Abstract
Biallelic inactivation of the NF2 gene occurs in the majority of schwannomas. This usually involves a combination of a point mutation or multiexon deletion, in conjunction with either a second point mutation or loss of heterozygosity (LOH). We have performed DNA sequence and dosage analysis of the NF2 gene in a panel of 239 schwannoma tumours: 97 neurofibromatosis type 2 (NF2)-related schwannomas, 104 sporadic vestibular schwannomas (VS) and 38 schwannomatosis-related schwannomas. In total, we identified germline NF2 mutations in 86 out of 97 (89%) NF2 patients and a second mutational event in 77 out of 97 (79%). LOH was by far the most common form of second hit. A combination of microsatellite analysis with either conventional comparative genomic hybridization (CGH) or multiplex ligation-dependent probe amplification (MLPA) identified mitotic recombination (MR) as the cause of LOH in 14 out of 72 (19%) total evaluable tumours. Among sporadic VS, at least one NF2 mutation was identified by sequence analysis or MLPA in 65 out of 98 (66%) tumours. LOH occurred in 54 out of 96 (56%) evaluable tumours, but MR only accounted for 5 out of 77 (6%) tested. LOH was present in 28 out of 34 (82%) schwannomatosis-related schwannomas. In all eight patients who had previously tested positive for a germline SMARCB1 mutation, this involved loss of the whole, or part of the long arm, of chromosome 22. In contrast, 5 out of 22 (23%) tumours from patients with no germline SMARCB1 mutation exhibited MR. High-resolution Affymetrix SNP6 genotyping and copy number (CN) analysis (Affymetrix, Santa Clara, CA, USA) were used to determine the chromosomal breakpoint locations in tumours with MR. A range of unique recombination sites, spanning approximately 11.4 Mb, were identified. This study shows that MR is a mechanism of LOH in NF2 and SMARCB1-negative schwannomatosis-related schwannomas, occurring less frequently in sporadic VS. We found no evidence of MR in SMARCB1-positive schwannomatosis, suggesting that susceptibility to MR varies according to the disease context.
Similar content being viewed by others
Introduction
Schwannomas are benign peripheral nerve sheath tumours that occur within the context of the tumour suppressor syndromes, neurofibromatosis type 2 (NF2) and schwannomatosis. They also occur sporadically within the general population. In most schwannoma tumours, the NF2 gene, located on chromosome 22q12.2, is biallelically inactivated. In NF2 patients, the first mutation is frequently a constitutional point mutation or a small deletion. This is followed by a second somatic mutation in the tumour, which is either a second point mutation, or, more commonly, by loss of the wild-type allele. Mutation within the NF2 gene promoter or hypermethylation of key CpG dinucleotides within this region may be an additional mechanism of inactivation (Kino et al., 2001). This region is not routinely tested and may account for a proportion of patients with unfound mutations. In schwannomas occurring outside NF2 disease, NF2 mutations are only found somatically, occurring in the tumour, but not in the germline (MacCollin et al., 2003), suggesting that other genes are involved in these cases.
The chromatin remodelling gene, SMARCB1, located approximately 6 Mb upstream of NF2 at 22q11.23, was recently found to be mutated in germline DNA in approximately 50% of familial schwannomatosis patients, and, less commonly, in sporadic schwannomatosis (5–10%) (Hulsebos et al., 2007; Boyd et al., 2008; Hadfield et al., 2008; Sestini et al., 2008). Our previous study has shown that these germline SMARCB1 mutations are frequently associated with a somatic NF2 mutation in tumours (Boyd et al., 2008; Hadfield et al., 2008), and a multihit hypothesis has been suggested, involving both of these loci (Boyd et al., 2008; Hadfield et al., 2008; Sestini et al., 2008).
The region 22q11 contains several low copy repeat domains, and is known to be a particularly unstable region of the genome (Dunham et al., 1999; Edelmann et al., 1999). Recombination events in this region are known to be involved in several diseases, occurring both constitutionally (for example, cat eye syndrome, velocardiofacial syndrome, DiGeorge syndrome) and somatically (for example, chronic myelogenous leukaemia Burkitt's lymphoma, Ewing's sarcoma) (Kaplan et al., 1987).
