Abstract
Background
Inadequate pregnancy cobalamin status has been associated with adverse offspring metabolic health in Indian and Nepalese studies. Studies of pregnancy cobalamin status and mid-childhood health outside of Asia are scarce.
Methods
Associations between pregnancy fasting plasma total homocysteine (tHcy), cobalamin status (plasma cobalamin, holotranscobalamin (holoTC), methylmalonic acid (MMA)) and mid-childhood metabolic score (MetSco) ((including fat mass index (zFMI), homeostatic model assessment of insulin resistance (zHOMA-IR) and dyslipidemia (zTG − zHDLc)/2) z-scores)) were investigated in a prospective study of 293 mother–child dyads.
Results
Highest versus low–mid pregnancy tHcy tertile was associated with higher mid-childhood MetSco, specifically with higher child zFMI. Stratifying by sex, the maternal tHcy–child MetSco association was limited to boys and confirmed for zFMI and zHOMA-IR. The maternal tHcy-child zFMI association was not mediated by birth weight z-score. First trimester plasma cobalamin was not associated with child outcomes, but other indicators of cobalamin status were. Lowest versus mid–high plasma holoTC tertile was associated with MetSco (specifically zFMI and zHOMA-IR) and highest versus low–mid plasma MMA tertile with higher MetSco and dyslipidemia in boys.
Conclusions
Moderately elevated pregnancy tHcy and low cobalamin status were associated with mid-childhood metabolic score in boys. The pregnancy tHcy–child zFMI association was not mediated by birth weight.
Impact
-
Fasting plasma total homocysteine (tHcy) during pregnancy and low cobalamin status during early pregnancy are associated with mid-childhood metabolic score and its components in the offspring. These findings were only significant in male offspring.
-
The study provides new evidence that impaired one carbon metabolism during pregnancy is associated with negative health outcomes in the offspring, in a population with low prevalence of cobalamin deficiency.
-
The maternal–offspring associations were observed in the functional markers of cobalamin status (holotranscobalamin and methylmalonic acid) and tHcy, not with plasma cobalamin concentration.
-
Screening for low pregnancy cobalamin status should be considered.
Similar content being viewed by others
Introduction
Low birth weight has been linked to cardiovascular disease,1,2 type 2 diabetes,3,4 hypertension,3,4,5 and elevated triglycerides.3 Elevated pregnancy fasting plasma total homocysteine (tHcy) has been associated with low birth weight and intrauterine growth retardation risk.6,7 In regions where cobalamin deficiency is prevalent, low pregnancy cobalamin status has been associated with impaired glucose metabolism in the mother and the offspring during childhood.8 Similar results were reported in Bangladeshi pregnant women, living in the UK.9 Combined with cobalamin deficiency, high folate status during pregnancy has been associated with gestational diabetes10 and exacerbation of high adiposity and insulin resistance in the offspring.8 Pregnancy tHcy has also been associated with impaired glucose metabolism and insulin resistance in the offspring.11 Cobalamin deficiency is less prevalent in European women,12,13,14 but we reported interactions between folic acid supplement regime and low first trimester plasma cobalamin status (≤221 pmol/L) leading to worse cobalamin status as pregnancy progressed in women exceeding 400 µg/day of folic acid compared to those who adhered to the recommended dose.12 Few studies outside Asia have investigated how pregnancy one-carbon metabolism (1-CM) status affects childhood metabolic and growth outcomes. In a multi-ethnic Dutch cohort where 11.9 and 13.8% of the mothers were folate and cobalamin deficient, respectively, maternal folate was inversely associated with body mass index (BMI) and cobalamin with heart rate in the children.15 Low postpartum maternal folate status was associated with increased risk of childhood overweight/obesity in the offspring in a USA study.16 In animal studies, folate- and cobalamin-deficient diets during pregnancy or lactation lead to impaired glucose and lipid metabolism in the offspring.17,18
We hypothesized that moderately elevated pregnancy tHcy and cobalamin is associated with alterations in metabolic parameters in the offspring. We aimed to investigate the association between pregnancy tHcy, cobalamin status, and metabolic score in children aged 6–8 years.
Methods
Participants
Mother–child dyads (n = 293) from the PreC (Preconception) and RTBC (Reus-Tarragona Birth Cohort [registered at www.clinicaltrials.gov, NCT01778205]) studies participated from preconception/early pregnancy over 7–9 years (Fig. 1). The studies were approved by the Sant Joan Reus (SJR) and Joan XXIII Tarragona (JXXIII) University Hospitals’ joint Ethics Committees (internal reference 22/2016, approved on 20/10/2016 and revised on 30/10/2019), and conducted according to the Declaration of Helsinki guidelines with informed consent from participants. Parents provided consent, and the children, verbal assent, for the child phase.
Recruitment, described previously (PreC7,19,20 and RTBC12,21), was by the Unit of Preventive Medicine and Public Health, Faculty of Medicine and Health Sciences, Universitat Rovira i Virgili and the Units of Obstetrics and Gynecology, SJR and JXXIII Hospitals. Non-pregnant women volunteered for the PreC study in response to local city hall and media advertisements. None of them took folic acid supplements periconceptionally because the study was before the introduction of current recommendations.22 Some took folic acid-containing supplements coinciding with iron supplementation in mid–late pregnancy and 35 women never took folic acid supplements throughout pregnancy.
