Abstract
Objective
To determine the impact of neuroprotection interventions bundle on the incidence of severe brain injury or early death (intraventricular hemorrhage grade 3/4 or death by 7 days or ventriculomegaly or cystic periventricular leukomalacia on 1-month head ultrasound, primary composite outcome) in very preterm (270/7 to ≤ 296/7 weeks gestational age) infants.
Study design
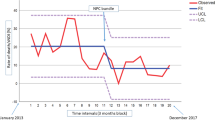
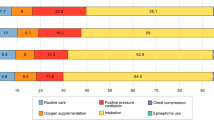
Prospective quality improvement initiative, from April 2017-September 2019, with neuroprotection interventions bundle including cerebral NIRS, TcCO2, and HeRO monitoring-based management algorithm, indomethacin prophylaxis, protocolized bicarbonate and inotropes use, noise reduction, and neutral positioning.
Result
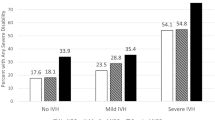
There was a decrease in the incidence of the primary composite outcome in the intervention period on unadjusted (N = 11/99, pre-intervention to N = 0/127, intervention period, p < 0.001) and adjusted analysis (adjusted for birthweight and Apgar score <5 at 5 min, aOR = 0.042, 95% CI = 0.003–0.670, p = 0.024).
Conclusions
Neuroprotection interventions bundle was associated with significant decrease in severe brain injury or early death in very preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Ment LR, Duncan CC, Ehrenkranz RA, Lange RC, Taylor KJ, Kleinman CS, et al. Intraventricular hemorrhage in the preterm neonate: timing and cerebral blood flow changes. J Pediatr. 1984;104:419–25.
Bolisetty S, Dhawan A, Abdel-Latif M, Bajuk B, Stack J, Lui K, et al. Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics 2014;133:55–62.
Payne AH, Hintz SR, Hibbs AM, Walsh MC, Vohr BR, Bann CM, et al. Neurodevelopmental outcomes of extremely low-gestational-age neonates with low-grade periventricular-intraventricular hemorrhage. JAMA Pediatr. 2013;167:451–9.
Pappas A, Adams-Chapman I, Shankaran S, McDonald SA, Stoll BJ, Laptook AR, et al. Neurodevelopmental and behavioral outcomes in extremely premature neonates with ventriculomegaly in the absence of periventricular-intraventricular hemorrhage. JAMA Pediatr. 2018;172:32–42.
Gotardo JW, Volkmer NFV, Stangler GP, Dornelles AD, Bohrer BBA, Carvalho CG. Impact of peri-intraventricular haemorrhage and periventricular leukomalacia in the neurodevelopment of preterms: A systematic review and meta-analysis. PLoS One. 2019;14:e0223427.
Mukerji A, Shah V, Shah PS. Periventricular/Intraventricular hemorrhage and neurodevelopmental outcomes: A meta-analysis. Pediatrics 2015;136:1132–43.
Twilhaar ES, Wade RM, de Kieviet JF, van Goudoever JB, van Elburg RM, Oosterlaan J. Cognitive outcomes of children born extremely or very preterm since the 1990s and associated risk factors: A meta-analysis and meta-regression. JAMA Pediatr. 2018;172:361–7.
Luu TM, Ment LR, Schneider KC, Katz KH, Allan WC, Vohr BR. Lasting effects of preterm birth and neonatal brain hemorrhage at 12 years of age. Pediatrics 2009;123:1037–44.
Volpe JJ. Neurobiology of periventricular leukomalacia in the premature infant. Pediatr Res. 2001;50:553–62.
Kusters CD, Chen ML, Follett PL, Dammann O. “Intraventricular” hemorrhage and cystic periventricular leukomalacia in preterm infants: how are they related? J Child Neurol. 2009;24:1158–70.
Vergani P, Locatelli A, Doria V, Assi F, Paterlini G, Pezzullo JC, et al. Intraventricular hemorrhage and periventricular leukomalacia in preterm infants. Obstet Gynecol. 2004;104:225–31.