Mitotic recombination (MR) is known to be an important mutational mechanism in neurofibromatosis type 1 and other tumour syndromes. Loss of heterozygosity (LOH) of 17q is a common somatic hit in neurofibromas lacking a germline microdeletion mutation, and is frequently the result of MR (Serra et al., 2001; De Raedt et al., 2006). As LOH is also a common event in tumours of patients with NF2, as well as with sporadic vestibular schwannomas (VS) and schwannomatosis, and chromosome 22 is prone to a variety of recombinational events, we analysed a panel of tumours from each of these groups to determine rates of LOH and MR with respect to the diagnosis and to the initial genetic event. The Genome-Wide Human SNP Array 6.0 (Affymetrix) platform was used to confirm the results and refine identified breakpoints, as the combination of high density of small-nucleotide polymorphism (SNP) genotyping and high density copy number (CN) probes provides a more accurate and sensitive way to determine both CN and homozygosity than do conventional methods.
Results
Mutation spectrum of NF2, sporadic VS and schwannomatosis tumours
We have performed DNA sequence and dosage analysis of the NF2 gene in a panel of 239 schwannoma tumours: 97 tumours from 97 patients with NF2, 104 sporadic VS and 38 tumours from 34 patients with schwannomatosis (Table 1). We identified germline mutations in NF2 in 89% (86 out of 97) of NF2 patients. Out of these, 70 were found by direct sequence analysis and consisted predominantly of nonsense mutations (36%) and frameshift mutations (21%). The remainder consisted of splice mutations (13%), a single missense mutation and an in-frame deletion of a single amino acid. In all, 16 additional tumours harboured single or multiexon deletions found by multiplex ligation-dependent probe amplification (MLPA). A second mutational event was found in 77 (79%). This was a second point mutation in 13, MLPA deletion of a part of NF2 in 2 and LOH in 62. MR was the cause of LOH in 14 out of 41 evaluable tumours. Excluding tumours with LOH, but not tested for MR, this leads to an overall rate of 14 out of 72 (19%). Analysis was not possible in some tumours, because of insufficient DNA or because of poor quality of some DNA samples extracted from paraffin blocks. In total, 7 of 15 NF2 patients with large multiexon deletions had LOH as the mechanism of second hit (including 3 with >6 exons deleted), although this did not occur in the two patients with whole-gene deletions. MR was not found to be the cause of LOH in any of these tumours.
Of the 41 NF2 patients tested for MR, 27 were mosaic, 13 were non-mosaic and 1 was uncertain. MR was the cause of LOH in seven of the non-mosaic patients (age range: 7–40 years; average: 23 years). These seven patients developed a total of 191 spinal and peripheral nerve schwannomas, with an average of 27 tumours per person. Sixteen non-mosaic NF2 patients with no evidence of MR, including those with no LOH (age range: 9–57 years; average: 32 years), had a total of 113 schwannomas, with an average of seven tumours per person. This may suggest that the MR mechanism functions as a modifier for NF2, leading to a more severe schwannoma phenotype, although the difference in tumour burden did not reach statistical significance by the two-tailed t-test (P=0.129). Furthermore, 5 out of 7 MR patients had an underlying truncating (nonsense/frameshift) mutation, compared with only 5 out of 16 non-mosaic patients. Out of the 27 mosaic patients, seven (six out of seven not identifiable in blood) showed MR and, strikingly, all seven developed spinal and/or peripheral nerve schwannomas (three out of seven aged <20 years); one as young as 10 years of age, despite the mutation being undetectable in the lymphocyte DNA. Of 21 mosaic patients without evidence of MR (16 out of 21 not identifiable in blood), only three developed a spinal or peripheral nerve schwannoma <20 years and five had no evidence of either spinal or cutaneous schwannomas. There was no evidence that these effects were primarily due to the underlying mutation: 6 out of 7 mosaic MR patients and 16 out of 21 mosaic non-MR patients had the more severe truncating mutations.
Among sporadic VS, we identified at least one point mutation in the NF2 gene in 65 out of 98 (66%) tumours, with a higher incidence of frameshift (34%) than nonsense mutations (17%) in comparison with NF2-related tumours. Splice mutations (10%) and missense mutations (1%) occurred in similar proportions to NF2 tumours. MLPA identified a single exon-11 deletion. LOH occurred in 54 out of 96 (56%), but MR only accounted for 5 out of 35 evaluable tumours, with an overall rate of 5 out of 7 (6%). The difference between MR rates in evaluable tumours between NF2 and sporadic VS is significant by χ2-test (P-value=0.0161) if we extrapolate our results to calculate the predicted overall number of tumours in each group by first extrapolating the predicted proportion of LOH hits in the total number of tumours and then extrapolating the proportion of LOH hits due to MR. This suggests that 22 out of 97 NF2 tumours and 8 out of 104 sporadic VS have been caused by MR in our cohort. This proportion is also significant by χ2-test, adjusting for the lower rate of LOH, in addition to MR in sporadic VS (P=0.010).