For the RTBC, participants were recruited from the high-risk obstetrics units and University/Hospital staff and contacts. They were advised at their first prenatal check-up to take supplements containing 400 µg folic acid/day and 2 µg cyanocobalamin/day for the first trimester and 40 mg iron/day after 12 gestational weeks (GW). Women with anemia were treated with iron supplements by their clinicians, and the iron doses were recorded.
Health check-up at 6–8 years
Child participation was at 6 (PreC) or 7.5 years of age (RTBC). Clinical data including anthropometric measurements were collected at the study check-up as well as from health records and lifestyle habits by interview with the parents.
Height was measured by stadiometer (with a precision of 0.1 cm). Children stood still, with their heels together and feet facing outwards at a 60° angle, head in the Frankfort plane, and palms of their hands placed on their legs.
Weight was measured on a mechanical beam scale with height rod (Pesperson model) (PreC) and electronic scale with a precision of 0.100 g (Tanita BC-420MA, Tanita Corporation, Tokyo, Japan) (RTBC).
Means of triplicate triceps (halfway between the acromion and the olecranon process at the back of the arm) and subscapular (20 mm below the tip of the scapula, at an angle of 45° to the lateral side of the body) skinfold thicknesses were measured by a Harpenden skinfold calliper (Holtain Ltd, Crymych, Wales), with an accuracy of 0.2 mm. Fat mass percentage (x) was determined from the sum of triceps (mm) and subscapular (mm) skinfold thicknesses (y)23. Fat mass percentage was used to calculate fat mass index24:
For y ≤ 35 mm:
For y > 35 mm:
Blood sample collection, processing and storage
Fasting blood samples were collected from the mothers at <12 GW (both cohorts), 32 GW (PreC), 34 GW (RTBC), and children in EDTA-K2 evacuated tubes, kept at 4 °C, and plasma separated within 1–2 h. Plasma samples were stored at −20 °C (PreC) and −80 °C (RTBC) until all samples from the same pregnancy were analysed in the same batch.
Biochemical determinations
tHcy was determined by immunoassay (PreC) (IMx autoanalyzer, Abbott, Chicago, USA)19 and liquid-tandem mass spectrometry (RTBC).25 Plasma methylmalonic acid (MMA) was determined by gas chromatography mass spectrometry with methylchloroformate derivatization,25 folate and cobalamin by microbiological assays with Lactobacillus casei26 and Lactobacillus leichmannii,27 respectively, and holoTC by immunoassay (AxSym autoanalyzer, Abbott Chicago, USA) in SJR Hospital.28 Plasma MMA measurements were not available for the children from the PreC cohort and plasma holoTC was not available for the children from the RTBC cohort. Plasma insulin concentration was determined by Iso-Insulin ELISA Kit (a solid-phase two-site enzyme immunoassay, Mercodia, Sweden) and glucose by the glucose oxidase (GOD) peroxidase (POD) method (Spinreact, Sant Esteve de Bas, Spain). Insulin resistance was calculated as HOMA-IR [homeostasis model assessment of insulin resistance] = (FPI [fasting plasma insulin concentration, mU/L] × FPG [fasting plasma glucose, mmol/L])/22.5.29 Plasma total cholesterol and high-density lipoprotein cholesterol (HDLc) were determined by enzymatic colorimetric techniques (Spinreact, Sant Esteve de Bas, Spain), and triglycerides (TG) by glycerol phosphate oxidase (GPO) peroxidase (POD) technique (Spinreact, Sant Esteve de Bas, Spain). Low-density lipoprotein cholesterol was calculated using the Friedewald formula (Total cholesterol − HDLc − triglycerides mg/dL/5).30 Plasma lipoprotein(a) (Lp(a)) was determined by quantitative turbidimetric test Lp(a)-turbilatex (Spinreact, Sant Esteve de Bas, Spain) and Apolipoprotein A1 (ApoA1) and B (ApoB) by turbidimetry technique (ABX Pentra, France).
Metabolic score
A modification of the risk score used in the IDEFICS cohort31 was used:
The IDEFICS score includes waist circumference (WC) and blood pressure. These were unavailable for PreC, so FMI was used and blood pressure was omitted. Dyslipidemia was measured as (zTG − zHDLc)/2, where HDLc is inversely associated with the metabolic risk profile. We derived z-scores (standardized residuals) from a generalized linear model (GLM) of each component (FMI, Lipids, HOMA-IR) as dependent variables, including age and sex as the predictors.
Sample size calculation
A priori, by way of orientation, sample size calculation was based on the hypothetical association between elevated pregnancy tHcy and childhood obesity. A type 1 error of 5% and power of 80% in unilateral contrast tests were assumed, for an expected odds ratio of ≥4 for childhood obesity for pregnancy tHcy in the highest tertile, compared to the other tertiles combined. We expected 38% of the children to be overweight and the others to have normal weight. Based on a pilot study, 10% of the mothers of normal weight children were expected to have had highest tertile pregnancy tHcy (unpublished data).
