Abstract
Gas in scattering media absorption spectroscopy (GASMAS) is a novel optical technology employing near-infrared light. It has a potential use in the medical setting as a monitoring and diagnostic tool by detecting molecular oxygen within gas pockets and thus may be a useful adjunct in respiratory monitoring. GASMAS has potential advantages over other monitoring devices currently used in clinical practice. It is a non-invasive, continuous, non-ionising technology and provides unique information about molecular oxygen content inside the lungs. GASMAS may have a future role in optimising respiratory management of neonates in different clinical scenarios such as monitoring cardiorespiratory transition in the delivery room, assessing surfactant deficiency, and optimising endotracheal tube positioning. This article aims to summarise current evidence exploring GASMAS application in a neonate, discuss possible clinical benefits, and compare with other devices that are currently used in neonatal care.
Impact
-
This article presents a novel optical technique to measure lung oxygen concentrations that may have important clinical uses.
-
This review summarises the current literature investigating the concept of optical lung oxygen measurement.
-
Information from this review can guide researchers in future studies.
Similar content being viewed by others
Introduction
Medical applications of laser light technology are an ever-expanding area, enabling the improvement of non-invasive diagnostic and treatment techniques in different areas of medicine. In particular, a technique such as gas in scattering media absorption spectroscopy (GASMAS) has the potential to become a beneficial respiratory monitoring tool in clinical practice. Initially, GASMAS has been employed in different commercial areas (e.g., food,1,2,3,4 pharmaceutical industries5,6,7) helping to detect, measure and analyse gas trapped inside diffuse materials. More recent in vitro and in vivo studies evaluated the concept of non-invasive oxygen detection inside biological tissues like sinuses,8,9,10,11,12,13 middle ear,14,15 femoral bone16 and lungs. Different lung phantom models were used for GASMAS measurements, such as porcine lung samples,17 or produced by 3D printing nylon shells filled with tissue optical phantom material and air18,19 or structured sponge.20 An in vivo study has demonstrated GASMAS effectiveness in detecting pneumothorax and lung collapse in ventilated piglets.21 Following feasibility studies involving infants,22,23 GASMAS have been identified as a potential respiratory monitoring tool that might play a role in neonatology, managing infants in delivery room and intensive care units, where quantitative, non-invasive bedside monitoring of sick newborn infants is essential.
Respiratory illness is the most common indication for admission to the neonatal unit.24 Whilst up to 10% of term and late preterm infants born between 34 and 40 weeks gestational age can have respiratory problems,24 more than 80% of infants born before 28 weeks will require respiratory support.25 Reasons include delayed clearance of foetal lung fluid or aspiration of meconium for term babies and surfactant deficiency for premature neonates,26,27 compromising oxygen diffusion, absorption and subsequently resulting in decreased blood oxygen levels.
Neonatal respiratory status is currently monitored using continuous pulse oximetry (PO), intermittent blood sampling, and X-ray imaging. These methods cannot measure oxygen concentration or lung volume directly and carry some short and long-term risks.28,29 Optical oxygen concentration measurements present a clinical and diagnostic advantage allowing fast and non-invasive detection of suboptimal oxygen concentrations within the lung, subsequently allowing prevention of potential respiratory complications.
Currently, there is no commercially available GASMAS-based monitoring/diagnostic method that could be used in clinical practice to assess real-time regional ventilation and oxygen content at the bedside on a continuous basis.
This review article aims to summarise current evidence exploring neonatal oxygen monitoring of the lungs, discuss possible clinical applications of a novel GASMAS-based device and compare with other devices/techniques that are currently used in neonatal units.
Gas in scattering media absorption spectroscopy
The most recurrent interactions between light and tissue are absorption and scattering (Supplementary 1 and 2). Characteristics of these interactions have been employed to develop optical technology called GASMAS. It is a technique, which measures the concentration of gas inside diffuse substances like biological tissue, relying on the difference between the absorption spectra of molecular gas and condensed matter (solids and liquids).30 A usual absorption band of biological tissue is 101 nm broad versus 10−4 nm for gases. For a GASMAS measurement, a narrow-band diode laser at a specific wavelength is scanned across a characteristic gas absorption line to interrogate the material and gas pockets contained within.
The diffuse light emerging from this media carries the spectroscopic information about the gas that it passed through, which is recorded by a detector/sensor placed away from the light source. This information is used to calculate the gas concentration by means of the Beer–Lambert law, which states that the intensity of the emerging light (I), propagating through gas with concentration (c) and absorption cross-section (ε) along an optical path length (l), decays in an exponential way.
