Abstract
An expansion in the availability of clinical drug trials for genetic neurodevelopmental conditions is underway. Delineating patient priorities is key to the success of drug development and clinical trial design. There is a lack of evidence about parent decision-making in the context of clinical drug trials for genetic neurodevelopmental conditions. We assessed parents’ priorities when making a decision whether to enroll their child with fragile X syndrome (FXS) in a clinical drug trial. An online survey included a best–worst scaling method for parents to prioritize motivating and discouraging factors for child enrollment. Parents were recruited through the National Fragile X Foundation and FRAXA. Sequential best–worst with conditional logit analysis was used to determine how parents prioritize motivating and discouraging factors about trial enrollment decisions. Respondents (N = 354) were largely biological mothers (83%) of an individual with FXS who ranged in age from under 5 to over 21 years. The highest motivating factor was a trial to test a drug targeting the underlying FXS mechanism (coeff = 3.28, p < 0.001), followed by the potential of the drug to help many people (coeff = 3.03, p < 0.001). Respondents rated requirement of blood draws (coeff = −3.09, p < 0.001), loss of access to the drug post trial (coeff = −3.01, p < 0.001), and drug side effects (coeff = −2.96, p < 0.001) as most discouraging. The priorities defined by parents can be incorporated into evidence-based trial design and execution to enhance the enrollment process.
Similar content being viewed by others
Introduction
Genomics has rapidly advanced understanding of the causes of neurodevelopmental conditions [1]. Promising evidence has emerged from studies of conditions with variants in a single gene such as fragile X syndrome (FXS), informing generation of novel pharmaceutical treatments. Such treatments target the underlying mechanism of the condition, for global symptom reduction, as opposed to current available treatments that target discrete symptoms (e.g., attention, learning, communication) [1]. Translation of treatment advances into the clinic requires drug trials to produce safety and efficacy data.
Little is known about patient and parent priorities in drug trials for genetic neurodevelopmental conditions such as FXS. There is evidence showing that less than one-third of parents rate currently available treatments as very effective [2]. The FDA endorses the advancement of patient-focused drug development [3]. This can be achieved through engagement with members of affected families to delineate their priorities for developing new treatments.
Significant progress in drug development for genetic neurodevelopmental conditions has occurred in FXS [4]. FXS is an X-linked inherited condition caused by a CGG repeat expansion in the FMR1 gene [5]. It is the most common form of inherited intellectual disability and over 50% of males and 20% of females with FXS meet the diagnostic criteria for autism [6]. Other common behavioral symptoms—seen most often in affected boys—include anxiety, aggression, attention deficits, and hyperactivity [7].
There have been 56 clinical drug trials for FXS [8]. The most commonly used outcome measure is the Aberrant Behavior Checklist. Language and learning outcomes have been included in a subset of studies as well [8]. There are 13 trials currently (or soon to start) recruiting and more anticipated. As such, parents are increasingly faced with complex trial enrollment decisions for their affected children.
Parents and caregivers of individuals with FXS are primarily responsible for decisions to enroll their child in a drug trial. Little is known about how these decisions are made. Prior research in parent decision-making for clinical trials has been conducted in the context of life-threatening, progressive, primarily physical conditions such as cancer [9, 10]. In the context of pediatric cancers, informed consent can be difficult to achieve as parents are often psychologically distressed, with limited alternative treatment options [11]. Such dire circumstances have been shown to leave many parents with high expectations for benefit from clinical trials and high tolerance level for adverse outcomes [11, 12].
There is limited evidence about parent decision-making in conditions that are not life-threatening or progressive such as FXS. Parents who consider enrolling their child in FXS research are likely managing symptoms with existing interventions [2, 13]. Thus, decisions to enroll in a trial for FXS may be made over a longer period of time as compared to trials in other disease contexts where rapid decisions are often needed to circumvent disease progression [14]. We sought to quantitatively determine how parents prioritize motivating and discouraging factors when making decisions to enroll a child with FXS into a clinical drug trial. We further sought to determine whether parent priorities differed based on clinical and demographic characteristics. Our evidence can contribute parent priorities in the drug development process and may be used to guide the design and execution of clinical trials for FXS to enhance enrollment [15, 16].
Results
In total, 475 parents accessed the link to the online questionnaire and began responding. We had 354 parents who completed the best–worst scaling task in its entirety. Parents were predominantly white, biological mothers, and educated beyond high school (Table 1). Most parents had only one child with FXS, though close to 30% had two or more affected children, and answered the best–worst scaling exercise in reference to their oldest affected child. Just over a quarter (28%) indicated their child has been in a clinical drug trial for FXS. Sixty-five percent indicated that their child was taking medication to manage symptoms of FXS. Just over half (57.9%) answered that a specialist cared for their child with FXS.
