Abstract
Study design
A retrospective study.
Objectives
To assess the validity and reliability of cervical sagittal alignment parameters from multipositional magnetic resonance imaging (MRI) and dynamic cervical radiography.
Setting
Hospital in Suzhou, China.
Methods
Patients who underwent both multipositional MRI and dynamic plain radiography of the cervical spine within a 2-week interval between January 2013 and October 2021 were retrospectively enrolled in this study. The C2–7 angle, C2–7 cervical sagittal vertical axis (C2–7 SVA), T1 slope (T1S), cervical tilt, cranial tilt, and K-line tilt were measured in three different positions (neutral, flexion, and extension) with multipositional MRI and dynamic radiography. Inter- and intraobserver reliabilities were assessed by intraclass correlation coefficients (ICCs). Pearson correlation coefficients were used for statistical analyses.
Results
A total of 65 (30 males and 35 females) patients with a mean age of 53.4 years (range 23–69 years) were retrospectively enrolled in this study. Significant positive correlations were noted regarding all parameters between the plain radiographs and multipositional MRI images. Inter- and intraobserver reliabilities were excellent for all cervical sagittal alignment parameters measured in the two imaging modalities. All cervical sagittal parameters had significant positive correlations with those from multipositional MRI in all three positions (p < 0.05). Pearson correlation coefficients demonstrated moderate and strong correlations between the two examinations.
Conclusions
Cervical sagittal alignment parameters measured on multipositional MRI could reliably substitute for those measured on plain radiographs. Multipositional MRI is a valuable, radiation-free alternative for diagnostic evaluation in degenerative cervical diseases.
Similar content being viewed by others
Introduction
The concept of cervical sagittal balance is closely associated with patients’ quality of life and has gained increasing interest in the field of spinal deformity in recent years [1,2,3,4]. Sagittal imbalance of the spine has been extensively studied in relation to acceleration of degenerative diseases, complications after spinal surgeries and the exacerbation of clinical symptoms [5,6,7,8,9]. Therefore, accurate assessment of the spine sagittal plane requires good cervical parameters and remains a heated topic among researchers. Many radiological parameters have been identified to be highly associated with cervical sagittal balance. For example, several studies proposed that the T1 slope (T1S) was correlated with cervical spinal sagittal balance and was as critical as the relationship between pelvic incidence and lumbar lordosis [10,11,12]. Xing et al. [13] investigated the characteristics and relationships of cervical sagittal parameters from both cervical conventional MRI images and radiographs. They found that T1S was involved in the occurrence and development of cervical disc degeneration. Fujiyoshi et al. [14] first reported the K-line, which could reflect the alignment and thickness of the ossification of the posterior longitudinal ligament (OPLL) and has been widely used in making decisions about the surgical approaches for patients with OPLL and assessing surgical outcomes [15, 16]. Recently, the K-line tilt, a newly studied concept and first described by Kim et al. [17], has been reported to be a good cervical parameter, just as the C2–7 cervical sagittal vertical axis (C2–7 SVA) is, and a close relationship between the K-line tilt and C2–7 SVA has been established.
Dynamic plain radiographs are frequently used to evaluate degenerative cervical diseases and are easily accessible and affordable. However, plain radiographs provide only two dimensions of bony structures and cannot accurately quantify parameters about cervical sagittal balance due to the invisible sternum contour and T1 vertebra. In addition, it is obvious that patients are exposed to harmful ionizing radiation during radiographic procedures, which enhances risks for health, especially for pregnant women, children, and individuals requiring repeated radiographic evaluations [18,19,20,21]. Therefore, an examination with no radiation or less radiation than plain radiographs should be considered.
Recently, studies focusing on the advantages of magnetic resonance imaging (MRI) in evaluating degenerative spinal diseases have begun to accumulate. Compared with plain radiography, MRI examinations lack ionizing radiation, provide clear visibility of anatomic landmarks and produce accurate measurement results [22, 23]. However, radiographic findings from conventional MRI with patients in the supine position may mismatch the dynamic changes that occur with motion due to the effects of gravity on the spine. This disadvantage could be ameliorated with multipositional MRI. Multipositional MRI, as a novel and noninvasive technology, allows imaging in various weight-bearing positions and offers evaluation in different positions [24] and has been considered a meaningful radiographic examination for evaluating degenerative spinal diseases [25, 26]. Nigro et al. [27] found that multipositional MRI could detect a large number of spinal cord compressions and could provide more useful information than static exams.
