Abstract
Systemic characterisation of the human faecal microbiome provides the opportunity to develop non-invasive approaches in the diagnosis of a major human disease. However, shared microbial signatures across different diseases make accurate diagnosis challenging in single-disease models. Herein, we present a machine-learning multi-class model using faecal metagenomic dataset of 2,320 individuals with nine well-characterised phenotypes, including colorectal cancer, colorectal adenomas, Crohn’s disease, ulcerative colitis, irritable bowel syndrome, obesity, cardiovascular disease, post-acute COVID-19 syndrome and healthy individuals. Our processed data covers 325 microbial species derived from 14.3 terabytes of sequence. The trained model achieves an area under the receiver operating characteristic curve (AUROC) of 0.90 to 0.99 (Interquartile range, IQR, 0.91–0.94) in predicting different diseases in the independent test set, with a sensitivity of 0.81 to 0.95 (IQR, 0.87–0.93) at a specificity of 0.76 to 0.98 (IQR 0.83–0.95). Metagenomic analysis from public datasets of 1,597 samples across different populations observes comparable predictions with AUROC of 0.69 to 0.91 (IQR 0.79–0.87). Correlation of the top 50 microbial species with disease phenotypes identifies 363 significant associations (FDR < 0.05). This microbiome-based multi-disease model has potential clinical application in disease diagnostics and treatment response monitoring and warrants further exploration.
Similar content being viewed by others
Introduction
Recent studies have shown that imbalanced intestinal microbiota, termed “dysbiosis”, contributes to various human diseases1. The current development of microbial markers has mostly used binary classifiers2,3,4,5. Emerging evidence, however, suggests that most health conditions exhibit overlapping gut microbiome signatures6, thus single-disease diagnostic models are likely to be confounded by unrelated diseases and may lead to misclassification. Although an attempt has been made to develop a multi-class diagnostic model, heterogeneity, technical bias and batch effects involved in the previous work relying on public datasets for analyses would limit accuracy7. Here, we develop the largest single-site dataset to date covering multiple diseases, adopt a machine learning multi-class model to predict different diseases using species-level faecal microbiome profiling, and validate the findings using public metagenome datasets across different populations.
Results
We performed metagenomic sequencing of faecal samples from 2320 Hong Kong Chinese (mean age 54.9, 48.7% female, Source Data, Supplementary Fig. 1a, see the “Methods” section) consisting of 9 well-characterised disease phenotypes: colorectal cancer (CRC, n = 174), colorectal adenomas (CA, n = 168), Crohn’s disease (CD, n = 200), ulcerative colitis (UC, n = 147), irritable bowel syndrome (diarrhoea subtype, IBS-D, n = 145), obesity (n = 148), cardiovascular disease (CVD, n = 143), post-acute COVID-19 syndrome (PACS, n = 302) and healthy controls (n = 893). In total, we obtained 14.3 terabytes of the sequence at an average depth of 6.15 gigabases for each metagenome and identified 1208 bacterial species. Amongst them, 325 bacterial species had a relative abundance higher than 0.15% and these species were present in over 5% of the subjects (Source Data).
Shared microbiome signatures across different phenotypes
We observed differences in bacterial diversity (Shannon) and richness (number of species) in different diseases, and we found that both indices vary across phenotypes (Source Data, Supplementary Fig. 1b, c). These results are consistent with a recent meta-analysis8, indicating that ecological indices may not be robust indicators of health or disease. Then, we explored associations of microbial composition at the species level with disease phenotypes using a linear model of MaAsLin2 after adjusting for biological and technical confounders (see the “Methods” section). We found a total of 1061 significant associations between these nine phenotypes and 215 bacterial taxa at the species level (FDR < 0.05). Amongst the 215 species, more than 94% were significantly associated with two or more diseases, which is consistent with previous works that numerous signals are shared among different diseases6,9 (Source Data, Supplementary Fig. 1d). For instance, Klebsiella pneumoniae, a well-characterised opportunistic pathogen10, was positively associated with CD, CRC, IBS-D, Obesity, PACS and UC in our cohort, whilst Roseburia intestinalis, a promising probiotic with butyrate-producing properties11, negatively correlated with these six disease phenotypes (Source Data, Supplementary Fig. 1d). Next, we found that both PCoA analysis based on beta-diversity and random forest (RF) binary classifier could significantly separate all disease phenotypes (Source Data, Supplementary Table 1, Supplementary Fig. 2a–c, all p < 0.001). Whilst common microbial signatures were shared across diseases, these findings pointed to the presence of disease-specific microbial composition. However, it is unknown whether binary classifiers can capture these disease-specific signatures. Therefore, we tested the specificity of our trained binary models in unrelated diseases, and the results showed a high misdiagnosis rate (average 0.52, IQR 0.41–0.65, Source Data, Supplementary Fig. 2d). These results suggested that the binary classifier failed to capture real disease-specific features based solely on single disease versus control samples.
