emotional syncope: how the mere sight of a needle, for example, triggers syncope in individuals even when lying down is a mystery. In orthostatic vasovagal syncope, the main contributory factor is a decrease in central blood volume due to pooling of blood in the lower regions of the body. Orthostatic vasovagal syncope consistently occurs when cardiac output decreases by around 50%,33,34 which might explain why vasovagal syncope is particularly likely to occur in the presence of hypovolemia (due to vomiting, diarrhea or blood loss) or skin vasodilatation (due to heat, fever or alcohol use). Mechanical stimuli such as straining can further decrease the central blood volume. Periods of anxiety and distress seem to increase the chance of vasovagal syncope.35
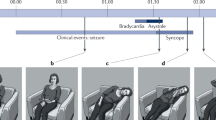
The current view is that unconsciousness ensues when mean cerebral blood pressure falls to around 40 mmHg.33 Arterial hypotension is normally counteracted by arterial baroreflexes, which attempt to maintain blood pressure by increasing systemic vascular resistance and heart rate. In orthostatic vasovagal syncope, a period of instability with oscillations of blood pressure and heart rate is often observed, after which blood pressure and/or heart rate fall sharply; this latter phase is the syncopal reflex proper (Figure 3, Figure 4). A fall in blood pressure usually occurs first, followed by bradycardia, which is attributable to increased vagal activity.33 Syncope in which bradycardia is thought to be a more important contributory factor than low blood pressure is termed 'cardioinhibitory vasovagal syncope'. By contrast, if blood pressure drops but the heart rate shows little or no decrease, the reflex is termed 'vasodepressive vasovagal syncope'.
Schematized heart rate and blood pressure patterns for vasovagal syncope evoked by standing and syncope due to orthostatic hypotension. a | Standing only rarely evokes vasovagal syncope, and the timing is not clearly related to the duration of standing. Sweating, nausea and pallor appear before frank drops in blood pressure or heart rate, indicating that autonomic adjustments to standing have started to malfunction. In both vasodepressor and cardioinhibitory vasovagal syncope, a fall in blood pressure signifies the onset of the reflex proper. Pronounced bradycardia or asystole indicates the cardioinhibitory type. Syncope usually causes a fall that quickly restores blood pressure, except when asystole occurs; in that case the circulation resumes when asystole ends. b | In syncope due to orthostatic hypotension, blood pressure starts to drop immediately on standing up. Unlike vasovagal syncope while standing, orthostatic hypotension tends to recur when a patient is asked to stand up repeatedly, although the degree of hypotension varies. A compensatory increase in heart rate might occur, depending on the extent of autonomic damage. Blood pressure falls less steeply as standing continues and tends to stabilize at a low level unless syncope intervenes. The lying position helps to restore blood pressure.
1 min segment of a tilt table test in a 40-year-old man suspected of having vasovagal syncope. Finger blood pressure was recorded continuously. A selection of EEG channels is shown, and the clinical observations were taken from a video. 1 min before the events shown, the patient had complained of nausea, sweating and light-headedness, and his blood pressure had started to drop. EEG slowing started when systolic blood pressure dropped to about 50 mmHg; the heart rate was ∼45 bpm at the time. Asystole lasted about 8 s. The EEG flattened for a similar period, but only after a delay. Transient loss of consciousness was observed, starting with sagging of the face and dropping of the head to one side. The eyes remained open and the patient was unresponsive for about 14 s. Muscle jerks were observed just before and just after the flat period of the EEG. The patient was tilted back when he became unresponsive. Permission obtained from Guarantors of Brain © Wieling, W. et al. Brain (in press).
Vasovagal syncope is commonly thought to result from a withdrawal of sympathetic activity, which releases vasoconstriction, leading to a fall in systemic vascular resistance. Recent studies, however, suggest that systemic vascular resistance does not decrease during presyncope in the majority of patients.34,36,37 In these studies, the fall in systolic blood pressure to around 80 mmHg depended on a decrease in cardiac output, suggesting that the classic observations—pronounced vasodilatation in the forearm and withdrawal of muscle sympathetic activity—only occur at a late stage during a severe vasovagal reaction. The fall in blood pressure is usually much less steep in elderly individuals than in younger patients.37
Vasovagal syncope can also occur shortly after exercise,38 and presumed vasovagal syncope might even occur without a clear trigger. Triggers vary between episodes; if patients present with an uncommon trigger, the existence of previous attacks with typical triggers aids the diagnosis. The phrase 'situational syncope' is used to indicate syncope elicited by various specific triggers, such as micturition, defecation, coughing and swallowing. Knowledge of the triggers that commonly evoke syncope aids recognition of the event as syncopal.
The term 'carotid sinus syncope' encompasses both spontaneous and induced carotid sinus syncope. Spontaneous carotid sinus syncope is a very rare form of syncope (<1% of cases in large series) in which external pressure exerted on the carotid sinus by, for example, tight clothing or shaving mimics high blood pressure. The baroreflex subsequently reduces the blood pressure through bradycardia and/or vasodilatation. Massage of the carotid sinus is used in elderly individuals to test for carotid sinus hypersensitivity, usually in the context of a tilt table test. If massage results in a short asystole of at least 3 s and/or a blood pressure drop of over 50 mm Hg but no syncope, the response is considered to be hypersensitive. If, on the other hand, massage results in syncope, which requires longer periods of asystole or very low blood pressure, the response is called induced carotid sinus syncope.13 Abnormal massage responses have been linked to the occurrence of syncope and falls in elderly individuals, but the consequences for patient care are not clear.39,40
Reflex syncope is not associated with increased cardiovascular or neurological morbidity or mortality. Recurrent syncope of any type, however, carries risks of associated trauma, and can be accompanied by psychological, schooling, employment and driving problems.35,41,42,43,44
Syncope due to orthostatic hypotension
Orthostatic hypotension is a physical sign defined as a fall in systolic blood pressure of 20 mmHg or more, and/or a drop in diastolic pressure of 10 mmHg or more, within 3 min of standing up.45,46,47 Orthostatic hypotension only causes syncope if the fall in blood pressure is particularly pronounced. The general definition of orthostatic hypotension should be distinguished from 'initial orthostatic hypotension' and 'delayed orthostatic hypotension', as described below. Orthostatic hypotension is essentially a measurement result that should be differentiated from associated complaints45,46,48 and from its underlying mechanisms. The 3-minute period is generally accepted for routine clinical purposes, and tests conducted on this basis yield abnormal results in at least 50% of patients with autonomic disturbances.13,49,50,51,52,53 Figure 3 compares and contrasts events in orthostatic hypotension with those in vasovagal syncope.
