Abstract
Randomized controlled trials (RCTs) have been considered as gold standard for establishing the efficacy and safety of investigational new drugs; nonetheless, the generalizability of their findings has been questioned. To address this issue, an increasing number of naturalistic studies and real-world database analyses have been conducted. The question of how much information from these two approaches is congruent or discrepant with each other is of great importance for the clinical practice. To answer this question, we focused on data from the antipsychotic (AP) treatment of schizophrenia. Our aim was two-fold: to conduct a meta-analysis of real-world studies (RWS), and to compare the results of RWS meta-analysis with previously published meta-analyses of RCTs. The principal measure of effectiveness was all-cause treatment discontinuation for both RWS and RCTs (when not available, then drop out for RCTs). We included publications for 8 selected APs (oral formulations of amisulpride, aripiprazole, clozapine, haloperidol, olanzapine, quetiapine, risperidone, and long-acting injectable (LAI) risperidone). We identified 11 RWS and 7 RCT meta-analyses for inclusion. Our results indicated that the RWS yielded statistically conclusive and consistent findings across individual investigations. For the overwhelming majority of the comparisons where both RWS and RCT meta-analyses were available, there was good congruency between the RWS and the RCT results. Our results support that RCTs, despite their limitations, provide evidence which is generalizable to real-world settings. This is an important finding for both regulators and clinicians. RWS can provide guidance for situations where no evidence is available from double-blind clinical trials.
Similar content being viewed by others
Introduction
Antipsychotic drugs (AP) are recommended both for the short-term treatment of acute episodes as well as for the long-term maintenance treatment in schizophrenia [1]. The development of antipsychotics is regulated by competent authorities, which require evidence about efficacy and safety from randomized controlled trials for their approval [2,3,4]. As a consequence, RCTs, used during drug development, mostly do not yield direct head-to-head comparisons with the relevant treatments already available in clinical practice. The use and the exclusive use of placebo controls in schizophrenia studies has been challenged [3, 5].
Even though RCTs are considered to provide the highest grade of evidence, the question of generalizability of their results to real life outcomes arises for several reasons. These are, for example, the inclusion of highly selected non-representative samples in RCTs [6], fix doses, short duration, small sample size, and predominantly placebo control associated with regulatory recommendations [7]. While shorter duration in acute trials has been supported by data, which guides clinical practice [3], the number of long-term follow-up RCT studies is still small [8, 9]. Moreover, there is still a lack of clinically important real-world endpoints, such as hospitalization in these studies [10].
Most meta-analyses based on data from the registration studies as well as on post-marketing data do not overcome the problem of the lack of data for individual head-to-head comparisons since their outcome is an effect size against placebo, and less frequently against a standard comparator [11]. Network meta-analyses could potentially overcome this problem, i.e., they may yield data for comparative efficacy among medications, but they suffer from certain assumptions, including the generalizability of the efficacy estimates across all pair-wise comparisons, and the use of sparse data from the various nodes of individual comparisons [12]. An additional issue both for meta-analyses and network meta-analyses is the increasing placebo response rate in schizophrenia trials [13, 14].
To address the problem of generalizability of data of RCTs to real-world environments, two major approaches have been used: (1) naturalistic observational studies in real-world settings, and (2) large scale database analyses from healthcare databases.
Open label effectiveness trials are intended to address the questions as to how certain medications work in real-world clinical and non-clinical settings, but once again for reasons of feasibility these trials rarely include a wide range of medications. While they tend to focus on clinically relevant real-world endpoints, they are, nonetheless, somewhat limited by certain factors that also restrict RCTs (e.g., small sample size, lack of long-term follow-up) [15].
Database analyses of representative samples or of full, nationwide populations may hold-out the promise to overcome the above problems. These analyses rely on large samples, allow for head-to-head comparisons for a wide range of medications, can capitalize on endpoints with clinical as well as public health relevance, and make possible the investigation of long-term outcomes. Following patients both retrospectively and prospectively, they may potentially emulate clinical trials and observational studies, and allow for the adjustment for important prognostic factors and confounders. However, large representative databases for such analyses are available only in a few countries [16]. Database analyses are also limited by various factors including the lack of random assignments, lack of assurance of treatment adherence to the medication, lack of assessments based on specialized clinical instruments (e.g., disease specific rating scales), or detailed characterization of general physical health, etc.
To the best of our knowledge only one meta-analysis has been conducted so far to summarize empirical evidence, which is currently available from such data (using a real-world effectiveness endpoint which was time to all-cause medication discontinuation) in individual studies [17]. This meta-analysis focused on both observational studies and RCTs, but it compared only a single AP (olanzapine) with a limited set of APs. It should also be noted here that a comprehensive meta-analysis would not have been possible earlier due to the lack of availability of sufficient empirical data; with accumulating evidence this has now become possible. One major reason for the current lack of meta-analysis of real-world data is that the sample size in these studies is typically rather large, which appears to obviate the reason for a meta-analytic summary. Nonetheless, meta-analysis for real-world studies (RWS) can still be an important tool to synthesize the evidence and to assess the consistency and reliability of data that come from many samples or even populations, which can be clinically rather heterogeneous.
Thus, one of our principal goals in this investigation was to address the relevance of data from RCTs in schizophrenia (i.e., their predictive value) for the clinical practice. This may or may not support how regulatory agencies specify clinical design requirements in order to obtain clinically generalizable data (e.g., in terms of inclusion and exclusion criteria, sample size, endpoint definition, length of treatment, etc). The clarification of this question is of great importance from societal and individual patient perspective as well. In particular, doctors want to provide, and patients want to receive the best available treatment; the exposure of patients to an ineffective medication may result in avoidable suffering, healthcare costs and burden for the society.
Based on the considerations mentioned above our aim in this study was (1) to conduct a meta-analysis of data obtained from real-world settings; and (2) to compare the results of this meta-analysis with previously published meta-analyses of randomized controlled trials (RCTmeta) implementing head-to-head comparisons of antipsychotic treatments in schizophrenia.