Development of faecal microbiome-based multi-class diagnosis model
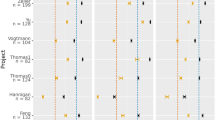
Classification tasks in machine learning involving more than two classes are known as “multi-class classification”, which can effectively account for confounding effects of unrelated classes12. Based on our cohort of 2320 Hong Kong Chinese, we trained five machine learning multi-class classifiers (RF, K-nearest neighbours (KNN), multi-layer perceptron (MLP), support vector machine (SVM), and graph convolutional neural network (GCN)) to classify different diseases using species-level data from the training set (70% samples with the same class proportions as the cohort) and presented their final performance from the withheld test set (30% samples, Fig. 1a, see the “Methods” section). All these models achieved a mean AUROC of 0.67–0.99 (Interquartile range, IQR 0.81–0.92), suggesting that multi-class disease classification based on the faecal microbiome was feasible (Source Data, Supplementary Fig. 3). Amongst them, the RF multi-class model achieved a mean AUROC of 0.90–0.99 (IQR 0.91–0.94, one versus all others, Fig. 1b) for different disease phenotypes in the test set. The performance of the RF model in the test set significantly outperformed all other models (Source Data, Supplementary Fig. 3b) and was similar to that of the training set (calculated by 5-fold cross-validation, Source Data, Supplementary Fig. 3c), suggesting high integrity of this classifier. Therefore, the RF multi-class model was used for further analyses. At a threshold based on the highest Youden’s Index, the sensitivities of our RF multi-class classifier ranged from 0.81 to 0.95 (IQR 0.87–0.93) at specificities of 0.76 to 0.98 (IQR 0.83–0.95) for different diseases with accuracy from 0.77 to 0.98 (IQR 0.82–0.92, one versus all others, Fig. 1c), highlighting good diagnostic performance. For example, our classifier achieved a mean AUROC of 0.94 for CRC with a sensitivity of 0.88 at a specificity of 0.85 (accuracy 0.85, one versus all others, Fig. 1b, c); this performance was superior to that of our trained binary classifier (CRC versus health, mean AUROC 0.91, Source Data, Supplementary Fig. 2c) and a previously published CRC diagnostic model2. Further assessment using predicted probabilities in the test set showed that the trained classifier achieved a mean AUROC of 0.94 for all one versus one classifications (IQR 0.92–0.98, Source Data, Supplementary Fig. 4a) with high sensitivities (IQR 0.88–0.95) and specificities (IQR 0.83–0.94, Source Data, Supplementary Fig. 4b), which supported a superior performance of multi-class model analyses over binary models (Source Data, Supplementary Fig. 2c).
a Framework for dataset partition, model training and independent validation. b Area under the receiver operating characteristic curve (AUROC, centre for the error bands is median). c Performance metric details of the trained random forest multi-class classifier for classifying one phenotype from all others using species-level faecal microbiome data in the independent test set. SVM support vector machine, KNN K-nearest neighbours, RF random forests; MLP multi-layer perceptron, GCN graph convolutional neural network, CA colorectal adenomas, CD Crohn’s disease, CRC colorectal cancer, CVD cardiovascular disease, IBS-D diarrhoea-dominant irritable bowel syndrome, PACS post-acute COVID-19 syndrome, UC ulcerative colitis. Source data are provided as a Source Data file.