In cases where the optical path length (l) of the gas is unknown, a dual diode laser source is used to interrogate a reference gas present in the same cavity (e.g., water vapour). The optical path length can be assumed equal for both gases if their absorption bands are spectrally close.
The novel clinical application of GASMAS technology is targeting the detection of molecular oxygen (O2) and water (H2O) vapour, common gases inside human body cavities, e.g., lung tissue. It uses a dual laser source with 760 and 935 nm to measure absorption signals from molecular O2 and H2O vapour, respectively. The concentration of H2O vapour in a cavity with 100% relative humidity and known central body temperature (like a neonate’s lung) can be calculated using the Arden Buck equation.31,32 Therefore, H2O vapour is used as a reference gas to estimate the optical path length and calculate the O2 concentration. Devices for the clinical application have the probe with integrated laser fibres attached to the skin as a light source and detector probe with the photosensitive area (Figs. 1 and 2).
1 – Dual laser source; 2 – Data acquisition and laser control module; 3 – PC; 4 – Signal pre-amplifier; 5 – Reference measurement cube; 6 – Fibre interference eliminator; 7 – Optical fibre; 8 – Light source probe (emitter); 9 – Diffuse light passing through the lung tissue; 10 – Photosensitive detector probe; 11 – Electric cable; 12 – Neonatal lung.
a, b Skin placement of the probes overlying lung area. LS - light source probe, DP - detector probe. c, d Illustration of light distribution using thoracic CT images of a full-term 4-week-old newborn as an example. Parental consent to use images obtained. Pink-coloured areas represent the approximate extent of near-infrared light illumination used for GASMAS. Given the difficulties in predicting photon migration, the areas of light illumination are not necessarily the same as the areas of light detection.
Oxygen measurement using GASMAS technology in clinical setting
GASMAS applications in adult medicine
GASMAS have been applied in several feasibility studies to describe common adult diseases, like sinusitis, otitis media and osteonecrosis of femoral head. Sinusitis is an inflammatory condition resulting in a blockage of normal gas drainage and affecting the gas volume and content inside the sinus cavity due to mucosal swelling and production of secretions. The resulting blockage of normal gas drainage affects the gas volume inside the sinus cavity.
Persson et al. used two plastic plates simulating light transmission through sinuses. One plate acted as a human facial bone-muscle layer, and another plate like the base of the sinus cavity composed of mucous membranes and bone. By altering the thickness of the plates and the distance between them, it was possible to show that the O2 absorption signal was proportional to the distance between plates and O2 volume, thus allowing the detection of reduced gas content in cases of sinus pathology.8 Later Persson et al. demonstrated that GASMAS can be used to detect O2 within the maxillary and frontal sinuses in 11 volunteers. No O2 signal was detected where the volunteer was experiencing recurrent sinus issues. Also, the gas exchange process inside the sinus cavity has been investigated by flushing the sinuses with nitrogen, which cleared the cavity from O2. It has shown a ‘real-time’ O2 signal drop, indicating normal gas drainage due to non-obstructed connections between air pockets.9 Frontal sinus H2O signal repeatability analysis demonstrated that the recorded values remain consistent within one day or 6-day span with persistent right and left asymmetry.13 Further investigations have shown, that several gases (H2O vapour and O2) can be detected simultaneously.11
Thirty-one patients with suspected mastoid sinus pathology underwent laser spectroscopy measurements and the results were compared with subsequently performed computer tomography (CT) scans. Correlation was found between sinus volume based on CT scan grading and H2O vapour absorption imprints (r2 = 0.69, 47% of variance related). Weak reproducibility has been demonstrated for H2O vapour and molecular O2. Although, all cases with radiological signs of mastoid pathology were identified with laser spectroscopy.12
Middle ear phantoms have been used to prove the concept of GASMAS ability to detect changes consistent with otitis media diagnosis when air volume behind eardrum reduces due to increment secretions. O2 signal increases when flushing the phantom middle ear cavity with pure O2 and stays stable over time. It decreases gradually when opening the orifice of the cavity and reduces when flushed with nitrogen, demonstrating the relation between the signal and O2 concentration.14,15
Chen et al. demonstrated the role of GASMAS in the early detection of osteonecrosis of the femoral head. Femoral head decay is associated with forming of air-filled pores replacing normal vessels, which can be detected using GASMAS. Eighteen hip samples obtained after routine joint replacement surgery were investigated. Eleven of them were affected by osteonecrosis. Comparing water vapour signals from normal bones and affected, a significant difference (P < 0.05) was found illustrating in vitro detection efficacy. In vivo studies using arthroscopy with integrated laser is to follow by this research group.16
Laser spectroscopy studies with infants
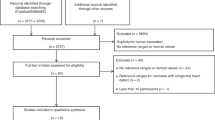
The first feasibility study performing lung measurements enrolled three healthy term-born babies. The study aimed to investigate the quality of signal detected by probes placed in different locations on the chest and abdomen. Most of the O2 and H2O signal received by the detector probe was weak. Poor signal quality was likely related to the thickness of the probed tissue. Because the measurements were performed on older babies (weighing above 4 kg) with a thicker subcutaneous layer, the light was likely to be scattered and attenuated before reaching the detector. However, one position gave a clear absorption signal for H2O vapour, with the laser source probe below the collar bone and detector just below the armpit. Few abdominal light source-detector positions were suitable to detect H2O vapour. The probe separation and absorption signal quality relationship was demonstrated by computer simulations.33,34
A subsequent study recruited 29 full-term healthy infants and obtained 390 lung optical measurements. The power of laser used for O2 detection has increased significantly (30 mW), compared to previous studies. A total of 60% of all measurements revealed good quality signals (SNR > 3), and O2 was detected at least once in each baby.23 Nevertheless, investigators suggested the need for technical improvements for the future development of a clinical device.