Statistical analysis
Variable distribution normality was tested by the Kolmogorov–Smirnov test and ln-transformation to approach normality applied as required for parametric tests. Quantitative variables were compared between categories by the Student’s unpaired t test, medians by the Median test for K independent samples (SPSS), and proportions by the Chi-square test. Correlations between variables are reported as Spearman’s rank-order correlation coefficients. Associations between pregnancy tHcy, cobalamin, and folate status and mid-childhood outcomes (MetSco and its components) were investigated by multiple linear regression analysis. Associations were determined for the highest maternal tertiles of plasma tHcy and MMA compared to the low–mid tertiles (combined) and lowest maternal tertiles of plasma cobalamin, holoTC, and folate compared to the mid–high tertiles (combined).
Models were adjusted for maternal characteristics (preconception (PreC) and first trimester (RTBC) BMI, socioeconomic status, pregnancy smoking pattern (never (reference group), first trimester only, throughout pregnancy), and child characteristics (breastfeeding (yes/no), BMI z-score32 as a substitute for energy intake that is unavailable for the PreC cohort, and tHcy). Mediation analysis was used to test whether the pregnancy tHcy–offspring outcome associations were mediated by birth weight z-score (Spanish birth weight tables).33
Assumptions in linear regression (linearity, homogeneity of variance (homoscedasticity), normality of errors, independence of errors between the two cohorts, model specification, and multicollinearity) were checked.
Unusual and influential data were detected by inspecting scatterplots of the independent and dependent variables for potential outliers and residuals, to exclude those with a Cook’s distance >4/n (N = 4). SPSS version 27.0 for Windows, with the PROCESS macro34 for the mediation analysis, was used.
Results
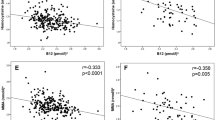
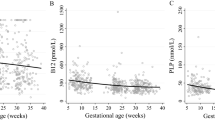
Participant characteristics according to pregnancy tHcy status are reported in Table 1. Maternal (including age, BMI, parity, smoking habits, and socioeconomic status) and child (including male sex prevalence, birth weight z-score, low birth weight (<P10), and breastfeeding regime) characteristics were similar between the pregnancy tHcy categories. Prevalence of overweight–obesity according to Spanish tables32 was higher in children born to mothers in the highest tHcy tertile in the first trimester of pregnancy compared to the low–mid tertiles but there was no difference among the third trimester tHcy tertiles. Detailed maternal and child characteristics of both cohorts are reported in Supplemental Table S1. RTBC mothers were slightly older, less of them smoked but more of the smokers continued smoking throughout pregnancy, and they had higher socioeconomic status. Generally, the biochemical indicators of first trimester 1-CM status were better in the RTBC, except for plasma MMA that did not differ between the two cohorts. The same was true for third trimester indicators, except for plasma folate that was lower in the RTBC. The prevalence of low birth weight was lower in the RTBC and less of the babies had been breastfed for at least 1 month. Child plasma tHcy and triglycerides were lower in the RTBC, and HDLc and glucose were higher. None of the other metabolic or biochemical parameters differed between the two cohorts. Pregnancy tHcy, plasma cobalamin, and holoTC were each weakly correlated with the same corresponding variables in the children (Supplemental Table S2). Maternal plasma holoTC was relatively strongly correlated with plasma cobalamin and tHcy, compared to plasma MMA. Plasma holoTC, cobalamin, and tHcy were all only weakly correlated with plasma MMA. The child holoTC–cobalamin correlation was relatively strong, and stronger than any of the other correlations among child nutrients or tHcy. Child folate, holoTC, and cobalamin were inversely correlated with tHcy in that decreasing order of strength of correlation. Pregnancy 1-CM status and child biochemical data by pregnancy tHcy status is reported in Table 2. Only folate status differed significantly between the corresponding tHcy categories in both trimesters. Folate status was lower and deficiency more prevalent in mothers in the highest versus low–mid tHcy tertiles. More mothers had cobalamin and folate deficiency in the third trimester compared to the first. None of the children had cobalamin deficiency (data not shown) but 4.6% had folate deficiency. Offspring tHcy and plasma glucose concentration were higher when pregnancy tHcy was in the highest versus low–mid tertiles and this was also true for HOMA-IR when mothers had high tertile tHcy in the third trimester. No differences were observed in any of the child lipid parameters ((total cholesterol, plasma lipoprotein (a), ApoA1 and ApoB, LDL cholesterol) by pregnancy tHcy status.
Determinants of first trimester maternal tHcy are reported in Supplemental Table S3. Plasma folate concentration was the strongest.
Associations between pregnancy tHcy status, child MetSco, and its components are reported in Table 3. Offspring of mothers with highest versus low–mid tHcy tertiles had higher MetSco and zFMI. Stratifying by sex, the associations were only significant in boys. Furthermore, in boys only, zHOMA-IR was higher when mothers had third trimester tHcy in the highest versus the low–mid tertiles.
