Key Points
-
Meningiomas are the most common primary intracranial tumours found in adults
-
Meningiomas can have an aggressive course characterized by local progression and, infrequently, metastasis to other organs, even when treated with surgery and radiotherapy
-
Key genetic and epigenetic alterations have been identified in meningiomas that strongly associate with clinicopathologic features, such as localization and prognosis, and could represent targets for drug treatment
-
Prospective clinical trials are evaluating novel drugs on the basis of advances in the understanding of the pathobiology of treatment-resistant meningiomas
Abstract
Meningiomas currently are among the most frequent intracranial tumours. Although the majority of meningiomas can be cured by surgical resection, ∼20% of patients have an aggressive clinical course with tumour recurrence or progressive disease, resulting in substantial morbidity and increased mortality of affected patients. During the past 3 years, exciting new data have been published that provide insights into the molecular background of meningiomas and link sites of tumour development with characteristic histopathological and molecular features, opening a new road to novel and promising treatment options for aggressive meningiomas. A growing number of the newly discovered recurrent mutations have been linked to a particular clinicopathological phenotype. Moreover, the updated WHO classification of brain tumours published in 2016 has incorporated some of these molecular findings, setting the stage for the improvement of future therapeutic efforts through the integration of essential molecular findings. Finally, an additional potential classification of meningiomas based on methylation profiling has been launched, which provides clues in the assessment of individual risk of meningioma recurrence. All of these developments are creating new prospects for effective molecularly driven diagnosis and therapy of meningiomas.
Similar content being viewed by others
Introduction
Meningiomas are tumours of the meninges — the tissue layers that cover the brain or spinal cord. These tumours arise primarily from meningothelial arachnoid cells, but they can also occur rarely as primary tumours in other localizations, such as within the ventricles of the CNS or even in extracranial organs such as the lungs. The natural development of arachnoid cells is complex, as these cells have different embryonic origins depending on their location — that is, the meninges covering the convexity of the brain have a different origin from those at the skull base. This difference affects not only the predominating histological subtypes of meningiomas that arise from these cells but also the distribution of recurrent somatic mutations.
Currently, meningiomas are among the most common intracranial tumours, with an estimated incidence of 7.86 cases per 100,000 people per year. Approximately 80% of cases are of benign histology and correspond to grade I according to the current WHO classification, whereas up to 20% of cases show signs of increased malignancy at histology and correspond to grade II or grade III meningiomas1. The majority (∼90%) of meningiomas are located intracranially, but 10% are found in the spinal meninges2. Meningiomas primarily occur in elderly individuals, with increased incidence in individuals older than 65 years of age2. These tumours are exceedingly rare in childhood (representing 0.4–4.1% of all paediatric tumours)3, and instances of paediatric meningiomas are strongly associated with germline alterations in the neurofibromin 2 (NF2) gene. Thus, diagnosis of a meningioma in a child should prompt a screen for clinical signs of NF2 mutations4,5. The incidence of meningiomas is increasing among adolescents and young adults, and these tumours now represent ∼16% of all intracranial tumours in people 15–39 years of age6. Meningiomas of adulthood preferentially affect women, with a female:male ratio of 3.5:1, whereas paediatric meningiomas are nearly equally distributed7. Other risk factors for meningiomas include ionizing radiation8, diabetes mellitus, arterial hypertension and (possibly) smoking, although data are conflicting regarding this last factor9,10. By contrast, despite some speculation, mobile phone use has not been associated with increased meningioma development11. Radiation-induced meningiomas tend to present as multiple tumours with aggressive histological features and are characterized by an aggressive clinical course, including frequent tumour recurrence12. Allergy seems to be associated with a reduced meningioma risk. Conversely, the presence of progesterone receptors in meningiomas and the high incidence of these tumours in women who have hormone-related conditions (for example, endometriosis or breast cancer) or who use exogenous hormones could indicate an endocrine influence on the pathogenesis of meningioma13,14. However, despite strong evidence for a relevant hormonal aspect in meningioma growth, antihormonal treatment attempts have been disappointing15.
Between 70 and 80% of meningiomas can be cured by surgical resection. However, one of the most relevant prognostic factors of meningiomas is the extent of resection (as assessed by the Simpson grading scale), with incomplete resection conferring a major risk of meningioma regrowth16,17,18. Meningiomas that are in surgically inaccessible locations, are incompletely resected and/or have features of aggressive histology (WHO grade II and III) tend to grow progressively or recur, and thereby pose a therapeutic challenge. Radiotherapy is usually recommended for recurrent meningiomas after initial surgical resection and is administered either as monotherapy or as adjuvant therapy after re-resection19. The role of radiotherapy in the first-line treatment of atypical meningiomas (that is, aggressive WHO grade II tumours characterized by increased proliferation and mitotic activity, cellular atypia and/or invasion of brain tissue) has been the subject of discussion, especially following complete resection of the tumour. The question of whether adjuvant radiotherapy or a wait-and-see strategy should be recommended is currently being addressed by the ROAM/EORTC-1308 trial (ISRCTN71502099)20, which is recruiting patients in the UK and Europe. For malignant (WHO grade III) meningiomas, surgery followed by adjuvant radiotherapy is recommended and improves 5-year progression-free survival from 15% to 80%21.
However, most patients with recurrent disease exhaust all surgical and radiotherapeutic options at some point in their disease course and become candidates for systemic therapies22. A meta-analysis of 47 publications that reported various treatment options in meningioma concluded that progression-free survival at 6 months (PFS-6) was the best marker of treatment efficacy to be used as a benchmark for clinical trials for the comparison of different treatment types. The PFS-6 was 29% for grade I meningiomas and 26% for WHO grade II and grade III meningiomas. A PFS-6 greater than 40% for tumours of WHO grade I and greater than 30% for WHO grade II and grade III meningiomas would indicate treatment efficacy18. Unfortunately, no effective drugs have been identified to date for the treatment of aggressive meningiomas18,23.
In the past few years, advances in the molecular characterization of meningioma have enabled the identification of recurring genetic alterations that are promising treatment targets. Moreover, research has also identified genetic alterations that are responsible for an increased likelihood of tumour recurrence. Together with the new WHO classification of brain tumours published in 2016 (Ref. 24), in which molecular findings have been substantially integrated into the view on meningioma biology, the stage has now been set to improve future therapeutic efforts by applying these essential molecular findings. Here, we summarize new developments and ongoing efforts towards molecularly driven therapies of meningioma.
Histopathological classification
One of the most intriguing characteristics of meningiomas is the diversity of their histological and biological features, as indicated by the 15 different subtypes listed in the current WHO classification of brain tumours (Table 1). Moreover, different histological features can co-occur in a large fraction of tumours, resulting in difficulties in correctly categorizing tumours. The WHO classification lists nine variants of meningiomas that correspond to grade I — that is, tumours with a slow growth rate and benign biological behaviour. Among the grade I meningiomas, which represent ∼80% of all meningiomas, the meningothelial and fibroblastic variants are very common, whereas other variants, such as metaplastic or lymphoplasmacyte-rich meningioma, are exceptionally rare. The WHO grade II group comprises ∼15–20% of all meningiomas and consists of three variants that are characterized by aggressive biology with increased proliferation, nuclear pleomorphism and tumour necrosis. Highly aggressive malignant meningiomas (that is, anaplastic meningiomas), which are categorized as three subtypes of WHO grade III meningiomas, account for only 1–2% of all cases, have a poor clinical course and present a challenge for treatment25. Importantly, the introduction of the improved diagnostic criteria by the 2007 WHO classification26 resulted in an increased recognition of grade II meningiomas, including the recognition of brain-invasive tumours, and has resulted in the identification of a larger proportion of meningioma patients who have a high risk of tumour recurrence and, consequently, who need additional nonsurgical therapies27,28. Because some uncertainty still remains as to whether histopathological evaluation is the single best criterion for risk assessment in meningiomas29, the inclusion of the newly identified recurrent molecular alterations in the diagnostic assessment might further improve accuracy in the identification of meningioma patients who need close surveillance and more-aggressive treatment.
