Abstract
Background
Stroke represents a major source of mortality and morbidity worldwide. Guidelines for stroke management and secondary prevention focus on reducing stroke-related risk factors such as smoking cessation, exercise and diet. Several clinical practice guidelines specifically recommend a Mediterranean diet (MD) for individuals with stroke. However, these recommendations rely primarily on observational research. The aim of this review is to critically appraise the current experimental evidence assessing the use of a Mediterranean diet on health outcomes in post-stroke adults.
Methods
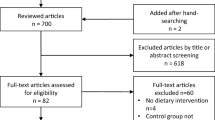
A systematic literature review was conducted of original research which assessed the role of a Mediterranean diet on health outcomes in post-stroke adults. The following databases were searched: PROQUEST, SCOPUS (Elsevier), MEDLINE (EBSCO), EMBase and Cochrane Library up to the 25th of August 2021.
Results
A total of 6 studies from a total of 5838 identified studies met the full inclusion criteria and were included in this review. Several different health outcomes were assessed, including blood pathology tests, physical examinations, secondary vascular events and mortality. The Mediterranean diet appears to be beneficial for systolic and diastolic blood pressure, LDL cholesterol, BMI and waist circumference.
Conclusion
This review suggests a Mediterranean diet may be helpful for several health outcomes in post-stroke adults. However, more research is needed to confirm these findings. To ensure robust methodology and replication of results, specific details of the included and excluded foods, quantities and serving sizes should be reported in future research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data analysed in this review can be obtained from the corresponding author by reasonable request.
References
Campbell BC, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nat Rev Dis Prim. 2019;5:1–22.
Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology. 2020;54:171–9.
Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120:439–48.
Crichton SL, Bray BD, McKevitt C, Rudd AG, Wolfe CD. Patient outcomes up to 15 years after stroke: survival, disability, quality of life, cognition and mental health. J Neurol Neurosurg Psychiatry. 2016;87:1091–8.
Clissold BB, Sundararajan V, Cameron P, McNeil J. Stroke incidence in Victoria, Australia—emerging improvements. Front Neurol. 2017;8:180.
Cerniauskaite M, Quintas R, Koutsogeorgou E, Meucci P, Sattin D, Leonardi M, et al. Quality-of-life and disability in patients with stroke. Am J Phys Med Rehabil. 2012;91:S39–S47.
Almborg AH, Ulander K, Thulin A, Berg S. Discharged after stroke–important factors for health‐related quality of life. J Clin Nurs. 2010;19:2196–206.
Gupta A, Deepika S, Taly A, Srivastava A, Surender V, Thyloth M. Quality of life and psychological problems in patients undergoing neurological rehabilitation. Ann Indian Acad Neurol. 2008;11:225.
Muus I, Petzold M, Ringsberg KC. Health‐related quality of life among Danish patients 3 and 12 months after TIA or mild stroke. Scand J Caring Sci. 2010;24:211–8.
Fisher RJ, Gaynor C, Kerr M, Langhorne P, Anderson C, Bautz-Holter E, et al. A consensus on stroke: early supported discharge. Stroke. 2011;42:1392–7.
Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014;95:986–95.e1.
Esenwa C, Gutierrez J. Secondary stroke prevention: challenges and solutions. Vasc Health Risk Manag. 2015;11:437.
Saulle R, Lia L, De Giusti M, La, Torre G. A systematic overview of the scientific literature on the association between Mediterranean Diet and the Stroke prevention. Clin Ter. 2019;170:e396–e408.
Serra-Majem L, Trichopoulou A, de la Cruz JN, Cervera P, Álvarez AG, La Vecchia C, et al. Does the definition of the Mediterranean diet need to be updated? Public Health Nutr. 2004;7:927–9.
Nestle M. Mediterranean diets: science and policy implications. The American journal of clinical nutrition. 1995;61(6 Suppl):ixS-xS, 1313S–1427S.
Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-hill D, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021:STR. 0000000000000375.
Stroke Foundation. Clinical guidelines for stroke management. Australia; 2021. https://informme.org.au/Guidelines/Clinical-Guidelines-for-Stroke-Management, Accessed 30/08/2021.
Gladstone DJ, Lindsay MP, Douketis J, Smith EE, Dowlatshahi D, Wein T, et al. Canadian stroke best practice recommendations: secondary prevention of stroke update 2020. Can J Neurol Sci. 2021:1–69.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:1–11.
Heron N, Kee F, Mant J, Cupples ME, Donnelly M. Rehabilitation of patients after transient ischaemic attack or minor stroke: pilot feasibility randomised trial of a home-based prevention programme. Br J Gen Pract. 2019;69:e706–e14.
Towfighi A, Cheng EM, Hill VA, Barry F, Lee M, Valle NP, et al. Results of a pilot trial of a lifestyle intervention for stroke survivors: healthy eating and lifestyle after stroke. J Stroke Cerebrovasc Dis. 2020;29:105323.