Previous studies have compared some cervical sagittal parameters on radiographs and supine MRI images. Qiao et al. [28] compared T1S with supine MRI and found no significant differences between the two imaging modalities. They concluded that supine MRI could serve as a good substitute for X-ray scans with regard to the measurement of T1S. Lee et al. [16] evaluated C2–7 SVA, C2–7 angle, and T1S from standing plain radiographs, supine CT scans, and supine MRI images and found that MRI images were a good alternative to plain radiographs regarding those parameters. In contrast, Xing et al. [29] measured and compared some cervical sagittal parameters on radiographs and MRI images, but they concluded that most sagittal parameters could be affected by positional changes, and supine MRI images could not substitute for upright cervical radiographs for the measurement of most parameters. However, few studies have been conducted to compare cervical sagittal parameters on plain radiographs and multipositional MRI images. Hence, whether these two imaging examinations could substitute each other remains unknown. The aim of this study was to assess the correlations and differences in cervical sagittal alignment parameters between multipositional MRI and dynamic plain radiography.
Materials and methods
From January 2013 to October 2021, patients who received cervical examinations with both multipositional MRI and dynamic plain radiography within two weeks were retrospectively enrolled in the study. The inclusion criteria were as follows: age ≥20 years; patients with neck pain, radiculopathy symptoms, and/or myelopathy. Patients with recent spinal trauma, congenital spinal anomaly, spinal deformity, spinal infection, spinal inflammatory disease, spinal tumor, and history of spinal surgery were excluded. This study was reviewed and approved by the institutional review board of the Second Affiliated Hospital of Soochow University, and written informed consent was obtained from all participants in this study.
All participants were scanned in a 0.25 Tesla MRI machine (G-scan, ESAOTE, Italy) in three positions: flexion (40°), neutral (0°), and extension (−20°). The scans included T1-weighted and T2-weighted sagittal fast spin-echo images. Each patient received dynamic plain radiography in neutral, flexion, and extension positions, with angles similar to those of multipositional MRI. All the images were viewed and measured using the PACS viewer system (version 5.5, Neusoft Corp., Shenyang, China).
Measurements
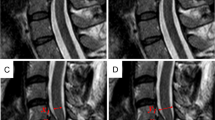
All cervical sagittal alignment parameters were measured using the methods described below (Figs. 1, 2).
-
1.
The C2–7 angle was defined as the angle between the tangent lines of the lower endplates of the C2 and C7 vertebral bodies in a weight-bearing sagittal view. A positive value indicated kyphotic alignment, whereas a negative value indicated lordotic alignment.
-
2.
The C2–7 SVA was defined as the horizontal distance between the center of C2 and the posterior edge of the C7 upper endplate. The C2 center was the point of intersection of crossing diagonals within the C2 vertebral body on the central sagittal MRI picture. A positive value of C2–7 SVA indicated that the C2 center was anterior to the posterior edge of the C7 upper endplate, while a negative value indicated that the C2 center was posterior to the posterior edge of the C7 upper endplate.
-
3.
T1S was measured as the angle between the T1 upper endplate (T1UEP) and a horizontal line.
-
4.
Cervical tilt is the angle formed between the vertical line from the center of T1UEP and the line from the center of T1UEP to the tip of the dens.
-
5.
Cranial tilt is the angle formed between the line from the center of the T1UEP to the dens and the SVA from the T1UEP.
-
6.
The K-line is a line that links the center of the spinal canal at C2 and C7.
-
7.
The K-line tilt is the angle between the K-line and a line perpendicular to the horizon.
Statistical analysis
All images were acquired from the PACS viewer system and were independently evaluated by two spine surgeons with 8 years of experience. The intra- and interobserver reliability for each parameter in both modalities was analyzed by the intraclass correlation coefficients (ICCs). The ICC values were assessed using the following criteria: ICC values <0.40 were considered poor; 0.40–0.59 were considered fair; 0.60–0.74 were considered good; and 0.75–1.00 was considered excellent. The correlation between the 2 measurement methods for each parameter was analyzed by the Pearson correlation test. A Pearson correlation coefficient (r) of 0.00–0.19 was considered very weak; 0.20–0.39, weak; 0.40–0.59, moderate; 0.60–0.79, strong; and 0.80–1.0, very strong. Statistical analyses were performed using SPSS Statistics software (version 23; SPSS Inc, Chicago, IL, USA), and a p-value less than 0.05 was considered significant.
Results
Demographic factors
Images from a total of 65 (30 males and 35 females) patients with a mean age of 53.4 years (range 23–69 years) were reviewed after careful evaluation based on the inclusion and exclusion criteria. The means and standard deviations of the C2–7 angle, C2–7 SVA, T1S, cervical tilt, cranial tilt, and K-line tilt measurements were shown in Table 1.