Genetic alterations
Copy-number alterations
Meningiomas generally have fewer copy-number alterations than do many other tumours of adulthood30. Although many grade I meningiomas are not characterized by recurrent copy-number alterations, a small subset of these tumours harbour complex genomic rearrangements, such as chromothripsis30. Higher meningioma grade is associated with the observation of higher rates of copy-number alterations and karyotypic abnormalities. As described in the next section, the most common cytogenetic alteration is loss of chromosome 22, which affects the NF2 gene31. Other cytogenetic abnormalities repeatedly described in meningiomas include losses of 1p, 6q, 9p, 10, 14q, 18q and 19 (Ref. 26).
Mutations
Neurofibromin 2. The first identification of a specific genetic aetiology of meningiomas was the discovery of alterations in the tumour suppressor gene NF2 (Refs 32,33), located on chromosome 22, which encodes the protein Merlin (also known as Schwannomin). Abnormalities in NF2 result in the familial syndrome neurofibromatosis 2, which is characterized by the development of benign tumours of the nervous system — primarily, schwannomas and meningiomas34. Most neurofibromatosis-associated meningiomas and more than half of sporadic meningiomas have alterations in NF235,36,37,38. Splice site, nonsense or frameshift mutations are the most common disruptors of NF2 and result in a truncated and nonfunctional protein. A two-hit mechanism of inactivation is usually observed in these meningiomas, in which NF2 is disrupted in one allele and loss of all or part of chromosome 22 occurs in the second allele30,39. Infrequently, NF2 inactivation is associated with other patterns of molecular alterations such as specific NF2 mutations on both alleles, mitotic recombinations or single or multiexon deletions. In a comparison of NF2-mutated and NF2-nonmutated meningiomas, overall chromosomal alterations were shown to be more frequent in NF2-mutated tumours, regardless of the histological grading. This finding suggests increased chromosomal instability in meningiomas with NF2 inactivation40.
Although the mechanisms by which inactivation of Merlin drives meningiomagenesis remain poorly understood, several hypotheses have been postulated. Merlin is a membrane–cytoskeleton linker that inhibits cell proliferation through contact-dependent regulation of various signalling pathways, including Hippo, Patched and Notch pathways41. Merlin also negatively regulates mammalian target of rapamycin complex 1 (mTORC1) and positively regulates the kinase activity of mTORC242,43, suggesting that Merlin has a role in the activation of the mammalian target of rapamycin (mTOR) pathway during meningioma development. Although in vitro data suggest that sensitivity to certain chemotherapeutical agents is modulated by NF2, the NF2 status of individual patients has not been systematically assessed in clinical studies44. Interestingly, sensitivity of NF2-altered tumours to inhibition of focal adhesion kinase (FAK) has been reported in other tumours; consequently, FAK inhibition could present a therapeutic opportunity for meningiomas carrying NF2 aberrations45,46.
Emerging mutational patterns. Whereas about half of sporadic meningiomas harbour NF2 alterations, the remaining NF2-nonmutated tumours clearly must be driven by other genetic aberrations. The introduction of next-generation sequencing technologies has revolutionized our understanding of the genetic underpinnings of sporadic meningiomas by uncovering a number of novel putative genetic drivers in certain subsets of meningiomas. In one landmark study, 65 meningiomas (47 grade I and 18 grade II or III) underwent massive parallel sequencing with whole-genome, whole-exome or targeted sequencing. NF2 inactivation was reported in 43% of the tumours, supporting a key role for this gene in meningioma development. Alterations affecting epigenetic modifiers were present in 8% of tumours, including mutations in KDM5C, KDM6A and SMARCB130. Alterations in SMARCB1, which is located on chromosome 22 in close proximity to NF2, have also been reported in other studies of meningiomas47 and schwannomas48. Interestingly, a 2016 study confirmed the co-occurrence of recurrent SMARCB1 mutations in NF2-mutated meningiomas, raising the question of whether additional SMARCB1 alterations might accelerate the growth of meningioma cells49. A fraction of NF2-nonmutated meningiomas (which comprised 6 of 65 total tumours examined) harboured alterations in AKT1 (5 of 65) and mTOR (1 of 65), both of which are members of the phosphoinositide 3-kinase (PI3K)–AKT–mTOR pathway. A p.Glu17Lys mutation reported in AKT1 was found to be recurrent in an oncogenic hot spot and resulted in constitutive activation of AKT1 protein. The Akt1 p.Glu17Lys mutation possesses oncogenic potential because it enables cells to form colonies in soft agar and induces leukaemia in mice, which cannot be induced by wild-type AKT1 alone50. Notably, patients presenting with clinical features of the so-called Proteus syndrome, which is characterized by progressive overgrowth of various tissues in association with mosaicism of the somatic activating AKT1 p.Glu17Lys mutation, frequently develop meningiomas. One study detected somatic AKT1 p.Glu17Lys mutations in affected tissue samples from 52 of 61 patients presenting with clinical features of Proteus syndrome, and brain MRI showed that the most common tumour in the patients with this mutation was meningioma, which occurred in close anatomical relation to hyperostosis51. On the basis of these findings, researchers have suggested that some sporadic meningiomas are a microform of Proteus syndrome and that activation of the PI3K–AKT pathway drives the hyperostosis associated with meningioma.
A subsequent study investigated 50 WHO grade I and II meningiomas with whole-exome sequencing and 250 meningiomas with targeted sequencing and found that 13% (38 of 300) of meningiomas harboured the AKT1 p.Glu17Lys mutation52. Interestingly, targeted sequencing focusing on skull-base meningiomas identified AKT1 p.Glu17Lys mutations in ∼30% of patients53. Meningiomas with AKT1 p.Glu17Lys mutations have distinct gene expression patterns compared with NF2-mutant meningiomas52 and show immunohistochemical evidence of PI3K–AKT–mTOR pathway activation30. These data strongly point towards a relevant biological function of the AKT1 p.Glu17Lys mutation in NF2-nonmutated meningiomas.
In addition to recurrent AKT1 p.Glu17Lys mutations, 1–5% of meningiomas without alterations in NF2 and AKT1 harbour recurrent alterations in SMO, which encodes smoothened homologue, a member of the Hedgehog signalling pathway30,52,54,55. Skull-base meningiomas in particular are associated with an increased frequency of SMO mutations (28%)56. Two hotspot mutations affect the SMO gene in meningiomas — Leu412Phe and Trp535Leu, with Leu412Phe present at a much higher prevalence than Trp535Leu56. GRB2-associated-binding protein (GAB1) expression indicated activation of the Hedgehog pathway in 10% of meningiomas30, confirming results from previous studies that suggested Hedgehog pathway activation in a fraction of meningiomas on the basis of increased mRNA expression levels of various Hedgehog pathway genes57. Binding of Hedgehog ligands to protein patched homologue 1 (PTCH1) causes internalization and degradation of PTCH1, which attenuates PTCH1-mediated suppression of transmembrane SMO protein. SMO then interacts with suppressor of fused homologue (SUFU), which results in nuclear translocation of zinc-finger protein GLI1 (GLI1) and activation of target genes58. SMO is involved in both embryogenesis and several key cellular processes, including proliferation and angiogenesis. Gain-of-function mutations in SMO have been identified in several types of cancers, and a molecular subgroup of medulloblastomas has been identified with distinct clinicopathological characteristics defined by alterations in sonic hedgehog pathway signalling59. Notably, two of three patients with germline mutations in SUFU who were treated with radiotherapy for childhood medulloblastomas subsequently developed meningiomas in the radiation field, indicating an increased risk of radiation-induced secondary meningioma development in such patients60.