To accomplish the above goals, in the current study we examined APs approved for the treatment of schizophrenia. We selected 8 APs: the first-generation AP haloperidol (date of approval (DOA) in Belgium = 1959 [18], and 1967 in the USA [19]); two early second-generation antipsychotics clozapine (DOA in the USA = 1989 [20], and in Switzerland and Austria 1972 [21]), and amisulpride (DOA in France = 1986 [22], and in the United Kingdom 1998 [22]); four new second-generation antipsychotics including risperidone (DOA in USA = 1993 [20]), olanzapine (DOA in USA = 1996 [20]), quetiapine (DOA in USA = 1997 [20]) and aripiprazole (DOA in USA = 2002 [20]), and finally the first second-generation long-acting injectable risperidone (DOA in USA = 2003 [20]). The reason for focusing on this group of medications was that they have been widely used for the treatment of schizophrenia across various countries, providing sufficient data for long-term follow-up in real-world settings (as the last marketing approval in the selected set of APs took place >15 years ago), and they are included in meta-analytic summaries yielding sufficient empirical data for our study. All-cause treatment discontinuation has been selected as an endpoint in this meta-analysis, since it has been found useful in treatment research as “…a clinically meaningful outcome that reflects the input of both the patient and the clinician” [23]. The adoption of all-cause treatment discontinuation as one of the endpoints in future RCTs may help better translate and back-translate treatment data between clinical trials and clinical practice.
Methods
Study endpoint
For real-world studies we focused on relative risk (RR) of all-cause treatment discontinuation due to any reason, adjusted for confounders in the original articles, as a principal measure of effectiveness in real-world environment. For RCTs we used all-cause discontinuation due to any reason or, in case this measure was unavailable, the drop out from the clinical trial was investigated as a surrogate measure. In case no data on relative risk was available in a paper, we used the odds ratio or the hazard ratio. If none of the above measures were available, the study was not included in our meta-analysis.
Included publications
The data source for the selection was the Pubmed database. The queries described below for selection were run on 25th of April 2020 without any limitation to the date of publication. We only focused on studies published in English.
Selection of real-world studies (RWS)
The selection of publications for the real-world dataset was conducted in two stages.
At stage 1, we applied a priori defined search criteria for the identification of potentially relevant articles. The search criteria were organized according to the following three queries (Q1–Q3):
-
Q1: antipsychotic*[Title/Abstract] AND ((real*[Title/Abstract] AND world*[Title/Abstract]) OR nationw*[Title/Abstract]) AND schizophren*[Title/Abstract] AND (effectiv*[Title/Abstract] OR discont*[Title/Abstract])
-
Q2: schizophren*[Title/Abstract] AND discont*[Title/Abstract] AND observational[Title/Abstract]
-
Q3: schizophren*[Title/Abstract] AND discont*[Title/Abstract] AND claim*[Title/Abstract]
The above queries yielded a total of 135, 69, and 36 articles, respectively, for the Q1, Q2, and Q3 queries. After merging the query results with the logical OR connection and omitting the duplicate entries, we obtained 224 unique articles. The dates when the articles were entered in Pubmed ranged from 01 March 1980 to 22 January 2020.
At stage 2, we implemented additional selection criteria in a hierarchical order to identify the final set of relevant publications. The selection criteria were employed using the full text papers (instead of the titles and abstracts) of the relevant publications. The selection process and the resultant set of publications is depicted in the flow chart shown in Fig. 1 (left panel). For further details of the selection process, please see Online Supplementary Information (Appendix 1). As a result of the selection process, we identified a total of 11 publications for the inclusion in the final set for our meta-analysis [16, 24,25,26,27,28,29,30,31,32,33].
As no direct head-to-head comparisons of monotherapies were published in the paper of Katona et al. [29], for the purpose of current investigation we used the relevant unpublished results available from the original analysis.
Selection of meta-analyses of RCTs
Similar to the selection process of RWS, the selection of publications for the meta-analytic dataset also included two stages.
At stage 1, we applied search criteria for the identification of relevant publications. The search criteria were organized according to the following query.
-
schizophren*[Title/Abstract] AND antipsychotic*[Title/Abstract] AND meta-analysis[Title/Abstract] AND (clinical[Title/Abstract] OR randomi*[Title/Abstract]) AND (trial*[Title/Abstract] OR study[Title/Abstract] OR studies[Title/Abstract])
The above query resulted in a total of 459 non-duplicate publications.
At Stage 2, we used additional selection criteria on the basis of the full text of the relevant publications. The selection process and the resultant set of publications is depicted in the flow chart shown in Fig. 1 (right panel). For further details of selection process, please see Online Supplementary Information (Appendix 2). As a result of the selection process, we identified six publications [17, 34,35,36,37,38], and our further literature review resulted in one more publication [39]. Hence, the set of publications that we used for the meta-analysis included a total of seven publications.
We note that during the selection for both RWS and meta-analytic summaries, the principal author identified the publications for inclusion; two of the authors (LK and PC) reviewed the results; in case of any discrepancy they had a discussion to achieve resolution.
Statistical methods
Statistical model
The pooled effect size for the relative risk of all-cause treatment discontinuation due to any reason for each of compared AP pairs was estimated using normal mixture model with random effect for meta-analysis. On the basis of individual publications, we used the estimated relative risks and their standard errors (SE) as input data for the meta-analysis. All analyses were conducted using the SAS statistical software version 9.4 (SAS Institute, Inc., Cary, NC). For further details of statistical model, please see Online Supplementary Information (Appendix 3).
Statistical procedures
Since our investigation is not a review of the literature but a meta-analysis, we did not include those AP pairs in the analyses which were compared in only one real-world study.
Thus, our meta-analysis of RWS studies was based on AP comparisons where at least two publications were available with respect to a given pair-wise comparison. Moreover, in order to take the weight of the evidence into consideration, we also separately examined AP comparisons where three or more individual study data were available for the analysis. We examined whether statistically conclusive evidence (p < 0.05 for the pooled meta-analytic estimate) was available for a given AP comparison, and further investigated whether this evidence was present consistently across all individual studies. Consistency was defined as the individual study outcomes pointing always in the same direction in terms of their estimated effect size. Thus, we classified AP comparisons into three classes including study outcomes as follows:
-
statistically conclusive and consistent;
-
statistically conclusive but inconsistent;
-
neither statistically conclusive nor consistent.