Associations between pregnancy indicators of cobalamin status and childhood outcomes are reported in Table 4. First trimester plasma cobalamin was not associated with any child outcomes but boys born to mothers with low third trimester plasma cobalamin status had lower mid-childhood FMI. On the other hand, first trimester holoTC in the lowest versus mid–high tertiles was associated with higher MetSco, FMI, and insulin resistance in boys. Highest first trimester MMA tertile versus low–mid tertiles was associated with increased child metabolic score and dyslipidemia ((zTG − zHDLc)/2) in boys. Associations between pregnancy folate status and mid-childhood outcomes are reported in Supplemental Table S4. Children of mothers with first trimester plasma folate concentration in the lowest (<14.6 nmol/L) versus mid–high tertiles had higher insulin resistance, and stratifying by sex, this was limited to girls. Boys born to mothers with third trimester plasma folate in the lowest compared to mid–high tertiles had lower dyslipidemia.
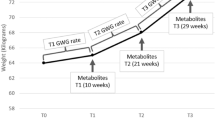
Mediation analysis was used to explore whether the associations between first trimester tHcy and zFMI are partially mediated via fetal growth (birth weight z-score) (Fig. 2). The direct effect (tHcy outcome, coefficient c’), indirect effect ((tHcy–birth weight z-score outcome, coefficient a (tHcy–birth weight), and coefficient b (birth weight z-score outcome)) and total effect (tHcy outcome, coefficient c, unadjusted for birth weight z-score) are illustrated. The indirect effect (a × b) represents the association between tHcy and child zFMI via the sequence tHcy–birth weight outcome. The Monte Carlo confidence interval for the indirect effect includes 0, indicating that birth weight does not play a role in the association between early pregnancy tHcy and fat mass index in the offspring.
a, b, c’, and c (linear regression analysis B coefficients adjusting for maternal age, BMI, socioeconomic status, smoking (a), and birth weight z-score, breastfeeding, and child zBMI, tHcy (b and c’) and excluding birth weight (c)). N = 196 mother–child dyads. a × b = indirect effect of tHcy on zFMI via birth weight z-score. *P < 0.05, **P < 0.01.
Discussion
Principal findings
Moderately elevated pregnancy tHcy was positively associated with MetSco in boys, and specifically zFMI and zHOMA-IR. First trimester low holoTC and high MMA were positively associated with MetSco, first trimester holoTC with zFMI and zHOMA-IR, and first trimester MMA with dyslipidemia in boys. The pregnancy tHcy-child zFMI association was not mediated by birth weight. Low third trimester plasma cobalamin was associated with lower FMI and low plasma folate with lower dyslipidemia in boys. In girls only, low first trimester plasma folate was positively associated with zHOMA-IR.
Comparison with previous studies
Overall, these findings in participants with a low prevalence of cobalamin deficiency support previous observations from studies in countries where cobalamin deficiency is highly prevalent. However, none of those were stratified by sex. Indian studies reported no association between pregnancy tHcy and percentage body fat or other anthropometric measurements in the offspring in mid-childhood.8,11 We observed no association between pregnancy folate and offspring FMI. However, a USA study observed that postpartum maternal folate protected against high BMI z-score and probability of overweight or obesity in the offspring. This was especially evident among obese mothers.16 The association between pregnancy tHcy and insulin resistance in boys agrees with the findings for child postload glucose concentrations, plasma insulin concentrations, and HOMA-IR reported in an Indian study.11 Maternal cobalamin status was not associated with insulin resistance in the offspring in our study, agreeing with one Indian study11 but not with another8 or a Nepalese study.35 However, we observed that low pregnancy holoTC (fraction of cobalamin bound to trans-cobalamin II for tissue uptake)36 status was associated with insulin resistance in boys. The observed association between low pregnancy folate status and higher HOMA-IR in the children (specifically girls) agrees with a USA study that reported higher insulin resistance in children born to obese mothers with low folate status.16 Our results disagree with those from the Indian studies reporting an association between high pregnancy folate status and insulin resistance in the offspring.8,11
Folic acid-deficient diets led to increased steatosis in mice (associated with insulin resistance).37 However, unlike our study where the low pregnancy folate–child insulin resistance association was limited to girls, in the mice the effects were more frequent and severe in males.