Another potentially important gene identified in meningiomas without an NF2 mutation is TRAF7, an E3 ubiquitin ligase that interacts with numerous signalling pathways (including MEKK3; also known as MAP3K3 (mitogen-activated protein kinase kinase kinase 3)) and induces apoptosis following overexpression61. The TRAF7 gene contains seven WD40 repeats in its carboxyl terminus61. TRAF7 mutations were found in up to one-quarter of WHO grade I and grade II meningiomas52,54,55. Interestingly, the majority of the mutations mapped to the WD40 domains, which are involved in the regulation of JUN N-terminal kinase (JNK) and p38 mitogen-activated protein kinase (MAPK) signalling, suggesting an important regulatory function of TRAF7 in meningiomas.
Recurrent mutations in KLF4 are also potential candidate drivers of WHO grade I meningiomas. KLF4 belongs to a large Kruppel-like factor gene family characterized by the presence of three Cys2–His2 zinc-finger motifs in the carboxy-terminal region. Members of this gene family are involved in transcriptional activation and repression, including oncogenic activation and tumour suppression62. Kruppel-like factors additionally act as key regulators in the reprogramming of somatic cells into induced pluripotent stem cells63. A hotspot mutation (KLF4 p.Lys409Gln) is present within the first zinc-finger domain of KLF4 at a location within the DNA-binding motif that makes direct contact in the major groove of DNA64. KLF4 mutations occur in up to 50% of NF2-nonmutated meningiomas52,53,54,65 and, most interestingly, have a high rate of co-occurrence with TRAF7 mutations52,65.
The frequent finding of AKT1 mutations in meningiomas, as well as previous data showing phosphorylation and activation of the AKT protein in meningiomas, strongly supports a deregulation of the PI3K signalling pathway in these tumours66,67. Indeed, a study of 150 meningiomas identified PIK3CA mutations in 7% of NF2-nonmutated cases55. All of these NF2-nonmutated tumours were graded as WHO grade I. The PIK3CA-mutant meningiomas lacked mutations in NF2, AKT1 and SMO, but they tended to harbour TRAF7 mutations. Lastly, a study aiming to identify oncogenic alterations in meningiomas — in the absence of any of the other previously mentioned mutations — found recurrent somatic mutations in POLR2A (encoding the DNA-directed RNA polymerase II subunit RPB1) in ∼6% of 775 meningiomas examined. POLR2A mutations did not coexist with any of the previously described meningioma driver mutations and tended to be associated with meningothelial histology and tumour location in the tuberculum sellae49. No POLR2A mutations were present in high-grade meningiomas. This study also confirmed that NF2-nonmutated benign meningiomas are genomically stable and do not exhibit large-scale chromosomal amplifications or deletions.
These studies have expanded our knowledge of the genetic basis of sporadic meningiomas. In addition, the fact that the vast majority of genetic alterations, except for NF2 mutations, affected WHO grade I meningiomas is intriguing30,52. To investigate this association, one study characterized the genetic landscape of primary (de novo) atypical meningiomas in detail and showed that NF2 alterations are the dominating molecular events (75%) in these aggressive tumours68. Of the remaining atypical meningiomas, 9% harboured TRAF7 or PI3K mutations, and 16% did not contain any of the mutations previously reported for WHO grade I meningiomas68. Owing to the finding that NF2-mutated atypical meningiomas are characterized by a hypermethylated phenotype, the researchers compared the molecular signature of methylated atypical meningiomas with benign meningiomas. Polycomb repressive complex 2 binding sites in human embryonic stem cells were differentially methylated in these tumours, indicating the presence of a primitive cellular state in hypermethylated atypical meningiomas68. Another important finding from this study is the lack of TERT promoter mutations in de novo atypical meningiomas, which is clearly in contrast to the reported occurrence of TERT promoter mutations in secondary atypical meningiomas that have progressed from grade I primary tumours69.
Clearly, molecular characterization of highly aggressive anaplastic meningiomas of WHO grade III is needed as molecular data for anaplastic meningiomas remain limited. However, data published recently have shown that NF2 alterations are the main finding in anaplastic grade II meningiomas70. A 2016 study characterized the molecular features of rhabdoid meningiomas (designated as WHO grade III tumours), which might aid our understanding of this rare subtype. The presence of considerable variation in the clinical course of patients diagnosed with a rhabdoid meningioma is well recognized and is at least partly caused by difficulties in the evaluation of rhabdoid features among individual pathologists71. Data have shown that the presence of a rhabdoid phenotype in the absence of other features of malignancy, such as high mitotic count and necroses, seems to define a clinical course comparable to WHO grade I meningiomas72. Identification of the frequent inactivation of BAP1 in rhabdoid meningiomas was an important step towards the separation of rhabdoid-appearing meningiomas into aggressive and less-aggressive tumour types73. BAP1 is a tumour suppressor gene that encodes a deubiquitylating enzyme (ubiquitin carboxyl-terminal hydrolase BAP1) that is mutated — frequently, on an inherited basis — in mesothelioma, uveal melanoma and renal cell cancer74. BAP1 mutations are more frequent in meningiomas with >50% rhabdoid cells, and a loss of BAP1 protein expression indicates early tumour recurrence. Consequently, BAP1 immunohistochemistry could be a promising tool for risk stratification in patients with rhabdoid meningiomas73.
As in other cancer types, future studies might be able to model the clonal evolution of meningiomas and the interplay of the various individual mutations found in these tumours31,75.
Genetics, histology and location
The emerging mutational patterns in meningiomas demonstrate the clear presence of distinct pathways for meningioma development. However, these findings can be understood fully only in the context of tumour localization and histological subtype. Differences in the histological subtypes that arise in various tumour sites can be attributed to differences in embryonic development, as meninges at the skull base are derived from the mesoderm, whereas telencephalic (that is, convexity) meninges are derived from the neural crest76. Consequently, meningothelial meningiomas are preferentially found at the skull base, whereas fibroblastic meningiomas occur mainly at the convexity of the brain77,78. Location might also be related to the grade of malignancy, as the proportion of grade II or grade III meningiomas at the convexity or with parasagittal location is much higher than that at the skull base, where grade I meningiomas dominate79. Meningiomas can occur at multiple sites; a population-based study revealed that multiple meningiomas were present in 1% (7 of 823) of patients with NF2 alterations and 4% (29 of 823) of patients without NF2 alterations80. In addition, NF2 alterations are associated with fibroblastic or transitional histology.
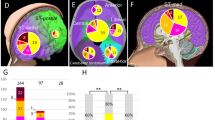
Meningiomas with recurrent AKT1 p.Glu17Lys mutations tend to have a skull-base or basal localization and are enriched for meningothelial histology30,53,56,81,82. SMO mutations predominate in the medial anterior skull base52 and, as with AKT1-mutated tumours, belong to the meningothelial subytype30,56,74. Meningothelial histology also dominates in POLR2A-mutated meningiomas49. Nearly all secretory meningiomas, which represent 3% of all meningiomas and are associated with peritumoural oedema, harbour recurrent mutations in KLF4 and TRAF7 (Refs 52,65). KLF4 mutations are specific to tumours with a secretory histology, whereas TRAF7 mutations can also occur in other meningioma histologies65. PIK3CA-mutant meningiomas showed mainly meningothelial or transitional histology and are preferentially localized at the skull base55. POLR2A-mutated grade I meningiomas are preferentially located at the tuberculum sellae region49. Higher-grade meningiomas (grade II and grade III tumours) have been reported to have TP53 mutations30 and loss of CDKN2A and CDKN2B40. Spinal cord meningiomas frequently show loss-of-function mutations in the SMARCE1 gene83. Interestingly, the presence of SMARCE1 mutations is strongly associated with clear cell histology in spinal cord and cranial meningiomas84. How the localization and histological subtype of meningioma affect potential treatment options is another question that needs to be addressed in future studies. Owing to the embryonic origin of arachnoidal cells in the encephalic meninges, the question whether the mesodermal or ectodermal origin of a meningeal tumour affects sensitivity to certain drugs remains unresolved. Figure 1 summarizes the relationship between localization, histological subtype and recurrent molecular alterations in meningiomas.
