Abstract
Background
Psychiatric implications of prostate cancer are increasingly recognised, having important effects on oncological and functional outcomes. However, findings for co-occurring depression, anxiety, and suicidality remain variable. Therefore, this review of observational studies aimed to establish best estimates of the prevalence and rates of these outcomes in prostate cancer patients.
Methods
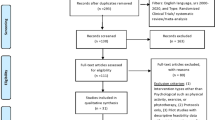
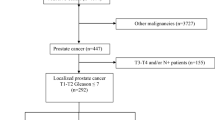
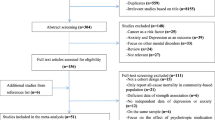
A systematic literature search was conducted using MEDLINE, Scopus, PsycInfo, and Cochrane Library databases from inception up to 26 May 2020. Observational studies using validated methods for evaluating prevalences of depression, anxiety and suicidal ideation, or suicide mortality rates post prostate cancer diagnosis were included. Random effect models were used to calculate pooled prevalences of depressive and anxiety symptoms or disorders, and suicidal ideation post diagnosis. Additionally, pooled crude suicide mortality rates per 100,000 person years were calculated. Heterogeneity was explored using a stratified analysis.
Results
Of 3537 articles screened, 117 were included. Pooled prevalence for depressive disorders was 5.81% (95% CI 4.36–7.46) in 11 studies, representing 655,149 patients. Significant depressive symptoms were identified in 17.07% (15.14–19.09) across 32,339 patients and 76 studies. In total, 16.86% (14.92–18.89) had significant anxiety symptoms in 56 studies combining 24,526 patients. In 6,173 patients and eight studies, recent suicidal ideation was present in 9.85% (7.31–12.70). Crude suicide mortality rate after diagnosis was 47.1 (39.85–54.96) per 100,000 person years in 12 studies. Significant heterogeneity was seen with potential sources identified through our sensitivity analysis including diagnostic method utilised, study size and location of study.
Conclusions
The mental health impact in patients with prostate cancer is significant. Depressive, anxiety, and suicidal symptoms were common. Additionally, a high suicide mortality rate was identified when compared to general population estimates. Screening of patients and integration of physical and mental health care should be evaluated further to improve quality of life and functional outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
De Angelis R, Sant M, Coleman MP, Francisci S, Baili P, Pierannunzio D, et al. Cancer survival in Europe 1999-2007 by country and age: results of EUROCARE-5-a population-based study. Lancet Oncol. 2014;15:23–34.
Bourke L, Boorjian SA, Briganti A, Klotz L, Mucci L, Resnick MJ, et al. Survivorship and improving quality of life in men with prostate cancer. Eur Urol. 2015;68:374–83.
Pitman A, Suleman S, Hyde N, Hodgkiss A. Depression and anxiety in patients with cancer. BMJ. 2018;361:k1415.
Fervaha G, Izard JP, Tripp DA, Rajan S, Leong DP, Siemens DR. Depression and prostate cancer: a focused review for the clinician. Urol Oncol. 2019;37:282–8.
Nead KT, Sinha S, Yang DD, Nguyen PL. Association of androgen deprivation therapy and depression in the treatment of prostate cancer: a systematic review and meta-analysis. Urol Oncol. 2017;35:664.e1–9.
Dickey SL, Grayson CJ. The quality of life among men receiving active surveillance for prostate cancer: an integrative review. Healthcare. 2019;7:14.
Dall’Era MA. Patient and disease factors affecting the choice and adherence to active surveillance. Curr Opin Urol. 2015;25:272–6.
Sciarra A, Gentilucci A, Salciccia S, Von Heland M, Ricciuti GP, Marzio V, et al. Psychological and functional effect of different primary treatments for prostate cancer: a comparative prospective analysis. Urol Oncol. 2018;36:340.e7–21.
Prasad SM, Eggener SE, Lipsitz SR, Irwin MR, Ganz PA, Hu JC. Effect of depression on diagnosis, treatment, and mortality of men with clinically localized prostate cancer. J Clin Oncol. 2014;32:2471–8.
Kolva E, Hoffecker L, Cox-Martin E. Suicidal ideation in patients with cancer: a systematic review of prevalence, risk factors, intervention and assessment. Palliat Support Care. 2020;18:206–19.
Amiri S, Behnezhad S. Cancer diagnosis and suicide mortality: a systematic review and meta-analysis. Arch Suicide Res. 2020;24:S94–S112.