The lack of association between maternal tHcy and offspring dyslipidemia agrees with a previous Indian study.11 On the other hand, pregnancy MMA was positively associated with MetSco and dyslipidemia in boys. The low pregnancy folate status–lower dyslipidemia in childhood (specifically boys) association disagrees with a Dutch study reporting no association between pregnancy folate and child triglycerides.15 High folic acid diets provoked alterations in hepatocyte lipid metabolism consistent with increased lipogenesis in male mice.38
Birth weight was not a mediator of the association between maternal tHcy and child zFMI. A previous study refuted birth weight as a mediator in the association between pre-pregnancy obesity and anthropometric outcomes in children.39
Interpretation
Elevated tHcy has been associated with endothelial dysfunction, affecting placental vasculature, and offspring cardiometabolic health.40 Previously, we reported a greater strain by pregnancy on cobalamin reserves (reflected by higher MMA) in women starting pregnancy with low holoTC status.13 Here low pregnancy holoTC and high MMA are associated with higher MetSco in boys. High MMA is also associated with dyslipidemia in boys and low holoTC with increased FMI and HOMA-IR. The holoTC and MMA findings suggest that the pregnancy tHcy–child MetSco association may reflect impaired cobalamin status as reported in previous studies.8,35 When metabolic syndrome develops in adults, anomalies in glucose metabolism have been reported to occur before obesity and dyslipidemia.41 Low fetal cobalamin supply leading to reduced protein synthesis and increased lipogenesis has been hypothesized to link maternal cobalamin deficiency to increased insulin resistance in the offspring.8,9 Regarding fat metabolism, animal studies showed that severe hepatic steatosis occurred, secondary to cobalamin deficiency in which elevated MMA inhibits the oxidation of free fatty acids within the liver.42,43 This is unlikely in our study because cobalamin deficiency was infrequent. However, 1-CM and impaired glucose and adiposity have been linked.8,9,11 An alternate hypothesis to a role for 1-CM should be considered. However, maternal–child associations (MetSco and its components) were independent of birth weight and maternal BMI, which has been associated with offspring central fat and cardiometabolic risk.40,44,45
Low first trimester cobalamin status, according to its indicators, holoTC and MMA, was associated with adverse metabolic outcomes in the child. However, lowest tertile third trimester cobalamin status was associated with lower FMI in boys and lowest tertile folate status with lower dyslipidemia. Cord plasma cobalamin and folate are higher than circulating cobalamin and folate, respectively, in the mother at birth.12 Low status in plasma concentrations of these nutrients in late pregnancy may reflect placental uptake of the vitamins rather than impaired status.46 We hypothesize that early pregnancy status in cobalamin is a more accurate reflection of the mother’s underlying status in this nutrient than late pregnancy status. This may also be true for folate but would be affected by current trends in early pregnancy folic acid supplement use.
Mostly, the observed pregnancy–offspring outcomes were specific to boys. Male animal47 and human48 embryos proliferate to the blastocyst stage at a faster rate than females and sex differences in gene expression in preimplantation embryos occur.49 Male preimplantation embryos are more responsive to intrauterine undernutrition than females.50 Also, placenta genes are differentially expressed in male and female mice on different folic acid supplementation regimes.51 Adult hepatocyte phosphatidylethanolamine N-methyltransferase differs between sexes52 and sex differences in other 1-CM enzymes have been described in mice.53 In animal studies, dietary restrictions in 1-CM nutrients during pregnancy led to genome-wide epigenetic modifications in offspring DNA methylation. More than half of the affected loci were specific to males and stronger effects were observed for insulin resistance, adiposity, altered immune function, and high blood pressure in males than in females.54 Glucose tolerance in the female rat offspring was unaffected by restricted diets but insulin was higher in males born to pregnant rat dams fed similar diets.55
Further investigation is required to determine whether similar maternal–offspring associations occur in girls but may be masked by the physiological factors that drive differences in FMI between girls and boys from 3 years onwards.56
Strengths and limitations
This study collected data prospectively from early pregnancy until mid-childhood in mother–child dyads unexposed to mandatory fortification with folic acid and with a low prevalence of cobalamin deficiency.
The cohorts were recruited before (PreC) and after (RTBC) periconceptional supplementation with folic acid recommendations were implemented. Nevertheless, they were from the same hospitals, samples were collected and processed using identical protocols, and all folate and cobalamin status determinations were by the same methods. The cohorts were combined to improve statistical power. Sensitivity analysis confirmed that the reported associations occurred when the RTBC mother–child dyads were analyzed alone (not shown).
WC or waist-to-height ratio are recommended for total body fat assessment.56 However, FMI can also be used56 and skinfold measurements are better alternatives to WC and BMI57 and predict obesity well58 in children and adolescents. WC is unavailable for the PreC cohort, but we confirmed the association between pregnancy tHcy and offspring body fat using WC z-score in RTBC (data not shown).
We assessed overweight–obesity using Spanish tables32 because the participants were almost exclusively Spanish. By using the international obesity task force tables,59 the prevalence of overweight–obesity in our population was higher (23.7 versus 20.2%). We considered the use of the Spanish tables appropriate because we use population-specific curves to determine birth weight and BMI z-scores and the aim of the study was to investigate maternal–offspring outcomes and not to compare prevalence between different countries.
Residual confounding from factors not considered in our models may occur. However, our models were controlled for numerous maternal and child factors that influence offspring growth.60
Conclusions
Moderately elevated pregnancy tHcy and low holoTC status were positively associated with MetSco, zFMI, and zHOMA-IR in boys. High pregnancy MMA was also positively associated with MetSco and dyslipidemia in boys. The association between pregnancy tHcy and child zFMI was not mediated by birth weight.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available because participant consent covers data exploration in response to hypothesis testing within a defined field and with the compromise that this will be vetted by the Principal Investigator (M.M.M.). The corresponding author (M.M.M.) is willing to provide the data to interested parties on reasonable request and agreement that it will be exploited under the terms of participant consent and following further approval by the Ethics Committees if required.