Orthostatic hypotension is most often caused by medication, particularly drugs that cause vasodilatation or hypovolemia. A less frequent cause is autonomic failure, which in this context denotes the inability of the autonomic nervous system to adjust blood pressure on rising to a vertical position. The term 'primary autonomic failure' refers to a group of relatively rare neurodegenerative diseases: pure autonomic failure, multiple system atrophy, Parkinson disease with autonomic failure, and Lewy body dementia.50 'Secondary autonomic failure' denotes diseases that are not primarily neurodegenerative in nature but can nevertheless cause damage to the autonomic nervous system, such as diabetes and amyloidosis.50
The main complaints associated with orthostatic hypotension fall under the heading of orthostatic intolerance, and include light-headedness, dizziness, and, relatively rarely, syncope.11,12 The symptoms do not necessarily occur immediately after standing up. Pain in the neck and shoulders ('coat hanger pain') due to ischemia of local muscles, which resolves quickly on lying down, provides a diagnostic clue.54 Many patients with orthostatic hypotension due to autonomic failure also have post-exercise hypotension,55,56 in which orthostatic intolerance occurs immediately after the cessation of physical exercise, such as resting at the top of a flight of stairs or stopping a brisk walk suddenly. Ingestion of food can result in postprandial hypotension in individuals with orthostatic hypotension.
Initial orthostatic hypotension refers to a brief light-headedness and blurring or darkening of vision on arising suddenly after long period of rest or from squatting. This phenomenon is common in otherwise healthy individuals, and can sometimes cause syncope. Initial orthostatic hypotension is attributable to a mismatch between cardiac output and systemic vascular resistance, and is caused by failure of an otherwise normal autonomic nervous system to adapt the circulation promptly to the upright position. By contrast, the autonomic nervous system is impaired or damaged in conventional forms of orthostatic hypotension. Also, unlike conventional orthostatic hypotension, initial orthostatic hypotension is transient in nature, and episodes are so brief that they can only be measured with continuous blood pressure monitoring.57
Delayed orthostatic hypotension appears more than 3 min after standing.53,58 This condition is poorly understood and merits further study.
Cardiac syncope
Cardiac syncope primarily involves a sudden impairment of cardiac output; however, inadequate autonomic vascular responsiveness is now recognized to have a crucial role in most cases. In cases of paroxysmal tachyarrhythmia, for example, prompt vasoconstriction can normally help prevent blood pressure from falling to symptomatic levels. Although the tachycardia rate is important, the vascular component is understood to determine whether the arrhythmia is tolerated or whether loss of consciousness occurs. Similarly, in the setting of structural disease such as aortic stenosis or obstructive cardiomyopathy, an inappropriate reflex response, resulting in vasodilation rather than vasoconstriction, has long been known to contribute to syncope susceptibility. Additionally, in elderly individuals, an inadequate increase in cardiac output during exertion (due to systolic and/or diastolic ventricular dysfunction, or to chronotropic incompetence) can be aggravated by varying degrees of otherwise subclinical autonomic failure, or by drugs prescribed for conditions such as hypertension or ischemic heart disease. The two main causes of cardiac syncope, arrhythmia (both tachycardias and bradycardias) and structural heart disease, are far more common in the elderly than in younger individuals. Syncope in elderly individuals is also frequently multifactorial.12,13
Cardiac syncope is much less common than reflex or orthostatic syncope, but is associated with a much more worrisome prognosis,59 although mortality risk is determined principally by the severity of underlying heart disease.
Cardiac arrhythmias can occur in otherwise seemingly healthy individuals. The most frequent sustained arrhythmias in this setting are paroxysmal supraventricular tachycardias and certain paroxysmal ventricular tachycardias that arise in the ventricular outflow tracts or in the fascicular conduction system. Arrhythmias are, however, more commonly associated with structural heart disease (especially ischemic disease, but also cardiomyopathies of diverse etiologies), or as a proarrhythmic effect of drugs used to treat co-existing conditions (for example, antiarrhythmic agents, psychotropic drugs, or antibiotics).60 With regard to the proarrhythmic effects of drugs, many commonly used medications adversely prolong ventricular repolarization and thereby predispose the individual to 'torsade de pointes' ventricular tachycardia, whereas others slow conduction in diseased myocardium and increase the risk of development of re-entry tachyarrhythmias or, conversely, bradycardias due to conduction block.
Syncope due to arrhythmia can occur without any recognizable trigger. In fact, repeated syncope without a recognizable triggering pattern, or syncope that is reported when the patient is supine, should raise suspicion of a cardiac cause, especially in individuals with a history and/or signs of structural heart disease. Furthermore, abnormally low heart rates (bradyarrhythmia) cause syncope more often than high rates (tachyarrhythmia). In fact, bradyarrhythmias are the most frequent cause of syncope in structural heart disease, owing to adverse effects of disease-induced fibrosis, ischemia or stretch on sinus node function and intraventricular conduction system integrity, the results of which are excessive sinus bradycardia or pauses and/or atrioventricular conduction block. In addition, certain drugs used to treat structural heart disease problems (for example, β-adrenergic blockers, calcium channel blockers or antiarrhythmic drugs) might inadvertently trigger or exacerbate susceptibility to symptomatic slow heart rhythms. As a rule, syncope can be attributable to a sustained low ventricular rate (usually <30 bpm for 15–30 s), or to a prolonged pause in heart rhythm, which probably needs to last for more than 5 s. The classic example of the latter is Stokes–Adams syncope due to intermittent atrioventricular heart block (but which could equally be due to a lengthy sinus pause), which is characterized by a sudden onset and absence of premonitory symptoms. Similar pauses that can trigger syncope or near-syncope or unexplained 'falls' can also occur after abrupt termination of certain common tachyarrhythmias, such as paroxysmal atrial fibrillation.
