Abstract
Background
To evaluate the singlet oxygen (1O2) production of oxygen assisted %0.1 riboflavin and ultraviolet-A (UVA) crosslinking therapy (with and without oxygen assistance), in combination with standard, accelerated and hyper-accelerated procedures via an important quantitive marker of 1O2 which is the photo-oxidation of 1,3 diphenylisobenzofuran (DPBF).
Methods
%0.1 riboflavin-containing wells were irradiated with UVA light (365-nm wavelength) with or without 2-4-6-8 L/min oxygen flow assistance. Measurements of decrease in absorbance of DPBF were made in 30 mW (hyper-accelerated), 9 mW (accelerated), and 3 mW UV-A (standard) applications, and with additional 2-4-6-8 L/min oxygen flow in 30 mW and 2 L/min oxygen flow in 9 mW. A total of 8 different UV-A irradiance with and without oxygen supplementation groups were formed.
Results
2 L/min oxygen assisted accelerated UV-A irradiance group has shown a greater decrease in DPBF absorbance compared to Dresden protocol. (p = 0.014) Also, Dresden protocol has shown a greater decrease in DPBF compared to all groups except accelerated crosslinking with 2 L/min oxygen. (p < 0.001) Oxygen assisted hyper-accelerated crosslinking groups were showed greater reduction in DPBF absorbance compared to standard crosslinking without oxygen groups. (p < 0.001).
Conclusion
Oxygen supplementation may increase the singlet oxygen generation to the similar levels of Dresden Protocol’s in accelerated group. Also, more singlet oxygen generation with oxygen supplementation compared to standard UV-A application might be considered to be promising in terms of shortening the crosslinking therapy.
Similar content being viewed by others
Introduction
Corneal Collagen Cross-linking (CXL), which is frequently used in the treatment of keratoconus, is a very successful method in stopping the progression of the disease [1]. CXL treatment stops disease progression by forming strong chemical bonds between collagen side chains in the anterior stroma [2]. In CXL treatment, photosensitive riboflavin molecule is induced with ultraviolet A and produces reactive oxygen species (ROS) [3]. One of the most important of these radicals is singlet oxygen which reacts with collagen fibres and proteoglycans to form desired strong covalent bonds between these molecules [3,4,5]. In the gold standard treatment, following the corneal epithelial removal, 30 mW/cm2 UVA application for 30 min is performed after riboflavin application for 30 min [1]. To shorten the treatment time and increase comfort, 10 min of 9 mW/cm2 and 3 min of 30 mW/cm2 CXL treatments with shorter irradiance time are applied [6]. However, these new shortened CXL treatment modalities are not as effective as the gold standard in the changing biomechanical properties of the corne [6]. Although there are various theories on this subject, the decrease in ROS formation can be considered as one of them, due to the lack of sufficient oxygen in the CXL modalities with short irradiance time [7]. Various probes are used to measure singlet oxygen formed after UVA in CXL, one of which is 1,3-diphenylisobenzofuran (DPBF) [8]. The reaction of singlet oxygen (1O2) with DPBF to form an endoperoxide via a [4+2] cycloaddition (Fig. 1), and the resulting loss of the extended π-electron system and its characteristic spectroscopic properties. DPBF forms endoperoxide which then decomposes to 1,2-dibenzoylbenzene [8].
In our study, the singlet oxygen amount generated during different CXL modalities and different oxygen currents was indirectly measured by reduction in DPBF concentration and compared with the gold standard method. We tried to evaluate whether oxygen flow application with different UVA irradiance times has a place in the keratoconus treatment.
Methods
In the present study, the photo-oxidation of DPBF was used to evaluate the singlet oxygen production and in this spectrophotometric method, DPBF is oxidized to its corresponding diketone upon interaction with singlet oxygen in stoichiometric equivalents. The loss in the absorbance at 410 nm provides an equivalence of singlet oxygen production [9].