References
Barker, D. J., Osmond, C., Golding, J., Kuh, D. & Wadsworth, M. E. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. Br. Med. J. 298, 564–567 (1989).
Barker, D. J., Winter, P. D., Osmond, C., Margetts, B. & Simmonds, S. J. Weight in infancy and death from ischaemic heart disease. Lancet 2, 577–580 (1989).
Barker, D. J. et al. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia 36, 62–67 (1993).
Curhan, G. C. et al. Birth weight and adult hypertension, diabetes mellitus, and obesity in US men. Circulation 94, 3246–3250 (1996).
Curhan, G. C. et al. Birth weight and adult hypertension and obesity in women. Circulation 94, 1310–1315 (1996).
Hogeveen, M., Blom, H. J. & den Heijer, M. Maternal homocysteine and small-for-gestational-age offspring: systematic review and meta-analysis. Am. J. Clin. Nutr. 95, 130–136 (2012).
Murphy, M. M., Scott, J. M., Arija, V., Molloy, A. M. & Fernandez-Ballart, J. D. Maternal homocysteine before conception and throughout pregnancy predicts fetal homocysteine and birth weight. Clin. Chem. 50, 1406–1412 (2004).
Yajnik, C. S. et al. Vitamin B12 and folate concentrations during pregnancy and insulin resistance in the offspring: the Pune Maternal Nutrition Study. Diabetologia 51, 29–38 (2008).
Sobczyńska-Malefora, A., Yajnik, C. S., Harrington, D. J., Hitman, G. A. & Finer, S. Vitamin B12 and folate markers are associated with insulin resistance during the third trimester of pregnancy in South Asian women, living in the United Kingdom, with gestational diabetes and normal glucose tolerance. J. Nutr. 152, 163–170 (2022).
Lai, J. S. et al. High folate and low vitamin B12 status during pregnancy is associated with gestational diabetes mellitus. Clin. Nutr. 37, 940–947 (2018).
Krishnaveni, G. V., Veena, S. R., Karat, S. C., Yajnik, C. S. & Fall, C. H. D. Association between maternal folate concentrations during pregnancy and insulin resistance in Indian children. Diabetologia 57, 110–121 (2014).
Solé-Navais, P. et al. Early pregnancy folate-cobalamin interactions and their effects on cobalamin status and hematologic variables throughout pregnancy. Am. J. Clin. Nutr. 107, 173–182 (2018).
Murphy, M. M. et al. Longitudinal study of the effect of pregnancy on maternal and fetal cobalamin status in healthy women and their offspring. J. Nutr. 137, 1863–1867 (2007).
Milman, N., Byg, K. E., Bergholt, T., Eriksen, L. & Hvas, A. M. Cobalamin status during normal pregnancy and postpartum: a longitudinal study comprising 406 Danish women. Eur. J. Haematol. 76, 521–525 (2006).
Krikke, G. G. et al. Vitamin B12 and folate status in early pregnancy and cardiometabolic risk factors in the offspring at age 5–6 years: findings from the ABCD multi-ethnic birth cohort. BJOG 23, 384–392 (2016).
Wang, G. et al. Association between maternal prepregnancy body mass index and plasma folate concentrations with child metabolic health. JAMA Pediatr. 170, e160845 (2016).
Bison, A. et al. Foetal programming by methyl donor deficiency produces steato-hepatitis in rats exposed to high fat diet. Sci. Rep. 6, 37207 (2016).
Kumar, K. A. et al. Chronic maternal vitamin B12 restriction induced changes in body composition & glucose metabolism in the Wistar rat offspring are partly correctable by rehabilitation. PLoS ONE 9, e112991 (2014).
Murphy, M. M., Scott, J. M., McPartlin, J. M. & Fernandez-Ballart, J. D. The pregnancy-related decrease in fasting plasma homocysteine is not explained by folic acid supplementation, hemodilution, or a decrease in albumin in a longitudinal study. Am. J. Clin. Nutr. 76, 614–619 (2002).
Murphy, M. M., Fernandez-Ballart, J. D., Molloy, A. M. & Canals, J. Moderately elevated maternal homocysteine at preconception is inversely associated with cognitive performance in children 4 months and 6 years after birth. Mat. Child Nutr. 13, e12289 (2017).
Fernàndez-Roig, S. et al. Low folate status enhances pregnancy changes in plasma betaine and dimethylglycine concentrations and the association between betaine and homocysteine. Am. J. Clin. Nutr. 97, 1252–1259 (2013).
Departament de Salut, Generalitat de Catalunya. Protocol de seguiment de l’embaràs a Catalunya [The prenatal care protocol in Catalonia] 3rd edn (Departament de Salut, Generalitat de Catalunya, 2018).
Slaughter, M. H. et al. Skinfold equations for estimation of body fatness in children and youth. Hum. Biol. 60, 709–723 (1988).