From the perspective of mortality, the most important causes of cardiac syncope are ventricular tachyarrhythmias in patients with ischemic heart disease or cardiomyopathies. However, as noted earlier, drug-induced arrhythmias are becoming an increasingly prevalent problem, particularly in the case of drugs that delay ventricular depolarization (that is, prolong the QT interval on the electrocardiogram).
Arrhythmic syncope is rare in the young, not only because the causes are less prevalent, but also because young people are better able to tolerate rapid heart rates than are older individuals. The main causes of arrhythmic syncope in the younger age group are hereditary channelopathies, in particular the hereditary prolonged QT syndromes and Brugada syndrome.61,62 Among the more common of the long QT syndromes, syncope can be induced by startling stimuli such as an alarm clock, diving or exercise. In Brugada syndrome, syncope typically occurs at night, with slow heart rates triggering a polymorphous ventricular tachyarrhythmia. If investigations in a patient with syncope suggest a family history of sudden death at a young age, the presence of a hereditary arrhythmia syndrome should be carefully considered.
Structural heart disease can cause syncope when cardiac output fails to meet demands. As a result, syncope might be provoked by exercise or even moderate exertion such as climbing stairs. The classic example is aortic stenosis, in which a fixed outflow obstruction restricts increase of cardiac output, and inappropriate vasodilation often occurs. A similar phenomenon occurs in severe mitral valvular stenosis and in obstructive cardiomyopathy. In ischemic heart disease, inadequacy of coronary perfusion can similarly cause syncope during exertion.
Important diagnostic clues to a cardiac cause of syncope are baseline ECG abnormalities (for example, wide QRS interval due to bundle branch block, pre-excitation syndrome, or QT interval prolongation), a prior history of cardiac disease (for example, previous myocardial infarction or history of heart failure), a family history of syncope (and, in particular, unexpected death at a young age), syncope during physical exercise or while lying down, and facial cyanosis during the episode.63,64 In addition, the likelihood of cardiac syncope increases with age, for the reasons that were outlined above.
Palpitations before syncope have limited predictive value for a cardiac or arrhythmic cause of syncope. The presence of palpitations is more helpful in older patients than in younger individuals, in whom so-called 'palpitations' might be attributable to innocent atrial or ventricular ectopic beats, or sinus tachycardia occurring due to emotion, stress, or even the early phase of evolving vasovagal syncope.
The absence of findings suggestive of 'autonomic activation' is a marker more consistent with cardiac syncope than reflex syncope, and may help to distinguish the two conditions during the initial history taking.64 On the other hand, a pronounced red color of the face during recovery has been noted to indicate arrhythmic syncope, but is not in fact a valuable diagnostic feature as it can also occur in reflex syncope if the onset and offset are sudden.65
Epileptic seizures
Tonic, tonic–clonic and atonic epileptic seizures are the only seizure types that fall under the TLOC heading.12,13,14 Recognition of epileptic seizures is usually straightforward, except in cases where eyewitness accounts are lacking and patients have no recollection of events. Atonic and tonic epileptic seizures are rare and mostly affect people with known neurological problems or learning disabilities.66 In contrast to syncope, epileptic seizures rarely have a trigger. Triggering does, however, occur in reflex epilepsies, in which the best-known triggers are flashing lights.67 One of the very few triggers that can evoke syncope as well as epilepsy is startling68—this trigger can evoke both startle epilepsy69 and syncope in hereditary prolonged QT syndromes.70
Convulsive seizures can start as partial seizures, and attacks that begin with mumbling or purposeless acts or with jerks of one extremity while the person is upright are strongly indicative of an epileptic nature. The classic epileptic aura with a rising sensation in the abdomen or an unpleasant smell is rare; aura patterns tend to repeat themselves in patients, who learn to recognise them as such.71
Epileptic seizures usually last 1 min or more, and are usually longer than syncopal attacks. The duration of either type of episode tends to be overestimated by eyewitnesses, but the timing difference is still useful for diagnosis. In epilepsy, but not in syncope, jerks can begin unilaterally and before the fall. The jerks are coarse, symmetrical and rhythmic, and might involve pronounced bending of the knees and elbows. Physicians can help eyewitnesses to recognize the nature of the jerks by mimicking the different types of movements.24 The eyes are usually open in epilepsy, as in syncope, but there is a stronger tendency for gaze to be directed to one side. A blue facial color can occur in both epileptic seizures and cardiac syncope, but is unlikely to be observed in reflex syncope.64,72 Other important clues to an epileptic etiology are a lateral tongue bite,64 a pronounced head deviation,73 and emission of a cry at the beginning of an attack. Recovery after an epileptic seizure can be slow, and disorientation and confusion can persist for an extended period.24
In rare cases, epileptic seizures can cause syncope through asystole,74 and, conversely, cerebral hypoperfusion in syncope can occasionally induce an epileptic seizure, particularly in children.75 In either case the dual nature of an attack will only be recognized if it differs from previous attacks in the same patient.