GASMAS safety
The International Electrotechnical Commission and the American National Standards Institute have published a standard that outlines the safety of laser products. Laser light at the wavelengths and power level used for GASMAS falls under Class I category that is considered safe and presents no hazard to the eye or the skin under direct exposure. Laser light is coupled to the skin using a diffuser, which spreads the light over the larger surface area over the skin, reducing power density and maintaining skin and eye safety.
In previous animal and human models, the safety of the device hasn’t been reported. This is particularly important when applying long-term monitoring of vulnerable populations such as newborn, especially preterm babies that have immature skin. This needs to be factored into future study designs.
Optical lung measurement versus other instrumental lung assessment techniques
Table 1 provides a comparative overview of the various technologies for lung evaluation available in the neonatal clinical setting.
Chest X-ray is the most common method of evaluating the lung status of newborns. Radiologic appearance of different neonatal lung pathologies can be non-specific,35 and is caused by different constituents remaining inside the alveoli: hyaline membrane, foetal lung fluid or meconium. Gaining more information about the optical features of lung constituents may lead to the development of light-based technologies to enable more specific differentiation.
Lung ultrasound provides the possibility to image air-filled or collapsed parts of the lungs and is now more often utilised in neonatal units.36,37,38,39,39 While there are defined diagnostic criteria available for differentiation of various neonatal respiratory pathologies40 obtaining and interpreting these images requires training and a new skill set for the operators.
Lung CT greatly improves imaging of the pulmonary parenchymal and airway pathology and is considered as the gold standard for lung evaluation. Unfortunately, CT delivers significant concentrations of radiation compared to other radiological imaging techniques and has been found to be associated with increased risk for intracranial tumours.41 Furthermore, chest CT is resource and time intensive, requiring skilled personnel and effective patient immobilisation.42
While magnetic resonance imaging is generally considered safer than CT, its uses for neonatal lung evaluation are predominantly restricted to research settings only as spatial resolution quality is inferior to CT. Moreover, patient sedation is often necessary to avoid movement artefacts. Unlike the described radiological technologies, GASMAS would allow continuous monitoring at the cot side with comparatively easy interpretation of the results. In addition, GASMAS enables the detection of O2 at the molecular level and, with advancing technology, could also be used to analyse gas mixtures of O2, nitric oxide, or carbon dioxide.43
Optical lung measurement versus other optical oxygen monitoring techniques: pulse oximetry and near-infrared spectroscopy
Neonatologists are familiar with other optical devices used daily in the neonatal units such as PO44 and near-infrared spectroscopy (NIRS). It is important to acknowledge the differences between PO, NIRS and GASMAS to understand how this new technology would add additional information about the overall O2 status of a neonate and what information is still missing to validate GASMAS. The main technical differences between these optical devices are demonstrated in Supplementary Fig. S3.