Riboflavin and 1,3-diphenylisobenzofuran were purchased from Sigma-Aldrich Co, and the quartz microplate was purchased from ZINSSER, Germany.
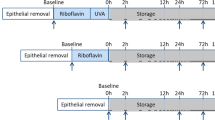
0.1% (w/v) riboflavin solution and 10 μM DPBF solution prepared in an ethanol: water (50:50 v/v) mixture were pipetted into a microplate well then the absorbance at 410 nm recorded as first absorbance using Molecular Devices-SpectraMax iD3. After the UV-A irradiance (CRS-X crosslinker, Yuratek-Turkey) of the same well, the second absorbance was recorded. (Fig. 2) All wells were irradiated separately and a new plate was used for each sample to avoid UV-A scattering to adjacent wells as described
previously [10]. (Fig. 2A) From these data, the degradation rates of DPBF were calculated as the percentage of decreased absorbance.
UV-A irradiance experiments were distributed into eight groups and all groups were repeated at least ten times (Table 1).
SPSS 26.0 software (SPSS Inc, Chicago, IL) was used for statistical analysis. The distribution pattern of variables was evaluated with the help of visual and analytical methods. The Independent t-test was used for variables with normal distribution, while Mann Whitney u test was used for variables with non-normal distribution
Results
A total of 80 samples in groups of 10 were used for this study. All UV-A irradiance and additional oxygen flow groups were shown in Table 1 (Fig. 3).
In order to investigate whether singlet oxygen formation can be achieved at the classical method level, UV-A application was done with different oxygen currents until a similar decrease in DPBF absorbance to the classical method was achieved. Pretest was not performed for power analysis because we did not know the results to be encountered. However, the sample size was not changed since observed power was detected as 100% in the posthoc power analysis.While these levels were not reached in the 30 mW groups, they were reached in the first attempt in the 9 mW group. Dresden protocol which is 3 mW UV-A irradiance for 30 min (Group I) has shown a greater decrease in DPBF absorbance compared to all groups except 9 mW UV-A irradiance (Group IV) for 10 min with 2 L/min oxygen flow. (Table 2) When 30 mW UV-A groups were compared with each other, groups that have additional oxygen flow with 2 L/min, 4 L/min, 6 L/min, 8 L/min (Groups V–VI–VII–VIII) were showed a greater reduction of absorbance compared to 30 mW UV-A irradiance without oxygen flow (Group III). (p < 0.001) 9 mW UV-A with 2 L/min oxygen flow (Group IV) showed a greater decrease in DPBF absorbance compared to the 9 mW UV-A group (Group II) (p < 0.001). All pairwise comparisons were shown in Table 2.
Discussion
Keratoconus and corneal ectatic diseases have been diagnosed at an earlier stage thanks to the corneal topography and corneal tomography that emerged with the advancement of technology [11]. Diagnosis of these ectatic diseases at an earlier stage has increased the desire to stop the disease progression with faster and effective treatment without the need for corneal transplantation [12]. Standard CXL treatment (Dresden Protocol) which involves the application of 3 mw/cm2 UV-A and 0.1% riboflavin for 30 min for each in the following order after the peeling of the corneal epithelium, is considered the gold standard in the treatment of these ectatic diseases defined by Wollensak et al. [1]. However, the long duration of Dresden protocol for both the ophthalmologist and the patient has led to the search for new modalities. As a result, accelerated CXL treatments have been suggested by different studies [5, 11, 12]. Accelerated CXL treatments are based on the Bunsen-Roscoe law of reciprocity which is based on the principle that as long as the applied total energy is equal, the applied light intensity and duration are in an inverse relationship and the total effect that will occur will be the same. However, recent studies suggest that Bunsen-Roscoe law’s application might be restricted in vivo samples [13, 14]. CXL treatment shows its effect through two different pathways, type 1 (anaerobic) and type 2 (aerobic) reaction [3]. Kamaev et al. suggested a faster oxygen depletion rate with higher irridance UV-A application models which might lead to a lesser cross-linking effect due to lesser ROS molecules [3]. Also, in a study by Richoz et al., porcine corneas which CXL application was done in a lesser oxygen concentration environment showed no change in corneal stiffness compared to controls [15]. These studies suggest that the most important limiting factor might be the oxygen availability in the environment [3, 15]. Several novel methods which showed promising results were tried to overcome the oxygen insufficiency such as using special oxygen delivery googles during UV-A application, delivering systemic oxygen via nasal cannula [16,17,18]. In the present study, it is aimed to objectively determine the formation of singlet oxygen which has a very important place in the CXL treatment, in different UV-A irradiances, and with different oxygen flows in the laboratory environment to reveal whether singlet oxygen formation close to the gold standard method can be obtained.
