Abstract
Design A multicentre, prospective, randomised, placebo-controlled, double-blinded clinical trial reported the early implant failure and postoperative infections of healthy or relatively healthy patients receiving 2 grams of amoxicillin one hour preoperatively from their scheduled dental implant placement. The registration of the study protocol in EudraCT and Clinical Trials.gov (#NCT03412305) followed the ethical principles of the Declaration of Helsinki and the CONSORT guidelines for clinical trials.
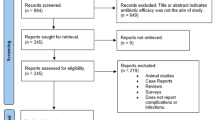
Case selection Several trial drugs expired before recruiting the intended 1,000 patients calculated based on previous trials reporting 2% and 5% early implant loss, with and without antibiotic prophylaxis. Thus, the study cohort (age >18 years, not planned for immediate loading, not requiring substantial bone augmentation, with an absence of severe diseases or immunosuppression or immunodeficiency) received 757 implants in total between November 2014 and April 2018, consisting of the prophylactic antibiotic therapy group (patients n = 235) and the placebo group (patients n = 235), with a fair sex distribution and a mean age of 57.4 ± 13.9 years. A computer-generated list of random numbers assisted the randomisation (test or control group) with a block-size six. For the clinical procedures, bone augmentation was limited to autogenous bone chips and bone debris. One- and two-stage surgery protocols were used in maxillary or mandibular single or multiple dental implants. The utilised implant systems were Straumann SLA (Straumann Implants, Switzerland), Astra Tech Dental Implant Systems (Dentsply Sirona, Sweden), Nobel Biocare (Sweden) and Southern Implants (Ltd, South Africa). Chlorhexidine 0.2% was prescribed preoperatively and/or postoperatively. Implant failure was the main measured outcome, whereas postoperative infections and adverse events were the secondary outcomes postoperatively assessed at 7-14-day (first follow-up) and 3-6-month (second follow-up) intervals.
Data analysis The sample size calculation (type one error: 0.05; power: 80%) estimated 500 patients in each group. Proportional differences and relative risk (RR) with a 95% confidence interval (CI) were calculated. Implant failure was the dependent variable for the multiple logistic regression (MLR) model examining the indicator variables smoking (yes or no), and age (<50 years; 50-64; and ≥65), as well as the independent variables bone augmentation (yes or no), number of implants (1, 2-3 and ≥4), and treatment group (antibiotic prophylaxis or placebo). P-values <0.05 or 95% CIs for ratios not including one were deemed statistically significant. The analyses were carried out using statistical software for data science (STATA).
Results Overall, six (2.5%) and seven patients (3.0%) from the amoxicillin and placebo groups had implant failures, respectively. Thus, the intergroup difference was not significant (RR: 0.85; 95% CI: 0.29-2.48, p = 0.75). Absolute risk reduction was 0.46%, with a number needed to treat (NNT) of 219. In other words, one in every 219 patients will benefit from receiving prophylactic antibiotics. In addition, no variable was associated with implant failure. Two (0.8%) and five patients (2.1%) from the amoxicillin and placebo groups, respectively, had postoperative infections at the first follow-up interval. Thus, the intergroup difference was not significant (RR: 0.29; 95% CI: 0.08-2.01, p = 0.25). Five (2.1%) and seven patients (3.0%) from the amoxicillin and placebo groups, respectively, had postoperative infections at the second follow-up interval. Thus, the intergroup difference was not significant (RR: 0.70; 95% CI: 0.23-2.18, p = 0.54). No adverse events were reported.
Conclusion Prophylactic antibiotic treatment for dental implant surgery to prevent implant loss may not be appropriate. Each dose must be prescribed based on evidence-based guidelines to avoid overuse and misuse of antibiotics promoting resistant bacteria.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Afrashtehfar K I, Schimmel M. Muscular activity may improve in edentulous patients after implant treatment. Evid Based Dent 2016; 17: 119-120.
Afrashtehfar K I. Conventional free-hand, dynamic navigation and static guided implant surgery produce similar short-term patient-reported outcome measures and experiences. Evid Based Dent 2021; 22: 143-145.
Afrashtehfar K I. The all-on-four concept may be a viable treatment option for edentulous rehabilitation. Evid Based Dent 2016; 17: 56-57.
Afrashtehfar K I, Katsoulis J, Koka S, Igarashi K. Single versus splinted short implants at sinus augmented sites: A systematic review and meta-analysis. J Stomatol Oral Maxillofac Surg 2021; 122: 303-310.
Afrashtehfar K I, Bryant S R. Understanding the Lived Experience of North American Dental Patients With a Single-Tooth Implant in the Upper Front Region of the Mouth: Protocol for a Qualitative Study. JMIR Res Protoc 2021; DOI: 10.2196/25767.