Prioritization of motivating and discouraging factors for clinical trial enrollment
Factor prioritization from the best–worst scaling is shown in Fig. 1. Factors with a positive value were selected as best more often than worst, and factors with a negative value were selected as worst more often than best. The most motivating factor was that the drug treats the underlying mechanism of FXS and addresses a wide range of FXS symptoms (Fig. 1). Other highly motivating factors were that the drug is likely to help many people with FXS, and that the trial participant is likely to benefit from participating in the trial. Three factors were rated as close to equally discouraging, including the requirement for blood draws as part of the trial, having no access to the study drug after the trial, and drug side effects—that the drug causes nausea leading to reduced food intake.
Stratified prioritization
We examined whether rankings would differ based on a variety of clinical and demographic characteristics (Table 2). There were no differences in the most motivating factors based on child’s age, gender, disease severity, number of children with FXS, or prior clinical trial experiences.
There were differences in rankings of discouraging factors based on clinical and demographic characteristics. The most discouraging factor among parents whose child with FXS was male was loss of access to the drug after the trial finished, whereas the requirement for blood draws was most discouraging amongst parents of affected females. The most discouraging factor for parents of children who are mildly or severely affected was loss of access to the study drug after the trial; however, the trial requiring blood draws was the most discouraging for those with children who are moderately affected. Drug side effects were the most discouraging for those with previous trial experience, whereas the most discouraging factor for those who had not previously enrolled their child in a trial was the trial requiring travel and overnight stays. Parents’ priorities of discouraging factors did not differ based on their child’s age.
Discussion
We found parents to be most motivated by a trial testing a drug treating the underlying mechanism of FXS. The possibility of the drug helping many with FXS was the second most motivating factor. The requirement of blood draws, loss of access to the drug after the trial, and side effects of the drug—causing nausea leading to reduced food intake—were most often selected as discouraging. These results align with the qualitative study from which the motivating and discouraging factors arose [17]. Our study extends this prior work, providing a quantitative assessment of these factors, revealing both order and relative strength of these priorities.
We note findings that may be specific to parents of children with genetic neurodevelopmental conditions, distinct from prior research in other contexts. For example, studies of children with physical, life-limiting conditions often cite personal benefit for their child as a principal motivating factor to enroll in a clinical drug trial [11, 18]. Parents in our study prioritized the possibility of a novel drug treatment targeting a range of symptoms, and the drug helping many people as the principal motivating factors, and more highly than individual benefit.
Parents’ motivations, of the possibility of a drug to treat the underlying mechanism of FXS, align with recent progress in novel drug treatments [4]. The progress in drug development is largely due to the well-characterized genetic cause of FXS. Future studies could compare motivating and discouraging factors for other neurodevelopmental conditions such as idiopathic autism to determine whether our findings are specific to neurodevelopmental conditions caused by a single gene or if they hold for other neurodevelopmental conditions. Furthermore, parents in our study reported to be motivated by altruistic factors (the drug helping many people) which may be indicative of an active advocacy community that generally supports research advances [19]. This is particularly salient in the rare disease community, where advocacy organizations representing affected individuals and their families are often partners in the conduct of clinical research [20].
While the most motivating factors did not change based on specific characteristics of the child of the parent completing the survey (i.e., gender, condition severity, and prior clinical trial experience), we did note some differences in parents’ rankings of discouraging factors. Of note, parents whose child had previously enrolled in a trial reported to be more discouraged by the risk of side effects compared to parents without prior trial experience. This could suggest some level of naivety about the impact of side effects for those participating in drug trials for the first time.
The variation in discouraging factors based on child gender and condition severity that we report could mean that families have unique needs and requirements to overcome different barriers and participate in research, based on their individual circumstances. Those designing and approving clinical trial research should be knowledgeable about such individual variations and may consider drawing on a person-orientated research ethics framework, which has recently been suggested to address the needs of participants with autism [21].
