Abstract
Testosterone therapy (TT) is a type of gender-affirming hormone therapy (GAHT) in lesbian, gay, bisexual, transgender, and genderqueer (LGBTQ) populations for gender dysphoria (GD), body uneasiness, and sexual dysfunction. The physical and physiological effects of TT vary widely depending on the dosing regimen and duration of treatment. An individualized approach prioritizing patient-specific desired effects in the context of pre-existing characteristics and health history is strongly recommended. Although TT is an effective treatment for many patients, there has been an increase in the illegitimate acquisition of TT in recent years. Non-judicious prescribing and lack of physician surveillance increases the risk of unintended side effects and potential serious health consequences.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Nieschlag E, Nieschlag S. Endocrine history: the history of discovery, synthesis and development of testosterone for clinical use. Eur J Endocrinol. 2019;180:R201–12.
Rastrelli G, Corona G, Maggi M. Testosterone and sexual function in men. Maturitas. 2018;112:46–52.
Tsametis CP, Isidori AM. Testosterone replacement therapy: for whom, when and how? Metabolism. 2018;86:69–78.
Vegunta S, Kling JM, Kapoor E. Androgen therapy in women. J Women’s Health. 2019;29:57–64.
Radix A. Hormone therapy for transgender adults. Urol Clin North Am. 2019;46:467–73.
American Psychological Association. Guidelines for psychological practice with transgender and gender nonconforming people. Am Psychol. 2015;70:832–64.
Defreyne J, T’Sjoen G. Transmasculine hormone therapy. Endocrinol Metab Clin North Am. 2019;48:357–75.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DMS-5®). Washington, DC. American Psychiatric Pub; 2013.
Nieschlag E, Nieschlag S. Testosterone deficiency: a historical perspective. Asian J Androl. 2014;16:161.
Morgentaler A, Traish A. The history of testosterone and the evolution of its therapeutic potential. Sex Med Rev. 2020;8:286–96.
Gagliano-Jucá T, Basaria S. Testosterone replacement therapy and cardiovascular risk. Nat Rev Cardiol. 2019;16:555–74.
Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy Response in Hypogonadal Men (TRAVERSE) Study. 2022. NCT03518034. https://www.clinicaltrials.gov/ct2/show/NCT03518034. Accessed 21 Sept 2021.
Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, et al. Testosterone therapy in men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2010;95:2536–59.
Mulhall JP, Trost LW, Brannigan RE, Kurtz EG, Redmon JB, Chiles KA, et al. Evaluation and management of testosterone deficiency: AUA guideline. J Urol. 2018;200:423.
Bhasin S, Enzlin P, Coviello A, Basson R. Sexual dysfunction in men and women with endocrine disorders. Lancet. 2007;369:597–611.
Wang C, Nieschlag E, Swerdloff R, Behre HM, Hellstrom WJ, Gooren LJ, et al. Investigation, treatment and monitoring of late-onset hypogonadism in males. Eur J Endocrinol. 2008;159:507–14.
Spitzer M, Huang G, Basaria S, Travison TG, Bhasin S. Risks and benefits of testosterone therapy in older men. Nat Rev Endocrinol. 2013;9:414–24.
Cunningham GR. Testosterone replacement therapy for late-onset hypogonadism. Nat Rev Urol. 2006;3:260–7.
FDA Drug Safety Communication. FDA cautions about using testosterone products for low testosterone due to aging; requires labeling change to inform of possible increased risk of heart attack and stroke with use. FDA. 2018. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-cautions-about-using-testosterone-products-low-testosterone-due. Accessed 13 June 2021.
Snyder PJ, Bhasin S, Cunningham GR, Matsumoto AM, Stephens-Shields AJ, Cauley JA, et al. Effects of testosterone treatment in older men. N. Engl J Med. 2016;374:611–24.
Cunningham GR, Stephens-Shields AJ, Rosen RC, Wang C, Bhasin S, Matsumoto AM, et al. Testosterone treatment and sexual function in older men with low testosterone levels. J Clin Endocrinol Metab. 2016;101:3096–104.