Functional TLOC
In somatization and conversion disorders, patients exhibit somatic symptoms that have no somatic explanation, but for which a psychological mechanism is thought to be present.76,77,78 These disorders often occur in the context of prior psychological problems, physical abuse and/or sexual abuse.79 Attacks occur much more often in women than in men, and are more prevalent in young than in old individuals. Few formal psychiatric studies have been aimed at these disorders.80,81 The word 'functional' is beginning to replace terms such as 'psychogenic', which are considered offensive by some patients because of the implication that the condition is 'all in the head'.82,83
Pseudo-epilepsy is a type of functional TLOC that resembles epileptic seizures. 'Psychogenic nonepileptic seizures' (PNES) is one of the more common names for these attacks. In tertiary epilepsy clinics, up to 20% of all patients might have PNES. The attacks differ in a number of ways from epileptic seizures; for example, tongue biting and incontinence are rare in pseudoseizures.84 Trauma is thought to occur less often in pseudo-epilepsy than in epilepsy, but might nevertheless be observed in over 50% of cases.79,85 Alternating movements of the limbs, an 'arc de cercle', and pelvic thrusting can occur.85 Movements can change in nature, as well as wax and wane in severity, during an attack. The eyes are almost always closed, in contrast to both syncope and epileptic seizures. Eye closing is a very useful diagnostic feature if the patient is observed by trained personnel,86 but eyewitness accounts are, unfortunately, considerably less reliable.8,7,88 The features that help to distinguish epilepsy from psychogenic attacks might be too subtle to allow a certain diagnosis to be made by history taking, so the gold standard is a video-EEG recording of an attack.85,89 In many cases, functional attacks can be induced by verbal suggestion or various provocations for the purpose of video-EEG recording.89,90
The second type of functional TLOC, pseudosyncope, is not characterized by jerks. In two studies, such attacks accounted for 6% of presumed syncope episodes,91,92 and other studies have suggested even higher proportions.93 The trigger pattern in pseudosyncope is often unclear. Attacks can occur while the patient is lying down, can last many minutes, and can recur dozens of times in a day. The eyes are closed during the attack. Recovery can be slow, and weeping might occur. Attacks of pseudosyncope can be provoked with a tilt table test, and the absence of low blood pressure and/or of a low heart rate during an attack rules out syncope. As a result, functional TLOC is one of the few forms of conversion disorder in which diagnostic certainty can be reached.82,83,85,93
Rare causes and TLOC mimics
In vertebrobasilar transient ischemic attacks (TIAs), loss of consciousness can occur in combination with brainstem signs; that is, limb paresis, ataxia, diplopia, and problems with swallowing and speech.94 Loss of consciousness has not been observed in the absence of focal neurological signs in TIA,94 and the same holds for the subclavian steal phenomenon.95,96 Carotid TIAs are generally characterized by focal neurological deficits without unconsciousness, the only exception seeming to be cases in which almost all the arteries supplying the brain are occluded, with unconsciousness occurring as a result of a perfusion problem in the remaining arteries.97 In general, loss of consciousness is so rare in the context of TIA that TLOC and TIA are not normally considered in one another's differential diagnoses.
Cataplexy, a TLOC mimic, is characterized by muscle atonia leading to falls, and can be elicited by laughter, telling a joke, unexpectedly meeting with a friend, or by other, rarer triggers.98,99 Patients with cataplexy often have some residual muscle control, and so are able to break their fall. Consciousness is preserved, so the patient is not amnesic for the event. Cataplexy can, however, progress into sleep, so patients might not remember the end of the attack. If excessive daytime sleepiness is also present, a diagnosis of narcolepsy is virtually certain. Cataplexy has often been mistaken for complex partial and tonic–clonic seizures,100,101 as well as for reflex syncope.102
The term 'drop attacks' is confusing, as it has been used not only to describe falls in Menière disease or in atonic epileptic seizures, but also to describe any type of sudden fall. A specific form of drop attack was described in 1973:103 middle-aged women, or, in rare cases men, were reported to suddenly fall to the floor and commonly land on their knees and hands. As patients remembered hitting the floor, there was, presumably, no loss of consciousness. The cause of the type of drop attack described in the 1973 report is unknown.
Differential diagnosis
Initial approach
The diagnosis of TLOC often rests on a combination of clues rather than on one or two elements.88 Detailed accounts of several attacks from patients and eyewitnesses might be needed to unearth these clues. Given the importance of triggering, a crucial question to ask is “what were you doing at the time?”. If syncope is a possibility, the physical examination should include heart auscultation, orthostatic blood pressure recording and an electrocardiogram. The sensitivity of these measures might be low, but so is their cost. Listing of antecedent disorders and medication is obligatory. Ancillary investigations should focus on the most probable causes, as a shotgun approach targeting all possible causes is costly and inefficient.1 The yield of the initial evaluation of syncope differs between studies, depending largely on the diagnostic criteria used;72 estimates for a correct diagnosis in reflex syncope range from 34–63%.72 In a study assessing the European Society of Cardiology syncope guidelines,12,13 the initial assessment resulted in 63% of cases with a highly likely diagnosis (>80% certainty).92
If no clues are present other than brief loss of consciousness, a diagnosis more detailed than 'TLOC' or 'syncope' might not be possible. Evaluation should then be directed towards those causes that carry the greatest risk, namely, cardiac syncope, probably followed by epilepsy.
Age and setting
The various causes of TLOC differ with age: several specific forms of TLOC exist in children, including the so-called 'breath-holding spells'—a misnomer, because the attacks are not due to the child voluntarily holding their breath. The incidence of reflex syncope initially peaks at 13–16 years, at which age psychogenic TLOC can also occur. Cardiac syncope is very rare in children, although the hereditary prolonged QT syndrome does occur (estimated annual incidence in children 1 in 10,000–15,000).104 Reflex syncope is rarer between the ages of 35 and 60 years than at other ages. In people over 60 years of age, cardiac syncope and orthostatic hypotension are common causes of TLOC, and reflex syncope also reaches its second peak in this age group. Unfortunately, for reasons that are not entirely certain, history taking is a much less reliable approach for distinguishing different forms of TLOC in the elderly than in younger individuals. Epilepsy has a bimodal distribution, with the first peak occurring in early childhood, and a second peak, largely attributable to stroke and tumors, occurring in the elderly population.105,106,107 The overall annual incidence of unprovoked seizures is about 55 per 100,000, and the annual incidence of recurrent seizures (epilepsy) is about 32 per 100,000.105,106
The theoretical likelihood of any particular cause of TLOC depends on the setting: a general practice would expect to be presented with less harmful forms of TLOC than a hospital. Syncope is commonly encountered in the emergency room, and estimates are fairly stable across countries, at around 1% of all visits.108 In the few studies that have attempted to calculate the relative frequencies of syncope and epilepsy in the emergency room, estimates, as expressed as percentages of all types of TLOC, have ranged from 33% to 88% for syncope, and from 5% to 53% for epilepsy.10,109,110,111 The large ranges suggest bias in one or more of the studies.