Tumour localization defines molecular characteristics and potential treatment options. Convexity meningiomas predominantly harbour NF2 and SMARCB1 alterations. Skull-base meningiomas are characterized by other recurrent mutations, including AKT1, SMO, KLF4, TRAF7 and POLR2A. Spinal cord meningiomas show frequent SMARCE1 mutations, whereas other recurrent mutations are rare in this localization. Most genes altered in meningiomas at the convexity or the skull base are essential drivers of key mitogenic pathways (phosphoinositide 3-kinase–AKT, mammalian target of rapamycin (mTOR) and extracellular-signal-regulated kinase (ERK)), and overexpression of tyrosine kinase receptors such as vascular endothelial growth factor receptor (VEGFR), platelet-derived growth factor receptor (PDGFR) or insulin-like growth factor receptor (IGFR) has been well characterized in these tumours. Consequently, several options for drug treatment of unresectable, recurrent and/or biologically aggressive high-grade meningiomas are currently under evaluation, such as tyrosine kinase inhibition, AKT inhibition and mTOR inhibition. Direct DNA targeting by trabectedin has shown promising in vitro results and is currently being investigated in a large clinical trial (EORTC-1320)20. mTORC, mTOR complex.
Genetics and prognosis
A number of studies have indicated that numerical and structural chromosome changes — including pronounced hypodiploidy or, rarely, hyperdiploidy75 — are accompanied by more-aggressive characteristics, most notably deletion of the short arm of chromosome 1. These results support the findings of former cytogenetic investigations, which indicated that the deletion of the distal part of the short arm of a chromosome 1 (1p) is associated with progression in meningiomas31,85,86,87.
Mutations in the TERT promoter have a clear effect on the prognosis of meningioma. Increased staining of telomerase reverse transcriptase (encoded by TERT) has been recognized in aggressive meningiomas88. More importantly, activating TERT promoter mutations are frequent in meningiomas with malignant histological progression89, and TERT promoter mutations were strongly associated with time to progression in a retrospective series of meningioma samples from 252 patients69. Mutations in the TERT promoter at the hotspot regions g.228C>T and g.250C>T were found in 6.4% of all cases in this retrospective series (1.7%, 5.7% and 20% of WHO grade I, II and III meningiomas, respectively). The median time to progression was 10.1 months in patients with TERT promoter mutations and 179 months in patients without a TERT promoter mutation. The prognostic effect of this alteration was independent from histological grade. Consequently, assessment of TERT promoter mutation status could be incorporated in future classification schemes if the prognostic role is validated in independent studies that also investigate the interaction of these mutations with overall survival times.
SMO-mutated meningiomas located in the olfactory groove region of the skull base that have meningothelial histology have been demonstrated to have considerably higher recurrence rates than do AKT1-mutated meningiomas, or meningiomas lacking SMO and AKT1 mutations56. Additionally, the presence of the AKT1 p.Glu17Lys mutation in skull-base meningiomas was significantly associated with reduced time to tumour recurrence53. By contrast, KLF4-mutated meningiomas did not recur within this study, in contrast to meningiomas without a KLF4 mutation; however, the number of mutated meningiomas with available follow-up information was too low to draw any firm conclusions from this observation53. On the basis of these preliminary data, incorporation of TERT promoter, SMO and AKT1 p.Glu17Lys mutation analysis in future diagnostic work-ups seems reasonable, at least in skull-base meningioma.
DNA methylation analyses have provided a completely new understanding of the complexity within meningioma pathobiology. In a retrospective multicentre analysis, the DNA methylation pattern from 500 meningiomas was assessed90. Interestingly, through the analysis of molecular alterations and histology, this approach was able to distinguish six clinically different meningioma groups — three benign, two intermediate and one malignant. This integrated approach could represent the future of meningioma diagnostics because it provides a risk of recurrence, groups tumours by histological subtype and identifies molecular alterations that might be targetable by specific therapies.
Animal models
As mentioned, NF2 alterations are the most frequent molecular alterations in sporadic meningiomas. The importance of NF2 in meningioma development was demonstrated by Kalamarides et al., who showed that Cre-recombinase-induced inactivation of Nf2 in leptomeningeal cells of mice was capable of inducing meningiomas91. Transorbital Cre recombinase injection resulted in meningioma development in 29% of these mice, and subdural injection generated meningiomas in 19% of mice. The tumours recapitulated the most common histological subtypes of NF2-mutated meningiomas observed in humans. This pioneering work was expanded upon via the generation mice in which meningeal Nf2 was conditionally inactivated under control of the prostaglandin D2 synthase (Pgds) gene promoter, a specific marker of arachnoidal cells92. Nf2 inactivation in PGDS-positive meningeal progenitor cells resulted in both meningothelial and fibroblastic meningiomas in 38% of mice93. Surprisingly, the additional knockout of Cdkn2a or Trp53 did not increase meningioma frequency or malignancy, despite the reduction of lifespan due to the development of other tumours in these animals.
Molecular signalling pathways
Molecular signalling pathways, including those involved in mitogenic signal transduction, have been extensively studied in meningiomas. Nearly all growth factor receptors and kinases known to be involved in tumour growth have been identified as contributing factors in meningiomas and/or meningioma cell lines, including epidermal growth factor receptor (EGFR), platelet-derived growth factor receptor β (PDGFRβ), vascular endothelial growth factor receptor (VEGFR) and insulin-like growth factor receptor (IGFR)94,95,96,97 (Fig. 2). Activation of these receptors drives intracellular signalling cascades that are involved in a plethora of cellular functions. Mitogenic signals of EGFR and PDGFR are usually transduced by activation of the RAS–RAF–MEK–MAPK pathway (where MEK is dual specificity MAPK kinase 1; also known as MAP2K1); accordingly, this signalling pathway has also been shown to be activated in meningiomas66,98.
A multitude of cell processes have been identified to play a part in meningioma growth, including the MAPK (mitogen-activated protein kinase) pathway, the phosphoinositide 3-kinase (PI3K)–AKT–mammalian target of rapamycin complex (mTORC) pathway and the Hedgehog pathway. This figure summarizes the current medical treatment options for meningioma, which act on a variety of molecular targets. Some of the available agents are employed for their effects on molecular targets that could represent biomarkers for patient selection. EGFR, epidermal growth factor receptor; FAK, focal adhesion kinase; PDGFR, platelet-derived growth factor receptor; PIP3, phosphatidylinositol 3,4,5-triphosphate; SMO, smoothened homologue; VEGFR, vascular endothelial growth factor receptor.