To fully characterise the RF multi-class model, we compared its performance under different split ratios and achieved similar results, suggesting high stability and good predictive power without risk of overfitting (Source Data, Supplementary Fig. 3d). Given that subjects with CRC or colorectal adenomas were older than other subjects (Source Data, Supplementary Fig. 1a), we assessed our model stratified by age and found consistent performance (Source Data, Supplementary Fig. 5). In addition, our model achieved a mean AUROC of 0.87 in distinguishing CRC and colorectal adenomas (Source Data, Supplementary Fig. 4), which supported that effect of age on the model was likely to be negligible. To rule out the possibility that uneven cohort sizes across different diseases may influence the classification performance, we trained a separate RF multi-class classifier by randomly pooling 143 subjects from each disease phenotype (a total of 1287 subjects, 70% training, 30% testing) and found an AUROC of 0.83–0.99 (one versus all others, IQR 0.89–0.96; one versus one, IQR 0.89–0.97; Source Data, Supplementary Fig. 6) which was comparable to the AUROC of 0.90–0.99 in the 2,320 individuals (one versus all others, IQR 0.91–0.94; one versus one, IQR 0.92–0.98; Fig. 1b, Source Data, Supplementary Fig. 4). Importantly, the AUROC values of the model increased with the increasing number of features which suggested again that overfitting based on the 325 selected features was unlikely (Source Data, Supplementary Fig. 7).
Validation of multi-class model on independent datasets
Then, we integrated 1597 shotgun faecal metagenome data from 12 public datasets from Asia, Europe and North America (Source Data, Supplementary Table 2, Supplementary Fig. 8a). Our RF multi-class classifier showed a mean AUROC of 0.69–0.91 (IQR 0.79–0.87, Source Data, Supplementary Table 3) in classifying different diseases, and generally outperformed all other models (Source Data, Supplementary Fig. 8b). Such performance from an independent validation cohort further confirmed the robustness and generalisability of our model across different populations and geographical locations. To further validate the accuracy of our model, we selected 60 patients who had a complete recovery from COVID-19 infection. Our trained model showed an accuracy of 83.3% (50/60) in classifying these subjects as healthy (Source Data, Supplementary Fig. 8c). These data verified that fully recovered COVID-19 survivors (and without PACS) shared similar gut microbiome profiles as healthy people13. Additionally, we also tested our trained RF model on diseases not included in our training dataset, including liver cirrhosis and constipation-dominant IBS datasets (n = 60, see the “Methods” section). We found that using our RF multi-class model there were high probabilities whereby prediction cannot be made as they failed the corresponding threshold for most subjects (48/60, Source Data, Supplementary Fig. 8d), and they might be categorised as undetermined. And, the misclassification rate for each phenotype is from 0% (0/60, CA, CVD, IBS-D, Obesity) to 5% (3/60, CD, CRC, PACS, Source Data, Supplementary Fig. 9d), suggesting that our model has a high specificity and accuracy for the nine phenotypes within our cohort with a low risk of misclassification for unrelated diseases.
Associations between bacterial features and phenotypes
Next, we correlated the top 50 bacterial species contributing to the model (Source Data, Supplementary Table 4) with different disease phenotypes to identify clues to model interpretability. These top 50 bacterial species achieved a mean AUROC of 0.88 to 0.99 (IQR 0.90–0.93, Source Data, Supplementary Fig. 9a) for different diseases in our test set, and a mean AUROC of 0.67 to 0.90 (IQR 0.78–0.86, Source Data, Supplementary Fig. 9b) in the public dataset. A total of 363 significant associations were found between these 50 species with different disease phenotypes (Hong Kong cohort, FDR < 0.05, Fig. 2). Compared with healthy controls, almost all disease states were associated with a significantly decreased abundance of microbiota from the bacteria phylum of Firmicutes or Actinobacteria (FDR < 0.05) and a significant increase in Bacteroidetes (FDR < 0.05). Imbalance in Firmicutes/Bacteroidetes ratio had previously been reported primarily in patients with obesity and IBD14, but its associations with other diseases have not been reported. Nonetheless, such shared microbial signatures may serve as a basis for distinguishing health and disease. Then, we identified specific microbial signatures that can classify different diseases (Fig. 2). Specifically, the abundance of several bacterial species in Bacteroidetes differed significantly between patients with PACS, UC and CD. Subjects with PACS showed a significant increase in abundance of Bacteroides vulgatus and Bacteroides xylanisolvens, while those with UC were enriched in Bacteroides ovatus, and subjects with CD showed significant decreases in Bacteroides uniformis, Bacteroides vulgatus and Bacteroides xylanisolvens, compared with healthy controls. Although patients with CRC and colorectal adenomas shared relatively similar gut bacteria composition, the abundance of Parvimonas micra was significantly higher in patients with CRC but not colorectal adenomas, compared to healthy controls, which was consistent with previous findings showing that Parvimonas micra can be used as a marker to distinguish CRC from colorectal adenomas15,16. For other diseases, microbiome differences were mainly driven by Actinobacteria. Subjects with obesity showed increases in Actinomyces naeslundii, Actinomyces odontolyticus and Actinomyces oris, and subjects with IBS-D showed increases in Collinsella aerofaciens and Collinsella stercoris. We further correlated bacteria and phenotypes in the assembled public dataset, and found that many disease-specific biomarker are stable across datasets, such as Bacteroides for UC, Parvimonas micra for CRC and Actinomyces for obesity (Source Data, Supplementary Fig. 9c). Overall, these results suggest that our model can capture various disease-specific microbial signatures, which may explain the robust diagnostic performance of this multi-class classifier.