Conclusions
Prospective validation will be required to determine whether the classification of and approach to TLOC described in this article will improve patient care. A blinkered approach focusing on only one cause of TLOC, be it epilepsy or cardiac syncope, will inevitably result in false or missing diagnoses. In epilepsy in particular, numerous examples exist in which a lack of knowledge of simple facts such as 'not all that jerks is epilepsy' has produced a false diagnosis. Epilepsy experts consider a false diagnosis to be very harmful, however, and tend to withhold diagnosis and treatment until they are certain.112,113
Appropriate care for TLOC requires a cooperative effort rather than successive independent investigations by various specialists. The nature of the specialty that takes overall responsibility for this care is less important than the willingness to cooperate with and learn from other specialties.
Review criteria
The references were obtained in part through work by two of the authors (J. G. van Dijk and W. Wieling) on the Task Force on Syncope of the European Society of Cardiology, which at present is preparing an update of the guidelines on syncope based on formal literature selection criteria. In that context, J. G. van Dijk and W. Wieling were primarily responsible for sections on pathophysiology, classification, orthostatic hypotension, epilepsy, and functional transient loss of consciousness. Additional material was obtained from the authors' own archives, supplemented by PubMed searches, using terms describing the various groups of transient loss of consciousness, to acquire recent data and to provide readers with relevant introductions or reviews.
References
Landau, W. M. & Nelson, D. A. Clinical neuromythology XV. Feinting science: neurocardiogenic syncope and collateral vasovagal confusion. Neurology 46, 609–618 (1996).
Josephson, C. B., Rahey, S. & Sadler, R. M. Neurocardiogenic syncope: frequency and consequences of its misdiagnosis as epilepsy. Can. J. Neurol. Sci. 34, 221–224 (2007).
Carreño, M. Recognition of nonepileptic events. Semin. Neurol. 28, 297–304 (2008).
Chowdhury, F. A., Nashef, L. & Elwes, R. D. Misdiagnosis in epilepsy: a review and recognition of diagnostic uncertainty. Eur. J. Neurol. 15, 1034–1042 (2008).
Colman, N. et al. Epidemiology of reflex syncope. Clin. Auton. Res. 14 (Suppl. 1), 9–17 (2004).
Ganzeboom, K. S., Colman, N., Reitsma, J. B., Shen, W. K. & Wieling, W. Prevalence and triggers of syncope in medical students. Am. J. Cardiol. 15, 1006–1008 (2003).
Ganzeboom, K. S. et al. Lifetime cumulative incidence of syncope in the general population: a study of 549 Dutch subjects aged 35–60 years. J. Cardiovasc. Electrophysiol. 17, 1172–1176 (2006).
van Dijk, J. G. Explaining syncope: faints need not confuse. Europace 7, 392–395 (2005).
van Dijk, J. G. & Fitzpatrick, A. P. What is syncope and what is not syncope: the importance of definitions. In The Evaluation and Treatment of Syncope. A Handbook for Clinical Practice 2nd edn (Eds Benditt, D. G., Blanc, J. J., Brignole, M. & Sutton, R.) 10–15 (Wiley-Blackwell, Oxford 2006).
Thijs, R. D., Granneman, E., Wieling, W. & van Dijk, J. G. Terms in use for transient loss of consciousness in the emergency ward; an inventory [Dutch]. Ned. Tijdschr. Geneeskd. 149, 1625–1630 (2005).
Thijs, R. D. et al. Unconscious confusion—a literature search for definitions of syncope and related disorders. Clin. Auton. Res. 15, 35–39 (2005).
Brignole, M. et al. Guidelines on management (diagnosis and treatment) of syncope. Eur. Heart J. 22, 1256–1306 (2001).
The Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope—update 2004. Europace 6, 467–537 (2004).
Thijs, R. D., Wieling, W., Kaufmann, H. & van Dijk, J. G. Defining and classifying syncope. Clin. Auton. Res. 14 (Suppl. 1), 4–8 (2004).
Jhanjee, R., van Dijk, J. G., Sakaguchi, S. & Benditt, D. G. Syncope in adults: terminology, classification, and diagnostic strategy. Pacing Clin. Electrophysiol. 29, 1160–1169 (2006).
Posner, J. B., Saper, C. B., Schiff, N. & Plum, F. Plum and Posner's Diagnosis of Stupor and Coma 4th edn (Oxford University Press, New York, 2007).
Bloem, R., Overeem, S. & van Dijk, J. G. Syncopal falls, drop attacks and their mimics. In Clinical Disorders of Balance, Posture and Gait 2nd edn (Eds Bronstein, A. M., Brandt, T., Woollacott, M. J. & Nutt, J. G.) 287–316 (Hodder Arnold, London, 2004).
Rossen, R., Kabat, H. & Anderson, J. P. Acute arrest of cerebral circulation in man. Arch. Neurol. Psychiatry 50, 510–528 (1943).
Lempert, T., Bauer, M. & Schmidt, D. Syncope: a videometric analysis of 56 episodes of transient cerebral hypoxia. Ann. Neurol. 36, 233–237 (1994).
Lempert, T. & von Brevern, M. The eye movements of syncope. Neurology 46, 1086–1088 (1996).