Our findings can contribute priorities defined by parents in the drug development process. Specifically, our data provide evidence that parents support development of treatments that target the underlying mechanism. This finding aligns with recent advances in the field in developing treatments for FXS, which are leading the way for dug development in genetic neurodevelopmental conditions. Given that one of most discouraging factors for parents in our sample was loss of drug access post trial, those designing trials may consider how access could be maintained after the trial where that may be appropriate. Alternatively, if access cannot be maintained, it is important to ensure this information is clearly communicated to families considering trial enrollment, to avoid disappointment at the close of the trial. Parents in our study were discouraged by blood draw requirements. Strategies that offer an alternative for collecting biological samples such as collection of saliva or buccal cells could overcome the barrier of blood draw requirements. Novel distraction methods such as virtual reality may be effective at reducing pain scores, fear, and anxiety in children undergoing blood draws [22]. Future research could investigate the suitability of such methods for children with neurodevelopmental conditions including FXS.
Further, the evidence may be used to inform conversations between parents of eligible children and investigators or clinicians recruiting families to these drug trials, enhancing informed choice and the enrollment process. For example, knowledge that many families will be motivated to enroll in a trial testing a drug treating the underlying mechanism of FXS suggests that enrollment discussions about clinical drug trials should explicitly include whether the drug targets the effects of the FMR1 expansion (i.e., the specific gene variation).
Parents of children with neurodevelopmental conditions face many difficult decisions throughout the child’s life, including decisions about treatment and clinical trial enrollment. Parents may find the decision-making process challenging and isolating, warranting further support for these families [17, 23]. Such support could consist of decision tools and interventions which contextualize parents’ situations and allow parents to consider whether a trial aligns with their values and priorities [24]. Support interventions can improve decision quality which has wide reaching implications including improved psychological outcomes for parents. While decision interventions such as these exist to facilitate decision-making in the adult clinical trial context, interventions for surrogate decision makers such as parents are less commonly available [25].
Limitations
The recruitment strategy through advocacy groups was efficient and successful, leading to a large sample size for a rare disease population. However, the strategy may have introduced selection bias. Parents who are more inclined to participate in research may be overrepresented in our sample. These parents may also have more positive attitudes toward clinical drug trials. We lack information about nonresponders to test this hypothesis. Future research should investigate how to capture the views of parents who are not engaged in the research enterprise. The sample lacked diversity (e.g., most respondents were white, female, and educated beyond high school) and study materials were only available in English which limits the generalizability of findings to the population. Of a total of 475 individuals who accessed the survey link, 121 did not complete the best–worst scaling task. These individuals’ responses could not be included in our analysis. Parents with more than one child with FXS provided responses based on their oldest child. Responses may have differed if parents were instructed to consider their child closest in age to the child in the fixed vignette. Further, it is possible that parents were unable to completely discount prior experiences when responding to the fixed vignette. Despite these limitations, our study provides nuanced data on both motivating and discouraging factors in one decision-making scenario, and the fixed vignette minimizes response variation due to personal circumstances.
We intentionally chose to use best–worst scaling case 1 due to the cognitive ease for respondents, and the ability to generate robust and reliable data. Alternative stated-preference techniques such as discrete-choice experiments could have been used to identify trade-offs between motivating and discouraging factors. Lastly, while the focus on FXS may produce data that are less generalizable, this context was selected due to the advanced stage of drug development compared to other neurodevelopmental conditions. In fact, close to one-third of our sample had a child who had been in an FXS drug trial. Further research should test whether these findings are comparable among other neurodevelopmental condition clinical drug trial contexts.
Methods
Best–worst scaling
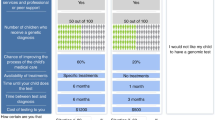
Object-case best–worst scaling is a quantitative stated-preferences method [26]. We used best–worst scaling to determine how parents prioritize motivating and discouraging factors for child enrollment in an FXS drug trial. We selected best–worst scaling case 1 over other stated-preference methods as this method is more understandable to the general population and aligned with our research objective to quantify parents’ priorities, rather than identify potential trade-offs. The application of best–worst scaling to healthcare research is relatively new, though increasingly being used and validated in a variety of contexts, in particular to study patient priorities in healthcare [27]. We used best–worst scaling case 1, also known as the object case. This best–worst scaling task presents respondents with a range of different combinations (sets) of related items (referred to as factors hereafter) and requires a forced choice response. When responding to the best–worst scaling task, factors are presented in a variety of sets and respondents are asked to select the most and least preferred (often described as the “best” and the “worst”) factor among each set. An example set is shown in Fig. 2. The best–worst scaling technique overcomes measurement problems that arise with standard rating scales such as poor discriminative ability and data skewing [28].