The PI3K–AKT–S6K1 signalling pathway (where S6K1 is ribosomal protein S6 kinase-β1) is another important mediator of growth-favouring signals in meningiomas66,99,100. The relevance of this pathway is underlined by the existence of PI3K mutations in a subset of meningiomas55. As discussed in a previous section, the mTOR signalling pathway plays a part in NF2-mutant meningiomas. Other mechanisms of mTOR pathway activation also have a role in other types of meningiomas, such as those caused by S6K amplification, and a few mTOR mutations have been reported30,42,101,102,103. Other signalling pathways shown to be activated in meningiomas include the phospholipase A2–arachadonic acid–cyclooxygenase104,105 pathway and the phospholipase C γ1 (PLCγ1)–protein kinase C (PKC) pathway66,106. The transforming growth factor-β (TGFβ)–SMAD signalling pathway represents an inhibitory mechanism in meningioma growth, and TGFβ, as well as the TGFβ receptor, are expressed in meningiomas, thus representing potential treatment targets107,108,109.
Unfortunately, the identification of relevant mitogenic signalling pathways has been restricted mainly to in vitro studies with fast-growing cell lines characterized by artificial immortalization110,111. By contrast, patient-derived primary cultures have only slow growth rates112; therefore, treatment studies of patient-derived cells transplanted into animals are less effective and more time-consuming than those that use immortalized cells. On the other hand, orthotopic xenograft models with rapid tumour growth can provide helpful information that enables the selection of drugs that can efficiently target specific signalling pathways and facilitate post-mortem analysis of tumour tissue100; however, the highly malignant meningioma cells used in these models do not recapitulate the situation present in the majority of meningioma patients. Consequently, the identification of new recurrent mutations in WHO grade I meningiomas should prompt the development of meningioma models with a greater clinical relevance to enable potential antitumour drugs to be tested.
Emerging therapeutic opportunities
Individuals with meningiomas in surgically inaccessible areas (for example, the skull base), en plaque meningiomas, multiple meningiomas, metastatic meningiomas and recurrent or progressive WHO grade I, II or III meningiomas who have exhausted all surgical or radiotherapeutic options are candidates for systemic therapies because local therapies are not feasible in such cases. However, to date, no effective systemic therapies for meningiomas have been identified, although conclusive clinical trials are lacking. A number of agents including hydroxyurea, temozolomide, irinotecan, interferon-α, somatostatin analogues, mifepristone, megestrol acetate, imatinib, erlotinib and gefitinib, as well as the combination of cyclophosphamide, doxorubicin (Adriamycin; Rubex) and vincristine, have been evaluated, mostly in small and uncontrolled studies and patient series, and seem largely ineffective18,113. Although somatostatin receptors are expressed in meningiomas, the long-acting somatostatin analogue pasireotide did not significantly increase PFS-6 in a 2015 multicentre study23. Some evidence indicates that antiangiogenic drugs such as bevacizumab, vatalanib and sunitinib might have some activity against recurrent or progressive meningioma, but confirmatory data in large randomized studies are lacking114,115,116. Even combination therapies — for instance, combinations of antiangiogenic drugs such as bevacizumab and mTORC1 inhibitors such as everolimus — have not resulted in notable success115. Overall, the available studies on medical therapy of meningiomas are difficult to interpret owing to methodological limitations such as small sample sizes, lack of a control arm and heterogeneous inclusion and response criteria18. Owing to the existing heterogeneity among meningioma studies, use of PFS-6 was recommended as the primary end point for trials testing chemotherapy in recurrent meningiomas18. Nevertheless, randomized trial designs are preferable over single-arm studies as the reliability of historical control data is limited owing to the heterogeneity and small size of the available studies.
The discovery of potential molecular therapeutic targets in meningiomas led to the design of a molecularly driven meningioma trial (NCT02523014)117, which is sponsored by the Alliance for Clinical Trials in Oncology Group and the National Cancer Institute and is now actively accruing patients. In this trial, tumour samples from patients with residual, recurrent or progressive meningiomas of all grades are screened for alterations in AKT1, SMO and NF2, and patients are treated with AKT, SMO and FAK inhibitors, respectively. Response rate and PFS-6 are co-primary end points for this trial. Inhibitors of the Hedgehog pathway are in clinical use in other cancers; for example, the SMO inhibitor vismodegib is approved by the FDA for use in advanced basal cell carcinoma118. The role of TRAF7 and KLF4 in meningioma development is an active area of investigation, but no therapeutic targets are currently known for these genetic alterations. Anecdotal evidence in a single meningioma patient with an AKT1-mutated tumour suggests that AKT inhibitors have therapeutic efficacy in AKT1-mutated meningiomas119. Additionally, the observation of an association between the presence of the AKT1 p.Glu17Lys mutation and activation of both the mTOR and extracellular signal-regulated kinase 1 and 2 signalling pathways53 might help to pave the way for novel therapeutic approaches in meningiomas that are targeted against distinct mutations.
Dual mTORC1 and mTORC2 inhibition with vistusertib (AZD2014) was demonstrated to have stronger antiproliferative activity than other rapalogues (synthetic analogues of rapamycin) in preclinical studies and is being explored in a phase II study enrolling recurrent-grade aggressive meningiomas (NCT03071874, NCT02831257)120,121,122.
On the basis of in vitro and anecdotal evidence of clinical activity of the tetrahydroisoquinoline trabectedin in high-grade meningioma, the multicentre and randomized EORTC-1320 trial (NCT02234050)123 has been initiated and has completed patient accrual124. The precise mode of action of trabectedin is not known. However, it is known to bind to the minor groove of the DNA double helix, forming trabectedin–DNA adducts that bend the DNA towards the major groove. Consequently, trabectedin might affect diverse DNA-binding proteins, including several transcription factors and DNA repair mechanisms, and has antiangiogenic and immunomodulatory properties125. In the EORTC-1320 trial, a total of 86 patients with recurrent grade II or III meningiomas are randomized in a 2:1 ratio to either local standard of care or trabectedin therapy. The primary end point is PFS-6, with secondary end points of objective response rate, overall survival, safety and health-related quality of life.
Conclusions
Meningiomas are the most frequent intracranial tumours. In addition to the common genetic alterations in NF2 in sporadic meningiomas, a number of other clinically actionable genetic events have been described in meningiomas over the past 2 years, including oncogenic mutations in SMO, AKT1, TRAF7, KLF4, PIK3CA and POLR2A. Mutations in SMO, AKT1 and the TERT promoter seem to indicate increased risk of tumour recurrence and might be an indicator for close surveillance of at-risk patients. Methylation-based classification of meningiomas is a promising tool for the stratification of patients to enable suitable treatment and surveillance. New mouse models have supported the role of NF2 and other genes in tumour progression. Although the therapy of aggressive and/or recurrent meningiomas has focused largely on surgery and/or irradiation, these new genetic findings offer alternative routes for medical therapy, and clinical trials are underway. Thus, genomics have altered our understanding of the molecular underpinnings of meningiomas, and the ongoing clinical trials have the potential to alter how meningiomas are treated.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Harter, P. N., Braun, Y. & Plate, K. H. Classification of meningiomas-advances and controversies. Chin. Clin. Oncol. 6 (Suppl. 1), S2 (2017).
Ostrom, Q. T. et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol. 17 (Suppl. 4), iv1–iv62 (2015).
Tufan, K. et al. Intracranial meningiomas of childhood and adolescence. Pediatr. Neurosurg. 41, 1–7 (2005).
Perry, A. et al. Aggressive phenotypic and genotypic features in pediatric and NF2-associated meningiomas: a clinicopathologic study of 53 cases. J. Neuropathol. Exp. Neurol. 60, 994–1003 (2001).
Evans, D. G. R. et al. Cancer and central nervous system tumor surveillance in pediatric neurofibromatosis 2 and related disorders. Clin. Cancer Res. 23, e54–e61 (2017).