Stephenson, J. B. P. Fits and Faints (MacKeith Press, Oxford, 1990).
Lin, J. T., Ziegler, D. K., Lai, C. W. & Bayer, W. Convulsive syncope in blood donors. Ann. Neurol. 11, 525–528 (1982).
Newman, B. H. & Graves, S. A study of 178 consecutive vasovagal syncopal reactions from the perspective of safety. Transfusion 41, 1475–1479 (2001).
Hoefnagels, W. A., Padberg, G. W., Overweg, J., van der Velde, E. A. & Roos, R. A. Transient loss of consciousness: the value of the history for distinguishing seizure from syncope. J. Neurol. 238, 39–43 (1991).
Romme, J. J. et al. Influence of age and gender on the occurrence and presentation of reflex syncope. Clin. Auton. Res. 18, 127–133 (2008).
Benbadis, S. R., Wolgamuth, B. R., Goren, H., Brener, S. & Fouad-Tarazi, F. Value of tongue biting in the diagnosis of seizures. Arch. Intern. Med. 155, 2346–2349 (1995).
Serletis, A., Rose, S., Sheldon, A. G. & Sheldon, R. S. Vasovagal syncope in medical students and their first-degree relatives. Eur. Heart J. 27, 1965–1970 (2006).
Olde Nordkamp, L. R., Wieling, W., Zwinderman, A. H., Wilde, A. A. & van Dijk, N. Genetic aspects of vasovagal syncope: a systematic review of current evidence. Europace 11, 414–420 (2009).
Sheldon, R. S. et al. Age of first faint in patients with vasovagal syncope. J. Cardiovasc. Electrophysiol. 17, 49–54 (2006).
Alboni, P., Alboni, M. & Bertorelle, G. The origin of vasovagal syncope: to protect the heart or to escape predation? Clin. Auton. Res. 18, 170–178 (2008).
van Dijk, J. G. Fainting in animals. Clin. Auton. Res. 13, 247–255 (2003).
van Dijk, J. G. & Sheldon, R. Is there any point to vasovagal syncope? Clin. Auton. Res. 18, 167–169 (2008).
Hainsworth, R. Pathophysiology of syncope. Clin. Auton. Res. 14 (Suppl. 1), 18–24 (2004).
Verheyden, B. et al. Steep fall in cardiac output is main determinant of hypotension during drug-free and nitroglycerine-induced orthostatic vasovagal syncope. Heart Rhythm 5, 1695–1701 (2008).
Gracie, J., Newton, J. L., Norton, M., Baker, C. & Freeston, M. The role of psychological factors in response to treatment in neurocardiogenic (vaovagal) syncope. Europace 8, 636–643 (2006).
Fucà, G. et al. The venous system is the main determinant of hypotension in patients with vasovagal syncope. Europace 8, 839–845 (2006).
Verheyden, B. et al. Impact of age on the vasovagal response provoked by sublingual nitroglycerine in routine tilt testing. Clin. Sci. (Lond.) 113, 329–337 (2007).
Krediet, C. T., Wilde, A. A., Wieling, W. & Halliwill, J. R. Exercise related syncope, when it's not the heart. Clin. Auton. Res. 14 (Suppl. 1), 25–36 (2004).
Kerr, S. R., Pearce, M. S., Brayne, C., Davis, R. J. & Kenny, R. A. Carotid sinus hypersensitivity in asymptomatic older persons: implications for diagnosis of syncope and falls. Arch. Intern. Med. 166, 515–520 (2006).
Parry, S. W., Steen, N., Bexton, R., Tynan, M. & Kenny, R. A. Pacing in elderly recurrent fallers with carotid sinus hypersensitivity: a randomised, double-blind, placebo controlled cross-over trial. Heart 95, 405–409 (2009).
van Dijk, N. et al. Clinical factors associated with quality of life in patients with transient loss of consciousness. J. Cardiovasc. Electrophysiol. 17, 998–1003 (2006).
van Dijk, N. et al. Quality of life within one year following presentation after transient loss of consciousness. Am. J. Cardiol. 100, 672–676 (2007).
Ross, R., Parry, S., Norton, M. & Newton, J. L. Self-reported symptom burden; outcome in 418 patients from the Newcastle Vasovagal (Neurocardiogenic) cohort. QJM 101, 127–135 (2008).
Ammirati, F. et al. Management of syncope: clinical and economic impact of a Syncope Unit. Europace 10, 471–476 (2008).
Kaufmann, H. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multiple system atrophy. Clin. Auton. Res. 6, 125–126 (1996).
Low, P. A. & Singer, W. Management of neurogenic orthostatic hypotension: an update. Lancet Neurol. 7, 451–458 (2008).
Lahrmann, H. et al. EFNS guidelines on the diagnosis and management of orthostatic hypotension. Eur. J. Neurol. 13, 930–936 (2006).
Robertson, D. The pathophysiology and diagnosis of orthostatic hypotension. Clin. Auton. Res. 18 (Suppl. 1), 2–7 (2008).
Naschitz, J. E. & Rosner, I. Orthostatic hypotension: framework of the syndrome. Postgrad. Med. J. 83, 568–574 (2007).
Freeman, R. Clinical Practice. Neurogenic orthostatic hypotension. N. Engl. J. Med. 358, 615–624 (2008).
Wieling, W. & Schatz, I. The consensus statement on the definition of orthostatic hypotension. A revisit after 13 years. J. Hypertension 27, 935–938 (2009).
Gehrking, J. A. et al. What is the minimum duration of head-up tilt necessary to detect orthostatic hypotension? Clin. Auton. Res. 15, 71–75 (2005).
Gibbons, C. H. & Freeman, R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology 67, 28–32 (2006).
Bleasdale-Barr, K. M. & Mathias, C. J. Neck and other muscle pains in autonomic failure: their association with orthostatic hypotension. J. R. Soc. Med. 91, 355–359 (1998).