Instrument development
We used a previously described process to develop and refine the list of motivating and discouraging factors for the best–worst scaling task [29]. These factors included a range of trial and drug related benefits, risks, side effects, and burdens (Table 3). The first step involved identifying general concepts to be later refined as factors. Concepts had been previously explored with 34 parents of children with FXS in qualitative interviews (undertaken by author CD) [17]. Inductive content analysis was used with a specific intent to elucidate motivating and discouraging concepts. For this experiment, these concepts were then compared with those in the published literature, in particular, see Tromp et al. [30]. Studies from Tromp et al.’s review are primarily in the context of oncology, diabetes, and respiratory disease, with only two in psychopharmacology (one in ADHD and one in depression and anxiety). We found seven concepts common to both the qualitative findings and the systematic literature review. The interview data identified four additional concepts (Table 3).
The next stage in developing the experiment involved progression from general concepts to defined factors to prepare a mock best–worst scaling task. ET drafted statements to describe the general concepts and feedback was sought from the research team. Incorporation of the feedback generated 14 defined factors. Ten clinical or research graduate-level trainees at the National Human Genome Research Institute provided feedback about the face validity of 14 factors, focusing on potential misunderstanding, overlapping, or confusing concepts and literacy level, for example, provision of additional information about the frequency of blood draws and severity of nausea as a side effect.
Following elimination of redundant or overlapping factors the research team agreed on, the factors were reduced to a final 11 factors. Three eliminated factors were determined too complex and multidimensional to include in the best–worst scaling task and were included elsewhere in the questionnaire. These three factors related to trust in trial personnel or child’s doctor, attitudes about children in research, and attitudes about using medication for FXS.
A best–worst scaling task was generated based on the 11 selected factors and tested through in-depth “think aloud” exercises with five parents of children with FXS whereby the factors and overall task were tested for comprehension, terminology, and cognitive ease [31]. Minor edits were made based on parents’ feedback to finalize the survey. For example, reference to the factors was changed from “motivating and discouraging factors” to “best and worst thing” in the final task.
A fixed vignette contextualized the best–worst scaling task (Fig. 2). The use of a fixed vignette enabled respondent engagement to understand how we can improve trial experiences for families in the future. It also allowed responses to be drawn from a wider pool of participants as certain factors may not be relevant to all families’ actual experiences. For example, it was necessary for the factor “the trial allows children to stay on their regular medicines” to be evaluated in the context of a child who takes regular medicines. As not all children take regular medication for FXS, a fixed vignette was required. Respondents were asked to indicate the “best thing” and the “worst thing” within a list of motivating and discouraging factors. Development of the scenario and specific details about the factors was based on a content analysis of information about past and current clinical drug trials for FXS available through clinicaltrials.gov. For example, nausea is the most common side effect for drugs currently tested in FXS clinical trials. Travel to the study site and blood draw frequency were also based on protocols for past and current FXS trials. A balanced incomplete block design was used to develop the sets to ensure that each item was displayed an equal number of times [32]. Set order was randomized independently for each participant.
The questionnaire also included items assessing demographic characteristics (parent and patient) (see Table 1), disease severity, past clinical trial experiences—“has your child ever been in a clinical drug trial for FXS”?—and medication use—“does your child take medication for FXS symptoms”?
Data collection
Respondents were aged 18 years or older, parents (or primary caregiver) of one or more person(s) with FXS, and who understood English. Recruitment was targeted at parents living in the USA. The questionnaire was administered online using SurveyMonkey and was made available to collect responses from June 1 to September 20, 2018. A study advertising campaign included in-person recruitment at the National Fragile X Syndrome meeting (July 11–15), emails sent to members of the NFXF membership and FRAXA research foundation membership, and listings on the NFXF and FRAXA website and social media (Twitter and Facebook). These recruitment avenues were selected as they have previously been shown to be most effective for rare disease groups and are commonly used to advertise clinical drug trials to families. Responses were anonymous. Parents were asked to consider their oldest child with FXS when responding to questions about their child. The study was determined exempt by the Office of Human Subjects Research Protections, National Institutes of Health (#17-NHGRI-00124-1).
Data analysis
Our analysis plan tested: (1) overall prioritization of motivating and discouraging factors and (2) whether priorities would differ among parents based on clinical or demographic variables (child’s age and gender, number of children with FXS in family, severity of child’s FXS, and whether or not their own child has previously participated in a drug trial for FXS). Data were analyzed descriptively whereby averages (means) and frequencies of items were calculated. We used a sequential best–worst process to analyze the best–worst scaling data [33, 34]. This method assumes respondents chose a factor they determined as best from the list presented to them, followed by a selection of the worst factor. Factors selected as best were coded as one, those selected as worst coded as negative one and those not chosen were coded as zero. A single dichotomous dependent variable described the choice of best and worst for each set.