Ostrom, Q. T. et al. American Brain Tumor Association adolescent and young adult primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol. 18 (Suppl. 1), i1–i50 (2016).
Klaeboe, L. et al. Incidence of intracranial meningiomas in Denmark, Finland, Norway and Sweden, 1968–1997. Int. J. Cancer 117, 996–1001 (2005).
Sadetzki, S., Flint-Richter, P. & Ben-Tal, T. Radiation induced meningioma: a descriptive study of 253 cases. J. Neurosurg. 97, 1078–1082 (2002).
Schneider, B., Pulhorn, H., Rohrig, B. & Rainov, N. G. Predisposing conditions and risk factors for development of symptomatic meningioma in adults. Cancer Detect. Prevent. 29, 440–447 (2005).
Flint-Richter, P., Mandelzweig, L., Oberman, B. & Sadetzki, S. Possible interaction between ionizing radiation, smoking, and gender in the causation of meningioma. Neuro Oncol. 13, 345–352 (2011).
Benson, V. S. et al. Mobile phone use and risk of brain neoplasms and other cancers: prospective study. Int. J. Epidemiol. 42, 792–802 (2013).
Al-Mefty, O., Topsakal, C., Pravdenkova, S., Sawyer, J. R. & Harrison, M. J. Radiation-induced meningiomas: clinical, pathological, cytokinetic, and cytogenetic characteristics. J. Neurosurg. 100, 1002–1013 (2004).
Claus, E. B. et al. Exogenous hormone use, reproductive factors, and risk of intracranial meningioma in females. J. Neurosurg. 118, 649–656 (2013).
Claus, E. B. et al. Family and personal medical history and risk of meningioma. J. Neurosurg. 115, 1072–1077 (2011).
Ji, Y. et al. Double-blind phase III randomized trial of the antiprogestin agent mifepristone in the treatment of unresectable meningioma: SWOG S9005. J. Clin. Oncol. 33, 4093–4098 (2015).
Simpson, D. The recurrence of intracranial meningiomas after surgical treatment. J. Neurol. Neurosurg. Psychiatry 20, 22–39 (1957).
Gousias, K., Schramm, J. & Simon, M. The Simpson grading revisited: aggressive surgery and its place in modern meningioma management. J. Neurosurg. 125, 551–560 (2016).
Kaley, T. et al. Historical benchmarks for medical therapy trials in surgery- and radiation-refractory meningioma: a RANO review. Neuro Oncol. 16, 829–840 (2014).
Mathiesen, T., Lindquist, C., Kihlstrom, L. & Karlsson, B. Recurrence of cranial base meningiomas. Neurosurgery 39, 2–9 (1996).
ISRCTN Registry. ISRCTN.com http://www.isrctn.com/ISRCTN71502099 (2017).
Dziuk, T. W. et al. Malignant meningioma: an indication for initial aggressive surgery and adjuvant radiotherapy. J. Neurooncol. 37, 177–188 (1998).
Goldbrunner, R. et al. EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol. 17, e383–e391 (2016).
Norden, A. D. et al. Phase II study of monthly pasireotide LAR (SOM230C) for recurrent or progressive meningioma. Neurology 84, 280–286 (2015).
Louis, D. N. et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 131, 803–820 (2016).
Perry, A., Scheithauer, B. W., Stafford, S. L., Lohse, C. M. & Wollan, P. C. “Malignancy” in meningiomas: a clinicopathologic study of 116 patients, with grading implications. Cancer 85, 2046–2056 (1999).
Mawrin, C. & Perry, A. Pathological classification and molecular genetics of meningiomas. J. Neurooncol 99, 379–391 (2010).
Combs, S. E., Schulz-Ertner, D., Debus, J., von Deimling, A. & Hartmann, C. Improved correlation of the neuropathologic classification according to adapted World Health Organization classification and outcome after radiotherapy in patients with atypical and anaplastic meningiomas. Int. J. Radiat. Oncol. Biol. Phys. 81, 1415–1421 (2011).
Pearson, B. E. et al. Hitting a moving target: evolution of a treatment paradigm for atypical meningiomas amid changing diagnostic criteria. Neurosurg. Focus 24, E3 (2008).
Rogers, L. et al. Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. J. Neurosurg. 122, 4–23 (2015).
Brastianos, P. K. et al. Genomic sequencing of meningiomas identifies oncogenic SMO and AKT1 mutations. Nat. Genet. 45, 285–289 (2013).
Zang, K. Meningioma: a cytogenetic model of a complex benign human tumor, including data on 394 karyotyped cases. Cytogenet. Cell Genet. 93, 207–220 (2001).
Trofatter, J. A. et al. A novel moesin-, ezrin-, radixin-like gene is a candidate for the neurofibromatosis 2 tumor suppressor. Cell 72, 791–800 (1993).
Rouleau, G. A. et al. Alteration in a new gene encoding a putative membrane-organizing protein causes neuro-fibromatosis type 2. Nature 363, 515–521 (1993).
Petrilli, A. M. & Fernandez-Valle, C. Role of Merlin/NF2 inactivation in tumor biology. Oncogene 35, 537–548 (2016).
Seizinger, B. R., de la Monte, S., Atkins, L., Gusella, J. F. & Martuza, R. L. Molecular genetic approach to human meningioma: loss of genes on chromosome 22. Proc. Natl Acad. Sci. USA 84, 5419–5423 (1987).
Ruttledge, M. H. et al. Evidence for the complete inactivation of the NF2 gene in the majority of sporadic meningiomas. Nat. Genet. 6, 180–184 (1994).
Wellenreuther, R. et al. Analysis of the neurofibromatosis 2 gene reveals molecular variants of meningioma. Am. J. Pathol. 146, 827–832 (1995).
Hartmann, C. et al. NF2 mutations in secretory and other rare variants of meningiomas. Brain Pathol. 16, 15–19 (2006).
Nunes, F. et al. Inactivation patterns of NF2 and DAL-1/4.1B (EPB41L3) in sporadic meningioma. Cancer Genet. Cytogenet. 162, 135–139 (2005).
Goutagny, S. et al. Genomic profiling reveals alternative genetic pathways of meningioma malignant progression dependent on the underlying NF2 status. Clin. Cancer Res. 16, 4155–4164 (2010).
Curto, M. & McClatchey, A. I. Nf2/Merlin: a coordinator of receptor signalling and intercellular contact. Br. J. Cancer. 98, 256–262 (2008).
James, M. F. et al. NF2/Merlin is a novel negative regulator of mTOR complex 1, and activation of mTORC1 is associated with meningioma and schwannoma growth. Mol. Cell. Biol. 29, 4250–4261 (2009).
James, M. F. et al. Regulation of mTOR complex 2 signaling in neurofibromatosis 2-deficient target cell types. Mol. Cancer Res. 10, 649–659 (2012).
Wilisch-Neumann, A. et al. Re-evaluation of cytostatic therapies for meningiomas in vitro. J. Cancer Res. Clin. Oncol. 140, 1343–1352 (2014).
Shah, N. R. et al. Analyses of Merlin/NF2 connection to FAK inhibitor responsiveness in serous ovarian cancer. Gynecol. Oncol. 134, 104–111 (2014).
Shapiro, I. M. et al. Merlin deficiency predicts FAK inhibitor sensitivity: a synthetic lethal relationship. Sci. Transl Med. 6, 237ra68 (2014).
Schmitz, U. et al. INI1 mutations in meningiomas at a potential hotspot in exon 9. Br. J. Cancer 84, 199–201 (2001).
Hadfield, K. D. et al. Molecular characterisation of SMARCB1 and NF2 in familial and sporadic schwannomatosis. J. Med. Genet. 45, 332–339 (2008).