PO is used for continuous monitoring of the pulsatile haemoglobin bound O2 saturation (SpO2) signal that is a product of gas exchange at the alveolar level present in a peripheral vascular bed, while GASMAS targets free O2 molecules inside the gas pockets of the alveoli before they diffuse through the pulmonary capillaries and bind to haemoglobin. The light source of PO is emitting red and near-infrared light at the wavelengths specific to the absorption of deoxygenated (HHb) and oxygenated haemoglobin (HbO2). A single detector is positioned using diffuse transmittance geometry on the opposite side of the palm, wrist, feet, or ankle. Measurements obtained are dependent on pulsatile activity: light absorption changes with increasing blood volume present under the light emitter during systolic phase of cardiac cycle and reduces with diastole. As most of these rhythmic changes are associated with arterial vessel dilatation and constriction, PO is calculating arterial O2 saturation, based on red and infrared light absorption ratio. If pulse signal is lost (e.g., due to probe displacement or in cases of non-pulsatile or bradycardic conditions), measurement of SpO2 becomes unreliable.45
NIRS is used to monitor regional tissue oxygenation status, most commonly assessing neonatal brain tissue, by placing the probe on the infant’s forehead. It operates using the non-pulsatile, continuous wave (CW) signal within the same tissue optical window (Supplementary Fig. S2), penetrating brain tissue to a depth of 1–3 cm.46 Unlike PO, NIRS values are based predominantly on venous HbO2 saturation rather than arterial, because most of the haemoglobin is found within the venous compartment.47
NIRS measurements can be achieved using three different modes: CW, frequency domain (FD) or time domain (TD).48,49 CW-NIRS uses a single emitter delivering steady light and two or more detectors with a specific distance. The photodetector is sensing the light coming back from the tissues after interacting with HbO2 and HHb. Analysing the ratio between the intensity and frequency of diffusely reflected light it calculates the regional percentage of brain O2 saturation (RStO2).46
TD-NIRS relies on the ability to measure the photon distribution of time-of-flight in a diffuse media, following the emission of pulsed light with a duration of tens of picoseconds. Analytical algorithms provide values of HbO2, HHb, total amount of haemoglobin and RStO2, by estimating the absorption coefficient at two or more wavelengths.50
NIRS measurements incorporating FD use multiple emitter-detector pairs and estimate absolute values by evaluating phase shift and time-of-flight information.
GASMAS measurements are performed using two wavelength light sources specific to H2O vapour and molecular O2 absorption and a single detector. It is not targeting the absorption differences between HbO2 and HHb, like PO and NIRS. The calculation of O2 concentration using GASMAS is described in paragraph 2. While the distance between the emitter and detector as well as geometry (reflectance or transmittance) are well defined in PO and NIRS, there is a lack of studies confirming optimal probe placement for GASMAS measurements. Furthermore, optimal positioning on the chest is not well validated (Supplementary Table S1). Other factors that possibly would influence signal detection, like patient movement, cardiac contractility, breathing activity have not been investigated to date.
Potential clinical applications of GASMAS in neonatal care
Cardiorespiratory transition monitoring in the delivery room
Current clinical practice to maintain optimal oxygenation of a preterm baby in the delivery room is based on SpO2 and electrocardiogram derived heart rate values. Not reaching an SpO2 of 80% at 5 min postnatally was found to be associated with adverse outcomes, including intraventricular haemorrhage.51 It has been shown that despite using SpO2 and heart rate-driven O2 titration strategies, many infants spend a significant portion of time outside of the targeted O2 saturation range.52,53 Delayed availability of PO values,54 inaccurate values in bradycardic situations and lack of information about the actual efficacy of lung ventilation and aeration contribute to this finding. Lung recruitment is the crucial first step of neonatal transition and resuscitation. There is no current standard monitoring method of lung ventilation in the delivery room. Tidal volume monitoring is feasible, but challenging55,56 and can be inaccurate, especially in high mask leak situations. Non-invasive lung O2 monitoring using an optical device may provide ‘real-time’ information on lung ventilation, and subsequently optimise respiratory management during the dynamic situation soon after birth.
Endotracheal tube placement
Endotracheal (ET) intubation is a high skill requiring procedure performed by clinicians in the delivery room and the neonatal intensive care unit. The success rate of correct ET tube placement on the first attempt is 24% by paediatric trainees, 52% by fellows, 64% by neonatologists.57 Chest radiography as well as clinical signs and exhaled carbon dioxide detector are commonly used to confirm the correct ET tube position. On the other hand, each monitoring modality has some limitations, for example, the end-tidal colorimeter may not change in colour if there is no cardiac output, but the ET tube is in the correct place; gastric secretions may cause the device to change colour, but the ET tube is in the oesophagus instead of trachea. While correct and prompt ET tube position confirmation is critical to avoid complications due to delayed effective ventilation, continuous non-invasive O2 monitoring could be beneficial. Optical monitoring of O2 content could reveal asymmetrical O2 distribution within a chest suggesting ET tube tip located too deep in one of the main bronchi or no O2 detected would prompt the clinician to consider a misplaced ET tube.