The top 50 microbial species contributing to the random forest multi-class classifier were clustered by taxonomy, and different phenotypes were clustered using hierarchical clustering. Associations were coloured by direction of effect (red, positive; blue, negative; p < 0.05), with associations significant at FDR < 0.05 marked with a plus (positive correlations) or minus (negative correlations), respectively. The nominal significance (p-value) of associations was calculated by MaAsLin 2, and the false discovery rate (FDR) was computed by Benjamini–Hochberg correction. CA colorectal adenomas, CD Crohn’s disease, CRC colorectal cancer, CVD cardiovascular disease, IBS-D diarrhoea-dominant irritable bowel syndrome, PACS post-acute COVID-19 syndrome, UC ulcerative colitis. Source data are provided as a Source Data file.
Discussion
Overall, our data showed that the faecal microbiome-based multi-class model for disease diagnosis is feasible. The novelty lies in the high-quality dataset, and superior and reproducible machine-learning methods which are of high clinical relevance. We believe this multi-class model of classifying diseases has potential clinical applications and can serve as a non-invasive way of screening various diseases in clinical practice or for disease risk assessment. Our results also have implications for the potential development of biomarkers for predicting drug response and common treatment strategies using the identified shared or specific marker for multiple diseases. This work has some limitations. Firstly, the disease spectrum of this study is still limited, and the inclusion of more phenotypes can further enhance the value of this multi-class diagnostic tool. Secondly, biological evidence to support the identified microbiome–phenotype associations is limited and future work to delineate the mechanisms of these associations is needed to facilitate our understanding of the role of the shared and disease-specific microbiome in disease pathogenesis. Also, the pooled public dataset did not specify co-morbidities and antibiotic use, thus model performance may vary upon the exclusion of these subjects. Since our model predicts probabilities for multiple diseases simultaneously, it may also apply to multi-disease diagnosis in a single patient. Though we could not validate it at this moment, this hypothesis should be tested in the future.
To our knowledge, we present the largest faecal microbiome datasets with different disease phenotypes and developed a machine learning multi-class model that achieved high performance for disease classification. This non-invasive microbiome-based model could potentially be applied clinically to complement disease diagnostics and treatment response monitoring.
Methods
Ethics statement
The study was approved by The Joint Chinese University of Hong Kong – New Territories East Cluster Clinical Research Ethics Committee (The Joint CUHK-NTEC CREC). All subjects provided written informed consent.