Conditional logit analysis was then used to model this choice set against other factors [35]. This analysis generates coefficients for each of the 11 factors which can be interpreted as priority scores. These priority scores can be ordered to produce a ranked list of the 11 barriers and facilitators. Finally, we explored differences in ranking based on demographic and clinical characteristics that have been empirically associated with clinical trial decisions [9,10,11, 36, 37]. This included child’s age and gender, severity of child’s FXS, and whether or not their own child has previously participated in a drug trial for FXS.
Conclusion
We report a prioritized list of motivating and discouraging factors for parents considering enrolling their child with FXS into a clinical drug trial. Patient engagement has been recognized by the FDA as essential in determining treatment developments and clinical trial priorities [3], and our data add to such efforts. Our findings further contribute to guiding discussions with families about clinical trial enrollment and development of decisional support tools.
References
Tărlungeanu DC, Novarino G. Genomics in neurodevelopmental disorders: an avenue to personalized medicine. Exp Mol Med. 2018;50:1–7.
Bailey DB, Raspa M, Bishop E, Olmsted M, Mallya UG, Berry-Kravis E. Medication utilization for targeted symptoms in children and adults with fragile X syndrome: US survey. J Dev Behav Pediatr. 2012;33:62–9.
U.S. Food and Drug Administration. Learn about FDA patient engagement. U.S. Food and Drug Administration; 2020. https://www.fda.gov/patients/learn-about-fda-patient-engagement.
Berry-Kravis EM, Lindemann L, Jønch AE, Apostol G, Bear MF, Carpenter RL, et al. Drug development for neurodevelopmental disorders: lessons learned from fragile X syndrome. Nat Rev Drug Discov. 2018;17:280–99.
Reiss AL, Hall SS. Fragile X syndrome: assessment and treatment implications. Child Adolesc Psychiatr Clin N Am. 2007;16:663–75.
Hall SS, Lightbody AA, Reiss AL. Compulsive, self-injurious, and autistic behavior in children and adolescents with fragile X syndrome. Am J Ment Retard. 2008;113:44–53.
Hagerman RJ, Berry-Kravis E, Kaufmann WE, Ono MY, Tartaglia N, Lachiewicz A, et al. Advances in the treatment of fragile X syndrome. Pediatrics. 2009;123:378–90.
U.S. National Library of Medicine. ClinicalTrials.gov. U.S. National Library of Medicine; 2020. https://clinicaltrials.gov/.
Fisher HR, McKevitt C, Boaz A. Why do parents enrol their children in research: a narrative synthesis. J Med Ethics. 2011;37:544–51.
Truong TH, Weeks JC, Cook EF, Joffe S. Altruism among participants in cancer clinical trials. Clin Trials. 2011;8:616–23.
de Vries MC, Houtlosser M, Wit JM, Engberts DP, Bresters D, Kaspers GJ, et al. Ethical issues at the interface of clinical care and research practice in pediatric oncology: a narrative review of parents’ and physicians’ experiences. BMC Med Ethics. 2011;12:1–11.
Mason SA, Allmark PJ, Group ES. Obtaining informed consent to neonatal randomised controlled trials: interviews with parents and clinicians in the Euricon study. Lancet. 2000;356:2045–51.
Becerra TA, Massolo ML, Yau VM, Owen-Smith AA, Lynch FL, Crawford PM, et al. A survey of parents with children on the autism spectrum: experience with services and treatments. Perm J. 2017;21:16–009.
Paquette E, Shukla A, Davidson J, Rychlik K, Davis M. Burden or opportunity? Parent experiences when approached for research in a pediatric intensive care unit. J Ethics Hum Res. 2019;41:2–12.
Johnson FR, Beusterien K, Özdemir S, Wilson L. Giving patients a meaningful voice in United States regulatory decision making: the role for health preference research. Patient. 2017;10:523–6.
Moultrie RR, Lewis MA, Paquin RS, Lucas A, Jarecki J, Peay HL. An evidence-based, community-engaged approach to develop an interactive deliberation tool for pediatric neuromuscular trials. J Genet Couns. 2018;27:416–25.
D’Amanda C, Peay H, Wheeler A, Turbitt E, Biesecker BB. Fragile X syndrome clinical trials: exploring parental decision making. J Intellect Disabil Res. 2019;63:926–35.