Clark, V. E. et al. Recurrent somatic mutations in POLR2A define a distinct subset of meningiomas. Nat. Genet. 48, 1253–1259 (2016).
Carpten, J. D. et al. A transforming mutation in the pleckstrin homology domain of AKT1 in cancer. Nature 448, 439–444 (2007).
Keppler-Noreuil, K. M., Baker, E. H., Sapp, J. C., Lindhurst, M. J. & Biesecker, L. G. Somatic AKT1 mutations cause meningiomas colocalizing with a characteristic pattern of cranial hyperostosis. Am. J. Med. Genet. A 170, 2605–2610 (2016).
Clark, V. E. et al. Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO. Science 339, 1077–1080 (2013).
Yesiloez, U. K. et al. Frequent AKT1E17K mutations in skull base meningiomas are associated with mTOR and ERK1/2 activation and reduced time to tumor recurrence. Neuro Oncol. 19, 1088–1096 (2017).
Yuzawa, S. et al. Clinical impact of targeted amplicon sequencing for meningioma as a practical clinical-sequencing system. Modern Pathol. 29, 708–716 (2016).
Abedalthagafi, M. et al. Oncogenic PI3K mutations are as common as AKT1 and SMO mutations in meningioma. Neuro Oncol. 18, 649–655 (2016).
Boetto, J., Bielle, F., Sanson, M., Peyre, M. & Kalamarides, M. SMO mutation status defines a distinct and frequent molecular subgroup in olfactory groove meningiomas. Neuro Oncol. 19, 345–351 (2017).
Laurendeau, I. et al. Gene expression profiling of the Hedgehog signaling pathway in human meningiomas. Mol. Med. 16, 262–270 (2010).
Ng, J. M. Y. & Curran, T. The Hedgehog's tale: developing strategies for targeting cancer. Nat. Rev. Cancer 11, 493–501 (2011).
Kieran, M. W. Targeted treatment for Sonic Hedgehog-dependent medulloblastoma. Neuro Oncol. 16, 1037–1047 (2014).
Smith, M. J. et al. Germline mutations in SUFU cause Gorlin syndrome-associated childhood medulloblastoma and redefine the risk associated with PTCH1 mutations. J. Clin. Oncol. 32, 4155–4161 (2014).
Xu, L. G., Li, L. Y. & Shu, H. B. TRAF7 potentiates MEKK3-induced AP1 and CHOP activation and induces apoptosis. J. Biol. Chem. 279, 17278–17282 (2004).
McConnell, B. B. & Yang, V. W. Mammalian Kruppel-like factors in health and diseases. Physiol. Rev. 90, 1337–1381 (2010).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676 (2006).
Schuetz, A. et al. The structure of the Klf4 DNA-binding domain links to self-renewal and macrophage differentiation. Cell. Mol. Life Sci. 68, 3121–3131 (2011).
Reuss, D. E. et al. Secretory meningiomas are defined by combined KLF4 K409Q and TRAF7 mutations. Acta Neuropathol. 125, 351–358 (2013).
Mawrin, C. et al. Different activation of mitogen-activated protein kinase and Akt signaling is associated with aggressive phenotype of human meningiomas. Clin. Cancer Res. 11, 4074–4082 (2005).
El-Habr, E. A. et al. Complex interactions between the components of the PI3K/AKT/mTOR pathway, and with components of MAPK, JAK/STAT and Notch-1 pathways, indicate their involvement in meningioma development. Virchows Arch. 465, 473–485 (2014).
Harmanci, A. S. et al. Integrated genomic analyses of de novo pathways underlying atypical meningiomas. Nat. Commun. 8, 14433 (2017).
Sahm, F. et al. TERT promoter mutations and risk of recurrence in meningioma. J. Natl Cancer Inst. 108, djv377 (2016).
Bi, W. L. et al. Genomic landscape of high-grade meningiomas. NPJ Genom. Med. 2, 15 (2017).
Rogers, C. L. et al. Pathology concordance levels for meningioma classification and grading in NRG Oncology RTOG Trial 0539. Neuro Oncol. 18, 565–574 (2016).
Vaubel, R. A. et al. Meningiomas with rhabdoid features lacking other histologic features of malignancy: a study of 44 cases and review of the literature. J. Neuropathol. Exp. Neurol. 75, 44–52 (2016).
Shankar, G. M. et al. Germline and somatic BAP1 mutations in high-grade rhabdoid meningiomas. Neuro Oncol. 19, 535–545 (2017).
Carbone, M. et al. BAP1 and cancer. Nat. Rev. Cancer 13, 153–159 (2013).
Ketter, R. et al. Application of oncogenetic trees mixtures as a biostatistical model of the clonal cytogenetic evolution of meningiomas. Int. J. Cancer 121, 1473–1480 (2007).
Catala, M. Embryonic and fetal development of structures associated with the cerebro-spinal fluid in man and other species. Part I: The ventricular system, meninges and choroid plexuses. Arch. d'Anatomie Cytol. Pathol. 46, 153–169 (1998).
Kros, J. et al. NF2 status of meningiomas is associated with tumour localization and histology. J. Pathol. 194, 367–372 (2001).
Lee, J. H., Sade, B., Choi, E., Golubic, M. & Prayson, R. Meningothelioma as the predominant histological subtype of midline skull base and spinal meningioma. J. Neurosurg. 105, 60–64 (2006).
Ketter, R. et al. Correspondence of tumor localization with tumor recurrence and cytogenetic progression in meningiomas. Neurosurgery 62, 61–69 (2008).
Antinheimo, J. et al. Population-based analysis of sporadic and type 2 neurofibromatosis-associated meningiomas and schwannomas. Neurology 54, 71–76 (2000).
Sahm, F. et al. AKT1E17K mutations cluster with meningothelial and transitional meningiomas and can be detected by SFRP1 immunohistochemistry. Acta Neuropathol. 126, 757–762 (2013).
Strickland, M. R. et al. Targeted sequencing of SMO and AKT1 in anterior skull base meningiomas. J. Neurosurg. 127, 438–444 (2016).
Smith, M. J. et al. Loss-of-function mutations in SMARCE1 cause an inherited disorder of multiple spinal meningiomas. Nat. Genet. 45, 295–298 (2013).
Smith, M. J. et al. Germline SMARCE1 mutations predispose to both spinal and cranial clear cell meningiomas. J. Pathol. 234, 436–440 (2014).
Simon, M. et al. Allelic losses on chromosomes 14, 10, and 1 in atypical and malignant meningiomas: a genetic model of meningioma progression. Cancer Res. 55, 4696–4701 (1995).
Ketter, R. et al. Predictive value of progression-associated chromosomal aberrations for the prognosis of meningiomas: a retrospective study of 198 cases. J. Neurosurg. 95, 601–607 (2001).
Bello, M. J. et al. Allelic loss at 1p is associated with tumor progression of meningiomas. Genes Chromosomes Cancer 9, 296–298 (1994).
Kalala, J. P., Maes, L., Vandenbroecke, C. & de Ridder, L. The hTERT protein as a marker for malignancy in meningiomas. Oncol. Rep. 13, 273–277 (2005).
Goutagny, S. et al. High incidence of activating TERT promoter mutations in meningiomas undergoing malignant progression. Brain Pathol. 24, 184–189 (2013).
Sahm, F. et al. DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol. 18, 682–694 (2017).
Kalamarides, M. et al. Nf2 gene inactivation in arachnoidal cells is rate-limiting for meningioma development in the mouse. Genes Dev. 16, 1060–1065 (2002).
Kawashima, M., Suzuki, S. O., Yamashima, T., Fukui, M. & Iwaki, T. Prostaglandin D synthase (β-trace) in meningeal hemangiopericytoma. Modern Pathol. 14, 197–201 (2001).