Afrashtehfar K I, Esfandiari S. Five things to know about teeth in a day with dental implants. J N J Dent Assoc 2014; 85: 24-25.
Afrashtehfar K I, Assery M K A, Bryant S R. Aesthetic Parameters and Patient-Perspective Assessment Tools for Maxillary Anterior Single Implants. Int J Dent 2021; DOI: 10.1155/2021/6684028.
Afrashtehfar K I, Del Fabbro M. Clinical performance of zirconia implants: A meta-review. J Prosthet Dent 2020; 123: 419-426.
Afrashtehfar K I, Moawad R A, F-Eddin A W, Wang H L. Mandibular full-arch fixed prostheses supported by three-dental-implants: A protocol of an overview of reviews. PLoS One 2022; DOI: 10.1371/journal.pone.0265491.
Afrashtehfar K I, Brägger U, Hicklin S P. Reliability of Interproximal Bone Height Measurements in Bone-and Tissue-Level Implants: A Methodological Study for Improved Calibration Purposes. Int J Oral Maxillofac Implants 2020; 35: 289-296.
Rodríguez Sánchez F, Arteagoitia I, Rodríguez Andrés C, Caiazzo A. Antibiotic prophylaxis habits in oral implant surgery among dentists in Italy: a cross-sectional survey. BMC Oral Health 2019; 19: 265.
Williams R G M. Antibiotic prophylaxis during dental implant placement in the UK. Br Dent J 2020; 229: 787-792.
Caiazzo A, Canullo L; Consensus Meeting Group, Pesce P. Consensus Report by the Italian Academy of Osseointegration on the Use of Antibiotics and Antiseptic Agents in Implant Surgery. Int J Oral Maxillofac Implants 2021; 36: 103-105.
Abd-Elwahab Radi I, Hassaan A. Which is the best antibiotic prophylaxis protocol to prevent early implant failures? Evid Based Dent 2019; 20: 105-106.
Kim A S, Abdelhay N, Levin L, Walters J D, Gibson M P. Antibiotic prophylaxis for implant placement: a systematic review of effects on reduction of implant failure. Br Dent J 2020; 228: 943-951.
Chen Z, Chen D, Zhang S, Tang L, Li Q. Antibiotic prophylaxis for preventing dental implant failure and postoperative infection: A systematic review of randomized controlled trials. Am J Dent 2017; 30: 89-95.
Kashani H, Hilon J, Rasoul M H, Friberg B. Influence of a single preoperative dose of antibiotics on the early implant failure rate. A randomized clinical trial. Clin Implant Dent Relat Res 2019; 21: 278-283.
Haque M, Sartelli M, Haque S Z. Dental infection and resistance-global health consequences. Dent J (Basel). 2019; 7: 22.
Patini R, Mangino G, Martellacci L, Quaranta G, Masucci L, Gallenzi P. The Effect of Different Antibiotic Regimens on Bacterial Resistance: A Systematic Review. Antibiotics (Basel) 2020; 9: 22.
Bansal R, Jain A, Goyal M, Singh T, Sood H, Malviya H S. Antibiotic abuse during endodontic treatment: A contributing factor to antibiotic resistance. J Family Med Prim Care 2019; 8: 3518-3524.
Momand P, Becktor J P, Naimi-Akbar A, Tobin G, Götrick B. Effect of antibiotic prophylaxis in dental implant surgery: A multicentre placebo-controlled double-blinded randomized clinical trial. Clin Implant Dent Relat Res 2022; 24: 116-124.
Jinno Y, Jimbo R, Hjalmarsson J, Johansson K, Stavropoulos A, Becktor J P. Impact of surface contamination of implants with saliva during placement in augmented bone defects in sheep calvaria. Br J Oral Maxillofac Surg 2019; 57: 41-46.
Chrcanovic B R, Kisch J, Albrektsson T, Wennerberg A. Factors Influencing Early Dental Implant Failures. J Dent Res 2016; 95: 995-1002.
Payer M, Tan W C, Han J et al. The effect of systemic antibiotics on clinical and patient-reported outcome measures of oral implant therapy with simultaneous guided bone regeneration. Clin Oral Implants Res 2020; 31: 442-451.
Author information
Authors and Affiliations
Ethics declarations
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Afrashtehfar, K., Desai, V. & Afrashtehfar, C. Preoperative administration of amoxicillin is not recommended in healthy patients undergoing implant surgery. Evid Based Dent 23, 78–80 (2022). https://doi.org/10.1038/s41432-022-0266-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-022-0266-7
This article is cited by
-
So führen wir die zahnärztliche Implantologie bei Patienten mit entzündlich rheumatischen Erkrankungen durch
Zeitschrift für Rheumatologie (2023)