Klaassen Z, Wallis CJD, Chandrasekar T, Goldberg H, Sayyid RK, Williams SB, et al. Cancer diagnosis and risk of suicide after accounting for prediagnosis psychiatric care: a matched-cohort study of patients with incident solid-organ malignancies. Cancer. 2019;125:2886–95.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:39.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–9.
World Health Organization. Depression and other common mental disorders: global health estimates. Geneva: World Health Organization; 2017.
Walker J, Holm Hansen C, Martin P, Sawhney A, Thekkumpurath P, Beale C, et al. Prevalence of depression in adults with cancer: a systematic review. Ann Oncol. 2013;24:895–900.
Krebber AMH, Buffart LM, Kleijn G, Riepma IC, de Bree R, Leemans CR, et al. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psychooncology. 2014;23:121–30.
Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. 2013;14:721–32.
Borges G, Nock MK, Haro Abad JM, Hwang I, Sampson NA, Alonso J, et al. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry. 2010;71:1617–28.
Misono S, Weiss NS, Fann JR, Redman M, Yueh B. Incidence of suicide in persons with cancer. J Clin Oncol. 2008;26:4731–8.
Watts S, Leydon G, Birch B, Prescott P, Lai L, Eardley S, et al. Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open. 2014;4:e003901.
Guo Z, Gan S, Li Y, Gu C, Xiang S, Zhou J, et al. Incidence and risk factors of suicide after a prostate cancer diagnosis: a meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 2018;21:499–508.
Kinsella N, Stattin P, Cahill D, Brown C, Bill-Axelson A, Bratt O, et al. Factors influencing men’s choice of and adherence to active surveillance for low-risk prostate cancer: a mixed-method systematic review. Eur Urol. 2018;74:261–80.
Nguyen TQ, Simpson PM, Braaf SC, Cameron PA, Judson R, Gabbe BJ. Level of agreement between medical record and ICD-10-AM coding of mental health, alcohol and drug conditions in trauma patients. Health Inf Manag. 2019;48:127–34.
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8:2861.
Levis B, Yan XW, He C, Sun Y, Benedetti A, Thombs BD. Comparison of depression prevalence estimates in meta-analyses based on screening tools and rating scales versus diagnostic interviews: a meta-research review. BMC Med. 2019;17:65.
Recklitis CJ, Syrjala KL. Provision of integrated psychosocial services for cancer survivors post-treatment. Lancet Oncol. 2017;18:e39–50.
Niedzwiedz CL, Knifton L, Robb KA, Katikireddi SV, Smith DJ. Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer. 2019;19:943.
Galway K, Black A, Cantwell M, Cardwell CR, Mills M, Donnelly M. Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients. Cochrane Database Syst Rev. 2012;11:CD007064.
Acknowledgements
OB, PD, and KA acknowledge research support from the Medical Research Council (MRC) Centre for Transplantation and funding from the King’s Medical Research Trust (KMRT). PD further acknowledges funding from the King’s College London-Vattikuti Institute of Robotic Surgery and the Guy’s and St. Thomas’ (GSTT) Charity. KA further acknowledges funding from the Royal College of Surgeons of England, The Urology Foundation, Coptcoat Charity and the Pelican Foundation. RS is part-funded by: (1) the National Institute for Health Research (NIHR) Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King’s College London; (2) a MRC Mental Health Data Pathfinder Award to King’s College London; (3) an NIHR Senior Investigator Award; (4) the NIHR Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
OB, SH, and KA contributed to the study concept and design. OB, SH, and AM contributed to the literature search and data collection. OB, GG, MVH, RS, and KA contributed to the data analysis and interpretation of the data. OB contributed to the drafting of the paper. OB, PD, RS, and KA contributed to the critical revision of the paper All authors approved the final paper for submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Brunckhorst, O., Hashemi, S., Martin, A. et al. Depression, anxiety, and suicidality in patients with prostate cancer: a systematic review and meta-analysis of observational studies. Prostate Cancer Prostatic Dis 24, 281–289 (2021). https://doi.org/10.1038/s41391-020-00286-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-00286-0
This article is cited by
-
Trends in suicide mortality among prostate cancer survivors in the United States, 1975–2019
BMC Public Health (2024)
-
Supportive care interventions for men with urological cancers: a scoping review
Supportive Care in Cancer (2023)
-
The relationship between loneliness, psychological resilience, quality of life and taste change in cancer patients receiving chemotherapy
Supportive Care in Cancer (2023)
-
Anxiety in oncology outpatients is associated with perturbations in pathways identified in anxiety focused network pharmacology research
Supportive Care in Cancer (2023)
-
Health status and associated factors of middle-aged and older adult cancer survivors in India: results from the Longitudinal Ageing Study in India
BMC Cancer (2022)