As expected, no germline NF2 mutations were found in any schwannomatosis patients. However, germline SMARCB1 mutations were found in eight patients (six from three different families and two sporadic patients) and somatic NF2 point mutations were found in 24 tumours (Hadfield et al., 2008). The proportions of NF2 frameshift mutations (37%) and splice mutations (11%) were similar to those found in sporadic VS, but with fewer nonsense mutations (5%) and a greater number of missense (8%) mutations.
LOH was present in 28 out of 38 (74%) schwannomatosis-related schwannomas. In all eight tumours from schwannomatosis patients who tested positive for a germline SMARCB1 mutation, this involved loss of the whole chromosome 22 or part of the long arm. In contrast, 5 out of 22 (23%) evaluable tumours from 19 patients who had tested negative for SMARCB1 mutations exhibited MR.
Determination of mitotic recombination breakpoints
To investigate the potential mechanisms leading to MR, we sought to define a critical region of recombination on chromosome 22q, relevant to the pathogenesis of schwannomas. We used Affymetrix SNP6.0 arrays to identify recombination breakpoints in a subset of tumour samples that were previously found to have undergone MR by a combination of dosage and heterozygosity analysis, consisting of either conventional CGH and microsatellite analysis or MLPA and microsatellite analysis. Genomic DNA was available for analysis from seven NF2-related schwannomas, one sporadic VS and two SMARCB1 mutation-negative schwannomatosis-related schwannomas, along with their respective matched blood DNAs.
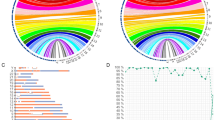
The data confirmed that MR was unique to chromosome 22 in each sample, as all other chromosomes showed normal CN and comparable heterozygosity in blood and tumour. We determined the breakpoint locations on chromosome 22q in six tumours obtained from five patients with NF2, one sporadic VS and two SMARCB1 mutation-negative schwannomatosis-related schwannomas (Table 2). Examples of the SNP array results are shown in Figure 1.
Examples of genotyping and copy number (CN) analysis in tumours displaying mitotic recombination. Results from paired blood and tumour DNA from each patient were compared side by side to identify regions of homozygosity and changes in CN. Allele difference plots show homozygous single-nucleotide polymorphism (SNP) calls in tracks +1 and −1 and heterozygous SNP calls at 0. Loss of heterozygous SNP calls,without loss of the entire chromosome and in conjunction with a CN of 2, indicates a mitotic recombination event.
NF2 tumours showed a range of unique breakpoints from 16 615 305 (SNP ID: rs181408) to 28 018 632 (SNP ID: rs3761426) on chromosome 22 (Figure 2a). Two tumours from the same patient (5i and 5ii) showed relatively close, but non-identical breakpoints, approximately 350 000 bases apart. For one further NF2-related sample, the combined genotyping and CN data analysis determined that the LOH previously identified as MR by a combination of microsatellite analysis and conventional comparative genomic hybridization (CGH) was in fact due to loss of genetic material.
A breakpoint was determined in a single sporadic VS after 16 754 150 (SNP ID: rs2075453).
Recombination breakpoints were determined for both SMARCB1 mutation-negative sporadic schwannomatosis tumours tested. Interestingly, the breakpoint in one of these tumours occurred at 23 283 227 (SNP ID: rs2298386), which is downstream of the SMARCB1 locus. Together, the results show a wide range of recombination breakpoints, spanning approximately 11.4 Mb with no shared recombination sites (Figure 2a).
Discussion
We have found that mitotic recombination events are responsible for the LOH found in a proportion of schwannoma tumours. These events are particularly important for SMARCB1 mutation-negative schwannomatosis and NF2-related tumours, in which 23 and 19% of evaluable tumours tested positive for MR, respectively. A lower proportion of patients with sporadic VS also seem to be susceptible to MR (6%). However, although all schwannomatosis patients who tested positive for a germline SMARCB1 mutation also harboured LOH in their tumour, none of this loss was due to an MR event, suggesting that tumours from this group of patients develop through an alternative mechanism.