CXL treatment shows its effect through 2 different pathways as mentioned previously, type 1 (anaerobic) and type 2 (aerobic) reaction [3]. In our study, only type 2 reaction could be measured by indirectly measuring singlet oxygen. Depletion of the oxygen in the environment at the beginning of UV-A application is one of the most important obstacles preventing the acceleration of UV-A application [3]. Furthermore, oxygen depletion during the UV-A application is accelerated when UV-A irridance is increased. Also, in previous studies, it is thought that the main effect of CXL treatment is created by type 2 (aerobic) reaction [3, 9]. In our study, lower singlet oxygen formation compared to Dresden protocol was observed in all 30 mW groups with and without oxygen even with the addition of oxygen flow during the UV-A application which is used to prevent this oxygen depletion in 30 mW/cm2 irradiance groups. Riboflavin is thought to undergo faster photodegradation at higher irradiance [3]. In in vivo and ex vivo studies, the application of fresh riboflavin to tissue renders this photodegradation negligible [3]. However, in our study, due to the riboflavin contained in the well, the photodegradation that occurred during the UV-A application might have resulted in less singlet oxygen formation despite the addition of oxygen.
In a recent study by Bao et al., significant corneal stiffness increase was obtained with the application of 3 mW UV-A for 30 min and 9 mW UV-A for 10 min, while no difference was found with the control group in higher irradiance and lower duration UV-A applications above 9 mW/10 min group [14]. As a result, Bao et al. suggested that the Bunsen-Roscoe law does not apply to CXL in corneal tissue [14]. Similarly, in our study, although the total energy is equal, the lower amount of singlet oxygen generation suggests that this reaction does not comply with the Bunsen-Roscoe law in in vitro conditions [14]. In addition, the exact oxygen concentration in the riboflavin solution could not be measured directly with the present setup. Similar to the study by Kamaev et al., the oxygen in the solution may be depleting at the early stages of the UV-A application, and oxygen concentration in the solution might need time to replenish to sufficient levels for aerobic CXL reaction [3]. In our study, the 30 mW groups cannot reach the Dresden Protocol’s singlet oxygen generation capacity even with the additional oxygen aid. However, it can reach values that are comparable with the 9 mW group, which is currently used for CXL and known to have a stiffening effect [14].
30 mw UV-A application with 8 L/min oxygen flow showed lesser singlet oxygen formation compared to lesser oxygen flow currents such as 6 L/min and 4 L/min. Although, there aren’t enough data in the literature to correctly interpret this finding, the presence of very high amounts of oxygen in the environment may slow down the singlet oxygen production by causing similar substrate inhibition to enzymatic reactions [19]. Also, the presence of a high amount of oxygen in the environment may have a restrictive effect on the reaction by changing the pressure in the environment [8].
