Abstract
Cognitive impairment is prevalent in bipolar disorder (BD) but treatments with pro-cognitive effects are lacking. Insight concerning the neurocircuitry of cognitive improvement could provide a biomarker for pro-cognitive effects to advance treatment development. The dorsal prefrontal cortex (dPFC) is a promising region for such treatment target engagement. The aim of this functional magnetic resonance imaging (fMRI) study was to examine the effects of action-based cognitive remediation (ABCR) on early change in the dPFC blood-oxygen-level-dependent response in patients with BD in remission, and whether the observed neural change predicted improved executive functions following 10 weeks of treatment. Forty-five participants with remitted BD (ABCR: n = 26, control treatment: n = 19) completed a spatial n-back working memory task during fMRI and executive function tasks outside the scanner before and after two weeks of ABCR/control treatment, and an additional assessment of executive function at treatment completion. Thirty-four healthy controls underwent a single fMRI and executive function assessment for baseline comparisons. We found an early reversal of pretreatment hypo-activity in the dorsolateral prefrontal cortex (dlPFC) following ABCR vs. control during both high-load (2-back > 1-back) working memory (WM) (F(1,43) = 5.69, p = 0.02, η2 = 0.12) and general WM (2-back > 0-back) (F(1,43) = 5.61, p = 0.02, η2 = 0.12). This dlPFC activity increase predicted improved executive functions at treatment completion (high-load WM: B = −0.45, p = 0.01, general WM: B = −0.41, p < 0.01), independent of changes in subsyndromal symptoms. In conclusion, early dPFC increase may provide a neurocircuitry-based biomarker for pro-cognitive effects. Future cognition trials should include fMRI assessments to confirm the validity of this putative biomarker model across disorders with cognitive impairment.
Similar content being viewed by others
Introduction
Patients with bipolar disorder (BD) present with objective cognitive impairment even during asymptomatic phases1, which hampers their quality of life and functional capacity2,3. Currently, no treatment targeting cognitive impairment in BD has shown robust and enduring pro-cognitive efficacy. However, cognitive remediation (CR) has shown preliminary effects on cognition4. Specifically, a randomized controlled trial (RCT) of 24 weeks of computerized CR vs. computer control demonstrated effects on global cognition5, and a recent proof-of-concept study assessing the effects of 12 weeks of CR vs. TAU observed effects within specific cognitive domains6,7,8. We recently conducted an RCT to investigate the effects of 10 weeks of action-based cognitive remediation (ABCR) vs. control treatment on cognitive functions in patients with remitted BD with objective cognitive impairment9. While ABCR had no significant effect on a broad cognitive composite score, there was a large, specific effect on executive function9. The pro-cognitive effects of CR have mostly been studied in patients with schizophrenia, and are believed to be due to increased neuroplasticity10, that is accompanied by increased neural response in dorsal prefrontal cortex (dPFC) during working memory (WM) tasks11,12.
In the recent Strategic Plan for Research by the National Institute of Mental Health (NIMH) the first of four high-level goals is to define the brain mechanisms underlying complex behaviors, with the specific objective to elucidate the brain mechanisms underlying cognitive processes13. This need for greater insight into the neurocircuitry involved in cognitive functions and changes in cognition is further underscored by the International Society of Bipolar Disorders (ISBD) Targeting Cognition Task Force recommendations stating that clinical treatment studies should include functional magnetic resonance imaging (fMRI) to examine if early neural changes can predict subsequent treatment-related cognitive improvements8. Still, in a recent review of the neural substrates of cognition, only one study in BD involved fMRI data pre-treatment and post-treatment14. As such, despite the recommendations by the NIMH and the ISBD Targeting Cognition Task Force, there is a lack of fMRI studies elucidating the neurocircuitry of pro-cognitive effects.
The neural correlates of executive functions have commonly been examined with n-back paradigms that recruit WM functions such as strategic updating and monitoring of items. A systematic review of the neural activity during the n-back task in euthymic patients with BD found both hypo-activity (n = 5), hyper-activity (n = 2) and both hyper-activity and hypo-activity (n = 1) in the dPFC15. These discrepant findings are reconciled in an integrative model of the association between task difficulty and dPFC response based on a general bell-shaped load-response curve16. According to the model, patients display hyper-activity in the dPFC when task performance is maintained at a normal level, and dPFC hypo-activity when performance declines compared with controls16. Importantly, emerging evidence indicates that distinct candidate cognition treatments commonly modulate dPFC activity. Specifically, both CR and the multifunctional growth factor erythropoietin (EPO) increased dPFC activity in schizophrenia and mood disorders, which was associated with improved behavioral performance17,18,19,20,21,22,23. Conversely, the antidepressant vortioxetine reduced dPFC response in cognitively intact patients with remitted unipolar depression in the absence of cognitive performance changes24. These findings support our proposed distinction between treatment-related increase in neural efficiency—as reflected by dPFC activity reduction without change in performance levels—and in cognitive capacity—as reflected by dPFC activity increase coupled with improved performance16. These findings point to modulation of dPFC activity as a common systems-level neurocircuitry biomarker model for pro-cognitive effects that arise from treatment-related increase in neuroplasticity. If the model is validated and shows predictive validity in terms of cognitive improvement it could represent a key to examine the potential of candidate treatments as a middle step between preclinical studies and costly large scale phase III clinical trials25.