We note that for comparisons which included only two RWS, we provide the results in the Online Supplementary Information (Appendix 9, Part 2).
Since for the majority of RWS and RCTmeta comparison only one or two meta-analytic summaries were available we selected one primary and, whenever available, one secondary analysis as a benchmark for further comparisons. To consider a meta-analysis as an RCTmeta benchmark, we reviewed all the RCTs included in the meta-analysis. If there was a significant overlap between the RCTs, i.e., the majority of trials was included in both meta-analyses, we selected the meta-analyses which (1) was more recently published and/or (2) involved a larger number of RCTs. For those comparisons where more than one meta-analysis was available, we identified one primary and one secondary benchmark. To learn more about the selection process, please see Online Supplementary Information (eTable 1, Appendix 4).
In the final step in our analysis, we examined the congruency of the RWS estimates with RCTmeta benchmark(s). Congruency was defined as the correspondence between the sign of the pooled effect size estimate from the RWS and the benchmark RCTmeta analysis. Our presentation of the pertinent results was organized based on the presence/absence of statistically conclusive results in the RWS studies. Accordingly, we classified the comparison outcomes as follows:
-
RWS statistically conclusive and showing congruency with RCTmetas;
-
RWS statistically inconclusive but showing congruency with RCTmetas;
-
RWS statistically conclusive with incongruence with RCTmetas;
-
RWS statistically inconclusive and incongruent with RCTmetas.
We note that a number of comparisons for congruency could not be carried out in this analysis since no RCTmetas were available in the literature for the given AP comparisons we examined.
We also note that in order to increase clarity for the presentation of AP comparisons we used alphabetical order; therefore, whenever needed, we reciprocated the value that was provided in the original paper.
Results
Analyses of RWS
Descriptive statistics
We included a total of 11 studies in our meta-analysis based on the real-world data. Table 1 provides a brief description of the included studies. With respect to study design, 8 of 11 were based on database analysis using electronic medical/health insurance records and three of them represented observational studies. The list of the eight selected APs we investigated were as follows: amisulpride oral (AMI), aripiprazole oral (ARI), clozapine oral (CLO), haloperidol oral (HAL), olanzapine oral (OLA), quetiapine oral (QUE), risperidone oral (RIS), and risperidone LAI (RIS LAI).
Table 1 for each study displays both the full list of APs investigated in a given study, and the ones from the set of the 8 APs we focused on (listed above). In the next column (termed as “Control APs” in the table), we depicted those APs which were used as comparators in the original study. There were two studies which had more than one comparator in their respective pair-wise comparisons [25, 29]. As to the follow-up period of selected studies, the minimum duration was 12 months (n = 4), while there were studies which lasted 3 years or longer (n = 4). In one article, the length of follow-up period was not reported [30]. For the overwhelming majority of studies, a unique number of patients assigned to a given study medication was provided for each study arm; there was one study [33] where a within-subject approach was applied and no disjunct patient groups were formed, thereby no unique number of patients was available for the individual treatments. For the ten studies where the data in terms of unique treatment assignments were available, the total number of patients were the following: AMI = 2332, ARI = 2045, CLO = 2446, HAL = 426, OLA = 16924, QUE = 6101, RIS = 11897, and RIS LAI = 2367. Regarding basic demographic data, the mean age and/or gender distributions were published in eight papers. The mean and standard deviation of patients’ age (in years) for the selected APs were as follows: AMI = 45.5 (4.54), ARI = 43.4 (0.24), CLO = 40.9 (8.65), HAL = 39.8 (10.06), OLA = 41.0 (7.26), QUE = 45.2 (7.58), RIS = 42.9 (8.42), and RIS LAI = 46.7 (1.04). Furthermore, the percentage of male patients for each of the selected APs were as follows: AMI = 40.4%, ARI = 43.8%, CLO = 48.5%, HAL = 54.0%, OLA = 49.2%, QUE = 47.3%, RIS = 49.2%, and RIS LAI = 43.8%.
Raw data sources of the current meta-analysis in the original publications are depicted in Online Supplementary Information (eTable 2, Appendix 5).
Meta-analyses of RWS
Pooled results with two or more RWS datasets available
Here we investigated only those AP comparisons where at least two real-world results were available for the given pair-wise comparisons. The 8 APs can potentially yield 28 unique pair-wise comparisons. Based on the criterion of the availability of multiple studies for the pair-wise comparisons, out of the 28 comparisons we identified a total of 25 AP comparisons that could be subjected to the meta-analysis.
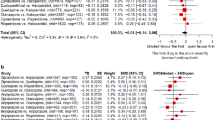
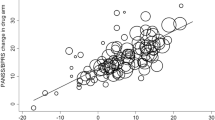
In 16 (64%) of the 25 individual paired comparisons our meta-analysis showed a significant difference between the two treatments. In terms of the magnitude of effect sizes, a large effect size was observed in one pair-wise comparison (CLO-HAL, RR = 0.33). In five of the remaining 24 comparisons the effect sizes were in the medium range (RR [or its reciprocal value] between 1.5 and 2). Figure 2A, B provide a graphical illustration and detailed numerical results of the individual pair-wise comparisons.
Results of individual studies included in the meta-analysis along with pooled meta-analytic estimates based on random effect model. The figure provides the results for the 25 individual pair-wise comparisons. The results of pair-wise comparison are arranged in alphabetical order. A Results for the first set of comparisons (n = 15); B Results for the second set of comparisons (n = 10). Relative Risk of discontinuation for the first and second APs is indicated as a value of <1 or >1, depending on whether the first or the second AP in the pair has superior or inferior efficacy, respectively. For example, in the clozapine vs. haloperidol pairwise comparison, clozapine was found to be superior over haloperidol as our pooled estimate was 0.33, while in the amisulpride vs. olanzapine comparison, olanzapine showed superiority over amisulpride with an RR of 1.45. For the graphical illustration, the UCL value (5.556) was truncated at 4 in the case of the haloperidol oral–olanzapine oral pair-wise comparison from the Jari Tiihonen (2006) study. RR relative risk, LCL lower confidence limit, UCL upper confidence limit. Blue The results of individual real-world studies, Red Pooled estimates of current meta-analysis.
