Abstract
Background/Objectives
The contribution of iron status at birth to iron status in infancy is not known. We used a physiologic framework to evaluate how iron status at birth related to iron status at 9 months, taking iron needs and sources into account.
Subjects/Methods
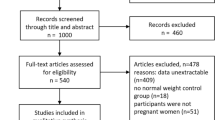
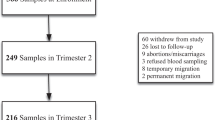
In a longitudinal birth cohort in China, iron status measures in cord blood and venous blood in infancy (9 months) and clinical data were prospectively collected in 545 healthy term maternal–infant dyads. We used structural equation modeling (SEM) to create a 9-month iron composite and to assess direct and indirect contributions of multiple influences on 9-month iron status. Logistic regression was used to calculate odds ratios for iron deficiency (ID), iron deficiency anemia (IDA), and anemia.
Results
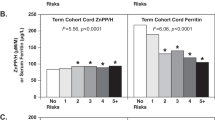
Approximately 15% (78/523) of infants were born with cord SF <75 µg/l, suggesting fetal-neonatal ID. At 9 months, 34.8% (186/535) and 19.6% (105/535) of infants had ID and IDA, respectively. The following factors were independently associated with poorer 9-month iron status: higher cord zinc protoporphyrin/heme (ZPP/H) (adjusted estimate −0.18, P < 0.001) and serum transferrin receptor (sTfR) (−0.11, P = 0.004), lower cord hemoglobin (Hb) (0.13, P = 0.004), lower birth weight (0.15, P < 0.001), male sex (0.10, P = 0.013), older age at testing (−0.26, P < 0.001), higher 9-month weight (−0.12, P = 0.006) and breastfeeding (0.38, P < 0.001). Breastfeeding at 9 months showed the strongest association, adjusting for all other factors. Compared to formula-fed infants, the odds of IDA were 19.1 (95% CI: 6.92, 52.49, P < 0.001) and 3.6 (95% CI: 1.04, 12.50, P = 0.043) times higher in breastfed and mixed-fed infants, respectively.
Conclusions
Indicators of iron status at birth, postnatal iron needs, and iron sources independently related to iron status at 9 months. Sex was an additional factor. Public health policies to identify and protect infants at increased risk of ID should be prioritized.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Georgieff MK. Long-term brain and behavioral consequences of early iron deficiency. Nutr Rev. 2011;69:S43–8.
World Health Organization. Guideline: Daily iron supplementation in infants and children. World Health Organization. 2016. Geneva.
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013;1:e16–25.
Huo J, Sun J, Fang Z, Chang S, Zhao L, Fu P, et al. Effect of home-based complementary food fortification on prevalence of anemia among infants and young children aged 6 to 23 months in poor rural regions of China. Food Nutr Bull. 2015;36:405–14.
Gupta PM, Hamner HC, Suchdev PS, Flores-Ayala R, Mei Z. Iron status of toddlers, nonpregnant females, and pregnant females in the United States. Am J Clin Nutr. 2017;106(Suppl 6):1640S–6S. https://doi.org/10.3945/ajcn.117.155978.
Brotanek JM, Gosz J, Weitzman M, Flores G. Secular trends in the prevalence of iron deficiency among US toddlers, 1976-2002. Arch Pediatr Adolesc Med. 2008;162:374–81.
Baker RD, Greer FR. Committee on nutrition. diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics. 2010;126:1040–50.
McDonagh MS, Blazina I, Dana T, Cantor A, Bougatsos C. Screening and routine supplementation for iron deficiency anemia: a systematic review. Pediatrics. 2015;135:723–33.
Lozoff B, Walter T, Kaciroti N. Iron deficiency in infancy: applying a physiologic framework for prediction. Am J Clin Nutr. 2006;84:1412–21.