There are three techniques currently used to estimate the depth of ET tube insertion to ensure optimal midtracheal position. The first is based on the calculation of estimated distance from the lip to midtracheal location (in centimetres) using equation 6 + baby’s weight (kg). Second, guided by a vocal cord mark present on the tube. And third, palpation of the ET tube tip at the suprasternal notch. The proportion of correctly positioned ET tubes was found to be similar using either of these techniques (suprasternal palpation 47%, weight 38–44%, vocal cord guide 40%). In all, 82–87% incorrectly positioned ET tubes were too low.58,59 This demonstrates the need for a more efficient method to detect the position of ET tubes in neonatal care.
It has been demonstrated that by simulating atelectasis of one lung because of ET tube malposition, GASMAS technology has the potential to detect the difference of gas content (reduced on the side of atelectasis) with suddenly dropping O2 absorption value.21 Moreover, prompt technique could allow monitoring of ET position in cases when X-ray imaging is not available.
Surfactant therapy
Surfactant therapy plays an essential role predominantly in the management of premature babies with RDS that is affecting approximately 80% of babies born at 28 weeks’ gestation.60 RDS causes diffuse alveolar collapse and compromises O2 delivery to the body. Multiple researchers are seeking to find an ideal standard of the best timing, dose, and methods of delivering surfactant treatment to maximise effect and minimise risks. GASMAS technology could help to detect early O2 level changes inside the lungs to determine optimal timing of surfactant administration. Moreover, different methods of delivering surfactant could be investigated by continuous real-time monitoring. A previously reported study has demonstrated that GASMAS technology can detect gas volume change.13 Furthermore, it is known that equally diffused spread of surfactant inside proximal airways is essential for the therapy to be effective.61 While distribution depends on multiple factors (instillation technique, speed, volume of preparation, ET tube position, ventilation strategy, gravity),62 continuous measurements of lung O2 would be the first available and informative method to monitor the surfactant administration procedure and potentially optimise the treatment algorithms.
Patient positioning improving lung ventilation
Multiple adult and animal models have shown gravity-dependent lung inhomogeneity with gas exchange and ventilation/perfusion matching improving when treated in the prone position. In the presence of an abdominal distension, which is a common issue for neonates, the prone position has a positive effect on gas exchange as well.63 Infants that require assisted ventilation are regularly repositioned to improve lung gas exchange. Studies comparing different neonatal positions have shown that arterial O2 saturation increases if the ventilated baby is being nursed in a prone or prone alternant position (P < 0.001).64,65 While baby’s body position has an impact on cardiopulmonary function,65 it is still unclear when the position should be changed, how often and which positions should be chosen. More knowledge about the changes in lung inflation obtained from continuous optical monitoring is required to give us the answers to the above questions.
Bronchopulmonary dysplasia diagnostics
Bronchopulmonary dysplasia (BPD) is a long-term adverse outcome of preterm delivery and often requires prolonged ventilation support and O2 therapy. Histopathological findings of BPD include alveolar simplification, dysmorphic capillaries, increased in vascular and airway smooth muscle cells, abnormal deposition of the extracellular components (e.g., elastin and collagen) and interstitial fluid accumulation.66 All these changes cause alveolar collapse (atelectasis) and compensatory overexpansion, subsequently impairing gas exchange and causing dependency on respiratory support and O2 therapy. BPD diagnosis has been evolving over time, initially based on histopathological findings, later relying on the duration of O2 supplementation, the amount of O2 required and most recently adding criteria of positive pressure ventilation support at ≥28 days post-natal age or at ≥36 weeks post-menstrual age.67 GASMAS with multisite measurements could be used to measure lung volume and O2 content to optimise diagnostic and management strategies for babies with BPD. To our knowledge, to date, no studies have reported the application of multiple light sources and detector probes and measuring signals simultaneously.
Conclusions
GASMAS-based devices have potential clinical use in neonatology, especially in the assessment and management of various respiratory conditions. Currently, only a few studies have assessed its feasibility in the neonatal population. More findings are available from studies performed with phantoms and will add important information on GASMAS applicability and required improvements in the future. Compared with other devices currently used in clinical practice for lung function monitoring, GASMAS has the advantages of bedside availability, continuous monitoring option, and unique information about molecular oxygen content inside the lung. Future research should aim to validate GASMAS measurements to prove reliability and precision.
References
Persson, L., Gao, H., Sjöholm, M. & Svanberg, S. Diode laser absorption spectroscopy for studies of gas exchange in fruits. Opt. Lasers Eng. 44, 687–698 (2006).