Due to the alphabetical order of pair-wise comparisons, in Fig. 2A, B we indicate by an asterisk (*) whenever a reciprocal value of RR was used in the presentation in this paragraph. The rationale for this was to present the relative risks of the effectiveness of a particular AP in a consistent way compared to its comparators. Overall, OLA showed superiority in 5 of 7 comparisons including AMI, ARI, HAL, QUE, and RIS with reducing the risk of all-cause discontinuation to 0.69*, 0.88*, 0.58*, 0.72, and 0.71, respectively, while for the rest of the comparators (CLO, RIS LAI) there was no significant difference. RIS LAI was superior over five APs in six available comparisons including AMI, ARI, CLO, QUE, and RIS with a risk reduction to 0.66*, 0.79*, 0.74*, 0.75*, and 0.6, respectively, while for one comparator (OLA) there was no significant difference. ARI had superior efficacy in two of six available comparisons (RR for AMI = 0.78, RIS = 0.83) with reducing the risk of all-cause discontinuation (while it was inferior to OLA and RIS LAI). QUE was superior in two of seven available AP comparisons (RR for AMI = 0.88*, HAL = 0.64*) with reducing the risk of all-cause discontinuation (while it was inferior to OLA and RIS LAI). CLO and RIS were superior, respectively, to one comparator (CLO vs. HAL RR = 0.33, RIS vs. HAL RR = 0.65*).
Pooled results with three or more RWS datasets available
There were 17 out of 25 comparisons with three or more real-world studies included. We investigated whether these groups (i.e., AP pairs compared) yielded homogenous or heterogenous results in terms of the estimated effect sizes. We considered a group homogenous if the majority of the input data (individual study level estimates of all the relative risks within a group) from real-word studies were significantly less than 1; or greater than 1; or not differentiated from 1. There were 12 AP pairs (70.6%) where the input data can be considered homogenous: AMI-OLA, AMI-RIS LAI, ARI-OLA, ARI-RIS LAI, CLO-HAL, CLO-RIS LAI, HAL-QUE, HAL-RIS, OLA-QUE, OLA-RIS, QUE-RIS LAI, RIS LAI-RIS. We identified five groups (29.4%) where the input data were heterogenous: CLO-OLA, CLO-RIS, HAL-OLA, OLA-RIS LAI, QUE-RIS.
Specifically, out of the 17 pair-wise comparisons we found that 12 (70.6%) provided both statistically conclusive and consistent evidence for the relative superiority of the respective APs in the comparisons. One of the comparisons (5.9%) yielded statistically conclusive but inconsistent result across individual studies. The remaining four comparisons (23.5%) were both statistically inconclusive and inconsistent among each other. Please note that the proportion of AP comparison which relied on more than three individual studies did not differ across the three categories. Specifically, considering the group with statistically conclusive and consistent results there was one comparison which included eight individual studies; there were two comparisons relying on five studies; one based on four studies; and eight on three studies. For the group of statistically conclusive but inconsistent results there was one comparison which was based on five individual studies. Finally, in the group of statistically inconclusive and inconsistent results there were three comparisons which included four individual studies; one based on three studies.
With respect to the both statistically conclusive and consistent outcomes we found the following order of superiority (indicated by “>” greater sign) in terms of relative risk of all-cause discontinuation for the AP pairs in the individual pair-wise comparisons: OLA > RIS, OLA > QUE, HAL < RIS, RIS LAI > RIS, AMI < OLA, ARI < OLA, ARI < RIS LAI, CLO > HAL, AMI < RIS LAI, CLO < RIS LAI, HAL < QUE, and QUE < RIS LAI. For the group with statistically conclusive but inconsistent results we found the following order of superiority: HAL < OLA. The remaining four pair-wise comparisons with statistically inconclusive and inconsistent results were as follows: CLO-OLA, QUE-RIS, OLA-RIS LAI, and CLO-RIS.
Detailed findings for each of the pair-wise comparisons according to above categories are provided in Online Supplementary Information (Appendix 6).
Previously published meta-analyses based on RCTs (RCTmeta) as compared to meta-analytic results of RWS
Selection of primary and secondary benchmarks for comparisons with RWS
Our literature search yielded seven meta-analyses of RCTs. As described in the “Methods” section, we selected one primary and, whenever available, one secondary benchmark comparison for the RCTmetas (please see “Methods” section for details of the selection process). Overall, for the 17 AP RWS comparisons which had three or more results (of the total of 25 comparisons), we identified 13 relevant AP comparisons in previously published meta-analyses. For those comparisons where more than one RCTmetas were available we used both the primary and secondary benchmarks.
In Online Supplementary Information (eTable 3, Appendix 7) we provide basic descriptive statistics (i.e., the number of RCTs included) about prior meta-analyses based on randomized clinical trials.
Comparison of RWS with meta-analytic benchmarks from RCTs
The following part of this section is organized according to whether RWS provided conclusive evidence and/or the evidence was congruent with RCTmetas. Our results indicated that of nine RWS with statistically conclusive findings, the majority (n = 7; 77.8%) were congruent with RCTmetas. Of the three RWSs with statistically inconclusive findings, (n = 2; 66.7%) were congruent with the RCTmetas (see Online Supplementary Information (eTable 4, Appendix 8) for details).
The results of current study juxtaposed with the results of RCTmetas are presented in detail in a summary table (Table 2). In the following four sections of the Results, we rely on this table.
AP comparisons of RWS with statistically conclusive (“significant”) results showing congruency with RCTmetas
OLA-RIS: Our meta-analysis yielded an RR of 0.71 (95% CI = 0.59-0.85) favoring OLA. We identified one RCTmeta for primary and one for secondary benchmark, respectively. These meta-analyses had both numerically and statistically congruent results with our estimate (RR = 0.88 (95% CI = 0.83–0.93); RR = 0.80 (95%CI = 0.71–0.90)).