Georgieff MK, Wewerka SW, Nelson CA, deRegnier RA. Iron status at 9 months of infants with low iron stores at birth. J Pediatr. 2002;141:405–9.
Strauss MB. Anemia of infancy from maternal iron deficiency in pregnancy. J Clin Invest. 1933;12:345–53.
de Pee S, Bloem MW, Sari M, Kiess L, Yip R. The high prevalence of low hemoglobin concentration among Indonesian infants aged 3-5 months is related to maternal anemia. J Nutr. 2002;132:2215–21.
Colomer J, Colomer C, Gutierrez D, Jubert A, Nolasco A, Donat J, et al. Anaemia during pregnancy as a risk factor for infant iron deficiency: report from the Valencia Infant Anaemia Cohort (VIAC) study. Paediatr Perinat Epidemiol. 1990;4:196–204.
Miller MF, Stoltzfus RJ, Mbuya NV, Malaba LC, Iliff PJ, Humphrey JH, et al. Total body iron in HIV-positive and HIV-negative Zimbabwean newborns strongly predicts anemia throughout infancy and is predicted by maternal hemoglobin concentration. J Nutr. 2003;133:3461–8.
Hay G, Refsum H, Whitelaw A, Melbye EL, Haug E, Borch-Iohnsen B. Predictors of serum ferritin and serum soluble transferrin receptor in newborns and their associations with iron status during the first 2 y of life. Am J Clin Nutr. 2007;86:64–73.
Clark KM, Li M, Shao J, Liang F, Zhang Y, Chai J, et al. Breastfeeding, mixed or formula feeding at 9 months and the prevalence of iron deficiency and iron deficiency anemia in two cohorts of infants in China. J Pediatr. 2017;181:56–61.
Chen CM, Mu SC, Shih CK, Chen YL, Tsai LY, Kuo YT, et al. Iron status of infants in the first year of life in Northern Taiwan. Nutrient. 2020;12:139–51. https://doi.org/10.3390/nu12010139
Armony-Sivan R, Zhu B, Clark KM, Ji C, Kaciroti N, Shao J et al. Iron deficiency(ID) at both birth and 9 months predicts right frontal EEG asymmetry in infancy. Dev Psychobiol. 2016;58:462–70.
Lorenz L, Peter A, Poets CF, Franz AR. A review of cord blood concentrations of iron status parameters to define reference ranges for preterm infants. Neonatology. 2013;104:194–202.
Shao J, Lou J, Rao R, Georgieff MK, Kaciroti N, Felt BT, et al. Maternal serum ferritin concentration is positively associated with newborn iron stores in women with low ferritin status in late pregnancy. J Nutr. 2012;142:2004–9.
Tamura T, Goldenberg RL, Hou J, Johnston KE, Cliver SP, Ramey SL, et al. Cord serum ferritin concentrations and mental and psychomotor development of children at five years of age. J Pediatr. 2002;140:165–70.
Amin SB, Orlando M, Eddins A, MacDonald M, Monczynski C, Wang H. In utero iron status and auditory neural maturation in premature infants as evaluated by auditory brainstem response. J Pediatr. 2010;156:377–81.
Amin SB, Orlando M, Wang H. Latent iron deficiency in utero is associated with abnormal auditory neural myelination in >= 35 weeks gestational age infants. J Pediatr. 2013;163:1267–71.
Armony-Sivan R, Eidelman AI, Lanir A, Sredni D, Yehuda S. Iron status and neurobehavioral development of premature infants. J Perinatol. 2004;24:757–62.
World Health Organization. Worldwide Prevalence of Anaemia 1993-2005: WHO Global Database on Anaemia. 2008; Geneva, Switzerland: WHO Press.
Centers for Disease Control. Healthy People - 2000 National Health Promotion and Disease Prevention Objectives Final Review. 2001. Hyattsville, MD, Department of Health and Human Services.
Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. MMWR. 1998;47:1–29.