The aim of this fMRI report, including a subsample of patients from Ott et al.9 with longitudinal fMRI data, was to assess the predictive validity of early change in the dPFC blood-oxygen-level-dependent (BOLD) response for subsequent improvement in executive function in ABCR vs. control treatment in patients with BD in full or partial remission. In keeping with the model by Petersen and Miskowiak16, we hypothesize that increased executive function capacity in ABCR vs. control (i) will be accompanied by an early enhancement of the dPFC response during WM performance towards ‘normalization’ (i.e. baseline HC activity) and (ii) that early increase in dPFC will predict subsequent treatment-related improvement in executive function.
Materials and methods
Participants
Participants were recruited from psychiatric outpatient clinics (primarily the Copenhagen Affective Disorder Clinic) and consultant psychiatrists in the Capital Region of Denmark. Eligibility criteria were: an ICD-10 diagnosis of BD, full or partial remission (full remission: ≤7, partial remission: 8–14 on the Hamilton Depression Rating Scale-17 items (HDRS-17)26 and the Young Mania Rating Scale (YMRS)27, respectively), 18–55 years, fluent in Danish, and objective cognitive impairment (total scores ≤74 or below the cutoffs on ≥2 subtests on the Screen for Cognitive Impairment in Psychiatry28). Exclusion criteria were: current drug or alcohol abuse, daily use of benzodiazepines ≥22.5 mg, dyslexia, severe somatic illness, neurological illness, schizophrenia or a schizoaffective disorder, previous severe head trauma, pregnancy, pacemaker or other internal metal objects and electroconvulsive treatment within the past 3 months. Data from 34 HC with no personal or first-degree family history of psychiatric illness from the ongoing Bipolar Illness Onset (BIO) study29 were included to assess whether a treatment-related neural change in ABCR vs. control treatment was towards normalization defined as baseline HC activation levels. Executive function data from 39 HC were included from our SCIP-NORM study30 for comparison with the entire BD sample.
Randomization and masking
In this outcome-assessor blind trial, patients were randomized to the ABCR or the control treatment in a 1:1 allocation order using allocation envelopes provided by Pharma Consulting Group (Uppsala, Sweden) which were kept in a locked filing cabinet to prevent unblinding. Randomization was stratified by gender and age (< or ≥35 years) due to the association between age and neuroplasticity31. Upon inclusion, the primary therapist (CO) opened randomization envelopes in a consecutive manner. For power calculation for the primary outcome see the full protocol32.
Procedure
Data were collected at the Psychiatric Centre Copenhagen, Rigshospitalet. An fMRI scan and a comprehensive neuropsychological assessment were carried out at baseline and after two weeks of treatment, and executive function was assessed again at treatment completion (for details see ref. 32). Participants were informed about the study procedures and written consent was obtained. The study was approved by the local ethics committee (H-16043480) and the Danish Data Protection Agency (2012-58-0004).
Measures
Neuropsychological assessment
The secondary cognitive outcome in the trial was an executive function task: the One Touch Stockings of Cambridge (OTS)33. Specifically, the ‘mean choices to correct’ measure, with lower scores indicating better performance. The Spatial Working Memory (SWM)33 task was used to impute missing data from the n-back task inside the scanner. Due to a random scanner trigger, data from the n-back task inside the scanner was contaminated for 66% of the patient sample and 56% of the HC sample (see details in Supplementary methods 1).
Treatment groups
The ABCR program is a manual-based CR treatment developed by Professor Christopher Bowie, Queen’s University, Canada. The ABCR program provides a top-down approach to the restoration of cognitive impairment. Treatment duration was 10 weeks with two-hour sessions, twice a week and daily computer training at home. Each session included computerized training on the Danish version of Happy Neuron Pro (for English: www.happyneuronpro.com/en), a practical activity (e.g., order food at a café, remembering messages, etc.) and goal setting discussions to encourage participation in cognitively stimulating activities during daily life. The control group also had a duration of 10 weeks but with a weekly 1-h session. The control group was an unstructured conversation group, discussing themes relevant to patients and did not entail any cognitive training.
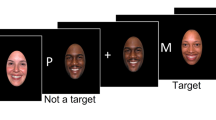
Spatial n-back fMRI task
A yellow circle would appear randomly in a 5 × 5 grid for 300 ms followed by an empty grid for 1200 ms. During the 0-back condition, the participants had to press a button on a response pad whenever the ball appeared in any of the grid corners. In the 1-back and 2-back conditions, the participants had to indicate whenever the ball appeared in the same grid square as one trial or two trials back, respectively. Each condition block had 14 trials (three targets) and was presented successively five times. Each block was interleaved by a fixation cross (8 s). Task duration was 7 min and 35 s.