Nagy, P. et al. Erratum: Percentile reference values for anthropometric body composition indices in European children from the IDEFICS study. Int. J. Obes. 40, 1604–1605 (2016).
Ueland, P. M. et al. Quantitative profiling of folate and one-carbon metabolism in large-scale epidemiological studies by mass spectrometry. Clin. Chem. Lab. Med. 45, 1737–1745 (2007).
Molloy, A. M. & Scott, J. M. Microbiological assay for serum, plasma, and red cell folate using cryopreserved, microtiter plate method. Methods Enzymol. 281, 43–53 (1997).
Kelleher, B. P. & Broin, S. D. Microbiological assay for vitamin B12 performed in 96-well microtitre plates. J. Clin. Pathol. 44, 592–595 (1991).
Orning, L. et al. Characterization of a monoclonal antibody with specificity for holo-transcobalamin. Nutr. Metab. 3, 3 (2006).
Wallace, T. M., Levy, J. C. & Matthews, D. R. Use and abuse of HOMA modeling. Diabetes Care 27, 1487–1495 (2004).
Friedewald, W. T., Levy, R. I. & Fredrickson, D. S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 18, 499–502 (1972).
Ahrens, W. et al. Metabolic syndrome in young children: definitions and results of the IDEFICS study. Int. J. Obes. 38, S4–14 (2014).
Carrascosa, A. et al. Estudio transversal español de crecimiento 2008. Parte II: valores de talla, peso e índice de masa corporal desde el nacimiento a la talla adulta. Ann. Pediatr. 68, 552–569 (2008).
Santamaría, R., Verdú, L.I., Caballero, M. & García, G. Tablas españolas de pesos neonatales según edad gestacional. Grupo de Trabajo de Segovia de la Sociedad Española de Ginecología y Obstetricia. https://www.menarini.es/aviso-legal/509-salud/areas-terapeuticas/ginecologia/3073-tablas-espanolas-de-pesos-neonatales.html (1998).
Hayes, A. F. Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach (Guilford Publications, 2017).
Stewart, C. P. et al. Low maternal vitamin b-12 status is associated with offspring insulin resistance regardless of antenatal micronutrient supplementation in rural Nepal. J. Nutr. 141, 1912–1917 (2011).
Nexo, E. & Hoffmann-Lücke, E. Holotranscobalamin, a marker of vitamin B-12 status: analytical aspects and clinical utility. Am. J. Clin. Nutr. 94, 359S–365S (2011).
Christensen, K. E. et al. Steatosis in mice is associated with gender, folate intake, and expression of genes of one-carbon metabolism. J. Nutr. 140, 1736–1741 (2010).
Christensen, K. E. et al. High folic acid consumption leads to pseudo-MTHFR deficiency, altered lipid metabolism, and liver injury in mice. Am. J. Clin. Nutr. 101, 646–658 (2015).
Adane, A. A., Tooth, L. R. & Mishra, G. D. The role of offspring’s birthweight on the association between pre-pregnancy obesity and offspring’s childhood anthropometrics: a mediation analysis. J. Dev. Orig. Health Dis. 10, 570–577 (2019).
Wang, H., Xu, B. P., Xu, R. B., Walker, S. O. & Wang, G. Joint effect of maternal plasma homocysteine and prepregnancy obesity on child blood pressure: a prospective birth cohort study. Int. J. Obes. 41, 1447–1453 (2017).
Barceló, M. A., Rodríguez-Poncelas, A., Saez, M. & Coll-de-Tuero, G. The dynamic behaviour of metabolic syndrome and its components in an eight-year population-based cohort from the Mediterranean. PLoS ONE 12, e0176665 (2017).
Clare, C. E., Brassington, A. H., Kwong, W. Y. & Sinclair, K. D. One-carbon metabolism: linking nutritional biochemistry to epigenetic programming of long-term development. Annu. Rev. Anim. Biosci. 7, 263–287 (2019).
Kennedy, D. G. et al. Cobalt-vitamin B12 deficiency causes accumulation of odd-numbered, branched-chain fatty acids in the tissues of sheep. Br. J. Nutr. 71, 67–76 (1994).
Gaillard, R. et al. Childhood cardiometabolic outcomes of maternal obesity during pregnancy: the Generation R Study. Hypertension 63, 683–691 (2014).
Perng, W., Gillman, M. W., Mantzoros, C. S. & Oken, E. A prospective study of maternal prenatal weight and offspring cardiometabolic health in midchildhood. Ann. Epidemiol. 24, 793–800 (2014). e1.
Graber, S. E., Scheffel, U., Hodkinson, B. & McIntyre, P. A. Placental transport of vitamin B12 in the pregnant rat. J. Clin. Investig. 50, 1000–1004 (1971).
Tiffin, G. J., Rieger, D., Betteridge, K. J., Yadav, B. R. & King, W. A. Glucose and glutamine metabolism in pre-attachment cattle embryos in relation to sex and stage of development. J. Reprod. Fertil. 93, 125–132 (1991).