Saarinen UM, Siimes MA. Serum ferritin in assessment of iron nutrition in healthy infants. Acta Pediatr. 1978;67:745–51.
Soldin OP, Miller M, Soldin SJ. Pediatric reference ranges for zinc protoporphyrin. Clin Biochem. 2003;36:21–25.
Cook JD, Flowers CH, Skikne BS. The quantitative assessment of body iron. Blood. 2003;101:3359–64.
Flowers CH, Skikne BS, Covell AM, Cook JD. The clinical measurement of serum transferrin receptor. J Lab Clin Med. 1989;114:368–77.
Pfeiffer CM, Cook JD, Mei Z, Cogswell ME, Looker AC, Lacher DA. Evaluation of an automated soluble transferrin receptor (sTfR) assay on the Roche Hitachi analyzer and its comparison to two ELISA assays. Clin Chim Acta. 2007;382:112–6.
World Health Organization. Child growth standards. WHO Anthro (version 3.2.2, January 2011) and macros [Internet]. Available from: http://www.who.int/childgrowth/software/en/. 2011. Geneva, World Health Organization.
Domellof M, Lonnerdal B, Dewey KG, Cohen RJ, Rivera LL, Hernell O. Sex differences in iron status during infancy. Pediatrics. 2002;110:545–52.
Labbé RF, Vreman HJ, Stevenson DK. Zinc protoporphyrin: a metabolite with a mission. Clin Chem. 1999;45:2060–72.
McLimore HM, Phillips AK, Blohowiak SE, Pham DQ, Coe CL, Fischer B, et al. Impact of multiple risk factors on newborn iron status. J Pediatr Hematol Oncol. 2013;35:473–7.
Rettmer RL, Carlson TH, Maurice L, Origenes ML, Jack RM, Labbe´ RF. Zinc protoporphyrin/Heme Ratio diagnosis preanemic iron deficiency. Pediatrics.1999;104:e37 https://doi.org/10.1542/peds.104.3.e37.
Yu KH. Effectiveness of zinc protoporphyrin/heme ratio for screening iron deficiency in preschool-aged children. Nutr. Res Pract. 2011;5:40–45. https://doi.org/10.4162/nrp.2011.5.1.40
Hennig G, Homann C, Teksan I, Hasbargen U, Hasmuller S, Holdt LM, et al. Non-invasive detection of iron deficiency by fluorescence measurement of erythrocyte zinc protoporphyrin in the lip. Nat Commun. 2016;17:10776 https://doi.org/10.1038/ncomms10776.
Acknowledgements
We acknowledge Drs. Sean Lynch and Bo Lonnerdalfor their service on the Independent Data Monitoring Committee, which had oversight of the small randomized clinical trial component. We also thank Dr. Yaping Shi and her colleagues for their assistance with participant enrollment and cord blood collection, Liqin Chen for the iron status assays, and Julie Sturza for data analysis.
Funding
This work was supported by grants from the National Institutes of Health (HD039386, B. Lozoff, Principal Investigator) and the China National Sciences Foundation (81273085, J. Shao, Principal Investigator). Iron supplements and placebo were donated by Lee’s Pharmaceutical Holdings Limited (Hong Kong). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Author information
Authors and Affiliations
Contributions
JS was a co-investigator in the Brain and Behavior in Early Iron Deficiency study and principal investigator (PI) in the grant from NSFC; BL was the overall PI of the study; BL and JS were responsible for designing and conducting the research, writing and interpreting results; NK conducted methodology and formal analysis; BR conducted data extraction and analysis; BZ was responsible for investigation and data collection. KMC contributed to writing, review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict ofinterest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shao, J., Richards, B., Kaciroti, N. et al. Contribution of iron status at birth to infant iron status at 9 months: data from a prospective maternal-infant birth cohort in China. Eur J Clin Nutr 75, 364–372 (2021). https://doi.org/10.1038/s41430-020-00705-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00705-4