fMRI data acquisition
Data were collected using a 3 Tesla Siemens Prisma scanner and a 64-channel head coil. The BOLD fMRI was acquired using a T2*-weighted gradient echo spiral echo-planar (EPI) sequence with an echo time (TE) of 30 ms, repetition time (TR) of 2 s, and flip angle of 90°. A total of 230 were acquired each consisting of 32 slices with a slice thickness of 3 mm with 25% gaps in-between, and a field of view (FOV) of 230 × 230 mm using a 64 × 64 grid. The BOLD images were registered to T1-weighted structural images (TR = 1900 ms; TE = 2.58 ms; flip angle = 9°; distance factor = 50%; FOV = 230 × 230 mm; slice thickness = 0.9 mm). We also acquired a B0 field map sequence with the same FOV and resolution as the BOLD sequence (TR = 400 ms; TE = 7.38 ms; flip angle = 60°) which was used for geometric distortion correction of the BOLD images.
fMRI data preprocessing and first-level
Data pre-processing and first-level analyses were conducted using fMRI Expert Analysis Tool (FEAT) version 6.034 from the FMRIB Software (FSL; http://www.fmrib.ox.ac.uk/fsl). Pre-processing included brain extraction, linear and nonlinear registration to structural space, spatial normalization to the Montreal Neurological Institute (MNI) standard space with 12 DOF, MCFLIRT motion correction, and spatial smoothing (Gaussian kernel full width half maximum = 5 mm FWHM). Registrations and 4D images were visually inspected, and upon motion outliers ≥ 2.0 mm, affected volumes were removed from the first-level statistical analyses. The time series were high pass-filtered (to max 0.008 Hz). We corrected for geometric distortions related to the B0 field based on the acquired B0 field map. Two conditions were modeled: 2-back > 1-back (high load-specific WM-related activity for assessment of the difference between 1-back and 2-back) and 2-back > 0-back (general WM-related activity). The conditions were convolved with a canonical hemodynamic response function.
fMRI group-level analysis
To investigate the early neural mechanisms of treatment-related executive function improvement, we first extracted mean percent BOLD signal change from a right dlPFC region of interest (ROI) based on the coordinates in Miskowiak, et al.23. The sphere had an 8 mm radius centered on (x = 40, y = 34, z = 29) and was constructed on an MNI template using tools within the FSL package. The mean percent BOLD signal change in the right dlPFC ROI was extracted using the FSL featquery tool for the contrasts 2-back > 1-back and 2-back > 0-back. A repeated measures ANOVA was conducted to assess any differential, longitudinal change between ABCR and control groups, with time as the within-subjects factor and group as the between-subjects factor. Significant interactions were followed-up with independent t tests or Mann–Whitney U tests (depending on the data distribution) and, for exploratory purposes, with post hoc paired samples t tests or Wilcoxon signed rank tests. Independent samples t tests or Mann–Whitney U tests were used to assess baseline activity in the dlPFC ROI for BD (and for the ABCR and the control groups separately) vs. HC.
Secondly, we conducted a FEAT analysis using a larger ROI of the entire dPFC. The dPFC ROI was defined on a standard MNI template in FSL to include the bilateral superior and medial frontal gyri, the superior portions of the anterior division of the cingulate gyrus and the frontal poles. We defined the ventral border of the dPFC by the area separating the dorsal from the ventral regions of medial PFC (MNI z > 5), defined according to Veit et al.35. The bilateral dPFC subregions were defined using probabilistic cortical maps thresholded at 5% provided by the Harvard-Oxford cortical structural Atlas36.
Main effect of task at baseline during 2-back > 1-back and 2-back > 0-back, respectively, was assessed in an exploratory whole-brain analysis across the entire patient group with a one sample t-test in FSL FEAT. Longitudinal interactions for ABCR vs. control across the whole brain and within the dPFC ROI as a pre-threshold mask for small volume correction were assessed with GLM models in FSL FEAT using a two-way mixed effects ANOVA. Post-hoc analyses assessing potential baseline differences for ABCR vs. control within the dPFC ROI during 2-back > 1-back and 2-back > 0-back were assessed with two-sample unpaired t tests. Baseline differences for BD (and exploratorily for the ABCR and the control groups separately) vs. HC within the dPFC ROI were assessed with two-sample unpaired t tests. All statistical models were estimated with the FMRIB’s local analysis of mixed effects (FLAME) 1 method. The significance level for clusters was set at p < 0.05 corrected for multiple comparisons using Gaussian Random Field (GRF) theory subsequent a cluster-forming threshold of z = 2.57 (p < 0.005). For clusters showing significant differential response to ABCR vs. control within the dPFC ROI and at a whole-brain level, the mean percent BOLD signal change were extracted for graphical illustration.
Behavioral data analysis
To assess the effect of ABCR vs. control treatment on executive function (OTS mean choices to correct), we conducted linear mixed-effect models. Factors were time, stratum (classifying age and gender) and treatment (control treatment as reference category). Fixed effects were time, stratum, time*stratum, and time*treatment. Baseline correction was applied. Independent t tests were used to assess differences between the BD vs. HC and the ABCR vs. control group, respectively, on executive functions and on performance on the spatial n-back task at baseline. n-back task performance was assessed by the discriminability index: d’ = ((number of hits + 0.5)/(total number of targets + 1))–((number of false alarms + 0.5)/(number of distractors + 1)) across 1-back and 2-back. To assess associations between change in WM-related neural activity and executive function, the change in extracted mean percent BOLD signal change was correlated with change on executive function from baseline to after two weeks of treatment and treatment completion, respectively. Significant correlations were followed up with multiple regression analyses, adjusting for change in depressive symptom severity from baseline to treatment completion, age, and gender, to assess whether early change in neural activity was predictive of later pro-cognitive effects. We planned a priori to not perform correlations between change in neural response and behavioral data from the n-back task in the scanner due to missing data following a technical error. Behavioral data was analyzed in SPSS version 25 and the α-level = 0.05.