OLA-QUE: The current meta-analysis resulted in an RR of 0.72 (95% CI = 0.56–0.92) favoring OLA. We identified one RCTmeta for primary benchmark, and none for secondary benchmark. The primary benchmark meta-analysis had both numerically and statistically congruent result with our estimate (RR = 0.79 (95% CI = 0.71–0.89)).
ARI-OLA: Our pooled estimate for RR was 1.14 (95% CI = 1.07–1.20) favoring OLA. We identified one primary and no secondary RCTmeta benchmark. The primary benchmark resulted in both numerically and statistically congruent result with our estimate (RR = 1.17 (95% CI = 1.05–1.30).
ARI-RIS LAI: Our meta-analysis yielded an RR of 1.26 (95% CI = 1.13–1.42) favoring RIS LAI. We found only one RCTmeta as benchmark which showed a numerically congruent result with our estimate (RR = 1.20 (95% CI = 0.77–1.89). However, the latter RCTmeta estimate did not reach statistical significance due to the low number of trials included in the meta-analysis (N = 2).
CLO-HAL: The current meta-analysis resulted in an RR of 0.33 (95% CI = 0.14–0.75) favoring CLO. We selected only one RCTmeta for benchmark, which had a numerically congruent result with our estimate (RR = 0.53 (95% CI = 0.29–1.12). The latter RCTmeta estimate was not statistically significant owing to the low number of trials included in the meta-analysis (N = 3).
AMI-OLA: Our pool estimate for RR was of 1.45 (95% CI = 1.34–1.58) favoring OLA. We identified only one RCTmeta for benchmark. This meta-analysis had numerically congruent result with our estimate in terms of direction (RR = 1.07 (95% CI = 0.91–1.27)). This RCTmeta estimate did not reach statistical significance due to the modest effect size (RR = 1.07).
HAL-OLA: Our meta-analysis provided an RR of 1.73 (95% CI = 1.22–2.46) favoring OLA. We identified one RCTmeta for primary and one for secondary benchmark, respectively. These meta-analyses had both numerically and statistically congruent results with our estimate (RR = 1.54 (95% CI = 0.94–2.56); RR = 1.40 (95% CI = 1.20–1.70)).
Comparisons of RWS with statistically inconclusive results showing congruency with RCTmetas
CLO-OLA: The current meta-analysis resulted in RR of 0.96 (95% CI = 0.63–1.47), showing a lack of difference. We identified one RCTmeta for primary and one for secondary benchmark, respectively. These meta-analyses had both numerically and statistically congruent results with our estimate (RR = 1.01 (95% CI = 0.86–1.18); RR = 1.05 (95% CI = 0.75–1.47)), with no difference between these two APs.
CLO-RIS: Our pooled estimate for RR was 0.76 (95% CI = 0.42–1.38) which failed to reach statistical significance. We found only one RCTmeta for benchmark, which had a numerically congruent result with our estimate (RR = 0.74 (95% CI = 0.57–0.95)).
ARI-QUE: The current meta-analysis resulted in RR of 0.93 (95% CI = 0.86–1.01), showing a lack of difference. We identified one RCTmeta as primary benchmark which showed congruent result with our estimate (RR = 0.75 (95% CI = 0.38–1.45)). However, we note that our estimate here was based on only two available RWS (this result is presented in Fig. 3 but not in Table 2).
Outcome measure: treatment discontinuation due to any reason Groups: primary benchmark (blue); secondary benchmark (green); and pooled estimates of current meta-analysis (red). Please note that for the comparison of aripiprazole-quetiapine the pooled estimate RWS is only based on two studies. RR relative risk, LCL lower confidence limit, UCL upper confidence limit. Blue The results of individual meta-analyses based on randomized controlled trials’ data considered as primary benchmark. Green The results of individual meta-analyses based on randomized controlled trials’ data considered as secondary benchmark. Red Pooled estimates of current meta-analysis.
Comparison of RWS with statistically conclusive results showing incongruence with RCTmetas
HAL-RIS: Our meta-analysis provided an RR estimate of 1.60 (95% CI = 1.43–1.79). We had only one RCTmeta for benchmark, which provided a numerically incongruent result with our estimate (RR = 0.87 (95% CI = 0.31–2.44)), but did not reach statistical significance.
RIS LAI-RIS: The current meta-analysis resulted in an RR of 0.60 (95% CI = 0.50–0.73). We identified one RCTmeta for primary and one for secondary benchmark, respectively. These RCTmetas yielded a numerical (but not statistically significant) advantage for RIS vs. RIS-LAI (RR = 1.17 (95% CI = 0.95–1.44); RR = 1.28 (95% CI = 0.92–1.79)), while the meta-analysis of RWS showed a statistically significant superiority for RIS-LAI over RIS.
Comparison of RWS with statistically inconclusive results showing incongruence with RCTmetas
QUE-RIS: Our meta-analysis resulted in an RR of 0.84 (95% CI = 0.63–1.13) which failed to reach statistical significance. We found only one RCTmeta for benchmark, which had a numerically incongruent result with our estimate (RR = 1.07 (95% CI = 0.98–1.18)).
No RCTmetas were available
There were five comparisons which we could not identify any RCTmetas for: AMI-RIS LAI, CLO-RIS LAI, HAL-QUE, QUE-RIS LAI, and OLA-RIS LAI.
Discussion
The first objective of our study was to address an existing lack of information in the literature, namely the availability of the summary of evidence from real-world studies about the head-to-head comparisons of antipsychotic medications. This goal is clinically highly relevant since RCTs very rarely yield information for the comparative efficacy (or effectiveness) of an individual AP against its potential comparators used in clinical practice. To achieve our goal, we conducted a meta-analysis of eight APs (amisulpride, aripiprazole, clozapine, haloperidol, olanzapine, quetiapine, risperidone, and risperidone LAI). Based on the analysis of the literature, we found that published data were available for most of the comparisons (25 of 28 theoretically possible contrasts).