Ahmadi M, Laumeier I, Ihl T, Steinicke M, Ferse C, Endres M, et al. A support programme for secondary prevention in patients with transient ischaemic attack and minor stroke (INSPiRE-TMS): an open-label, randomised controlled trial. Lancet Neurol. 2020;19:49–60.
Magnusson G, Ballegaard S, Karpatschof B, Nyboe J. Long-term effects of integrated rehabilitation in patients with stroke: a nonrandomized comparative feasibility study. J Altern Complement Med. 2010;16:369–74.
Prior PL, Hachinski V, Unsworth K, Chan R, Mytka S, O’Callaghan C, et al. Comprehensive cardiac rehabilitation for secondary prevention after transient ischemic attack or mild stroke: I: feasibility and risk factors. Stroke. 2011;42:3207–13.
Leistner S, Benik S, Laumeier I, Ziegler A, Nieweler G, Nolte CH, et al. Secondary prevention after minor stroke and TIA—usual care and development of a support program. PloS One. 2012;7:e49985.
Guthrie NL, Berman MA, Edwards KL, Appelbaum KJ, Dey S, Carpenter J, et al. Achieving rapid blood pressure control with digital therapeutics: retrospective cohort and machine learning study. JMIR Cardio. 2019;3:e13030.
Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–6.
Verweij LM, Terwee CB, Proper KI, Hulshof CT, van Mechelen W. Measurement error of waist circumference: gaps in knowledge. Public Health Nutr. 2013;16:281–8.
Jennings A, Berendsen AM, De Groot LC, Feskens EJ, Brzozowska A, Sicinska E, et al. Mediterranean-style diet improves systolic blood pressure and arterial stiffness in older adults: results of a 1-year European multi-center trial. Hypertension. 2019;73:578–86.
Doménech M, Roman P, Lapetra J, Garcia de la Corte FJ, Sala-Vila A, de la Torre R, et al. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension. 2014;64:69–76.
Storniolo CE, Casillas R, Bulló M, Castañer O, Ros E, Sáez G, et al. A Mediterranean diet supplemented with extra virgin olive oil or nuts improves endothelial markers involved in blood pressure control in hypertensive women. Eur J Nutr. 2017;56:89–97.
Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum hypertension. 2003;17:471–80.
Kokkinos P, Panagiotakos DB, Polychronopoulos E. Dietary influences on blood pressure: the effect of the Mediterranean diet on the prevalence of hypertension. J Clin Hypertens. 2005;7:165–72.
Rasmussen B.M, Vessby B, Uusitupa M, Berglund L, Pedersen E, Riccardi G. Effects of dietary saturated, monounsaturated, and n− 3 fatty acids on blood pressure in healthy subjects. Am J Clin Nutr. 2006;83:221–6.
Laloux P, Lemonnier F, Jamart J. Risk factors and treatment of stroke at the time of recurrence. Acta Neurol Belg. 2010;110:299.
Agnoli C, Sieri S, Ricceri F, Giraudo MT, Masala G, Assedi M, et al. Adherence to a Mediterranean diet and long-term changes in weight and waist circumference in the EPIC-Italy cohort. Nutr Diabetes. 2018;8:1–10.
Hu G, Barengo NC, Tuomilehto J, Lakka TA, Nissinen A, Jousilahti P. Relationship of physical activity and body mass index to the risk of hypertension: a prospective study in Finland. Hypertension. 2004;43:25–30.
Hu G, Lindström J, Valle TT, Eriksson JG, Jousilahti P, Silventoinen K, et al. Physical activity, body mass index, and risk of type 2 diabetes in patients with normal or impaired glucose regulation. Arch Intern Med. 2004;164:892–6.
Wietlisbach V, Marques-Vidal P, Kuulasmaa K, Karvanen J, Paccaud F. The relation of body mass index and abdominal adiposity with dyslipidemia in 27 general populations of the WHO MONICA Project. Nutr, Metab Cardiovasc Dis. 2013;23:432–42.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492.
Serra-Majem L, Roman B, Estruch R. Scientific evidence of interventions using the Mediterranean diet: a systematic review. Nutr Rev. 2006;64:S27–S47.
Davis C, Bryan J, Hodgson J, Murphy K. Definition of the Mediterranean diet; a literature review. Nutrients. 2015;7:9139–53.
García-Conesa M-T, Philippou E, Pafilas C, Massaro M, Quarta S, Andrade V, et al. Exploring the validity of the 14-item mediterranean diet adherence screener (Medas): a cross-national study in seven european countries around the mediterranean region. Nutrients. 2020;12:2960.
Author information
Authors and Affiliations
Contributions
All authors contributed to the design of the research question, development of the search terms, and contributed to the review protocol. JB conducted the literature search, analysed the data, and drafted the manuscript. JB and DS conducted the critical appraisal of all included articles. All authors contributed to the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bayes, J., Peng, W., Adams, J. et al. The effect of the Mediterranean diet on health outcomes in post-stroke adults: a systematic literature review of intervention trials. Eur J Clin Nutr 77, 551–560 (2023). https://doi.org/10.1038/s41430-022-01212-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01212-4