Study population
All participants were recruited and diagnosed at the Prince of Wales Hospital in Hong Kong from January 2017 to March 2022. Subjects with CRC and CA were diagnosed by colonoscopy and confirmed on histology examinations; Subjects with CD and UC were diagnosed based on standard criteria of endoscopy, radiology, and histological examinations. Subjects with IBS were diagnosed according to the ROME III criteria, and endoscopy and enteroscopy were performed to exclude other GI disorders such as IBD, coeliac disease, parasite infestations, or other organic disorders. Obesity was defined as subjects with a body mass index (BMI) of over 28 and with no other medical co-morbidities. Subjects with cardiovascular disease (CVD) were recruited from the public as part of a survey of cardiovascular health in the Hong Kong general population. Subjects underwent carotid ultrasounds to measure intima-media thickness (IMT) of the common, internal, and external carotid arteries (CCA, ICA and ECA, respectively) and carotid bulbs and subjects that had ≥50% stenosis in a single or multiple vessels were regarded as having the risk of CVD. Subjects with post-acute covid-19 syndrome (PACS) were defined as those with at least one persistent symptom or long-term complications of SARS-CoV-2 infection beyond 4 weeks from the viral clearance which could not be explained by an alternative diagnosis, and we assessed the presence of the 30 most commonly reported symptoms post-COVID after illness onset13,17 (Source Data, Supplementary Table 5). All subjects with other diseases (apart from the obesity group) had a normal range of BMI of 18.5–22.9. All subjects are on a stable traditional Chinese style diet and are of Han Chinese ethnicity. Patients were excluded if they had the following: age under 18 or over 80; self-reported comorbidities of other diseases; infection with an enteric pathogen; acquired immunodeficiency syndrome; known history of organ dysfunction or failure and abdominal surgery; active malignancy or undergoing radio-chemotherapy; short bowel syndrome; taking drugs commonly known to affect the gut microbiome including proton pump inhibitors, oral anti-diabetics, non-steroidal anti-inflammatory drugs, corticosteroids, laxatives or selective serotonin reactive inhibitors and antibiotics or probiotics use within three months of sample collection; pregnant or breastfeeding; on special diets such as vegetarians.
Healthy controls were recruited during the same recruitment period from the community through advertisement and from the endoscopy centre at the Prince of Wales Hospital and included subjects who had a normal colonoscopy (faecal samples collected before bowel preparation). The exclusion criteria for healthy controls were known complex infections or sepsis; known history of severe organ failure (including decompensated cirrhosis, malignant disease, kidney failure, epilepsy, active serious infection, acquired immunodeficiency syndrome); bowel surgery in the last 6 months (excluding colonoscopy/procedure related to perianal disease); the presence of an ileostomy/stoma; and current pregnancy; any long term drugs for chronic diseases; the use of antibiotics in the last 3 months; the use of laxatives or anti-diarrhoeal drugs in the last 3 months or recent dietary changes (e.g., becoming vegetarian/vegan). Finally, a total of 2320 subjects were recruited. Clinical metadata and dietary data were collected during clinical interviews. Besides, an additional 60 subjects (mean age 53.5, 48.3% female) were prospectively followed up for up to two years after the COVID-19 infection and were confirmed to have fully recovered from the initial infection without any symptoms of PACS. These subjects served as an independent validation cohort and provided serial faecal samples after SARS-CoV-2 clearance.
Faecal samples
Faecal samples were collected at home by all subjects using tubes prepared by investigators containing preservative media (cat. 63700, Norgen Biotek Corp, Ontario Canada). The Norgen preservative can preserve and allow safe transportation of microbial DNA & RNA at ambient temperature eliminating sample variability. The stool sample was sent to the hospital within 24 h of collection and stored at −80 °C refrigerators until further processing. We have previously shown that data on gut microbiota composition generated from faecal samples collected using this preservative medium was comparable to data obtained from fresh samples that were immediately stored at −80 °C18.
Faecal DNA extraction and sequencing
After removing the preservative media, microbial DNA was isolated with the Qiagen (Hilden, Germany) QIAamp DNA Stool Mini Kit, according to the manufacturer’s instructions. After the quality control procedures by Qubit 2.0, agarose gel electrophoresis, and Agilent 2100, extracted DNA was subject to DNA libraries construction, completed through the processes of end repairing, adding A to tails, purification and PCR amplification, using Nextera DNA Flex Library Preparation kit (Illumina, San Diego, CA). Libraries were subsequently sequenced on our in-house sequencer Illumina NextSeq 550 (150 base pairs paired-end) at the Center for Microbiota Research, The Chinese University of Hong Kong. All samples were in random order for DNA extraction, library construction and sequencing. ZymoBIOMICS Spike-in Control I (High Microbial Load, Cat: D6320-10, ZYMO Research, USA) and ZymoBIOMICS Microbial Community DNA Standard (Cat: D6306-A) were used as positive controls during DNA extraction, library construction, sequencing and quality assessment.
Microbiome profiling
Raw sequence data were quality filtered using Trimmomatic V.39 to remove the adaptor, low-quality sequences (quality score < 20), and reads shorter than 50 base pairs. Contaminating human reads were filtered using Kneaddata (V.0.10.0, Reference database: GRCh38 p12) with default parameters. Following this, microbiota composition profiles were inferred from quality-filtered forward reads using MetaPhlAn3 version 3.0.14. GNU parallel (v2018) was used for parallel analysis jobs to accelerate data processing. Species whose average abundance and prevalence were <0.15% and 5% were filtered out. Alpha diversity metrics (Shannon diversity, Chao1 richness) were calculated by using the phyloseq package (v1.26.0).