Results
Patient flow and missing data
Randomization was carried out from July 2017–April 2019, data collection was completed in January 2020 (Supplementary Fig. 1 for CONSORT flowchart and MR exclusion reasons). Among the participants that received treatment (ABCR: n = 32, control: n = 29), fMRI data were analyzed for n = 26 (81%) ABCR participants and n = 19 (66%) control participants. Among the n = 45 patients with fMRI data, n = 44 (ABCR: n = 25, control: n = 19) had executive functions (OTS ‘mean choices to correct’) data at treatment completion. There were no significant differences between the sample with complete fMRI data (n = 45) and the sample without fMRI data (n = 16) on age, gender, mood symptoms, illness duration, hospitalizations, mood episodes, years of education, BD type, and verbal IQ (ps ≥ 0.23). There was no significant between-group difference in the time from the fMRI assessment at baseline to the fMRI assessment after two weeks of treatment (ABCR: Mdn = 21.5 days, interquartile range = 2, control: Mdn = 21.0, interquartile range = 2, U = 207, p ≥ 0.34).
Comparison of patient groups and the healthy control groups
The ABCR and control groups were well-balanced for demographic and clinical data, although more participants in the control group took antidepressants (p = 0.02) (Table 1). The BD group had fewer years of education and more subsyndromal mood symptoms than HC (ps ≤ 0.01) (Supplementary Table 1).
Behavioral results
In this subgroup of patients with fMRI data, we found again a significant effect of ACBR vs. control on executive function (OTS mean choices to correct) at treatment completion (treatment effect = −0.17, 95% CI[−0.30, −0.04], p = 0.01, Cohen’s d = 0.73), which had not emerged after two weeks of treatment (p = 0.66) (Table 2 for OTS scores). Exploratory analyses of the imputed n-back d’ data showed no differences at baseline or after two weeks of treatment between ABCR vs. control (ps ≥ 0.66) (Table 2). At baseline, the BD group performed worse on the n-back task (p < 0.01) than HC (Table 2).
Functional resonance imaging (fMRI) results
Dorsolatoral prefrontal cortex region-of-interest analysis
There was a statistically significant differential change in the right dlPFC response during high load specific WM (2-back > 1-back) for ABCR vs. control group (F(1,43) = 5.69, p = 0.02, η2 = 0.12); post hoc independent samples t tests/Mann–Whitney U tests: ps ≥ 0.12; post hoc paired samples t tests within each group separately indicated a non-significant trend towards a decrease in the control group: ABCR: p = 0.16, control: p = 0.06), with enhancement of the neural activity towards normalization in the ABCR group (Fig. 1). Similarly, there was a significant differential change in the right dlPFC response during general WM (2-back > 0-back for ABCR vs. control (F(1,43) = 5.61, p = 0.02, η2 = 0.12; post hoc independent samples t tests/Mann–Whitney U test: ps ≥ 0.16; exploratory post hoc paired samples t tests/Wilcoxon signed rank tests within each group showed that the interaction was driven by a significant increase in the ABCR group: Z = −2.2, p = 0.03, control: p = 0.42), with enhancement of the dlPFC response in the ABCR group also indicating normalization (Fig. 2).
A Dorsal prefrontal cortex (dPFC) region of interest (ROI) mask (light green). A priori region of interest (ROI) in the right dorsolateral prefrontal cortex (dlPFC) (dark green). Inferior frontal gyrus (IFG) and middle frontal gyrus (MFG) clusters identified in the dPFC ROI analysis showing differential longitudinal response to action-based cognitive remediation (ABCR) vs. control (yellow and orange). B Bar chart of change in mean % blood oxygen level-dependent (BOLD) signal change during high-load working memory (WM) at baseline and follow-up for the ABCR (red) and control (blue) groups within the right dlPFC, the IFG and the MFG. The bar charts of the change in mean % BOLD signal change within the IFG and the MFG are displayed for visual inspection to understand what drives the treatment × time interactions. Baseline change in the BOLD response displayed for the healthy controls (HC) (white) Bars show the mean; error bars show the SE. C Association between enhanced high load WM-related response of the right dlPFC ROI, MFG, and IFG dPFC ROI clusters (change scores calculated as ‘after two weeks of treatment–baseline’) and improved executive function.