Osborn DA, Evans N, Kluckow M. Hemodynamic and antecedent risk factors of early and late periventricular/intraventricular hemorrhage in premature infants. Pediatrics 2003;112:33–9.
Lee JY, Kim HS, Jung E, Kim ES, Shim GH, Lee HJ, et al. Risk factors for periventricular-intraventricular hemorrhage in premature infants. J Korean Med Sci. 2010;25:418–24.
Khwaja O, Volpe JJ. Pathogenesis of cerebral white matter injury of prematurity. Arch Dis Child Fetal Neonatal Ed. 2008;93:F153–61.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3:CD004454.
Kochan M, Leonardi B, Firestine A, McPadden J, Cobb D, Shah TA, et al. Elevated midline head positioning of extremely low birth weight infants: effects on cardiopulmonary function and the incidence of periventricular-intraventricular hemorrhage. J Perinatol. 2019;39:54–62.
Fowlie PW, Davis PG, McGuire W. Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants. Cochrane Database Syst Rev. 2010:CD000174. https://doi.org/10.1002/14651858.CD000174.pub2.
Rabe H, Gyte GM, Diaz-Rossello JL, Duley L. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2019;9:CD003248.
Kugelman A, Golan A, Riskin A, Shoris I, Ronen M, Qumqam N, et al. Impact of continuous capnography in ventilated neonates: A randomized, multicenter study. J Pediatr. 2016;168:56–61. e2
McCrea HJ, Ment LR. The diagnosis, management, and postnatal prevention of intraventricular hemorrhage in the preterm neonate. Clin Perinatol. 2008;35:777–92.
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355:2725–32.
Zilberberg MD, Shorr AF, Kollef MH. Implementing quality improvements in the intensive care unit: Ventilator bundle as an example. Crit Care Med. 2009;37:305–9.
Romantsik O, Bruschettini M, Ley D. Intraventricular hemorrhage and white matter injury in preclinical and clinical studies. Neoreviews. 2019;20:e636–e52.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Levene MI. Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch Dis Child. 1981;56:900–4.
Noori S, Anderson M, Soleymani S, Seri I. Effect of carbon dioxide on cerebral blood flow velocity in preterm infants during postnatal transition. Acta Paediatr. 2014;103:e334–9.
Kaiser JR, Gauss CH, Pont MM, Williams DK. Hypercapnia during the first 3 days of life is associated with severe intraventricular hemorrhage in very low birth weight infants. J Perinatol. 2006;26:279–85.
Alderliesten T, Dix L, Baerts W, Caicedo A, van Huffel S, Naulaers G, et al. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr Res. 2016;79:55–64.
Plomgaard AM, van Oeveren W, Petersen TH, Alderliesten T, Austin T, van Bel F, et al. The SafeBoosC II randomized trial: treatment guided by near-infrared spectroscopy reduces cerebral hypoxia without changing early biomarkers of brain injury. Pediatr Res. 2016;79:528–35.
Fairchild KD, Schelonka RL, Kaufman DA, Carlo WA, Kattwinkel J, Porcelli PJ, et al. Septicemia mortality reduction in neonates in a heart rate characteristics monitoring trial. Pediatr Res. 2013;74:570–5.
Bhat R, Zayek M, Maertens P, Eyal F. A single-dose indomethacin prophylaxis for reducing perinatal brain injury in extremely low birth weight infants: a non-inferiority analysis. J Perinatol. 2019;39:1462–71.
van Alfen-van der Velden AA, Hopman JC, Klaessens JH, Feuth T, Sengers RC, Liem KD. Effects of rapid versus slow infusion of sodium bicarbonate on cerebral hemodynamics and oxygenation in preterm infants. Biol Neonate. 2006;90:122–7.
Lokesh L, Kumar P, Murki S, Narang A. A randomized controlled trial of sodium bicarbonate in neonatal resuscitation-effect on immediate outcome. Resuscitation 2004;60:219–23.
Lightburn MH, Gauss CH, Williams DK, Kaiser JR. Observational study of cerebral hemodynamics during dopamine treatment in hypotensive ELBW infants on the first day of life. J Perinatol. 2013;33:698–702.