For the majority of comparisons based on three or more RWS, our results indicated that the real-world studies yielded statistically conclusive and, clinically even more importantly, consistent findings across the individual investigations. Indeed, out of 17 studies with sufficient empirical data (i.e., ≥3 RWS), the proportion of studies with both conclusive and consistent results was 70.6% (12 of 17). For those studies with statistically inconclusive and inconsistent results, several factors might have come into play, including the lack of true difference among medications in real-world settings, sampling variation, heterogeneity of study populations, study design, or confounding by indication due to differing clinical practices across countries (discussion of these studies is provided in Online Supplementary Information (Appendix 9)).
When we examined AP comparisons with at least two available studies, we found replicated evidence for certain AP comparisons. Specifically, OLA showed superiority in five of seven comparison APs including AMI, ARI, HAL, QUE, as well as RIS in terms of reducing the risk of all-cause discontinuation, and no difference against CLO and RIS LAI. RIS LAI was superior over five APs of six available comparisons including AMI, ARI, CLO, QUE, and RIS with a risk reduction (even though for AMI, ARI, CLO, QUE only one national database provided information for the analysis). QUE was superior at reducing the risk of all-cause discontinuation in two of seven available comparisons, one of which was against HAL, and the other one was AMI (with data available only from one national database).
Our second objective was to compare the real-world evidence with evidence from RCTs. This comparison is crucial from a clinical standpoint since RCTs are considered as providing the highest level of evidence for clinical practice in individual studies, yet the matching of the two types of evidence (real-world and RCT) is seldom accomplished in the literature. Our results showed that for the overwhelming majority of the comparisons where both real-world and RCTmeta were available (12 comparisons), there was a good congruency (75%, i.e., nine of 12) between the real-world and the RCT results. In addition, among the real-world studies with statistically conclusive results, most comparisons (77.7%, i.e., seven of nine) yielded results similar to those in RCT trials. Findings of the current study are therefore consistent with findings from Soares-Weiser et al.’s meta-analysis [17], which showed a good overall consistency between RCTs and observational studies based on a limited set of pair-wise comparisons (comparing olanzapine to six other APs). Specifically, the effect sizes were numerically similar between RCTs and observational studies in terms of their direction, apart from a single comparison (olanzapine vs. clozapine). For further details, please see Online Supplementary Information (eTable 5, Appendix 10).
Thus, our results support that randomized controlled trials, despite all of their limitations, provide evidence which is generalizable to real-world settings. These include that RCTs focus on special populations (e.g., exclude difficult to treat or violent subjects), apply a small sample size (typically less than 150 subjects per study arm), placebo control (as it is easier to demonstrate pivotal evidence for efficacy against placebo than an active comparator), have short duration (typically less than 24 weeks), very limited follow-up period (precluding the detection of late occurring drug effects), and lack of clinically highly relevant real-world endpoints as primary measures (e.g., hospitalization, treatment discontinuation). Altogether, this is an important finding from the perspective of the regulators, who strive to set up study specifications and guidelines in order to achieve the highest level of generalizability from the clinical trial domain to the actual clinical practice. These results are also encouraging for the clinical practice: the results of RCTs showed a good correspondence with those of real-world data from large healthcare datasets. Nonetheless, the predictive value of RCTs for real-world practice should regularly be assessed. Specifically, there still remains a need to examine the generalizability of the results of RCTs in long-term multi-arm non-randomized naturalistic studies or in analyses of healthcare databases.
As we expected, while head-to-head comparisons were more readily available in real-world studies, they were much less frequent in randomized clinical trials. Specifically, we found that only for 12 of 17 RWS comparisons with sufficient evidence (i.e., three or more real-world studies included) were data available from RCT meta-analyses; these constituted the set of pair-wise comparisons used for studying the congruency between RWS and RCT studies. Thus, our study provides empirical evidence that the RCT data adequately translate to clinical settings. Nevertheless, while our results show the generalizability of evidence with respect to a number of AP comparisons, they evidently do not pertain to AP comparisons with no available data from RCTs. Hence, the theoretical questions of how the RWS data would translate back to RCT settings, and whether the results for AP pairs with missing data in RCT settings would similarly generalize remain to be studied further.
Finally, we would like to note that there were three comparisons with incongruent results between RWS and RCTs, which included HAL-RIS, RIS LAI-RIS, and QUE-RIS. These may be resulted from several factors including the small sample size of the individual trials, as well as the heterogeneity of samples (see a discussion of this issue in Online Supplementary Information (Appendix 11).
Limitations
Pair-wise meta-analyses have been criticized in the literature because they typically rely on data from one pair of individual treatment comparison. In the current real-world meta-analysis, however, this limitation was not present when we took the weight of the evidence into consideration and relied predominantly on individual AP comparisons where at least three or more studies provided data. The fact that we were able to use multiple studies for the same pair-wise comparisons obviates the problem of heterogeneity at pooling data across various studies which is present in the current practice in network meta-analysis.
We also note that some of the differences in findings across RWS may come from differences in the methodological approaches including study design used by the various groups of investigators involved in the analysis (e.g., varying selection criteria such as inclusion of patients with first hospitalization). An additional limitation of our comparison of RWS and RCT meta-analyses could be that the studies included into the two analyses may have relied on different patient cohorts since therapeutic guidelines and practices changed over time with the introduction of newly approved APs to the market. However, an overview of publication dates and entry time window (2005–2019) for the two types of studies (i.e., RWS and RCT meta-analyses) reveals that they covered similar time periods, when the new second-generation antipsychotics were widely available on the market for treatment.
Furthermore, our analyses were limited by the fact that some of the basic descriptive demographic information was not available in five of the 11 RWS. Therefore, these data could not be included in our analysis in order to identify the sources that might have caused heterogeneity in the estimates of RWS. The availability of such data for the purpose of research synthesis including meta-analysis underlines the importance of reporting this information. In addition, the inconsistent findings in RCTs versus RWS about the comparative effectiveness of oral versus LAI formulations of second-generation APs have been addressed earlier: “LAIs are thought to be better via improved adherence, not via intrinsically better efficacy. Therefore, it is unclear whether LAIs were not superior because compliance with oral APs was good enough in the context of RCTs.” [40]. Thus, these findings may be explained by different rates of adherence in pivotal RCTs versus RWS.