A Neural network activated during general working memory (WM) load (2-back > 0-back) across all patients at baseline (light green). A priori region of interest (ROI) in the right dorsolateral prefrontal cortex (dlPFC) (dark green). Middle temporal gyrus cluster identified in the exploratory whole-brain analysis showing differential longitudinal response to action-based cognitive remediation (ABCR) vs. control (yellow and orange). B Bar chart of change in mean % blood oxygen level-dependent (BOLD) signal change during general WM at baseline and follow-up for the ABCR (red) and control (blue) groups within the right dlPFC and middle temporal gyrus. The bar chart of the change in mean % BOLD signal change within the middle temporal gyrus is displayed for visual inspection to understand what drives the treatment × time interaction. Baseline change in the BOLD response displayed for the healthy controls (HC) (white) Bars show the mean; error bars show the SE. C Association between enhanced general WM-related response of the right dlPFC ROI and the middle temporal gyrus cluster (change scores calculated as ‘after two weeks of treatment minus baseline’) and improved executive function.
dPFC region-of-interest analysis
There was a differential change in BOLD response in two clusters of the dPFC, the right middle frontal gyrus (MFG, BA 9), and inferior frontal gyrus (IFG, BA 46) during high load specific WM, reflecting enhanced activity over time in the ABCR vs. control group towards the baseline activity level of HC (normalization) (Fig. 1 for significant clusters and for graphs displaying extracted signal change for visualization purposes only, Table 3 for peak cluster activations). A post-hoc analysis showed no baseline differences for ABCR vs. control during high load specific WM. These neural changes in the dPFC during high load specific WM occurred in the absence of dPFC changes during general WM.
Whole brain exploratory analysis
Across the entire patient sample, a distributed task relevant network including the MFG, IFG and superior frontal gyrus, parietal and temporal regions were activated during high load specific WM, and during general WM, the insula and parietal lobe were activated (Table 3 for peak cluster activations). There was a significant effect of ABCR vs. control treatment in the right middle temporal gyrus (BA 21) (Fig. 2, Table 3 for peak cluster activations), with ABCR vs. control participants showing increased neural activity (towards normalization) (Fig. 2 for significant cluster and for graphs displaying extracted signal change for visualization purposes only).
BD vs. HC baseline WM-related activity
Within the dPFC ROI, BD patients displayed hypo-activity in bilateral superior frontal regions (BA 6) compared with HC (Table 3), which was also observed in the ABCR and the control groups separately. There was also a trend towards hypo-activity in the right dlPFC ROI during general WM (U = 586, p = 0.08) for BD vs. HC, with only the ABCR group showing hypo-activity in the right dlPFC ROI during general WM (U = 290, p = 0.02) when assessing the patient groups separately.
Associations between WM neural response and executive function
There was a significant correlation between increase in high-load specific WM-related right dlPFC response and improved executive function from baseline to treatment completion across the entire cohort (r(42) = −0.41, p = 0.006) and in the ABCR group alone (r(23) = −0.43, p = 0.03) (Fig. 1). Notably, this early increase in the right dlPFC response was the only significant predictor of improved executive function (B = −0.45, p = 0.01) (for change in subsyndromal depressive symptoms, age and gender: ps ≥ 0.35) across the entire cohort, and in the ABCR group (B = −0.44, p = 0.03; remaining predictors: ps ≥ 0.15), but not in the control group (ps ≥ 0.61) (Supplementary Table 2). There was also a significant correlation between increase in general WM-related right dlPFC response and improved executive function from baseline to treatment completion (r(42) = −0.49, p = 0.001) across the entire sample and in the ABCR group (r(23) = −0.59, p = 0.003) (Fig. 2). Again, the increase in the right dlPFC response was the only significant predictor of change in executive function across the entire cohort (B = −0.41, p < 0.01; remaining predictors: ps ≥ 0.25) and in the ABCR group (B = −0.52, p < 0.01) but not in the control group (ps ≥ 0.65) (Supplementary Table 2).
There was a correlation between increase in high load specific WM-related activity in the right MFG and IFG clusters within the dPFC ROI and improvement of executive function from baseline to treatment completion across the entire cohort (MFG: r(42) = −0.47, p = 0.001, IFG: r(42) = −0.47, p = 0.001, Fig. 1), which prevailed in the ABCR group (MFG: r(23) = −0.48, p = 0.02, IFG: r(23) = −0.48, p = 0.02). Further, the increase in high load specific WM-related right MFG and IFG gyrus were the only significant predictors of improved executive function from baseline to treatment completion across the entire cohort (MFG: B = −0.54, p < 0.01, IFG: B = −0.58, p < 0.01;for remaining predictors: ps ≥ 0.10) and in the ABCR group (MFG: B = −0.51, p < 0.01, IFG: B = −0.57, p = 0.04, for remaining predictors: ps ≥ 0.08), but not in the control group (ps ≥ 0.53) (Supplementary Table 2). Across the entire cohort, there was a correlation between increased general WM-related middle temporal gyrus response (exploratory whole-brain analysis) and improved executive function from baseline to treatment completion (r(42) = −0.51, p < 0.001), which prevailed in the ABCR group (r(23) = −0.58, p = 0.003) (Fig. 2).
Across the entire cohort, none of the associations between changes in high load specific or general WM-related neural activity and executive function had emerged after two weeks of treatment (ps ≥ 0.21). Finally, across the entire group, removing an outlier in the ABCR group did not change the significant associations between change in the dlPFC response (high-load and general WM), the dPFC response during high-load WM, the middle temporal gyrus response during general WM and change in executive functions (ps ≤ 0.03).