Graven SN. Sound and the developing infant in the NICU: Conclusions and recommendations for care. J Perinatol. 2000;20:S88–93.
Pellicer A, Gaya F, Madero R, Quero J, Cabanas F. Noninvasive continuous monitoring of the effects of head position on brain hemodynamics in ventilated infants. Pediatrics 2002;109:434–40.
Emery JR, Peabody JL. Head position affects intracranial pressure in newborn infants. J Pediatr. 1983;103:950–3.
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. J Nurs Care Qual. 2016;31:1–8.
Kribs A, Roll C, Gopel W, Wieg C, Groneck P, Laux R, et al. Nonintubated surfactant application vs conventional therapy in extremely preterm infants: A randomized clinical trial. JAMA Pediatr. 2015;169:723–30.
Thorp JA, Parriott J, Ferrette-Smith D, Meyer BA, Cohen GR, Johnson J. Antepartum vitamin K and phenobarbital for preventing intraventricular hemorrhage in the premature newborn: A randomized, double-blind, placebo-controlled trial. Obstet Gynecol. 1994;83:70–6.
McLendon D, Check J, Carteaux P, Michael L, Moehring J, Secrest JW, et al. Implementation of potentially better practices for the prevention of brain hemorrhage and ischemic brain injury in very low birth weight infants. Pediatrics 2003;111:e497–503.
Carteaux P, Cohen H, Check J, George J, McKinley P, Lewis W, et al. Evaluation and development of potentially better practices for the prevention of brain hemorrhage and ischemic brain injury in very low birth weight infants. Pediatrics 2003;111:e489–96.
Schmid MB, Reister F, Mayer B, Hopfner RJ, Fuchs H, Hummler HD. Prospective risk factor monitoring reduces intracranial hemorrhage rates in preterm infants. Dtsch Arztebl Int. 2013;110:489–96.
de Bijl-Marcus K, Brouwer AJ, De Vries LS, Groenendaal F, Wezel-Meijler GV. Neonatal care bundles are associated with a reduction in the incidence of intraventricular haemorrhage in preterm infants: A multicentre cohort study. Arch Dis Child Fetal Neonatal Ed. 2020;105:419–24.
Murthy P, Zein H, Thomas S, Scott JN, Abou Mehrem A, Esser MJ, et al. Neuroprotection care bundle implementation to decrease acute brain injury in preterm infants. Pediatr Neurol. 2020;110:42–8.
Ferreira DM, Girao ALA, AVS ES, Chaves EMC, de Almeida PC, Freire VS, et al. Application of a bundle in the prevention of peri-intraventricular hemorrhage in preterm newborns. J Perinat Neonatal Nurs. 2020;34:E5–E11.
Wallau CAK, Costa-Nobre DT, Leslie A, Guinsburg R. Impact of bundle implementation on the incidence of peri/intraventricular hemorrhage among preterm infants: a pre-post interventional study. Sao Paulo Med J. 2021;139:251–8.
Acknowledgements
We acknowledge the significant assistance of nurses and respiratory therapists in the neonatal intensive care unit at the University of Alabama Hospital for their contribution to this work, and the parents and infants in the RNICU.
Funding
No external funding was sought for the current study. We would like to thank the Perinatal Health and Human Development Research Program of the University of Alabama at Birmingham and the Children’s of Alabama Centennial Scholar Fund for supporting the divisional research projects.
Author information
Authors and Affiliations
Contributions
AK, MR, VS, WC, and NA, and were involved in the conceptualization of this study and in implementation of quality improvement initiatives. AB, SW, SY, AK, and VS were responsible for collecting data through chart review for this study. AFR, VS, MR were responsible for data analysis. All authors were involved in drafting and revising the paper and agree to be accountable for all aspects of the work and final approval of the version to be published. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Shukla, V.V., Klinger, A., Yazdi, S. et al. Prevention of severe brain injury in very preterm neonates: A quality improvement initiative. J Perinatol 42, 1417–1423 (2022). https://doi.org/10.1038/s41372-022-01437-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01437-y