Microbiome analysis
All statistical analyses were done using R version 4.0.3. The ggpubr package (https://github.com/kassambara/ggpubr) performed nonparametric statistical testing between groups and accounted for multiple hypothesis testing corrections when necessary. Principal coordinates analysis (PCoA) based on beta-diversity (Bray–Curtis distance matrix calculated using relative abundances of microbial species) was used to visualise the clustering of samples based on their species-level compositional profiles. The microbiome composition differences between different phenotypes were calculated by permutational multivariate analysis of variance (PERMANOVA) using distance matrices (adonis) in the adonis function of vegan R package V.2.5–7 with 999 permutations. Associations of specific microbial species with phenotypes were identified using the multivariate analysis by linear models (MaAsLin2) statistical frameworks implemented in the Huttenhower Lab Galaxy instance (http://huttenhower.sph.harvard.edu/galaxy/) with healthy controls as reference. The linear model also included age, sex and technical factors (library DNA concentration, sequencing read depth, sequencing batch) to further correct for potential batch effects and confounders. BMI was not included as apart from the obese group, all subjects from other disease groups had a normal BMI requirement (18.5–22.9) and there was no difference in the BMI across different phenotypes. Benjamini–Hochberg correction was used to control for multiple testing, and results were considered significant at false discovery rate (FDR) < 0.05.
Random Forest binary classifier
To account for sequencing batch effects for all samples processed in different periods, we performed Combat by SVA package (v3.44.0)19 for relative abundance before machine learning model development. Binary sub-cohorts were composed of two phenotypes drawn from the entire cohort. A total of 36 binary sub-cohorts were generated, covering all cross-comparisons of different phenotypes. Machine learning binary classifier used random forest through the Sklearn20 library under Python 3.6.7, as this algorithm has been shown to outperform, on average, other learning tools for microbiota data5. Normalised abundance table from each binary sub-cohort to train the model. Machine learning models were first trained on the randomly selected training set (70%, 20-times repeated, fivefold-stratified cross-validation) and then were applied to the withheld validation set (30%) to access the final performance. This process was repeated 20 times to obtain a distribution of random forest prediction evaluations on the validation set, and the mean AUROC value was calculated accordingly for the visualisation of and reporting of results.
Machine learning for diagnosis of multi-diseases
Multi-class models are implemented by Python 3.6.7 using standard libraries that are publicly available: pandas (0.23.4), numpy (1.14.5), scikit-learn (1.1), and matplotlib (2.2.3). For each phenotype, samples were randomly divided into a training set (70% of samples, total n = 1724) and a test set for independent evaluation (remaining 30%, total n = 696) with balancing class proportions across the cohort, training set and test set. Random forests (RF), K-nearest neighbours (KNN), SVM multi-layer perceptron (MLP) and support vector machine (SVM) were used as classifier models for the diagnosis of different phenotypes by using taxonomic profiles at the species level of the faecal microbiome. We implemented the RF multi-class classifier with the following modifications to the default SciKit-learn settings: n_estimaters = 2000 and class_weight = balanced. KNN, SVM and MLP were implemented from SciKit-learn with the default settings. Besides, we reconstructed a graph convolutional neural network (GCN) model based on a published work with the same parameter settings7. A nested cross-validation procedure was applied to calculate within-training set accuracy by splitting data into training and test sets for 20-times repeated, fivefold-stratified cross-validation (balancing class proportions across folds). The optimal models selected based on cross-validated results were evaluated in the withheld evaluation dataset as the final performance for predicting different diseases. This process was repeated 20 times to obtain a distribution of random forest prediction evaluations on the validation set, and the mean AUROC and AUPR value was calculated accordingly for the visualisation of results. The highly ranked and frequently selected microbial features were considered predictive signatures for further interpretation. We retrieved prediction performance using the same training datasets.