Discussion
This randomized fMRI study investigated the early neuronal activity changes within the dPFC after two weeks of ABCR vs. control treatment in patients with remitted BD and its association with subsequent improvement in executive functions after 10 weeks of treatment. The effect of ABCR vs. control treatment on executive function at treatment completion, seen in Ott et al. 9, was also observed in this subsample MR study. At baseline, patients with remitted BD displayed WM-related hypo-activity in the dPFC compared to healthy controls. Action-based cognitive remediation was associated with an early dPFC activity increase, towards HC activation levels at baseline (normalization), from baseline to after two weeks of treatment during high-load and general WM in comparison with control intervention. Further, early enhancement of the high load specific and general WM neural response predicted improved executive function at treatment completion, independent of changes in mood symptoms.
The findings converge with prior observations of treatment-related increase in dPFC activity and cognitive capacity in CR-studies in schizophrenia and mood disorders17,18,19,20,21,22,23. However, these studies involved fMRI assessments pre-intervention and post-intervention to explore the neural correlates of CR-related cognitive improvements rather than early neurocircuitry target engagement. We applied a novel design with follow-up fMRI assessment after only two weeks of treatment enabling investigation of whether the early treatment-related neural change was predictive of subsequent improved cognitive capacity after treatment completion. As expected, there was no statistically significant difference in executive function between the ABCR and the control group after two weeks of treatment, but there was a greater numerical improvement in the ABCR group, which reached significance at treatment completion. This indicates that treatment-related neural change is not merely an epiphenomenon of cognitive improvement but predates and may be mechanistically important for cognitive improvement.
The study has implications for validation of the putative neurocircuitry biomarker model for pro-cognitive effects proposed by Petersen and Miskowiak16. The model must meet five criteria: (i) respond to pro-cognitive treatments, (ii) produce similar effects in patients and HC, (iii) respond to different treatment modalities, (iv) be unresponsive to ineffective treatments, and (v) respond inversely to challenges with adverse cognitive effects37. These criteria have been used to validate the cognitive neuropsychological biomarker model of antidepressant drug action37. Similarly, an early enhancement of the dlPFC activity during cognitive performance may provide a sensitive biomarker for pro-cognitive effects14,16. Specifically, a shift in the dPFC activity has been demonstrated (i) following candidate cognition treatments18,19,20, (ii) following EPO infusions in HC, and (iii) following different treatment modalities (e.g. EPO and CR)23 but not (iv) in response to ineffective treatments38,39. Finally, in support of criterion (v), attenuated WM-related dPFC response coupled with impaired performance has been observed in female binge drinkers40.
The neurobiological basis for the cognitive impairments and aberrant dPFC activity in neuropsychiatric disorders is likely to originate from disruption of neuroplasticity, including altered GABAergic function, low-grade inflammation, glucocorticoid toxicity, oxidative stress and low levels of neurotrophins such as brain-derived neurotrophic factor (BDNF)41,42,43,44,45. In keeping with this, upregulation of neuroplasticity in response to distinct treatment modalities (e.g. EPO and CR) is likely to result in the common treatment-related dPFC activity change at a systems level in the brain12,23,46. In addition to the advancements of the neurocircuitry-based biomarker model, the findings of the study have implications for future cognition trials. In line with the ISBD Task Force recommendations, our findings suggest that future treatments would benefit from including fMRI-assessment of the dPFC activity change in clinical phase II trials. Notably, our study provides the first evidence that such early neural target engagement can predict subsequent cognitive improvement pointing to a mechanistic role of early dPFC modulation for interventions with efficacy on cognition that only emerges at a behavioral level after longer-term treatment. Although the findings provide a basis for mechanistically informed treatment development, it is not readily applicable for predicting treatment response at an individual level due to the large costs of fMRI scans and potential MR contraindications.
A limitation was that almost all patients received pharmacological treatment which could influence their neural response. However, a recent review assessing the neural substrates of WM in BD showed no clear effects of medication on WM-related neural activity15. Further, although the sample size was modest, it was larger than seven of nine pro-cognitive RCTs with pre- and post fMRI (range = [N = 12–56])17,18,19,20,21,22,23,24,47. Regarding lack of follow-up scans for the HC to assess ‘normalization’, the intra-individual stability of the BOLD signal in the dlPFC during the n-back following is high48. Finally, post hoc exploratory analysis indicated that the observed significant group by time interaction for high-load specific BOLD signal change in the right dlPFC ROI was partially driven by a trend towards a decreased dlPFC response over time in the control group.
In conclusion, there was an early enhancement of the WM-related dPFC activity in the ABCR vs. control groups, which predicted ABCR efficacy after 10 weeks of treatment. Together with evidence for similar effects of other candidate pro-cognitive interventions, the findings point to early dPFC activity change as a common neurocircuitry biomarker of pro-cognitive effects. If replicated in future pro-cognitive studies, this biomarker model could be implemented to inform go/no-go decisions in treatment development before embarking on larger-scale clinical efficacy trials.
Funding and disclosure
The study was supported by the Lundbeck Foundation (grant R215–20154121) awarded to Kamilla Miskowiak. The Lundbeck Foundation has not been involved in writing the present manuscript, the design of the study, the data collection, analysis, or interpretation of data. Kamilla Miskowiak holds a five-year Lundbeck Foundation Fellowship (grant R215–20154121) and a grant from the Weiman Foundation. KWM has received consultant fees from Lundbeck and Janssen-Cilag in the past three years. LVK has been a consultant for Lundbeck in the past three years. CRB has received honoraria from Boehringer Ingelheim, Lundbeck, Otsuka, and Abbie and is the developer of ABCR. CVO has received honoraria from Lundbeck. JM reports no conflicts of interest. GMK has received honoraria as a speaker for Janssen Pharmaceuticals and as an expert advisor for Sanos and Sage Pharmaceuticals. PMF reports no conflict of interest.
