Abstract
Objective
To investigate whether hospital rates of active treatment for infants born at 22–23 weeks is associated with survival of infants born at 24–27 weeks.
Study design
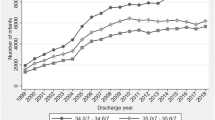
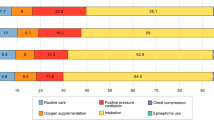
We included all liveborn infants 22–27 weeks of gestation delivered at California Perinatal Quality Care Collaborative hospitals from 2015 to 2019. We assessed (1) the correlation of active treatment (e.g., endotracheal intubation, epinephrine) in 22–23 week infants and survival until discharge for 24–27 week infants and (2) the association of active treatment with survival using multilevel models.
Result
The 22–23 week active treatment rate was associated with infant outcomes at 22–23 weeks but not 24–27 weeks. A 10% increase in active treatment did not relate to 24–25 week (adjusted OR: 1.00 [95% CI: 0.95–1.05]), or 26–27 week survival (aOR: 1.02 [0.95–1.09]).
Conclusion
The hospital rate of active treatment for infants born at 22–23 weeks was not associated with improved survival for 24–27 week infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data are available upon request and completion of requirements from CPQCC. Code is also available upon request.
References
United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Division of Vital Statistics. Natality public-use data 2016-2019, on CDC WONDER Online Database, October 2020. Accessed July 8, 2021. https://wonder.cdc.gov/controller/datarequest/D149;jsessionid=87F7F0097232707320A45E0DC8F2
Macdorman MF, Mathews TJ, Zeitlin J National Vital Statistics Report (Volume 63, Number 5 - September 24, 2014)—International Comparisons of Infant Mortality and Related Factors: United States and Europe, 2010. Vol 63.; 2014. Accessed August 14, 2020. http://www.oecd.org.
Raju TNK, Mercer BM, Burchfield DJ, Joseph GF. Periviable birth: Executive summary of a joint workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. Obstet Gynecol. 2014;123:1083–96. https://doi.org/10.1097/AOG.0000000000000243
Ecker JL, Kaimal A, Mercer BM, Blackwell SC, DeRegnier RAO, Farrell RM, et al. Periviable birth. Obstet Gynecol. 2017;130:e187–e199. https://doi.org/10.1097/AOG.0000000000002352
American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Periviable Birth. Obstet Care Consens. 2017;130.
Hajdu SA, Rossi RM, DeFranco EA. Factors associated with maternal and neonatal interventions at the threshold of viability. Obstet Gynecol. 2020;135:1398–408. https://doi.org/10.1097/AOG.0000000000003875
Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ, et al. Between-hospital variation in treatment and outcomes in extremely preterm infants. N Engl J Med. 2015;372:1801–11. https://doi.org/10.1056/NEJMoa1410689
Smith PB, Ambalavanan N, Li L, Cotten CM, Laughon M, Walsh MC, et al. Approach to infants born at 22 to 24 weeks’ gestation: Relationship to outcomes of more-mature infants. Pediatrics. 2012;129. https://doi.org/10.1542/peds.2011-2216
Morgan AS, Khoshnood B, Diguisto C, Foix L’Helias L, Marchand-Martin L, Kaminski M, et al. Intensity of perinatal care for extremely preterm babies and outcomes at a higher gestational age: Evidence from the EPIPAGE-2 cohort study. BMC Pediatr. 2020;20. https://doi.org/10.1186/s12887-019-1856-1
Gould JB. The role of regional collaboratives: The California perinatal quality care collaborative model. Clin Perinatol. 2010;37:71–86. https://doi.org/10.1016/j.clp.2010.01.004
Shih Z, Lee HC. Improving outcomes for preterm infants in the California Perinatal Quality Care Collaborative. Pediatr Med. 2019;2:54–54. https://doi.org/10.21037/pm.2019.10.03
California Perinatal Quality Care Collaborative. NICU Data Manual of Definitions. Accessed November 30, 2021. https://www.cpqcc.org/sites/default/files/2021 NICU Data Manual.pdf
Rysavy MA, Horbar JD, Bell EF, Li L, Greenberg LT, Tyson JE, et al. Assessment of an Updated Neonatal Research Network Extremely Preterm Birth Outcome Model in the Vermont Oxford Network. JAMA Pediatr. 2020;174. https://doi.org/10.1001/jamapediatrics.2019.6294
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34. https://doi.org/10.1016/S0022-3476(78)80282-0
Lee HC, Liu J, Profit J, Hintz SR, Gould JB Survival Without Major Morbidity Among Very Low Birth Weight Infants in California. Pediatrics. 2020;146. https://doi.org/10.1542/PEDS.2019-3865
Alexander G, Himes J, Kaufman R, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163–8. https://doi.org/10.1016/0029-7844(95)00386-X
CCS Approved Hospitals. Accessed November 19, 2021. https://www.dhcs.ca.gov/services/ccs/scc/Pages/SCCName.aspx
Rysavy MA, Mehler K, Oberthür A, Ågren J, Kusuda S, McNamara PJ, et al. An Immature Science: Intensive Care for Infants Born at ≤23 Weeks of Gestation. J Pediatr. 2021;233:16–25.e1. https://doi.org/10.1016/J.JPEDS.2021.03.006
Phibbs CS, Bronstein JM, Buxton E, Phibbs RH. the effects of patient volume and level of care at the hospital of birth on neonatal mortality. JAMA. 1996;276:1054–9. https://doi.org/10.1001/JAMA.1996.03540130052029
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med. 2007;356:2165–75. https://doi.org/10.1056/NEJMSA065029/SUPPL_FILE/NEJM_PHIBBS_2165SA1.PDF
Our Publications | California Perinatal Quality Care Collaborative. Accessed November 19, 2021. https://www.cpqcc.org/analysis/our-publications
Hagadorn JI, Bennett MV, Brownell EA, Payton KSE, Benitz WE, Lee HC. Covariation of neonatal intensive care unit-level patent ductus arteriosus management and in-neonatal intensive care unit outcomes following preterm birth. J Pediatr. 2018;203:225–233.e1. https://doi.org/10.1016/J.JPEDS.2018.07.025
Lee HC, Powers RJ, Bennett MV, Finer NN, Halamek LP, Nisbet C, et al. Implementation methods for delivery room management: a quality improvement comparison study. Pediatrics. 2014;134:e1378–e1386. https://doi.org/10.1542/PEDS.2014-0863
Handley SC, Steinhorn RH, Hopper AO, Govindaswami B, Bhatt DR, Van Meurs KP, et al. Inhaled nitric oxide use in preterm infants in California neonatal intensive care units. J Perinatol. 2016;36:635–9. https://doi.org/10.1038/JP.2016.49
Funding
Research reported in this manuscript was supported by the National Institutes of Health under award number R01HD098287. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
SB and HCL conceived and designed this work and drafted the manuscript. SB conducted the study analysis with input from all other co-authors (HL, MAR, SLC, TL, MB). All authors provided critical feedback on study design and interpretation of results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bane, S., Rysavy, M.A., Carmichael, S.L. et al. Does active treatment in infants born at 22–23 weeks correlate with outcomes of more mature infants at the same hospital? An analysis of California NICU data, 2015–2019. J Perinatol 42, 1301–1305 (2022). https://doi.org/10.1038/s41372-022-01381-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01381-x