Reliability
The reliability results were shown in Table 2. Intraobserver reliability was excellent for all cervical sagittal alignment parameters, with ICCs ranging from 0.792 to 0.992 for plain radiographs and 0.854 to 0.942 for multipositional MRI images. Interobserver reliability was excellent for all parameters, with ICCs ranging from 0.761 to 0.915 for plain radiographs and 0.853 to 0.901 for multipositional MRI images.
Validity
All cervical sagittal parameters had a significantly positive correlation with those from multipositional MRI in all three positions (p < 0.05). Pearson correlation coefficients demonstrated moderate and strong correlations between the two imaging modalities, with r values ranging from 0.421 to 0.752 (Table 1).
Discussion
Dynamic radiographs are frequently used in the evaluation of cervical instability. However, it is difficult to accurately measure the T1S due to the unsatisfactory visibility of the T1 vertebra in cervical plain radiographs. In our study, 45 of 110 subjects were excluded due to this issue. MRI, on the contrary, can provide clear details of soft tissues and easily measure cervical sagittal parameters. Cervical sagittal alignments in previous studies were mostly obtained from plain radiographs, and little attention had been given to MRI until recently. Oshina et al. [30] investigated the difference in alignment between standing radiographs and supine MRI images and assessed whether neck position could affect cervical parameters and neurological changes. The results showed that neck tilt was a constant parameter, and the C2–7 angle in the kyphotic group was similar; however, in the lordotic group, these measures were different between the two imaging examinations. Lee et al. [16] assessed the validity and reliability of cervical alignment parameters from standing cervical radiographs and supine MRI images and found significant differences regarding C2–7 SVA and C2–7 angle. Other studies also revealed that radiological images obtained from conventional MRI with patients in the supine position may not precisely reflect the actual conditions of the cervical spine in the upright position [28, 31].
The effects of gravity on the spine differ between upright and supine positions, and assessments of the actual condition of spine pathologies might be significantly altered. Multipositional MRI can be used to define spine motion regions and capture each segment’s mobility of the cervical spine, which are not identifiable with the conventional MRI. Further, it can be used to assess not only the angular parameters of the cervical spine, but also the quality of cervical structures including intervertebral discs or ligamentum flavum (LF). For example, a previous research by Zhong et al. [32] found that the frequency and depth of missed LF bulge were highest at C5–C6 and C4–C5 segments in the extension position. Another study by Hayashi et al. [33] showed that dynamic cord compression was mostly detected at the C5–C6 segment. Therefore, multipositional MRI allowing patients to be scanned in three weight-bearing positions seems to be a better alternative.
In this study, our results showed that cervical sagittal alignment parameters measured from lateral cervical dynamic plain radiographs and multipositional MRI images had significantly positive correlations. The intra- and interobserver reliability in both groups was excellent. Our results were in line with a previous study conducted by Paholpak et al. [34], which also showed a positive correlation between multipositional MRI and dynamic X-ray for measuring the C2–7 angle and segmental cervical angles, with excellent ICC results (0.762–0.968). However, other cervical parameters, such as C2–7 SVA, T1S, cervical tilt, cranial tilt, and K-line tilt, were not measured and analyzed in that study. The regression analysis for each parameter also revealed a significant correlation between the two imaging modalities. These findings suggested that radiographic parameters measured from the two examinations could substitute for each other. In addition, it is highly possible that multipositional MRI with patients in different weight-bearing positions can show the actual status of the spine and reveal abnormalities that are usually missed in supine MRI.
Cumulative radiation exposure from medical imaging is reported to be associated with cancer risks [35] and may be hazardous to patients with recurrent or chronic diseases due to multiple imaging procedures. Moreover, it has been reported that children with scoliosis may exhibit a higher incidence of breast cancer and leukemia later in life because of repeated spinal radiographic examinations [18, 36]. Hence, there is no doubt that every effort should be made to lower radiation exposure for adults and children. From this perspective, MRI without radiation should be considered before consideration of plain radiography.
Although multipositional MRI has many advantages, it is not universally available due to limited access to it. To the best of our knowledge, although multipositional MRI has been investigated for many years, only several spine centers are currently equipped with multipositional MRI machines. As a result, plain radiographs should still be the first choice for the evaluation of degenerative cervical diseases due to their availability and affordability. However, since multipositional MRI could be reliably used to measure several cervical parameters according to our results, it might serve as an alternative for patients with cervical degenerative diseases. In addition, multipositional MRI images provide clearer visualization and more accurate results than plain radiographs in assessing lower cervical levels, which are not accurately measured in plain radiographs [37]. For the measurement of T1S in our study, both intra- and interobserver reliability of plain radiographs were lower than those obtained with the multipositional MRI, indicating the advantages of multipositional MRI in measuring T1S. Given these benefits, multipositional MRI images could be a substitute for plain radiographs, especially for individuals with high radiation risk, such as pregnant women and children.