Smith, G. D., Watson, L. P., Pavitt, D. V. & Mathias, C. J. Abnormal cardiovascular and catecholamine responses to supine exercise in human subjects with sympathetic dysfunction. J. Physiol. 484, 255–265 (1995).
Smith, G. D. & Mathias, C. J. Postural hypotension enhanced by exercise in patients with chronic autonomic failure. QJM 88, 251–256 (1995).
Wieling, W., Krediet, C. T., van Dijk, N., Linzer, M. & Tschakovsky, M. E. Initial orthostatic hypotension: review of a forgotten condition. Clin. Sci. (Lond.) 112, 157–165 (2007).
Podoleanu, C. et al. Lower limb and abdominal compression bandages prevent progressive orthostatic hypotension in elderly persons: a randomized single-blind controlled study. J. Am. Coll. Cardiol. 48, 1425–1432 (2006).
Soteriades, E. S. et al. Incidence and prognosis of syncope. N. Engl. J. Med. 347, 878–885 (2002).
Kannankeril, P. J. & Roden, D. M. Drug-induced long QT and torsade de pointes: recent advances. Curr. Opin. Cardiol. 22, 39–43 (2007).
Meyer, J. S., Mehdirad, A., Salem, B. I., Kulikowska, A. & Kulikowski, P. Sudden arrhythmia death syndrome: importance of the long QT syndrome. Am. Fam. Physician 68, 483–488 (2003).
Vohra, J. The long QT syndrome. Heart Lung Circ. 16 (Suppl. 3), S5–S12 (2007).
Alboni, P. et al. Diagnostic value of history in patients with syncope with or without heart disease. J. Am. Coll. Cardiol. 37, 1921–1928 (2001).
Sheldon, R. et al. Diagnostic criteria for vasovagal syncope based on a quantitative history. Eur. Heart J. 27, 344–350 (2006).
Wieling, W., Krediet, C. T. & Wilde, A. A. Flush after syncope: not always an arrhythmia. J. Cardiovasc. Electrophysiol. 17, 804–805 (2006).
So, N. K. Atonic phenomena and partial seizures. A reappraisal. Adv. Neurol. 67, 29–39 (1995).
Trenité, D. G. Photosensitivity, visually sensitive seizures and epilepsies. Epilepsy Res. 70 (Suppl. 1), S269–S279 (2006).
Bakker, M. J., van Dijk, J. G., van den Maagdenberg, A. M. & Tijssen, M. A. Startle syndromes. Lancet Neurol. 5, 513–524 (2006).
Tibussek, D., Wohlrab, G., Boltshauser, E. & Schmitt, B. Proven startle-provoked epileptic seizures in childhood: semiologic and electrophysiologic variability. Epilepsia 47, 1050–1058 (2006).
Levine, E. et al. Congenital long QT syndrome: considerations for primary care physicians. Cleve. Clin. J. Med. 75, 591–600 (2008).
van Donselaar, C. A., Geerts, A. T. & Schimsheimer, R. J. Usefulness of an aura for classification of a first generalized seizure. Epilepsia 31, 529–535 (1990).
Colman, N. et al. Diagnostic value of history taking in reflex syncope. Clin. Auton. Res. 14 (Suppl. 1), 37–44 (2004).
Sheldon, R. et al. Historical criteria that distinguish syncope from seizures. J. Am. Coll. Cardiol. 40, 142–148 (2002).
Ghearing, G. R., Munger, T. M., Jaffe, A. S., Benarroch, E. E. & Britton, J. W. Clinical clues for detecting ictal asystole. Clin. Auton. Res. 17, 221–226 (2007).
Horrocks, I. A., Nechay, A., Stephenson, J. B. & Zuberi, S. M. Anoxic-epileptic seizures: observational study of epileptic seizures induced by syncopes. Arch. Dis. Child. 90, 1283–1287 (2005).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR Fourth Edition (Text Revision) 4th edn (American Psychiatric Publishing, Inc., Arlington, VA, 2000).
Kroenke, K., Sharpe, M. & Sykes, R. Revising the classification of somatoform disorders: key questions and preliminary recommendations. Psychosomatics 48, 277–285 (2007).
Kroenke, K. & Rosmalen, J. G. Symptoms, syndromes, and the value of psychiatric diagnostics in patients who have functional somatic disorders. Med. Clin. North Am. 90, 603–626 (2006).
Reuber, M., Howlet, S., Khan, A. & Grünewald, R. A. Non-epileptic seizures and other functional neurological symptoms: predisposing, precipitating, and perpetuating factors. Psychosomatics 48, 230–238 (2007).
Strassnig, M., Stowell, K. R., First, M. B. & Pincus, H. A. General medical and psychiatric perspectives on somatoform disorders: separated by an uncommon language. Curr. Opin. Psychiatry 19, 194–200 (2006).
Benbadis, S. R. The problem of psychogenic symptoms: is the psychiatric community in denial? Epilepsy Behav. 6, 9–14 (2005).
Reuber, M., Mitchell, A. J., Howlett, S. J., Crimlisk, H. L. & Grünewald, R. A. Functional symptoms in neurology: questions and answers. J. Neurol. Neurosurg. Psychiatry 76, 307–314 (2005).
Stone, J. et al. What should we call pseudoseizures? The patient's perspective. Seizure 12, 568–572 (2003).
Oliva, M. et al. The diagnostic value of oral lacerations and incontinence during convulsive 'seizures'. Epilepsia 49, 962–967 (2008).
LaFrance, W. C. Jr. Psychogenic nonepileptic seizures. Curr. Opin. Neurol. 21, 195–201 (2008).
Chung, S. S., Gerber, P. & Kirlin, K. A. Ictal eye closure is a reliable indicator for psychogenic nonepileptic seizures. Neurology 66, 1730–1731 (2006).
Syed, T. U. et al. Do observer and self-reports of ictal eye closure predict psychogenic nonepileptic seizures? Epilepsia 49, 898–904 (2008).