We used high-density SNP analysis to refine the breakpoints and identify any common regions of recombination in 10 tumours. This method provides much more information than the combination of microsatellite analysis and conventional CGH or MLPA used previously. In this study, one NF2 tumour, originally identified with somatic LOH caused by MR, was shown to be due to loss of one chromosome 22. One reason for a false-positive result in the original analysis is the mixed population of normal and tumour cell DNA in some tumour samples, which is more difficult to identify by conventional methods. In the nine remaining tumours, MR was confirmed as the cause of LOH.
The low copy repeat (LCR22) domains within the 22q11.2 region are distributed across an approximately 6.3 Mb region. The constitutional breakpoints responsible for deletions in the velocardiofacial syndrome only tend to occur within three of these (Edelmann et al., 1999), whereas the somatic translocation events that occur in chronic myelogenous leukaemia are found in the breakpoint cluster region (BCR) gene, in a separate low copy repeat domain. In our study, seven of the nine approximate breakpoints that we were able to determine were distributed across region 22q11.2. However, each breakpoint was unique and found outside of the LCR22 sequences (Figure 2b). The distribution of breakpoints showed no particular clustering and in each case the recombinant region extended from the breakpoint to the chromosome terminus, suggesting an alternative trigger for this type of recombination. The two remaining recombination breakpoints occurred outside of the q11.2 region, in q12.1 (patient 1) and q12.2 (patient 4). Both of these were from NF2 patients and occurred upstream of the NF2 gene.
Four schwannomas from our panel (from patients 1, 2, 4 and 7) harboured a recombination breakpoint between the SMARCB1 and NF2 loci (Figure 2a). One of these was a SMARCB1 mutation-negative schwannomatosis-related tumour. The breakpoint for this tumour causes disruption of the NF2 gene by effecting homozygosity of a somatic mutation identified in the tumour, but may also have a positional effect on the SMARCB1 gene, despite occurring downstream of this locus.
Interestingly, none of the LOH in SMARCB1 mutation-positive schwannomas was due to MR. It is possible that the initiating genetic event may influence the type of second hit that occurs in the tumour, as has been suggested for the difference in occurrence of LOH in neurofibromatosis type 1 neurofibromas with and without germline microdeletions (De Raedt et al., 2006). In our cohort of NF2 patients, the most common sequence of mutation events was a constitutional point mutation, followed by a somatic LOH event, whereas the two patients with whole-gene deletions as a first hit had a point mutation as the second hit.
In SMARCB1-positive schwannomatosis, the initiating event is a germline SMARCB1 mutation with the second proposed event being an LOH deletion of 22q that removes the wild-type SMARCB1 and an allelic copy of NF2 (Hulsebos et al., 2007; Boyd et al., 2008; Hadfield et al., 2008; Sestini et al., 2008). The third hit would be an NF2 mutation on the remaining ipsilateral allele to the germline SMARCB1 mutation. MR would not have a role in this three-hit hypothesis, as reduplication of the mutant allele would only be possible if the ipsilateral NF2 mutation occurred second. It is possible that loss of SMARCB1 and a dosage loss of half of NF2 would cause schwann cell proliferation, thus driving the third mutation.
Aberrant methylation of three CpG islands in the NF2 gene promoter has been shown to downregulate its expression (Kino et al., 2001) and has been suggested as a mechanism for progression to growth of VS (Gonzalez-Gomez et al., 2003). It is possible that increased rates of aberrant methylation in sporadic VS may account for the reduced detection rate of NF2 point mutations in sporadic VS in comparison with NF2 tumours. As a reduction in the levels of methylation has also been proposed as a mechanism of increased occurrence of genomic recombination events (Carbone et al., 2009), it is also possible that an increased incidence of methylation in certain tumours would reduce the likelihood of MR involvement. Further work is necessary to test this hypothesis.
A number of patients have shown MR in more than one tumour and there seems to be a trend towards an increased schwannoma formation in those patients who develop schwannomas by this mechanism. We were unable to demonstrate a formal statistical significance for this, but it remains possible that some individuals with non-mosaic NF2 or SMARCB1-negative schwannomatosis and an increased susceptibility to MR have a higher risk of increased tumour burden.