Despite the benefits and encouraging results, the present study has several limitations. First, the number of enrolled subjects was small. Studies with a larger sample size are warranted to reveal the potential differences between the two imaging modalities. Second, differences in cervical sagittal alignment parameters might have existed due to changes in symptoms and deformity during the 2-week interval between scans. A smaller time interval between assessments with the two imaging modalities should be considered. Third, some small changes in the cervical spine might have been overlooked due to the low magnetic field strength (0.25 T) of multipositional imaging [38], even though the inter- and intraobserver reliability was high in our results. What’s more, the lower radiation exposure using multipositional MRI has to be weighed against its higher cost compared with X-Rays, and the cost and time cost are of great challenge for multipositional MRI to become a routine tool currently. Further research into MRI algorithms for the rapid and inexpensive evaluation of the spine is therefore required.
Conclusions
Cervical sagittal alignment parameters measured on multipositional MRI images could reliably substitute for those measured on plain radiographs. Given its affordability and accessibility, plain radiography is the first choice for evaluating cervical spinal diseases, while multipositional MRI provides satisfactory visibility of anatomical landmarks while minimizing exposure to ionizing radiation. Multipositional MRI is a meaningful alternative for evaluating degenerative cervical diseases and could be an alternative for patients with radiation risks, including pregnant women and children. The selection of imaging modalities should be individualized with regard to the cost, radiation risk, and the parameter of cervical alignment being measured. However, since the number of enrolled subjects was small, further study in a broader population (i.e., patients with spinal deformity, degenerative spinal instability) should be performed to determine how generalisable these findings are.
Data availability
The data generated or analyzed during this study can be found in the published article.
References
Batzdorf U, Batzdorff A. Analysis of cervical spine curvature in patients with cervical spondylosis. Neurosurgery. 1988;22:827–36.
Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Relationship between T1 slope and cervical alignment following multilevel posterior cervical fusion surgery: Impact of T1 slope minus cervical Lordosis. Spine (Phila Pa 1976). 2016;41:E396–402.
Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2015;76:S14–21.
Scheer JK, Tang JA, Smith JS, Acosta FL Jr., Protopsaltis TS, Blondel B, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine. 2013;19:141–59.
Ferrara LA. The biomechanics of cervical spondylosis. Adv Orthop. 2012;2012:493605.
Boseker EH, Moe JH, Winter RB, Koop SE. Determination of “normal” thoracic kyphosis: a roentgenographic study of 121 “normal” children. J Pediatr Orthop. 2000;20:796–8.
Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10:994–8.
Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976). 2009;34:785–91.
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine. 2006;31:2329–36.
Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012;25:E41–7.
Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–8.
Jang JS, Lee SH, Min JH, Kim SK, Han KM, Maeng DH. Surgical treatment of failed back surgery syndrome due to sagittal imbalance. Spine. 2007;32:3081–7.
Xing R, Liu W, Li X, Jiang L, Yishakea M, Dong J. Characteristics of cervical sagittal parameters in healthy cervical spine adults and patients with cervical disc degeneration. BMC Musculoskelet Disord. 2018;19:37.
Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine. 2008;33:E990–3.
Lee H, Nicholson LL, Adams RD. Cervical range of motion associations with subclinical neck pain. Spine. 2004;29:33–40.
Lee HD, Jeon CH, Chung NS, Kwon HJ. Comparative analysis of three imaging modalities for evaluation of cervical sagittal alignment parameters: a validity and reliability study. Spine. 2017;42:1901–7.
Kim HS, Kim TH, Park MS, Kim SW, Chang HG, Kim JH, et al. K-line tilt as a novel radiographic parameter in cervical sagittal alignment. Eur Spine J. 2018;27:2023–8.
Nash CL Jr., Gregg EC, Brown RH, Pillai K. Risks of exposure to X-rays in patients undergoing long-term treatment for scoliosis. J Bone Joint Surg Am. 1979;61:371–4.
Goldberg MS, Mayo NE, Levy AR, Scott SC, Poitras B. Adverse reproductive outcomes among women exposed to low levels of ionizing radiation from diagnostic radiography for adolescent idiopathic scoliosis. Epidemiology. 1998;9:271–8.
Bone CM, Hsieh GH. The risk of carcinogenesis from radiographs to pediatric orthopaedic patients. J Pediatr Orthop. 2000;20:251–4.