References
Cullen B, et al. Prevalence and correlates of cognitive impairment in euthymic adults with bipolar disorder: a systematic review. J Affect Disord. 2016;205:165–81.
Wingo AP, Harvey PD, Baldessarini RJ. Neurocognitive impairment in bipolar disorder patients: functional implications. Bipolar Disord. 2009;11:113–25.
Brissos S, Dias VV, Kapczinski F. Cognitive performance and quality of life in bipolar disorder. Can J Psychiatry. 2008;53:517–24.
Tsapekos D, et al. Cognitive enhancement interventions for people with bipolar disorder: a systematic review of methodological quality, treatment approaches, and outcomes. Bipolar Disord. 2019:216–30.
Lewandowski KE, et al. Treatment to enhance cognition in bipolar disorder (TREC-BD): efficacy of a randomized controlled trial of cognitive remediation versus active control. J Clin Psychiatry. 2017;78:e1242–e49.
Strawbridge R, et al. Cognitive remediation therapy for patients with bipolar disorder: a randomised proof-of-concept trial. Bipolar Disord. 2020:1–17.
Miskowiak KW, Carvalho AF, Vieta E, Kessing LV. Cognitive enhancement treatments for bipolar disorder: a systematic review and methodological recommendations. Eur Neuropsychopharmacol. 2016;26:1541–61.
Miskowiak KW, et al. Methodological recommendations for cognition trials in bipolar disorder by the International Society for Bipolar Disorders Targeting Cognition Task Force. Bipolar Disord. 2017;19:614–26.
Ott CV, Vinberg M, Kessing LV, Bowie CR, Forman JL, Miskowiak KW. Effect of Action‐Based Cognitive Remediation on cognitive impairment in patients with remitted bipolar disorder: a randomized controlled trial. Bipolar Disord. 2020;00:1–13. https://doi.org/10.1111/bdi.13021.
Keshavan MS, Vinogradov S, Rumsey J, Sherrill J, Wagner A. Cognitive training in mental disorders: update and future directions. Am J Psychiatry. 2014;171:510–22.
Minzenberg MJ, Laird AR, Thelen S, Carter CS, Glahn DC. Meta-analysis of 41 functional neuroimaging studies of executive function in schizophrenia. Arch Gen Psychiatry. 2009;66:811–22.
Ramsay IS, MacDonald AW III. Brain correlates of cognitive remediation in schizophrenia: activation likelihood analysis shows preliminary evidence of neural target engagement. Schizophr Bull. 2015;41:1276–84.
U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health. (2020). NIMH Strategic Plan for Research (NIH Publication No. 20-MH-8096). Retrieved from https://www.nimh.nih.gov/about/strategic-planning-reports/2020_nimh_strategic_plan_508_160162.pdf.
Miskowiak KW, Petersen CS. Neuronal underpinnings of cognitive impairment and—improvement in mood disorders. CNS Spectr. 2019;24:30–53.
Cremaschi L, et al. Assessing working memory via N-back task in euthymic bipolar I disorder patients: a review of functional magnetic resonance imaging studies. Neuropsychobiology. 2013;68:63–70.
Petersen CS, Miskowiak KW. Toward a transdiagnostic neurocircuitry-based biomarker model for pro-cognitive effects: challenges, opportunities, and next steps. CNS Spectr. 2020:1–5. https://doi.org/10.1017/S1092852920000061.
Wykes T, et al. Effects on the brain of a psychological treatment: cognitive remediation therapy: functional magnetic resonance imaging in schizophrenia. Br J Psychiatry. 2002;181:144–52.
Haut KM, Lim KO, MacDonald A III. Prefrontal cortical changes following cognitive training in patients with chronic schizophrenia: effects of practice, generalization, and specificity. Neuropsychopharmacology. 2010;35:1850–9.
Bor J, et al. How can cognitive remediation therapy modulate brain activations in schizophrenia? An fMRI study. Psychiatry Res. 2011;192:160–6.
Subramaniam K, et al. Intensive cognitive training in schizophrenia enhances working memory and associated prefrontal cortical efficiency in a manner that drives long-term functional gains. NeuroImage. 2014;99:281–92.
Meusel LA, Hall GB, Fougere P, McKinnon MC, MacQueen GM. Neural correlates of cognitive remediation in patients with mood disorders. Psychiatry Res. 2013;214:142–52.
Ramsay IS, Nienow TM, Marggraf MP, MacDonald AW. Neuroplastic changes in patients with schizophrenia undergoing cognitive remediation: triple-blind trial. Br J Psychiatry. 2017;210:216–222.
Miskowiak KW, et al. Neural correlates of improved executive function following erythropoietin treatment in mood disorders. Psychol Med. 2016;46:1679–91.
Smith J, et al. Vortioxetine reduces BOLD signal during performance of the N-back working memory task: a randomised neuroimaging trial in remitted depressed patients and healthy controls. Mol Psychiatry. 2018;23:1127–33.