Roy CN, Snyder PJ, Stephens-Shields AJ, Artz AS, Bhasin S, Cohen HJ, et al. Association of testosterone levels with anemia in older men: a controlled clinical trial. JAMA Intern Med. 2017;177:480.
Dimopoulou C, Ceausu I, Depypere H, Lambrinoudaki I, Mueck A, Pérez-López FR, et al. EMAS position statement: testosterone replacement therapy in the aging male. Maturitas. 2016;84:94–99.
Isidori AM, Balercia G, Calogero AE, Corona G, Ferlin A, Francavilla S, et al. Outcomes of androgen replacement therapy in adult male hypogonadism: recommendations from the Italian society of endocrinology. J Endocrinol Investig. 2015;38:103–12.
Layton JB, Li D, Meier CR, Sharpless JL, Stürmer T, Jick SS, et al. Testosterone lab testing and initiation in the United Kingdom and the United States, 2000 to 2011. J Endocrinol Metab. 2014;99:835–42.
Handelsman DJ. Global trends in testosterone prescribing, 2000–2011: expanding the spectrum of prescription drug misuse. Med J Aust. 2013;199:548–51.
Baillargeon J, Urban RJ, Ottenbacher KJ, Pierson KS, Goodwin JS. Trends in androgen prescribing in the United States, 2001 to 2011. JAMA Intern Med. 2013;173:1465.
Purcell DW, Wolitski RJ, Hoff CC, Parsons JT, Woods WJ, Halkitis PN. Predictors of the use of viagra, testosterone, and antidepressants among HIV-seropositive gay and bisexual men. AIDS. 2005;19:S57–S66.
Hackett G, Kirby M, Wylie K, Heald A, Ossei-Gerning N, Edwards D, et al. British society for sexual medicine guidelines on the management of erectile dysfunction in men—2017. J Sex Med. 2018;15:430–57.
Hackett GI, Cole NS, Deshpande AA, Popple MD, Kennedy D, Wilkinson P. Biochemical hypogonadism in men with type 2 diabetes in primary care practice. Br J Diabetes Vasc. 2009;9:226–31.
Cui Y, Zong H, Yan H, Zhang Y. The effect of testosterone replacement therapy on prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2014;17:132–43.
Hackett GI. Testosterone replacement therapy and mortality in older men. Drug Saf. 2016;39:117–30.
Hodgson TK, Braunstein GD Physiological Effects of Androgens in Women. In: Azziz R, Nestler JE, Dewailly D (eds). Androgen Excess Disorders in Women. 2nd ed. Totowa, NJ: Humana Press; 2007. p. 49–62.
Elraiyah T, Sonbol MB, Wang Z, Khairalseed T, Asi N, Undavalli C, et al. The benefits and harms of systemic dehydroepiandrosterone (DHEA) in postmenopausal women with normal adrenal function: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2014;99:3536–42.
Davis SR, Moreau M, Kroll R, Bouchard C, Panay N, Gass M, et al. Testosterone for low libido in postmenopausal women not taking estrogen. N. Engl J Med. 2008;359:2005–17.
Braunstein GD, Sundwall DA, Katz M, Shifren JL, Buster JE, Simon JA, et al. Safety and efficacy of a testosterone patch for the treatment of hypoactive sexual desire disorder in surgically menopausal women: a randomized, placebo-controlled trial. Arch Intern Med. 2005;165:1582–9.
Somboonporn W, Bell RJ, Davis SR. Testosterone for peri and postmenopausal women. Cochrane Database Syst Rev. 2005;4:CD004509.
Panzer C, Guay A. Testosterone replacement therapy in naturally and surgically menopausal women. J Sex Med. 2009;6:8–18.
Davis SR, Braunstein GD. Efficacy and safety of testosterone in the management of hypoactive sexual desire disorder in postmenopausal women. J Sex Med. 2012;9:1134–48.
Dimitrakakis C, Jones RA, Liu A, Bondy CA. Breast cancer incidence in postmenopausal women using testosterone in addition to usual hormone therapy. Menopause. 2004;11:531–5.