Thijs, R. D., Wagenaar, W. A., Middelkoop, H. A., Wieling, W. & van Dijk, J. G. Transient loss of consciousness through the eyes of a witness. Neurology 71, 1713–1718 (2008).
Zaidi, A., Crampton, S., Clough, P., Fitzpatrick, A. & Scheepers, B. Head-up tilting is a useful provocative test for psychogenic non-epileptic seizures. Seizure 8, 353–355 (1999).
Ribaï, P., Tugendhaft, P. & Legros, B. Usefulness of prolonged video-EEG monitoring and provocative procedure with saline injection for the diagnosis of nonepileptic seizures of psychogenic origin. J. Neurol. 253, 328–332 (2006).
Petersen, M. E., Williams, T. R. & Sutton, R. Psychogenic syncope diagnosed by prolonged head-up tilt testing. QJM 88, 209–213 (1995).
van Dijk, N. et al. High diagnostic yield and accuracy of history, physical examination, and ECG in patients with transient loss of consciousness in FAST: the Fainting Assessment study. J. Cardiovasc. Electrophysiol. 19, 48–55 (2008).
Benbadis, S. R. & Chichkova, R. Psychogenic pseudosyncope: an underestimated and provable diagnosis. Epilepsy Behav. 9, 106–110 (2006).
Savitz, S. I. & Caplan, L. R. Vertebrobasilar disease. N. Engl. J. Med. 352, 2618–2626 (2005).
Hennerici, M., Klemm, C. & Rautenberg, W. The subclavian steal phenomenon: a common vascular disorder with rare neurologic deficits. Neurology 38, 669–673 (1988).
Taylor, C. L., Selman, W. R. & Ratchson, R. A. Steal affecting the central nervous system. Neurosurgery 50, 679–689 (2002).
Stark, R. J. & Wodak, J. Primary orthostatic cerebral ischaemia. J. Neurol. Neurosurg. Psychiatry 46, 883–891 (1983).
American Academy of Sleep Medicine. The International Classification of Sleep Disorders. Diagnostic and Coding Manual 2nd edn (American Academy of Sleep Medicine, Westchester, Illinois, 2005).
Overeem, S., Mignot, E., van Dijk, J. G. & Lammers, G. J. Narcolepsy: clinical features, new pathophysiological insights, and future perspectives. J. Clin. Neurophysiol. 18, 78–105 (2001).
Macleod, S., Ferrie, C. & Zuberi, S. M. Symptoms of narcolepsy in children misinterpreted as epilepsy. Epileptic Disord. 7, 13–17 (2005).
Zeman, A., Douglas, N. & Aylward, R. Lesson of the week: narcolepsy mistaken for epilepsy. BMJ 322, 216–218 (2001).
Calabrò, R. S. et al. Status cataplecticus misdiagnosed as recurrent syncope. Neurol. Sci. 28, 336–338 (2007).
Stevens, D. L. & Matthews, W. B. Cryptogenic drop attacks: an affliction of women. BMJ 1, 439–442 (1973).
Friedman, M. J., Mull, C. C., Sharieff, G. Q. & Tsarouhas, N. Prolonged QT syndrome in children: an uncommon but potentially fatal entity. J. Emerg. Med. 24, 173–179 (2003).
Kotsopoulos, I. et al. Incidence of epilepsy and predictive factors of epileptic and non-epileptic seizures. Seizure 14, 175–182 (2005).
Olafsson, E. et al. Incidence of unprovoked seizures and epilepsy in Iceland and assessment of the epilepsy syndrome classification: a prospective study. Lancet Neurol. 4, 627–634 (2005).
Sillanpää, M., Kälviäinen, R., Klaukka, T., Helenius, H. & Shinnar, S. Temporal changes in the incidence of epilepsy in Finland: nationwide study. Epilepsy Res. 71, 206–215 (2006).
Olde Noordkamp, L. R. et al. Syncope prevalence in the ED compared to that in the genral practice and population: a strong selection process. Am. J. Emergency Med. 27, 271–279 (2009).
Martikainen, K. et al. Transient loss of consciousness with and without injuries: where to treat these patients? Eur. J. Gen. Pract. 9, 91–95 (2003).
Martikainen, K. et al. Transient loss of consciousness as reason for admission to primary health care emergency room. Scand. J. Prim. Health Care 21, 61–64 (2003).
Bartoletti, A. et al. Physical injuries caused by a transient loss of consciousness: main clinical characteristics of patients and diagnostic contribution of carotid sinus massage. Eur. Heart J. 29, 618–624 (2008).
Gilbert, D. L., Sthuraman, G., Kotagal, U. & Buncher, R. Meta-analysis of EEG test performance shows wide variation among studies. Neurology 60, 564–570 (2002).
van Donselaar, C. A., Stroink, H., Arts, W. F. & Dutch Study Group of Epilepsy in Childhood. How confident are we of the diagnosis of epilepsy? Epilepsia 47 (Suppl. 1), 9–13 (2006).
Acknowledgements
The authors are indebted to Ley Sander and Wil Hoefnagels for helpful comments on the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
van Dijk, J., Thijs, R., Benditt, D. et al. A guide to disorders causing transient loss of consciousness: focus on syncope. Nat Rev Neurol 5, 438–448 (2009). https://doi.org/10.1038/nrneurol.2009.99
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2009.99
This article is cited by
-
Vagal sensory neurons mediate the Bezold–Jarisch reflex and induce syncope
Nature (2023)
-
Calgary score and modified calgary score in the differential diagnosis between syncope and genetic generalized epilepsy in children
Scientific Reports (2023)
-
Diagnostic and societal impact of implementing the syncope guidelines of the European Society of Cardiology (SYNERGY study)
BMC Medicine (2023)
-
Recommendations for tilt table testing and other provocative cardiovascular autonomic tests in conditions that may cause transient loss of consciousness
Clinical Autonomic Research (2021)
-
Classification of orthostatic intolerance through data analytics
Medical & Biological Engineering & Computing (2021)