Statistically lesser oxygen radicals were formed in the group treated with 9 mw/cm2 UV-A for 10 min compared to the 3 mW/cm2 UV-a application for 30 min, while it was found that when 2 L/min oxygen flow was added to 9 mW/cm2 application, more singlet oxygen radicals were formed. Lesser riboflavin photodegradation compared to the 30 mW group due to lower irradiance might have led to more singlet oxygen generation [3]. Also, the addition of oxygen flow to the UV-A application might have been prevented the depletion of oxygen in the 9 mW/10 min group due to usage of lesser power compared to 30 mW groups which might have led to singlet oxygen generation similar and even greater to conventional CXL. In a recent study that compares classic and accelerated CXL methods, accelerated CXL groups of 9 mW/min for 10 min and 30 mW/min groups showed improvements in terms of topographical keratoconus indices, best-corrected visual acuity [20]. In the same study, despite the similar functional outcomes in all groups, standard CXL with 30 mW/min UV-A group showed a greater change in keratoconus indices compared to accelerated UV-A regimens [20]. Similar to our results, Faramarzi et al. suggested that systemic oxygen supplementation during the accelerated UV-A application with 9 mW UV-A might lead to topographic changes comparable to the Dresden protocol [16]. Although, to the best of our knowledge, there is no study in the literature comparing 9 mW UV-A CXL application with oxygen supplementation and classical CXL treatment, comparable singlet oxygen generation might suggest that similar efficacy might be established in the future in vivo and ex vivo studies.
Diakonis et al. suggested that accelerated CXL with 30 mW UV-A irradiance might cause a similar stiffening effect whether done in an oxygen-rich environment or not [21]. However, corneal stiffening was achieved to some degree with accelerated CXL but could not reach the corneal stiffening effect of the Dresden protocol [21]. Although, singlet oxygen formation in 30 mW groups with oxygen aid was found to be comparable to the 9 mW group in our study, it is not possible to fully interpret our results to in vivo or ex vivo conditions, since the oxygenation of the cornea cannot be imitated in laboratory settings.
In conclusion, oxygen supplementation can be considered to be promising in terms of shortening CXL therapy. Future ex vivo and in vivo studies are needed to investigate the effects of oxygen radical formation and find a safer and optimal CXL treatment modality with oxygen supplementation.
Summary table
What was known before
-
The corneal cross-link (CXL)reaction is divided into type 1 and type 2 reactions.
-
The type 2 reaction is thought to be oxygen dependent and its CXL effect is mediated by reactive oxygen species.
What this study adds
-
This study may show that the reactive oxygen radical formation during UV-A irradiance can be increased by increasing the oxygen density in the environment.
References
Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7.
Meiri Z, Keren S, Rosenblatt A, Sarig T, Shenhav L, Varssano D. Efficacy of corneal collagen cross-linking for the treatment of keratoconus: a systematic review and meta-analysis. Cornea. 2016;35:417–28.
Kamaev P, Friedman MD, Sherr E, Muller D. Photochemical kinetics of corneal cross-linking with riboflavin. Invest Ophthalmol Vis Sci. 2012;53:2360–7.
McCall AS, Kraft S, Edelhauser HF, Kidder GW, Lundquist RR, Bradshaw HE, et al. Mechanisms of corneal tissue cross-linking in response to treatment with topical riboflavin and long-wavelength ultraviolet radiation (UVA). Invest Ophthalmol Vis Sci. 2010;51:129–38.
Zhang Y, Conrad AH, Conrad GW. Effects of ultraviolet-A and riboflavin on the interaction of collagen and proteoglycans during corneal cross-linking. J Biol Chem. 2011;286:13011–22.
Beloshevski B, Shashar S, Mimouni M, Novack V, Malyugin BE, Boiko M, et al. Comparison between three protocols of corneal collagen crosslinking in adults with progressive keratoconus: Standard versus accelerated CXL for keratoconus. Eur J Ophthalmol. 2020;1120672120972632. https://doi.org/10.1177/1120672120972632. Epub ahead of print.
Mazzotta C, Traversi C, Caragiuli S, Rechichi M. Pulsed vs continuous light accelerated corneal collagen crosslinking: in vivo qualitative investigation by confocal microscopy and corneal OCT. Eye. 2014;28:1179–83.
Entradas T, Waldron S, Volk M. The detection sensitivity of commonly used singlet oxygen probes in aqueous environments. J Photochem Photobiol B: Biol. 2020;204:111787.