Finally, our findings from the real-world studies that rely mostly on a limited set of countries (e.g., Scandinavian countries and Hungary) can be influenced by regional differences [41], therefore we cannot be certain that the results would generalize to most countries and regions of the world. We note, however, that some of RWS cover broad geographical regions that include the four continents or multiple European countries, which can add support to the notion of the broader generalizability of the results. Furthermore, the RWS show an imbalance in terms of the representations of the countries as some of the countries provided disproportionally more impute data for our analysis. For example, with respect to the comparisons with data from three or more RWS, there were some important comparisons where data was only available from one national health database (for amisulpride, aripiprazole and quetiapine vs risperidone LAI). Additionally, the RWS from various countries that we used in our study can be influenced by between country or regional differences in therapeutic practices, which determine medication assignments to various APs (e.g., due to different national guidelines). Nonetheless, we conclude that our results show a rather remarkable consistency in individual pairs of AP comparisons across studies, as well as a good congruency with the results of RCT meta-analyses.
Conclusions
The principal conclusion of the current study is that results of RCTs evidence a good congruency with those of the real-world studies. Moreover, the results of our analyses, taken together, hold out a promise that the findings of the RWS analysis would provide useful and much needed information for clinicians for everyday practice. Importantly, the findings of RWSs that pertain to comparisons of antipsychotic medications not yet subjected to clinical testing in RCTs are essential for three major reasons. First, they may provide putative guidance for practicing clinicians for situations where no evidence is available from double-blind clinical trials. Second, they can also provide specific testable hypotheses for clinically important questions in future clinical trials. Third, data from RWS analysis can provide essential information for regulators with respect to design requirements for future studies. For example, in terms of effect size criteria, RWS data would be essential to demonstrate superiority or equivalence of a new antipsychotic under development in the context of differences among currently available antipsychotic medications. While we focused on APs, we think that our results may have relevance to other therapeutic areas (e.g., diabetes, high blood pressure, etc.) since the use of APs can be considered as a prototype for medical conditions, where long term therapy presents a major challenge in patients living with chronic lifelong conditions. However, further studies are needed in other areas of indications in order to confirm the generalizability of our findings.
References
McCutcheon RA, Reis Marques T, Howes OD. Schizophrenia—an overview. JAMA Psychiatry. 2020;77:201–10.
European Medicines Agency: Guideline on clinical investigation of medicinal products in the treatment of schizophrenia. 2011. Publicly available document: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-investigation-medicinal-products-including-depot-preparations-treatment_en.pdf. Accessed 28 Apr 2021.
Younis IR, Gopalakrishnan M, Mathis M, Mehta M, Uppoor R, Zhu H. et al. Association of end point definition and randomized clinical trial duration in clinical trials of Schizophrenia medications. JAMA Psychiatry. 2020;77:1064–71.
Buchanan RW, Keefe RS, Umbricht D, Green MF, Laughren T, Marder SR. The FDA-NIMH-MATRICS guidelines for clinical trial design of cognitive-enhancing drugs: what do we know 5 years later? Schizophr Bull. 2011;37:1209–17.
Fleischhacker WW, Czobor P, Hummer M, Kemmler G, Kohnen R, Volavka J. Placebo or active control trials of antipsychotic drugs? Arch Gen Psychiatry. 2003;60:458–64.
Hofer A, Hummer M, Huber R, Kurz M, Walch T, Fleischhacker WW. Selection bias in clinical trials with antipsychotics. J Clin Psychopharmacol. 2000;20:699–702.
Leucht C, Heres S, Kane JM, Kissling W, Davis JM, Leucht S. Oral versus depot antipsychotic drugs for schizophrenia—a critical systematic review and meta-analysis of randomised long-term trials. Schizophr Res. 2011;127:83–92.
Hegarty JD, Baldessarini RJ, Tohen M, Waternaux C, Oepen G. One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am J Psychiatry. 1994;151:1409–16.
Jobe TH, Harrow M. Long-term outcome of patients with schizophrenia: a review. Can J Psychiatry. 2005;50:892–900.
Kishimoto T, Hagi K, Nitta M, Leucht S, Olfson M, Kane JM. et al. Effectiveness of long-acting injectable vs. oral antipsychotics in patients with Schizophrenia: a meta-analysis of prospective and retrospective cohort studies. Schizophr Bull. 2018;44:603–19.
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379:2063–71.
Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N. et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394:939–51.
Agid O, Siu CO, Potkin SG, Kapur S, Watsky E, Vanderburg D. et al. Meta-regression analysis of placebo response in antipsychotic trials, 1970–2010. Am J Psychiatry. 2013;170:1335–44.
Leucht S, Leucht C, Huhn M, Chaimani A, Mavridis D, Helfer B. et al. Sixty years of placebo-controlled antipsychotic drug trials in acute Schizophrenia: systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry. 2017;174:927–42.
Kahn RS, Fleischhacker WW, Boter H, Davidson M, Vergouwe Y, Keet IP. et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet. 2008;371:1085–97.
Takács P, Czobor P, Fehér L, Gimesi-Országh J, Fadgyas-Freyler P, Bacskai M. et al. Comparative effectiveness of second generation long-acting injectable antipsychotics based on nationwide database research in Hungary. PLoS ONE. 2019;14:e0218071.
Soares-Weiser K, Béchard-Evans L, Lawson AH, Davis J, Ascher-Svanum H. Time to all-cause treatment discontinuation of olanzapine compared to other antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2013;23:118–25.
Granger B, Albu S. The haloperidol story. Ann Clin Psychiatry. 2005;17:137–40.
Wikipedia. Haloperidol, Publicly available document: https://en.wikipedia.org/wiki/HaloperidolHist. Last accessed 28 Apr 2021.
Drugs @ FDA: FDA-Approved Drugs, Publicly available document: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm. Last accessed 28 Apr 2021.