Kleinerman RA. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr Radiol. 2006;36:121–5.
Shi B, Mao S, Wang Z, Lam TP, Yu FW, Ng BK, et al. How does the Supine MRI correlate with standing radiographs of different curve severity in adolescent idiopathic Scoliosis? Spine. 2015;40:1206–12.
Lee MC, Solomito M, Patel A. Supine magnetic resonance imaging Cobb measurements for idiopathic scoliosis are linearly related to measurements from standing plain radiographs. Spine. 2013;38:E656–61.
Tykocki T, du Plessis J, Wynne-Jones G. Correlation between the severity of myelopathy and cervical morphometric parameters on dynamic magnetic resonance imaging. Acta Neurochir. 2018;160:1251–8.
Joaquim AF, Baum GR, Tan LA, Riew KD. Dynamic cord compression causing cervical myelopathy. Neurospine. 2019;16:448–53.
Michelini G, Corridore A, Torlone S, Bruno F, Marsecano C, Capasso R, et al. Dynamic MRI in the evaluation of the spine: state of the art. Acta Biomed. 2018;89:89–101.
Nigro L, Donnarumma P, Tarantino R, Rullo M, Santoro A, Delfini R. Static and dynamic cervical MRI: two useful exams in cervical myelopathy. J Spine Surg. 2017;3:212–6.
Qiao J, Zhu F, Liu Z, Xu L, Zhu Z, Qian B, et al. Measurement of thoracic inlet alignment on MRI: Reliability and the influence of body position. Clin Spine Surg. 2017;30:E377–E380.
Xing R, Zhou G, Chen Q, Liang Y, Dong J. MRI to measure cervical sagittal parameters: a comparison with plain radiographs. Arch Orthop Trauma Surg. 2017;137:451–5.
Oshina M, Tanaka M, Oshima Y, Tanaka S, Riew KD. Correlation and differences in cervical sagittal alignment parameters between cervical radiographs and magnetic resonance images. Eur Spine J. 2018;27:1408–15.
Jun HS, Chang IB, Song JH, Kim TH, Park MS, Kim SW, et al. Is it possible to evaluate the parameters of cervical sagittal alignment on cervical computed tomographic scans? Spine. 2014;39:E630–6.
Zhong G, Buser Z, Lao L, Yin R, Wang JC. Kinematic relationship between missed ligamentum flavum bulge and degenerative factors in the cervical spine. Spine J. 2015;15:2216–21.
Hayashi T, Wang JC, Suzuki A, Takahashi S, Scott TP, Phan K, et al. Risk factors for missed dynamic canal stenosis in the cervical spine. Spine. 2014;39:812–9.
Paholpak P, Tamai K, Shoell K, Sessumpun K, Buser Z, Wang JC. Can multi-positional magnetic resonance imaging be used to evaluate angular parameters in cervical spine? A comparison of multi-positional MRI to dynamic plain radiograph. Eur Spine J. 2018;27:1021–7.
Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology. 2009;251:175–84.
Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE. Breast cancer mortality after diagnostic radiography: findings from the U.S. Scoliosis Cohort Study. Spine. 2000;25:2052–63.
Sierink JC, van Lieshout WA, Beenen LF, Schep NW, Vandertop WP, Goslings JC. Systematic review of flexion/extension radiography of the cervical spine in trauma patients. Eur J Radiol. 2013;82:974–81.
Zhou Z, Jin Z, Zhang P, Shan B, Zhou Z, Zhang Y, et al. Correlation between dural sac size in dynamic magnetic resonance imaging and clinical symptoms in patients with lumbar spinal Stenosis. World Neurosurg. 2020;134:e866–e873.
Funding
This research is funded by the Suzhou Special Foundation of Clinical Key Diseases Diagnosis and Therapy (LCZX501904).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Zhiqiang Zhou, Fanguo Lin, Yao Zhang, Zhigao Jin, Dong Liu, and Yekun Deng. The first draft of the manuscript was written by Zhiqiang Zhou, Fanguo Lin, and Yao Zhang, reviewed and edited by Xiaotong Wang and Xiaozhong Zhou. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standard of the institutional and/or national research committee and with the 1964 Helsinki declaration and its amendments or comparable ethical standards. This study was ethically approved by the institutional review board of the Second Affiliated Hospital of Soochow University.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publication
Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, Z., Lin, F., Zhang, Y. et al. Correlation and reliability of cervical sagittal alignment parameters between plain radiographs and multipositional MRI images. Spinal Cord 61, 307–312 (2023). https://doi.org/10.1038/s41393-023-00895-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00895-1