Nachtigall L, Casson P, Lucas J, Schofield V, Melson C, Simon JA. Safety and tolerability of testosterone patch therapy for up to 4 years in surgically menopausal women receiving oral or transdermal oestrogen. Gynecol Endocrinol. 2011;27:39–48.
Clayton AH, Goldstein I, Kim NN, Althof SE, Faubion SS, Faught BM, et al. The International Society for the Study of Women’s Sexual Health Process of Care for Management of Hypoactive Sexual Desire Disorder in Women. Mayo Clin Proc. 2018;93:467–87.
Wierman ME, Arlt W, Basson R, Davis SR, Miller KK, Murad MH, et al. Androgen Therapy in Women: A Reappraisal: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2014;99:3489–510.
UCSF Transgender Care, Department of Family and Community Medicine, University of California San Francisco. Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People. Deutsch MB (ed). 2nd ed. June 2016. transcare.ucsf.edu/guidelines.
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals. J Clin Med. 2020;9:1609.
Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. Int J Transgend. 2012;13:165–232.
Heylens G, Verroken C, Cock SD, T’Sjoen G, Cuypere GD. Effects of different steps in gender reassignment therapy on psychopathology: a prospective study of persons with a gender identity disorder. J Sex Med. 2014;11:119–26.
Fisher AD, Castellini G, Ristori J, Casale H, Cassioli E, Sensi C, et al. Cross-sex hormone treatment and psychobiological changes in transsexual persons: two-year follow-up data. J Clin Endocrinol Metab. 2016;101:4260–9.
Fisher AD, Castellini G, Bandini E, Casale H, Fanni E, Benni L, et al. Cross-sex hormonal treatment and body uneasiness in individuals with gender dysphoria. J Sex Med. 2014;11:709–19.
Zucker KJ. Epidemiology of gender dysphoria and transgender identity. Sex Health. 2017;14:404–11.
Johns MM, Lowry R, Andrzejewski J, Barrios LC, Demissie Z, McManus T, et al. Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students—19 States and Large Urban School Districts, 2017. MMWR Morb Mortal Wkly Rep. 2019;68:67–71.
Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab. 2017;102:3869–903.
Beckwith N, Reisner SL, Zaslow S, Mayer KH, Keuroghlian AS. Factors associated with gender-affirming surgery and age of hormone therapy initiation among transgender adults. Transgend Health. 2017;2:156–64.
James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality. 2016. https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf. Accessed 19 June 2021.
Moravek MB. Gender-affirming hormone therapy for transgender men. Clin Obstet Gynecol. 2018;61:687–704.
Fabris B, Bernardi S, Trombetta C. Cross-sex hormone therapy for gender dysphoria. J Endocrinol Investig. 2015;38:269–82.
Irving A, Lehault WB. Clinical pearls of gender-affirming hormone therapy in transgender patients. Ment Health Clin. 2017;7:164–7.
Miller MG, Rogol AD, ZumBrunnen TL. Secondary exposure to testosterone from patients receiving replacement therapy with transdermal testosterone gels. Curr Med Res Opin. 2012;28:267–9.
Costa LB, Rosa-e-Silva A, Medeiros S, Nacul A, Carvalho B, Benetti-Pinto C, et al. Recommendations for the use of testosterone in male transgender. Rev Bras Ginecol Obstet. 2018;40:275–80.
T’Sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine. Endocr Rev. 2019;40:97–117.
Baker KE, Wilson LM, Sharma R, Dukhanin V, McArthur K, Robinson KA. Hormone therapy, mental health, and quality of life among transgender people: a systematic review. J Endocr Soc. 2021;5:bvab011.
Colton Meier SL, Fitzgerald KM, Pardo ST, Babcock J. The Effects of Hormonal Gender Affirmation Treatment on Mental Health in Female-to-Male Transsexuals. J Gay Lesbian. J Gay Lesbian Ment Health. 2011;15:281–99.
Moreno-Arrones OM, Becerra A, Vano-Galvan S. Therapeutic experience with oral finasteride for androgenetic alopecia in female-to-male transgender patients. Clin Exp Dermatol. 2017;42:743–8.