Tylewicz, U. et al. Gas in scattering media absorption spectroscopy (GASMAS) detected persistent vacuum in apple tissue after vacuum impregnation. Food Biophys. 7 (2012).
Olarewaju, O. O., Bertling, I. & Magwaza, L. S. Non-destructive evaluation of avocado fruit maturity using near infrared spectroscopy and PLS regression models. Sci. Horticulturae 199, 229–236 (2016).
Li, W., Lin, H., Zhang, H., Svanberg, K. & Svanberg, S. Detection of free oxygen and water vapor in fertilized and unfertilized eggs by diode laser spectroscopy-exploration of diagnostics possibilities. J. Biophotonics 11 (2018).
Svensson, T. et al. Noninvasive characterization of pharmaceutical solids by diode laser oxygen spectroscopy. Appl Spectrosc. 61, 784–786 (2007).
Khoptyar, D. et al. Broadband photon time-of-flight spectroscopy of pharmaceuticals and highly scattering plastics in the VIS and close NIR spectral ranges. Opt. Express 21, 20941–20953 (2013).
Johansson, J. et al. Optical porosimetry by gas in scattering media absorption spectroscopy (GASMAS) applied to roller compaction ribbons. Int. J. Pharm. 592, 120056 (2020).
Persson, L., Svanberg, K. & Svanberg, S. On the potential of human sinus cavity diagnostics using diode laser gas spectroscopy. Appl. Phys. B 82, 313–317 (2006).
Persson, L., Andersson, M., Cassel-Engquist, M., Svanberg, K. & Svanberg, S. Gas monitoring in human sinuses using tunable diode laser spectroscopy. J. Biomed. Opt. 12, 054001 (2007).
Persson, L. et al. Non-intrusive optical study of gas and its exchange in human maxillary sinuses. Proc. Spie. 6628 (2007).
Persson, L., Lewander, M., Andersson, M., Svanberg, K. & Svanberg, S. Simultaneous detection of molecular oxygen and water vapor in the tissue optical window using tunable diode laser spectroscopy. Appl. Opt. 47, 2028 (2008).
Lindberg, S. et al. Method for studying gas composition in the human mastoid cavity by use of laser spectroscopy. Ann. Otol. Rhinol. Laryngol. 121, 217–223 (2012).
Huang, J. et al. Assessment of human sinus cavity air volume using tunable diode laser spectroscopy, with application to sinusitis diagnostics. J. Biophotonics 8, 985–992 (2015).
Hu, L. et al. Towards an optical diagnostic system for otitis media using a combination of otoscopy and spectroscopy. J. Biophotonics 12, e201800305 (2019).
Zhang, H., Huang, J., Li, T., Svanberg, S. & Svanberg, K. Optical detection of middle ear infection using spectroscopic techniques: phantom experiments. J. Biomed. Opt. 20, 057001 (2015).
Chen, D. et al. Laser-based gas absorption spectroscopy in decaying hip bone: water vapor as a predictor of osteonecrosis. J. Biomed. Opt. 24, 1 (2019).
Lewander, M., Bruzelius, A., Svanberg, S., Svanberg, K. & Fellman, V. Nonintrusive gas monitoring in neonatal lungs using diode laser spectroscopy: feasibility study. J. Biomed. Opt. 16, 127002 (2011).
Larsson, J. et al. Development of a 3-dimensional tissue lung phantom of a preterm infant for optical measurements of oxygen-laser-detector position considerations. J. Biophotonics 11 (2018).
Pacheco Tobo, A. L., Li, H., Chakravarty, M., Konugolu Venkata Sekar, S. & Andersson-Engels, S. Anthropomorphic optical phantom of the neonatal thorax: a key tool for pulmonary studies in preterm infants. J. Biomed. Opt. 25, 115001 (2020).
Larsson, J. et al. Comparison of dermal vs internal light administration in human lungs using the TDLAS‐GASMAS technique—Phantom Studies. J. Biophotonics 12, e201800350 (2019).
Svanberg, E. K. et al. Changes in pulmonary oxygen content are detectable with laser absorption spectroscopy: proof of concept in newborn piglets. Pediatr. Res. 89, 823–829 (2021).
Lundin, P. et al. Noninvasive monitoring of gas in the lungs and intestines of newborn infants using diode lasers: feasibility study. J. Biomed. Opt. 18, 127005 (2013).
Svanberg, E. K. et al. Diode laser spectroscopy for noninvasive monitoring of oxygen in the lungs of newborn infants. Pediatr. Res. 79, 621–628 (2015).
Hibbard, J. U. et al. Respiratory morbidity in late preterm births. JAMA 304, 419–425 (2010).