Crilly J. The history of clozapine and its emergence in the US market: a review and analysis. Hist Psychiatry. 2007;18:39–60.
Mortimer AM. Update on the management of symptoms in schizophrenia: focus on amisulpride. Neuropsychiatr Dis Treat. 2009;5:267–77.
Stroup TS, McEvoy JP, Swartz MS, Byerly MJ, Glick ID, Canive JM. et al. The National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) project: schizophrenia trial design and protocol development. Schizophr Bull. 2003;29:15–31.
Ascher-Svanum H, Zhu B, Faries D, Landbloom R, Swartz M, Swanson J. Time to discontinuation of atypical versus typical antipsychotics in the naturalistic treatment of schizophrenia. BMC Psychiatry. 2006;6:8.
Bitter I, Katona L, Zámbori J, Takács P, Fehér L, Diels J. et al. Comparative effectiveness of depot and oral second generation antipsychotic drugs in schizophrenia: a nationwide study in Hungary. Eur Neuropsychopharmacol. 2013;23:1383–90.
Cooper D, Moisan J, Gaudet M, Abdous B, Grégoire JP. Ambulatory use of olanzapine and risperidone: a population-based study on persistence and the use of concomitant therapy in the treatment of schizophrenia. Can J Psychiatry. 2005;50:901–8.
Dossenbach M, Pecenak J, Szulc A, Irimia V, Anders M, Logozar-Perkovic D. et al. Long-term antipsychotic monotherapy for schizophrenia: disease burden and comparative outcomes for patients treated with olanzapine, quetiapine, risperidone, or haloperidol monotherapy in a pan-continental observational study. J Clin Psychiatry. 2008;69:1901–15.
Haro JM, Suarez D, Novick D, Brown J, Usall J, Naber D. et al. Three-year antipsychotic effectiveness in the outpatient care of schizophrenia: observational versus randomized studies results. Eur Neuropsychopharmacol. 2007;17:235–44.
Katona L, Czobor P, Bitter I. Real-world effectiveness of antipsychotic monotherapy vs. polypharmacy in schizophrenia: to switch or to combine? A nationwide study in Hungary. Schizophr Res. 2014;152:246–54.
Kilzieh N, Todd-Stenberg JA, Kennedy A, Wood AE, Tapp AM. Time to discontinuation and self-discontinuation of olanzapine and risperidone in patients with schizophrenia in a naturalistic outpatient setting. J Clin Psychopharmacol. 2008;28:74–7.
Tiihonen J, Wahlbeck K, Lönnqvist J, Klaukka T, Ioannidis JP, Volavka J. et al. Effectiveness of antipsychotic treatments in a nationwide cohort of patients in community care after first hospitalisation due to schizophrenia and schizoaffective disorder: observational follow-up study. BMJ. 2006;333:224
Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011;168:603–9.
Tiihonen J, Mittendorfer-Rutz E, Majak M, Mehtälä J, Hoti F, Jedenius E. et al. Real-world effectiveness of antipsychotic treatments in a Nationwide Cohort of 29,823 patients with Schizophrenia. JAMA Psychiatry. 2017;74:686–93.
Beasley CM Jr, Stauffer VL, Liu-Seifert H, Taylor CC, Dunayevich E, Davis JM. All-cause treatment discontinuation in schizophrenia during treatment with olanzapine relative to other antipsychotics: an integrated analysis. J Clin Psychopharmacol. 2007;27:252–8.
Kishimoto T, Hagi K, Nitta M, Kane JM, Correll CU. Long-term effectiveness of oral second-generation antipsychotics in patients with schizophrenia and related disorders: a systematic review and meta-analysis of direct head-to-head comparisons. World Psychiatry. 2019;18:208–24.
Krause M, Huhn M, Schneider-Thoma J, Rothe P, Smith RC, Leucht S. Antipsychotic drugs for elderly patients with schizophrenia: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2018;28:1360–70.
Ostuzzi G, Bighelli I, So R, Furukawa TA, Barbui C. Does formulation matter? A systematic review and meta-analysis of oral versus long-acting antipsychotic studies. Schizophr Res. 2017;183:10–21.
Samara MT, Dold M, Gianatsi M, Nikolakopoulou A, Helfer B, Salanti G. et al. Efficacy, acceptability, and tolerability of antipsychotics in treatment-resistant Schizophrenia: a network meta-analysis. JAMA Psychiatry. 2016;73:199–210.
Sampson S, Hosalli P, Furtado VA, Davis JM. Risperidone (depot) for schizophrenia. Cochrane Database Syst Rev. 2016;4:CD004161.
Kishimoto T, et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophr Bull. 2014;40:192–213.
Bitter I. et al. Antipsychotic prescription patterns in outpatient settings: 24-month results from the Intercontinental Schizophrenia Outpatient Health Outcomes (IC-SOHO) study. Eur Neuropsychopharmacol. 2008;18:170–180.
Acknowledgements
This study was supported by the Hungarian Brain Research Program (2017-1.2.1-NKP-2017-0002).
Author information
Authors and Affiliations
Contributions
LK, PC, and IB developed the concept of the study. LK and PC designed the data collection and analysis. For the selection for both RWS and meta-analytic summaries, LK identified the publications for inclusion; LK and PC reviewed the results; in case of any discrepancy they had a discussion to achieve resolution. LK and PC conducted the analysis. LK, PC, and IB contributed significantly to the data interpretation and the discussion of the results. LK, PC, and IB contributed to the manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
IB has been an advisory board member/consultant/lecturer in the last 5 years for ACADIA, Angelini, Gedeon Richter, Hikma Pharmaceuticals, Janssen/Janssen Cilag, Lundbeck, Medichem Pharmaceuticals, Inc. by Unilab, Inc. LK and PC declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Katona, L., Bitter, I. & Czobor, P. A meta-analysis of effectiveness of real-world studies of antipsychotics in schizophrenia: Are the results consistent with the findings of randomized controlled trials?. Transl Psychiatry 11, 510 (2021). https://doi.org/10.1038/s41398-021-01636-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-021-01636-9