Peay H, Tibben A, Fisher T, Brenna E, Biesecker B. Expectations and experiences of investigators and parents involved in a clinical trial for Duchenne/Becker muscular dystrophy. Clin Trials. 2013;11:77–85.
Richstein J, Cohen J, Hardiman B. Fragile X research from a parental perspective. In: Fragile X syndrome. Elsevier; 2017. p. 457–70.
Landy DC, Brinich MA, Colten ME, Horn EJ, Terry SF, Sharp RR. How disease advocacy organizations participate in clinical research: a survey of genetic organizations. Genet Med. 2012;14:223–8.
Cascio MA, Weiss JA, Racine E. Person-oriented research ethics to address the needs of participants on the autism spectrum. Ethics Hum Res. 2020;42:2–16.
Özalp Gerçeker G, Ayar D, Özdemir EZ, Bektaş M. Effects of virtual reality on pain, fear and anxiety during blood draw in children aged 5–12 years old: a randomised controlled study. J Clin Nurs. 2020;29:1151–61.
Nicholas DB, Zwaigenbaum L, Ing S, MacCulloch R, Roberts W, McKeever P, et al. “Live it to understand it” the experiences of mothers of children with autism spectrum disorder. Qual Health Res. 2016;26:921–34.
Bombard Y, Hayeems RZ. How digital tools can advance quality and equity in genomic medicine. Nat Rev Genet. 2020;21:505–6.
Gillies K, Cotton SC, Brehaut JC, Politi MC, Skea Z. Decision aids for people considering taking part in clinical trials. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD009736.pub2.
Cheung KL, Wijnen BF, Hollin IL, Janssen EM, Bridges JF, Evers SM, et al. Using best–worst scaling to investigate preferences in health care. Pharmacoeconomics. 2016;34:1195–209.
Louviere J, Lings I, Islam T, Gudergan S, Flynn T. An introduction to the application of (case 1) best–worst scaling in marketing research. Int J Res Mark. 2013;30:292–303.
Louviere J, Flynn TN. Using best-worst scaling choice experiments to measure public perceptions and preferences for healthcare reform in Australia. Patient. 2010;3:275–83.
Bridges JF, Oakes AH, Reinhart CA, Voyard E, O’Donoghue B. Developing and piloting an instrument to prioritize the worries of patients with acute myeloid leukemia. Patient Prefer Adherence. 2018;12:647–55.
Tromp K, Zwaan CM, van de Vathorst S. Motivations of children and their parents to participate in drug research: a systematic review. Eur J Pediatr. 2016;175:599–612.
Ryan M, Watson V, Entwistle V. Rationalising the ‘irrational’: a think aloud study of discrete choice experiment responses. Health Econ. 2009;18:321–36.
Louviere JJ, Flynn TN, Marley AAJ. Best-worst scaling: theory, methods and applications. Cambridge University Press, Cambridge; 2015.
Flynn TN. Valuing citizen and patient preferences in health: recent developments in three types of best–worst scaling. Expert Rev Pharm Outcomes Res. 2014;10:259–67.
Flynn TN, Louviere JJ, Peters TJ, Coast J. Using discrete choice experiments to understand preferences for quality of life. Variance-scale heterogeneity matters. Soc Sci Med. 2010;70:1957–65.
McFadden D. Conditional logit analysis of qualitative choice behavior. In: Frontiers in econometrics. Academic Press; 1973. p. 105–42.
Tait AR, Voepel-Lewis T, Malviya S. Participation of children in clinical research factors that influence a parent’s decision to consent. J Am Soc Anesthesiol. 2003;99:819–25.
Caldwell PH, Butow PN, Craig JC. Parents’ attitudes to children’s participation in randomized controlled trials. J Pediatr. 2003;142:554–9.
Acknowledgements
The authors would like to thank the parents and caregivers who provided responses to the survey and those who helped with survey development. The authors are grateful to Dr Philip Shaw at the National Human Genome Research Institute for recruitment support. The authors would like to thank the National Fragile X Foundation and FRAXA for their help advertising our study.
Funding
This research study was funded by the National Human Genome Research Institute Intramural Research Program, National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Turbitt, E., D’Amanda, C., Hyman, S. et al. Parent clinical trial priorities for fragile X syndrome: a best–worst scaling. Eur J Hum Genet 29, 1245–1251 (2021). https://doi.org/10.1038/s41431-021-00922-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-021-00922-w
This article is cited by
-
A new impact factor for European Journal of Human Genetics
European Journal of Human Genetics (2021)