Gorman A, Killoran J, O’Shea C, Kenna T, Gallagher WM, O’Shea DF. In vitro demonstration of the heavy-atom effect for photodynamic therapy. J Am Chem Soc. 2004;126:10619–31.
Bilgihan K, Kalkanci A, Ozdemir HB, Yazar R, Karakurt F, Yuksel E, et al. Evaluation of antifungal efficacy of 0.1% and 0.25% riboflavin with UVA: a comparative in vitro study. Curr Eye Res. 2016;41:1050–6.
Waszczykowska A, Jurowski P. Two-year accelerated corneal cross-linking outcome in patients with progressive keratoconus. Biomed Res Int. 2015;2015:325157.
Hashemi H, Mohebbi M, Asgari S. Standard and accelerated corneal cross-linking long-term results: a randomized clinical trial. Eur J Ophthalmol. 2020;30:650–7.
Hammer A, Richoz O, Mosquera SA, Tabibian D, Hoogewoud F, Hafezi F. Corneal biomechanical properties at different corneal cross-linking (CXL) irradiances. Investigative Ophthalmol Vis Sci. 2014;55:2881–4.
Bao F, Zheng Y, Liu C, Zheng X, Zhao Y, Wang Y, et al. Changes in corneal biomechanical properties with different corneal cross-linking irradiances. J Refract Surg. 2018;34:51–8.
Richoz O, Hammer A, Tabibian D, Gatzioufas Z, Hafezi F. The biomechanical effect of corneal collagen cross-linking (CXL) with riboflavin and UV-A is oxygen dependent. Transl Vis Sci Technol. 2013;2:6.
Faramarzi A, Hassanpour K, Rahmani B, Yazdani S, Kheiri B, Sadoughi MM. Systemic supplemental oxygen therapy during accelerated corneal crosslinking for progressive keratoconus: randomized clinical trial. J Cataract Refract Surg. 2021;47:773–9.
Mazzotta C, Sgheri A, Bagaglia SA, Rechichi M, Di Maggio A. Customized corneal crosslinking for treatment of progressive keratoconus: Clinical and OCT outcomes using a transepithelial approach with supplemental oxygen. J Cataract Refract Surg. 2020;46:1582–7.
Matthys A, Cassagne M, Galiacy SD, El Hout S, Fournié P, Malecaze F. Transepithelial corneal cross-linking with supplemental oxygen in Keratoconus: 1-year clinical results. J Refract Surg. 2021;37:42–8.
Wu B. Substrate inhibition kinetics in drug metabolism reactions. Drug Metab Rev. 2011;43:440–56.
Lang PZ, Hafezi NL, Khandelwal SS, Torres-Netto EA, Hafezi F, Randleman JB. Comparative functional outcomes after corneal crosslinking using standard, accelerated, and accelerated with higher total fluence protocols. Cornea 2019;38:433–41.
Diakonis VF, Likht NY, Yesilirmak N, Delgado D, Karatapanis AE, Yesilirmak Y, et al. Corneal elasticity after oxygen enriched high intensity corneal cross linking assessed using atomic force microscopy. Exp Eye Res. 2016;153:51–5.
Acknowledgements
The authors thank Naime Tömek who is the supporter of the ÖNTAL (Teacher Naime Tömek Research Laboratory).
Author information
Authors and Affiliations
Contributions
I, Kamil Bilgihan hereby confirm that all named authors meet the ICMJE requirement of authorship and meet all three criteria as mentioned below: (1) substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published.
Corresponding author
Ethics declarations
Declaration of interest statement
We have no financial disclosure or conflicts of interest with the presented material in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ercin, U., Aribas, Y.K., Tefon Aribas, A.B. et al. Singlet oxygen formation during accelerated and hyperaccelerated corneal cross-linking: in vitro study. Eye 35, 3147–3151 (2021). https://doi.org/10.1038/s41433-021-01731-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01731-7