Dyer, J. Neonatal respiratory distress syndrome: tackling a worldwide problem. PT 44, 12–14 (2019).
Ainsworth, S. B. Pathophysiology of neonatal respiratory distress syndrome: implications for early treatment strategies. Treat. Respir. Med 4, 423–437 (2005).
Guglani, L., Lakshminrusimha, S. & Ryan, R. M. Transient tachypnea of the newborn. Pediatr. Rev. 29, e59–e65 (2008).
Olgar, T. et al. Radiation exposure to premature infants in a neonatal intensive care unit in Turkey. Korean J. Radio. 9, 416–419 (2008).
Jakacka, N., Snarski, E. & Mekuria, S. Prevention of iatrogenic anemia in critical and neonatal care. Adv. Clin. Exp. Med 25, 191–197 (2016).
Sjöholm, M., Somesfalean, G., Alnis, J., Andersson-Engels, S. & Svanberg, S. Analysis of gas dispersed in scattering media. Opt. Lett. 26, 16–18 (2001).
Buck, A. L. New equations for computing vapor pressure and enhancement factor. J. Appl. Meteorol. 20, 1527–1532 (1981).
Pacheco, A., Grygoryev, K., Messina, W. & Andersson-Engels, S. Lung tissue phantom mimicking pulmonary optical properties, relative humidity, and temperature: a tool to analyze the changes in oxygen gas absorption for different inflated volumes. J. Biomed. Opt. 27, 074707 (2021).
Persson, L., Kristensson, E., Simonsson, L. & Svanberg, S. Monte Carlo simulations related to gas-based optical diagnosis of human sinusitis. J. Biomed. Opt. 12, 054002 (2007).
Liao, P. et al. Computer simulation analysis of source-detector position for percutaneously measured O2 gas signal in a three-dimensional preterm infant lung. J. Biophotonics 11, e201800023 (2018).
Liszewski, M. C. & Lee, E. Y. Neonatal lung disorders: pattern recognition approach to diagnosis. AJR Am. J. Roentgenol. 210, 964–975 (2018).
Perri, A. et al. Lung ultrasonography score versus chest X-ray score to predict surfactant administration in newborns with respiratory distress syndrome. Pediatr. Pulmonol. 53, 1231–1236 (2018).
Kartikeswar, G. A. P., Parikh, T. B., Pandya, D. & Pandit, A. Ionizing radiation exposure in NICU. Indian J. Pediatr. 87, 158–160 (2020).
Choi, G. et al. Development of quality-controlled low-dose protocols for radiography in the neonatal ICU using a new mobile digital radiography system. AJR Am. J. Roentgenol. 215, 488–493 (2020).
Hong, J. Y., Han, K., Jung, J. H. & Kim, J. S. Association of exposure to diagnostic low-dose ionizing radiation with risk of cancer among youths in South Korea. JAMA Netw. Open 2, e1910584 (2019).
Corsini, I., Parri, N., Ficial, B. & Dani, C. Lung ultrasound in the neonatal intensive care unit: review of the literature and future perspectives. Pediatr. Pulmonol. 55, 1550–1562 (2020).
Meulepas, J. M. et al. Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J. Natl Cancer Inst. 111, 256–263 (2019).
Semple, T., Akhtar, M. R. & Owens, C. M. Imaging bronchopulmonary dysplasia—a multimodality update. Front Med (Lausanne) 4, 88 (2017).
Lundin, P., Mei, L., Andersson-Engels, S. & Svanberg, S. Laser spectroscopic gas concentration measurements in situations with unknown optical path length enabled by absorption line shape analysis. Appl. Phys. Lett. 103, 034105 (2013).
Millikan, G. A. The oximeter, an instrument for measuring continuously the oxygen saturation of arterial blood in man. Rev. Sci. Instrum. 13, 434–444 (1942).
Chan, E. D., Chan, M. M. & Chan, M. M. Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respir. Med. 107, 789–799 (2013).
Bruns, N. et al. How to administer near-infrared spectroscopy in critically Ill neonates, infants, and children. J. Vis. Exp. (2020).
Watzman, H. M. et al. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology 93, 947–953 (2000).
Davies, D. J. et al. Frequency-domain vs continuous-wave near-infrared spectroscopy devices: a comparison of clinically viable monitors in controlled hypoxia. J. Clin. Monit. Comput 31, 967–974 (2017).
van Essen, T. et al. Comparison of frequency-domain and continuous-wave near-infrared spectroscopy devices during the immediate transition. BMC Pediatr. 20, 94 (2020).
Torricelli, A. et al. Time domain functional NIRS imaging for human brain mapping. NeuroImage 85, 28–50 (2014).