Ray, P. F., Conaghan, J., Winston, R. M. & Handyside, A. H. Increased number of cells and metabolic activity in male human preimplantation embryos following in vitro fertilization. J. Reprod. Fertil. 104, 165–171 (1995).
Erickson, R. P. Does sex determination start at conception? Bioessays 19, 1027–1032 (1997).
Kwong, W. Y., Wild, A. E., Roberts, P., Willis, A. C. & Fleming, T. P. Maternal undernutrition during the preimplantation period of rat development causes blastocyst abnormalities and programming of postnatal hypertension. Development 127, 4195–4202 (2000).
Luan, Y. et al. Moderate folic acid supplementation in pregnant mice results in altered methyl metabolism and in sex-specific placental transcription changes. Mol. Nutr. Food Res. 65, e2100197 (2021).
Resseguie, M. et al. Phosphatidylethanolamine N-methyltransferase (PEMT) gene expression is induced by estrogen in human and mouse primary hepatocytes. FASEB J. 21, 2622–2632 (2007).
Sadre-Marandi, F., Dahdoul, T., Reed, M. C. & Nijhout, H. F. Sex differences in hepatic one-carbon metabolism. BMC Syst. Biol. 12, 89 (2018).
Sinclair, K. D. et al. DNA methylation, insulin resistance, and blood pressure in offspring determined by maternal periconceptional B vitamin and methionine status. Proc. Natl Acad. Sci. USA 104, 19351–19356 (2007).
Maloney, C. A., Hay, S. M., Young, L. E., Sinclair, K. D. & Rees, W. D. A methyl-deficient diet fed to rat dams during the peri-conception period programs glucose homeostasis in adult male but not female offspring. J. Nutr. 141, 95–100 (2011).
Nagy, P. et al. Percentile reference values for anthropometric body composition indices in European children from the IDEFICS study. Int. J. Obes. 38, S15–25 (2014).
Kriemler, S. et al. Estimation of percentage body fat in 6- to 13-year-old children by skinfold thickness, body mass index and waist circumference. Br. J. Nutr. 104, 1565–1572 (2010).
Sardinha, L. B., Going, S. B., Teixeira, P. J. & Lohman, T. G. Receiver operating characteristic analysis of body mass index, triceps skinfold thickness, and arm girth for obesity screening in children and adolescents. Am. J. Clin. Nutr. 70, 1090–1095 (1999).
Cole, T. J. & Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 7, 284–294 (2012).
González-Jiménez, E., Montero-Alonso, M. A., Schmidt-RioValle, J., García-García, C. J. & Padez, C. Metabolic syndrome in Spanish adolescents and its association with birth weight, breastfeeding duration, maternal smoking, and maternal obesity: a cross-sectional study. Eur. J. Nutr. 54, 589–597 (2015).
Acknowledgements
We thank the families who participated in the study and the University, Clinical, Laboratory, and Biobank teams involved in the field work of the study.
Funding
This work was supported by grants from The Interministerial Science and Technology Committee (ALI 89-0388 and SAF2005-05096); The Carlos III Health Institute, National Scientific Research, Development and Technological Innovation Program Health Investigation Resources, cofinanced by The European Regional Development Fund (10/00335, 13/02500, 16/00506, 19/00844); The European Union Horizon 2020 Research and Innovation program (EPIBRAIN project, funded by the Joint Programming Initiative “A Healthy Diet for a Healthy Life” (ERA HDHL); JFA2 Nutrition and the Epigenome, Horizon2020 grant agreement number 696300, with funding provided by The Spanish State Agency for Investigation PCI2018-093098/AEI); Pere Virgili Health Research Institute (IISPV-2010/21); Biomedical Research Networking Center for the Pathophysiology of Obesity (CIBERobn); Agency for Management of University and Research grants, Generalitat de Catalunya (Support to Research Groups: 2009-1237, 2014-332); Italfarmaco S.A., Spain; predoctoral research fellowship from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie and from the Universitat Rovira i Virgili (URV) (713679 [to A.R.-G.]) and the URV Martí-Franques program [to P.S.-N., G.O.-M., C.R.-R.]. The funders played no role of any sort in the design and execution of the study or the reporting and interpretation of the results.
Author information
Authors and Affiliations
Contributions
A.R.-G. and M.M.M. conceptualized and designed the study, the data collection instruments, collected data, analyzed data, drafted the initial manuscript, and reviewed and revised the manuscript. J.F.-B., P.C.-B., P.S.-N., G.O.-M., M.B., C.G., and C.R.-R. participated in the conceptualization and design of the study, designed the data collection instruments, collected data, and reviewed and revised the manuscript. P.M.U. and L.M. participated in the conceptualization and design of the study and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Signed informed consent to participate in the study was obtained from all participants, from either parent on behalf of the children and verbal assent from the children.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rojas-Gómez, A., Solé-Navais, P., Cavallé-Busquets, P. et al. Pregnancy homocysteine and cobalamin status predict childhood metabolic health in the offspring. Pediatr Res 93, 633–642 (2023). https://doi.org/10.1038/s41390-022-02117-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02117-5