In summary, our study demonstrates a role for mitotic recombination events in the development of a proportion of schwannoma tumours and shows that the rates of MR vary, depending on the disease context. The lack of SMARCB1 mutations in schwannomatosis-related schwannomas with MR suggests that there are additional genetic causes of schwannomatosis, one of which may involve an increased susceptibility to mitotic recombination. Further studies will be required to determine the specific combination of genetic events that initiates tumour growth
Materials and methods
Patient tumours
Tumour DNA from a total of 239 patients was included in the study. In total, 97 patients fulfilled the clinical criteria for NF2 disease (Evans et al., 1992). Another 104 patients had suffered only a unilateral VS and had tested negative for germline NF2 mutation.
There were 38 tumours from 34 schwannomatosis patients; eight patients were from families with multiple affected members who were negative for VS and germline NF2 mutations. The remaining 26 were sporadic patients with at least three schwannomas in more than one body segment and who were negative for VS and germline NF2 mutations. Approval for the study was provided by the Central Manchester local ethics committee. Informed consent was obtained from patients and their families for publication of their details in this report.
Mutational analysis
DNA sequence analysis of NF2 and SMARCB1 genes, CN analysis of SMARCB1 exon deletions or amplifications by quantitative RT–PCR (TaqMan) assay and LOH analysis by microsatellite markers D22S303, D22S310, D22S446, D22S449, D22S1174, D22S275, NF2CA3 and D22S268 were carried out as described by Hadfield et al, 2008. The microsatellite markers spanned a total of approximately 12.7 Mb of chromosome 22, covering both the NF2 and SMARCB1 loci. Analysis of the centromeric microsatellite marker D22S420, which is found 6.3 Mb upstream of SMARCB1, was used to confirm that any observed LOH was not due to deletion, followed by reduplication of the homologous chromosome 22.
Hybridization, ligation and amplification of MLPA probes for exon CN analysis were carried out according to the manufacturer's instructions (MRC-Holland, Amsterdam, The Netherlands). The method for CGH was previously described in (James and Varley, 1996; James et al., 1999; Warren et al., 2003).
High-resolution genotyping and CN analysis
Matched blood and tumour samples for each patient were genotyped using the Genome-Wide Human SNP Array 6.0 (Affymetrix). Genomic DNA was purified by ethanol precipitation and 500 ng was hybridized to an SNP6 chip according to the manufacturer's instructions. This array contains a total of ∼1.8 million probes, comprised of 906 600 SNP probes and 946 000 CN probes spaced throughout the genome. Staining of the array was carried out on a Fluidics Station 450 (Affymetrix) and the array was scanned using the GeneChip scanner 3000 7G system (Affymetrix).
Data analysis
The CN data were generated using the BRLMM-P-Plus algorithm from Affymetrix using reference model files generated from a pool of 56 unaffected genomic DNA control samples. Genotype and CN analysis were carried out using the Genotyping Console 3.0.2 (Affymetrix). The genotyping no-call threshold was set to 0.01 and the CN/LOH detection threshold was set to 0.02. Mitotic recombination was demonstrated by tumour-specific, incomplete loss of heterozygosity, with no change in CN throughout the homozygous region. In tumour samples containing a heterogeneous population of normal and tumour cell DNA, regions of MR appeared as dual tracks of SNP calls on allele difference plots and were not called as LOH by the Genotyping Console. However, the copy number remained at 2, whereas heterozygous base calls were lost in comparison with blood. For these samples, an approximate recombination breakpoint was determined from the allele difference plots.
Chromosomal numbering is taken from the NCBI Build 36=hg18.
References
Boyd C, Smith MJ, Kluwe L, Balogh A, Maccollin M, Plotkin SR . (2008). Alterations in the SMARCB1 (INI1) tumor suppressor gene in familial schwannomatosis. Clin Genet 74: 358–366.
Carbone L, Harris RA, Vessere GM, Mootnick AR, Humphray S, Rogers J et al. (2009). Evolutionary breakpoints in the gibbon suggest association between cytosine methylation and karyotype evolution. PLoS Genet 5: e1000538.
De Raedt T, Maertens O, Chmara M, Brems H, Heyns I, Sciot R et al. (2006). Somatic loss of wild type NF1 allele in neurofibromas: Comparison of NF1 microdeletion and non-microdeletion patients. Genes Chromosomes Cancer 45: 893–904.