Model evaluation
We included AUROC to characterise the model performance as our models initially provided outputs of probabilities for each disease phenotype, and these predicted probabilities were then used to estimate the risk of disease occurrence or absence, which formed a binary status that was analysed to provide an AUROC value. The AUROC is a widely applied metric that considers the trade-offs between sensitivity and specificity at all possible thresholds for comparing the performance across various classifiers with a baseline value of 0.5 for a random classifier. AUPR was provided as a complimentary assessment, which considers the trade-offs between precision (or positive predictive value) and recall (or sensitivity) with a baseline that equals the proportion of positive disease cases in all samples.
Public data download and processing
For the construction of the external dataset, a total of 1,597 raw shotgun faecal metagenomes were acquired from 12 independently published studies across 11 countries (114 for UC21,22,23, 102 for CD22,23,24, 218 for CVD25, 177 for CRC26,27,28, 86 for adenoma27,28, 83 for IBS-D29,30,31, 81 for Obesity32, and corresponding 736 health controls). Besides, a total of 60 raw shotgun faecal metagenomes from subjects with liver cirrhosis33 (n = 38, validation cohort from Qin et al.33) or constipation-dominant IBS31 (IBS-C, n = 22) were downloaded to construct an unrelated disease dataset. After downloading, the quality filtration and species-level taxonomic profiling were performed according to the above process.
Statistics and reproducibility
No statistical method was used to predetermine the sample size. Instead, the study focused on obtaining the largest possible sample size to capture the highest performance of the machine learning multi-class model. 2,320 samples were all successfully sequenced and passed the quality assessment (read depth > 10 million), thus no data were excluded from the analyses. For the machine learning multi-class model, a nested cross-validation procedure was applied to calculate within-training set accuracy by splitting data into training and test sets for 20-times repeated, fivefold-stratified cross-validation (balancing class proportions across folds). The optimal models selected based on cross-validated results were evaluated in the withheld evaluation dataset as the final performance for predicting different diseases. This process was repeated 20 times to obtain a distribution of random forest prediction evaluations on the validation set, and the mean AUROC and AUPR value was calculated accordingly for the visualisation of results. For each phenotype, samples were randomly divided into a training set (70% of samples, total n = 1724) and a test set for independent evaluation (remaining 30%, total n = 696). Within the training set, a nested cross-validation procedure was applied to calculate within-training set accuracy by randomly splitting data into training and test sets for 20-times repeated, fivefold-stratified cross-validation (balancing class proportions across folds). The study did not include any interventions and thus the conventional blinding (as used in clinical trials or intervention studies) was not relevant to this study.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The raw metagenomes generated in this study have been deposited in the NCBI Sequence Read Archive database under accession code PRJNA841786. The public available raw sequencing data were downloaded through the NCBI Sequence Read Archive using the retrieved accession numbers from cited papers, including DRA006684, DRA008156, ERP008729, ERP005534, ERP023788, ERP021923, PRJEB36140, PRJEB37924, PRJEB33500, PRJNA400072, PRJEB1220, PRJNA429990, PRJEB1220, PRJNA429990, PRJEB15371, and PRJEB6337. The reference database GRCh38.p12 was downloaded from https://www.ncbi.nlm.nih.gov/assembly/GCF_000001405.38. Source data are provided with this paper.
Code availability
Codes and scripts developed in this study are all available at the GitHub repository (https://github.com/qsu123/multi_class_diagnosis34).
References
Lynch, S. V. & Pedersen, O. The human intestinal microbiome in health and disease. N. Engl. J. Med. 375, 2369–2379 (2016).
Liang, J. Q. et al. A novel faecal Lachnoclostridium marker for the non-invasive diagnosis of colorectal adenoma and cancer. Gut 69, 1248–1257 (2020).
Vila, A. V. et al. Gut microbiota composition and functional changes in inflammatory bowel disease and irritable bowel syndrome. Sci. Transl. Med. 10, eaap8914 (2018).
Shaukat, A. & Levin, T. R. Current and future colorectal cancer screening strategies. Nat. Rev. Gastroenterol. Hepatol. 19, 521–531 (2022).
Pasolli, E., Truong, D. T., Malik, F., Waldron, L. & Segata, N. Machine learning meta-analysis of large metagenomic datasets: tools and biological insights. PLoS Comput. Biol. 12, e1004977 (2016).
Gacesa, R. et al. Environmental factors shaping the gut microbiome in a Dutch population. Nature 604, 732–739 (2022).
Saad Khan, L. K. Multiclass disease classification from microbial wholecommunity metagenomes. Pac. Symp. Biocomput. 25, 55–66 (2020).