Leiblum S, Bachmann G, Kemmann E, Colburn D, Swartzman L. Vaginal atrophy in the postmenopausal woman: the importance of sexual activity and hormones. JAMA. 1983;249:2195–8.
Miyajima T, Kim YT, Oda H. A study of changes in bone metabolism in cases of gender identity disorder. J Bone Min Metab. 2012;30:468–73.
Goh HH, Ratnam SS. Effects of hormone deficiency, androgen therapy and calcium supplementation on bone mineral density in female transsexuals. Maturitas. 1997;26:45–52.
Kesteren PV, Lips P, Gooren LJG, Asscheman H, Megens J. Long-term follow-up of bone mineral density and bone metabolism in transsexuals treated with cross-sex hormones. Clin Endocrinol. 1998;48:347–54.
Connelly PJ, Marie Freel E, Perry C, Ewan J, Touyz RM, Currie G, et al. Gender-affirming hormone therapy, vascular health and cardiovascular disease in transgender adults. Hypertension. 2019;74:1266–74.
Walker WH. Non-classical actions of testosterone and spermatogenesis. Philos Trans R Soc Lond B Biol Sci. 2010;365:1557–69.
Smith LB, Walker WH. The regulation of spermatogenesis by androgens. Semin Cell Dev Biol. 2014;30:2–13.
Gu Y, Liang X, Wu W, Liu M, Song S, Cheng L, et al. Multicenter contraceptive efficacy trial of injectable testosterone undecanoate in Chinese men. J Clin Endocrinol Metab. 2009;94:1910–5.
Light AD, Obedin-Maliver J, Sevelius JM, Kerns JL. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol. 2014;124:1120–7.
Moravek MB. Fertility preservation options for transgender and gender-nonconforming individuals. Curr Opin Obstet Gynecol. 2019;31:170–6.
Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022–33.
Cobo A, Bellver J, Domingo J, Pérez S, Crespo J, Pellicer A, et al. New options in assisted reproduction technology: the Cryotop method of oocyte vitrification. Repro Biomed Online. 2008;17:68–72.
Mitu K. Transgender reproductive choice and fertility preservation. AMA J Ethics. 2016:18:1119–25.
Jasuja GK, Bhasin S, Rose AJ. Patterns of testosterone prescription overuse. Curr Opin Endocrinol Diabetes Obes. 2017;24:240–5.
Xavier JM. The Washington, DC Transgender Needs Assessment Survey. Administration for HIV/Aids of the District of Columbia Government. 2000. http://www.glaa.org/archive/2000/tgneedsassessment1112.shtml. Accessed 13 June 2021.
Rotondi NK, Bauer GR, Scanlon K, Kaay M, Travers R, Travers A. Nonprescribed Hormone Use and Self-Performed Surgeries: “Do-It-Yourself” Transitions in Transgender Communities in Ontario, Canada. Am J Public Health. 2013;103:1830–6.
Mepham N, Bouman WP, Arcelus J, Hayter M, Wylie KR. People with Gender Dysphoria Who Self‐Prescribe Cross‐Sex Hormones: Prevalence, Sources, and Side Effects Knowledge. J Sex Med. 2014;11:2995–3001.
Stroumsa D, Crissman HP, Dalton VK, Kolenic G, Richardson CR. Insurance Coverage and Use of Hormones Among Transgender Respondents to a National Survey. Ann Fam Med. 2020;18:528–34.
Author information
Authors and Affiliations
Contributions
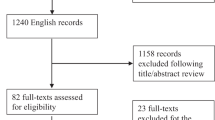
ANT and ECO conceived and designed the manuscript. ANT, AVS, and VRP collected data, interpreted findings, and drafted the manuscript with support from ECO. All authors participated in critical revision and agreed on final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tijerina, A.N., Srivastava, A.V., Patel, V.R. et al. Current use of testosterone therapy in LGBTQ populations. Int J Impot Res 34, 642–648 (2022). https://doi.org/10.1038/s41443-021-00490-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-021-00490-z