Dunham I, Shimizu N, Roe BA, Chissoe S, Hunt AR, Collins JE et al. (1999). The DNA sequence of human chromosome 22. Nature 402: 489–495.
Edelmann L, Pandita RK, Morrow BE . (1999). Low-copy repeats mediate the common 3-Mb deletion in patients with velo-cardio-facial syndrome. Am J Hum Genet 64: 1076–1086.
Evans DG, Huson SM, Donnai D, Neary W, Blair V, Newton V et al. (1992). A clinical study of type 2 neurofibromatosis. Q J Med 84: 603–618.
Gonzalez-Gomez P, Bello MJ, Alonso ME, Lomas J, Arjona D, Campos JM et al. (2003). CpG island methylation in sporadic and neurofibromatis type 2-associated schwannomas. Clin Cancer Res 9: 5601–5606.
Hadfield KD, Newman WG, Bowers NL, Wallace A, Bolger C, Colley A et al. (2008). Molecular characterisation of SMARCB1 and NF2 in familial and sporadic schwannomatosis. J Med Genet 45: 332–339.
Hulsebos TJ, Plomp AS, Wolterman RA, Robanus-Maandag EC, Baas F, Wesseling P . (2007). Germline mutation of INI1/SMARCB1 in familial schwannomatosis. Am J Hum Genet 80: 805–810.
James L, Varley J . (1996). Preparation, labelling and detection of DNA from archival tissue sections suitable for comparative genomic hybridization. Chromosome Res 4: 163–164.
James LA, Kelsey AM, Birch JM, Varley JM . (1999). Highly consistent genetic alterations in childhood adrenocortical tumours detected by comparative genomic hybridization. Br J Cancer 81: 300–304.
Kaplan JC, Aurias A, Julier C, Prieur M, Szajnert MF . (1987). Human chromosome 22. J Med Genet 24: 65–78.
Kino T, Takeshima H, Nakao M, Nishi T, Yamamoto K, Kimura T et al. (2001). Identification of the cis-acting region in the NF2 gene promoter as a potential target for mutation and methylation-dependent silencing in schwannoma. Genes Cells 6: 441–454.
MacCollin M, Willett C, Heinrich B, Jacoby LB, Acierno JS . (2003). Familial schwannomatosis: exclusion of the NF2 locus as the germline event. Neurology 60: 1968–1974.
Serra E, Rosenbaum T, Nadal M, Winner U, Ars E, Estivill X et al. (2001). Mitotic recombination effects homozygosity for NF1 germline mutations in neurofibromas. Nat Genet 28: 294–296.
Sestini R, Bacci C, Provenzano A, Genuardi M, Papi L . (2008). Evidence of a four-hit mechanism involving SMARCB1 and NF2 in schwannomatosis-associated schwannomas. Hum Mutat 29: 227–231.
Warren C, James LA, Ramsden RT, Wallace A, Baser ME, Varley JM et al. (2003). Identification of recurrent regions of chromosome loss and gain in vestibular schwannomas using comparative genomic hybridisation. J Med Genet 40: 802–806.
Acknowledgements
This work was supported by a grant from the Children's Tumor Foundation. The Department of Genetic Medicine is supported by the NIHR Manchester Biomedical Research Centre. We also thank all the patients who provided samples for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hadfield, K., Smith, M., Urquhart, J. et al. Rates of loss of heterozygosity and mitotic recombination in NF2 schwannomas, sporadic vestibular schwannomas and schwannomatosis schwannomas. Oncogene 29, 6216–6221 (2010). https://doi.org/10.1038/onc.2010.363
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2010.363
Keywords
This article is cited by
-
Correlation between genotype and phenotype with special attention to hearing in 14 Japanese cases of NF2-related schwannomatosis
Scientific Reports (2023)
-
A mechanistic mathematical model of initiation and malignant transformation in sporadic vestibular schwannoma
British Journal of Cancer (2022)
-
Brainstem intraparenchymal schwannoma with genetic analysis: a case report and literature review
BMC Medical Genomics (2021)
-
Why are olfactory ensheathing cell tumors so rare?
Cancer Cell International (2019)
-
Age-dependent copy number variations of TP53 tumour suppressor gene associated with altered phosphorylation status of p53 protein in sporadic schwannomas
Journal of Neuro-Oncology (2019)