Millan MJ, et al. Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov. 2012;11:141–68.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35.
Jensen JH, et al. Optimising screening for cognitive dysfunction in bipolar disorder: validation and evaluation of objective and subjective tools. J Affect Disord. 2015;187:10–9.
Kessing LV, et al. The Bipolar Illness Onset study: research protocol for the BIO cohort study. BMJ Open. 2017;7:e015462.
Ott CV, et al. Norms for the screen for cognitive impairment in psychiatry and cognitive trajectories in bipolar disorder. 2020 (in press).
Park DC, Bischof GN. The aging mind: neuroplasticity in response to cognitive training. Dialogues Clin Neurosci. 2013;15:109–19.
Ott CV, et al. Effect of action-based cognitive remediation on cognition and neural activity in bipolar disorder: study protocol for a randomized controlled trial. Trials 2018;19:487.
Cambridge Cognition. wwwcantabcom. 2019.
Woolrich MW, Ripley BD, Brady M, Smith SM. Temporal autocorrelation in univariate linear modeling of FMRI data. NeuroImage. 2001;14:1370–86.
Veit R, et al. Aberrant social and cerebral responding in a competitive reaction time paradigm in criminal psychopaths. NeuroImage. 2010;49:3365–72.
Desikan RS, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage. 2006;31:968–80.
Harmer CJ, Cowen PJ, Goodwin GM. Efficacy markers in depression. J Psychopharmacol. 2011;25:1148–58.
Demant KM, Vinberg M, Kessing LV, Miskowiak KW. Effects of short-term cognitive remediation on cognitive dysfunction in partially or fully remitted individuals with bipolar disorder: results of a randomised controlled trial. PLoS ONE. 2015;10:e0127955.
Macoveanu J, et al. Towards a biomarker model for cognitive improvement: no change in memory-related prefrontal engagement following a negative cognitive remediation trial in bipolar disorder. J Psychopharmacol. 2018;32:1075–85.
Squeglia LM, Schweinsburg AD, Pulido C, Tapert SF. Adolescent binge drinking linked to abnormal spatial working memory brain activation: differential gender effects. Alcohol Clin Exp Res. 2011;35:1831–41.
Keshavan MS, Mehta UM, Padmanabhan JL, Shah JL. Dysplasticity, metaplasticity, and schizophrenia: Implications for risk, illness, and novel interventions. Dev Psychopathol. 2015;27:615–35.
Kapczinski F, Frey BN, Kauer-Sant’Anna M, Grassi-Oliveira R. Brain-derived neurotrophic factor and neuroplasticity in bipolar disorder. Expert Rev Neurother. 2008;8:1101–13.
Maas DA, Valles A, Martens GJM. Oxidative stress, prefrontal cortex hypomyelination and cognitive symptoms in schizophrenia. Transl Psychiatry. 2017;7:e1171.
Benedetti F, Aggio V, Pratesi ML, Greco G, Furlan R. Neuroinflammation in bipolar depression. Front Psychiatry. 2020;11:71. Published 2020 Feb 26. https://doi.org/10.3389/fpsyt.2020.00071.
Young AH. The effects of HPA axis function on cognition and its implications for the pathophysiology of bipolar disorder. Harv Rev Psychiatry. 2014;22:331–3.
Vinogradov S, Fisher M, de Villers-Sidani E. Cognitive training for impaired neural systems in neuropsychiatric illness. Neuropsychopharmacology. 2012;37:43–76.
Haldane M, et al. Changes in brain activation during working memory and facial recognition tasks in patients with bipolar disorder with Lamotrigine monotherapy. Eur Neuropsychopharmacol. 2008;18:48–54.
Plichta MM, et al. Test-retest reliability of evoked BOLD signals from a cognitive-emotive fMRI test battery. NeuroImage. 2012;60:1746–58.
Acknowledgements
We wish to acknowledge the Copenhagen Affective Disorder Clinic, Rigshospitalet, Copenhagen, Denmark for assistance with recruitment, and specialist in psychotherapy Nanna Tuxen for her involvement in the ABCR treatment. The computer software used in the ABCR group is provided free of charge by HappyNeuron Pro (www.happyneuronpro.com).
Author information
Authors and Affiliations
Contributions
KWM conceived the study, wrote the study protocol and obtained the required funding for the study. LVK and CRB contributed to the study design and revising the study protocol. KWM, JM, GMK, and PMF set up the fMRI paradigm. CRB developed the ABCR intervention for this patient group following discussions with KWM, and trained CVO and KWM in delivering the treatment. CVO, KWM, and LVK contributed to the recruitment of participants. CVO was responsible for delivering the treatments and data collection. CVO analyzed and interpreted the data under the supervision of KWM and JM. CVO drafted the manuscript which was revised by KWM. All authors have contributed to and approved the final version of the manuscript.
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ott, C.V., Macoveanu, J., Bowie, C.R. et al. Change in prefrontal activity and executive functions after action-based cognitive remediation in bipolar disorder: a randomized controlled trial. Neuropsychopharmacol. 46, 1113–1121 (2021). https://doi.org/10.1038/s41386-020-00901-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-020-00901-7