Oei, J. L. et al. Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 103, F446–F454 (2018).
White, L. N. et al. Achievement of saturation targets in preterm infants <32 weeks’ gestational age in the delivery room. Arch. Dis. Child Fetal Neonatal Ed. 102, F423–f427 (2017).
Brouwer, E. et al. Physiological-based cord clamping in preterm infants using a new purpose-built resuscitation table: a feasibility study. Arch. Dis. Child Fetal Neonatal Ed. 104, F396–f402 (2019).
Rabi, Y., Yee, W., Chen, S. Y. & Singhal, N. Oxygen saturation trends immediately after birth. J. Pediatr. 148, 590–594 (2006).
te Pas, A. B. et al. Spontaneous breathing patterns of very preterm infants treated with continuous positive airway pressure at birth. Pediatr. Res. 64, 281–285 (2008).
Schmolzer, G. M. et al. Assessment of tidal volume and gas leak during mask ventilation of preterm infants in the delivery room. Arch. Dis. Child Fetal Neonatal Ed. 95, F393–F397 (2010).
Foglia, E. E. et al. Neonatal intubation practice and outcomes: an international registry study. Pediatrics 143, e20180902 (2019).
Gill, I. et al. Randomised trial of estimating oral endotracheal tube insertion depth in newborns using weight or vocal cord guide. Arch. Dis. Child Fetal Neonatal Ed. 103, F312–f316 (2018).
Murphy, M. C., Donoghue, V. B. & O’Donnell, C. P. F. Randomised trial of estimating oral endotracheal tube insertion depth in newborns using suprasternal palpation of the tip or weight. Arch. Dis. Child Fetal Neonatal Ed. 105, 196–200 (2020).
Sweet, D. G. et al. European consensus guidelines on the management of respiratory distress syndrome - 2019 update. Neonatology 115, 432–450 (2019).
Tarawneh, A., Kaczmarek, J., Bottino, M. N. & Sant’anna, G. M. Severe airway obstruction during surfactant administration using a standardized protocol: a prospective, observational study. J. Perinatol. 32, 270–275 (2012).
Nouraeyan, N., Lambrinakos-Raymond, A., Leone, M. & Sant’Anna, G. Surfactant administration in neonates: a review of delivery methods. Can. J. Respir. Ther. 50, 91–95 (2014).
Mure, M. & Lindahl, S. G. Prone position improves gas exchange-but how? Acta Anaesthesiol. Scand. 45, 150–159 (2001).
Rivas-Fernandez, M., Roque, I. F. M., Diez-Izquierdo, A., Escribano, J. & Balaguer, A. Infant position in neonates receiving mechanical ventilation. Cochrane Database Syst. Rev. 11, CD003668 (2016).
Barsan Kaya, T., Aydemir, O. & Tekin, A. N. Prone versus supine position for regional cerebral tissue oxygenation in preterm neonates receiving noninvasive ventilation. J. Matern. Fetal Neonatal Med. 34, 3127–3132 (2021).
Hilgendorff, A., Reiss, I., Ehrhardt, H., Eickelberg, O. & Alvira, C. M. Chronic lung disease in the preterm infant. Lessons learned from animal models. Am. J. Respir. Cell Mol. Biol. 50, 233–245 (2014).
Ochiai, M. et al. A new scoring system for computed tomography of the chest for assessing the clinical status of bronchopulmonary dysplasia. J. Pediatr. 152, 90–95 (2008).
Acknowledgements
We would like to thank for the funding support from Science Foundation Ireland (SFI) (Project No. SFI/15/RP/2828).
Funding
J.P., A.P., K.G., S.A.-E. have been supported by Science Foundation Ireland (SFI) grant No. SFI/15/RP/2828 during the preparation of this manuscript. C.E.S. was supported by Deutsche Forschungsgemeinschaft (DFG, German Research Foundation, Project number 420536451) during the work on this manuscript. Open Access funding provided by the IReL Consortium.
Author information
Authors and Affiliations
Contributions
All authors contributed to the design of review manuscript, made critical revisions to ensure the accuracy and integrity of information. All authors have approved the final version of the review manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Panaviene, J., Pacheco, A., Schwarz, C.E. et al. Gas in scattering media absorption spectroscopy as a potential tool in neonatal respiratory care. Pediatr Res 92, 1240–1246 (2022). https://doi.org/10.1038/s41390-022-02110-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02110-y
This article is cited by
-
Evolution of gas in scattering media absorption spectroscopy as a neonatal pulmonary monitoring device
Pediatric Research (2022)