Kalamarides, M. et al. Identification of a progenitor cell of origin capable of generating diverse meningioma histological subtypes. Oncogene 30, 2333–2344 (2011).
Weisman, A. S., Raguet, S. S. & Kelly, P. A. Characterization of the epidermal growth factor receptor in human meningioma. Cancer Res. 47, 2172–2176 (1987).
Maxwell, M., Galanopoulos, T., Hedley-Whyte, E. T., Black, P. M. & Antoniades, H. N. Human meningiomas co-express platelet-derived growth factor (PDGF) and PDGF-receptor genes and their protein products. Int. J. Cancer 46, 16–21 (1990).
Baumgarten, P. et al. Expression of vascular endothelial growth factor (VEGF) and its receptors VEGFR1 and VEGFR2 in primary and recurrent WHO grade III meningiomas. Histol. Histopathol. 28, 1157–1166 (2013).
Lichtor, T., Kurpakus, M. A. & Gurney, M. E. Expression of insulin-like growth factors and their receptors in human meningiomas. J. Neurooncol. 17, 183–190 (1993).
Johnson, M. D., Woodard, A., Kim, P. & Frexes-Steed, M. Evidence for mitogen-associated protein kinase activation and transduction of mitogenic signals by platelet-derived growth factor in human meningioma cells. J. Neurosurg. 94, 293–300 (2001).
Johnson, M. D., Okedli, E., Woodard, A., Toms, S. A. & Allen, G. S. Evidence for phosphatidylinositol 3-kinase-Akt-p7S6K pathway activation and transduction of mitogenic signals by platelet-derived growth factor in meningioma cells. J. Neurosurg. 97, 668–675 (2002).
Pachow, D. et al. mTORC1 inhibitors suppress meningioma growth in mouse models. Clin. Cancer Res. 19, 1180–1189 (2013).
Cai, D. X., James, C. D., Scheithauer, B. W., Couch, F. J. & Perry, A. PS6K amplification characterizes a small subset of anaplastic meningiomas. Am. J. Clin. Pathol. 115, 213–218 (2001).
Surace, E. I., Lusis, E., Haipek, C. A. & Gutmann, D. H. Functional significance of S6K overexpression in meningioma progression. Ann. Neurol. 56, 295–298 (2004).
Lopez-Lago, M. A., Okada, T., Murillo, M. M., Socci, N. & Giancotti, F. G. Loss of the tumor suppressor gene NF2, encoding merlin, constitutively activates integrin-dependent mTORC1 signaling. Mol. Cell. Biol. 29, 4235–4249 (2009).
Castelli, M. G. et al. Prostaglandin and thromboxane synthesis by human intracranial tumors. Cancer Res. 49, 1505–1508 (1989).
Kang, H. C., Kim, I. H., Park, C. I. & Park, S. H. Immunohistochemical analysis of cyclooxygenase-2 and brain fatty acid binding protein expression in grades I-II meningiomas: correlation with tumor grade and clinical outcome after radiotherapy. Neuropathology 34, 446–454 (2014).
Johnson, M. D., Horiba, M., Winnier, A. R. & Arteaga, C. L. The epidermal growth factor receptor is associated with phospholipase C-γ1 in meningiomas. Hum. Pathol. 25, 146–153 (1994).
Johnson, M. D., Shaw, A. K., O'Connell, M. J., Sim, F. J. & Moses, H. L. Analysis of transforming growth factor β receptor expression and signaling in higher grade meningiomas. J. Neurooncol. 103, 277–285 (2011).
Nagashima, G., Asai, J., Suzuki, R. & Fujimoto, T. Different distribution of c-myc and MIB-1 positive cells in malignant meningiomas with reference to TGFs, PDGF, and PgR expression. Brain Tumor Pathol. 18, 1–5 (2001).
Johnson, M. D., O'Connell, M. J., Vito, F. & Pilcher, W. Bone morphogenetic protein 4 and its receptors are expressed in the leptomeninges and meningiomas and signal via the Smad pathway. J. Neuropathol. Exp. Neurol. 68, 1177–1183 (2009).
Ragel, B. T. et al. A comparison of the cell lines used in meningioma research. Surg. Neurol. 70, 295–307 (2008).
Puttmann, S. et al. Establishment of a benign meningioma cell line by hTERT-mediated immortalization. Lab. Invest. 85, 1163–1171 (2005).
Friedrich, S. et al. Comparative morphological and immunohistochemical study of human meningioma after intracranial transplantation into nude mice. J. Neurosci. Methods 205, 1–9 (2012).
Wen, P., Quant, E., Drappatz, J., Beroukhim, R. & Norden, A. Medical therapies for meningiomas. J. Neurooncol 99, 365–378 (2010).
Kaley, T. J. et al. Phase II trial of sunitinib for recurrent and progressive atypical and anaplastic meningioma. Neuro Oncol. 17, 116–121 (2015).
Shih, K. C. et al. A phase II trial of bevacizumab and everolimus as treatment for patients with refractory, progressive intracranial meningioma. J. Neurooncol. 129, 281–288 (2016).
Mawrin, C., Chung, C. & Preusser, M. Biology and clinical management challenges in meningioma. Am. Soc. Clin. Oncol. Educ. Book https://doi.org/10.14694/EdBook_AM.2015.35.e106 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02523014 (2017).
Von Hoff, D. D. et al. Inhibition of the Hedgehog pathway in advanced basal-cell carcinoma. N. Engl. J. Med. 361, 1164–1172 (2009).
Weller, M. et al. Durable control of metastatic AKT1-mutant WHO-grade I meningothelial meningioma by the AKT inhibitor, AZD5363. J. Natl Cancer Inst. 109, djw320 (2016).
Beauchamp, R. L. et al. A high-throughput kinome screen reveals serum/glucocorticoid-regulated kinase 1 as a therapeutic target for NF2-deficient meningiomas. Oncotarget 6, 16981–16997 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03071874 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02831257 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02234050 (2017).
Preusser, M. et al. Trabectedin has promising antineoplastic activity in high-grade meningioma. Cancer. 118, 5038–5049 (2012).
Germano, G. et al. Role of macrophage targeting in the antitumor activity of trabectedin. Cancer Cell. 11, 249–262 (2013).
Acknowledgements
The meningioma research of C.M.'s group is supported by Deutsche Forschungsgemeinschaft (Germany; grant MA2530/6-1 and MA2530/8-1), Wilhelm Sander-Stiftung (Germany; grant 2014.092.1) and Deutsche Krebshilfe (Germany; grant #111853).
Author information
Authors and Affiliations
Contributions
All authors contributed to the research, discussion, writing and review of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Preusser, M., Brastianos, P. & Mawrin, C. Advances in meningioma genetics: novel therapeutic opportunities. Nat Rev Neurol 14, 106–115 (2018). https://doi.org/10.1038/nrneurol.2017.168
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2017.168
This article is cited by
-
Establishment of tumor microenvironment-preserving organoid model from patients with intracranial meningioma
Cancer Cell International (2024)
-
Meningioma segmentation with GV-UNet: a hybrid model using a ghost module and vision transformer
Signal, Image and Video Processing (2024)
-
Drug target therapy and emerging clinical relevance of exosomes in meningeal tumors
Molecular and Cellular Biochemistry (2024)
-
Complete loss of E-cadherin expression in a rare case of metastatic malignant meningioma: a case report
BMC Neurology (2023)
-
A novel patient-derived meningioma spheroid model as a tool to study and treat epithelial-to-mesenchymal transition (EMT) in meningiomas
Acta Neuropathologica Communications (2023)