Gupta, V. K. et al. A predictive index for health status using species-level gut microbiome profiling. Nat. Commun. 11, 4635 (2020).
Duvallet, C., Gibbons, S. M., Gurry, T., Irizarry, R. A. & Alm, E. J. Meta-analysis of gut microbiome studies identifies disease-specific and shared responses. Nat. Commun. 8, 1784 (2017).
Wyres, K. L., Lam, M. M. C. & Holt, K. E. Population genomics of Klebsiella pneumoniae. Nat. Rev. Microbiol. 18, 344–359 (2020).
Nie, K. et al. Roseburia intestinalis: a beneficial gut organism from the discoveries in genus and species. Front. Cell. Infect. Microbiol. 11, 757718 (2021).
Grandini, M., E. Bagli, E. & Visani, G. Metrics for multi-class classification: an overview. Preprint at arXiv.2008.05756 (2020).
Liu, Q. et al. Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut 71, 544–552 (2022).
Stojanov, S., Berlec, A. & Štrukelj, B. The influence of probiotics on the Firmicutes/Bacteroidetes ratio in the treatment of obesity and inflammatory bowel disease. Microorganisms 8, 1715 (2020).
Xu, J. et al. Alteration of the abundance of Parvimonas micra in the gut along the adenoma-carcinoma sequence. Oncol. Lett. 20, 106 (2020).
Lowenmark, T. et al. Parvimonas micra as a putative non-invasive faecal biomarker for colorectal cancer. Sci. Rep. 10, 15250 (2020).
Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. 27, 601–615 (2021).
Chen, Z. et al. Impact of preservation method and 16S rRNA hypervariable region on gut microbiota profiling. mSystems 4, e00271–00218 (2019).
Chen, C. et al. Removing batch effects in analysis of expression microarray data: an evaluation of six batch adjustment methods. PLoS ONE 6, e17238 (2011).
Pedregosa, F. et al. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
Franzosa, E. A. et al. Gut microbiome structure and metabolic activity in inflammatory bowel disease. Nat. Microbiol. 4, 293–305 (2019).
Nielsen, H. B. et al. Identification and assembly of genomes and genetic elements in complex metagenomic samples without using reference genomes. Nat. Biotechnol. 32, 822–828 (2014).
Weng, Y. J. et al. Correlation of diet, microbiota and metabolite networks in inflammatory bowel disease. J. Dig. Dis. 20, 447–459 (2019).
He, Q. et al. Two distinct metacommunities characterize the gut microbiota in Crohn’s disease patients. Gigascience 6, 1–11 (2017).
Jie, Z. et al. The gut microbiome in atherosclerotic cardiovascular disease. Nat. Commun. 8, 845 (2017).
Yachida, S. et al. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat. Med. 25, 968–976 (2019).
Feng, Q. et al. Gut microbiome development along the colorectal adenoma-carcinoma sequence. Nat. Commun. 6, 6528 (2015).
Zeller, G. et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol. Syst. Biol. 10, 766 (2014).
Vervier, K. et al. Two microbiota subtypes identified in irritable bowel syndrome with distinct responses to the low FODMAP diet. Gut. 71, 1821–1830 (2022).
Goll, R. et al. Effects of fecal microbiota transplantation in subjects with irritable bowel syndrome are mirrored by changes in gut microbiome. Gut Microbes 12, 1794263 (2020).
Mars, R. A. T. et al. Longitudinal multi-omics reveals subset-specific mechanisms underlying irritable Bowel syndrome. Cell 182, 1460–1473 e1417 (2020).
Meslier, V. et al. Mediterranean diet intervention in overweight and obese subjects lowers plasma cholesterol and causes changes in the gut microbiome and metabolome independently of energy intake. Gut 69, 1258–1268 (2020).
Qin, N. et al. Alterations of the human gut microbiome in liver cirrhosis. Nature 513, 59–64 (2014).
Su, Q. Faecal microbiome-based machine learning for multi-class disease diagnosis. Github https://doi.org/10.5281/zenodo.7193183 (2022).
Acknowledgements
We thank Gabriel Lee for manuscript proofreading. We thank Anki Miu, Bonaventure YM Ip, Joyce Wing Yan Mak, Paul KS Chan and other clinical research staff/students for their technical contribution to this study, including clinical data and sample collection, inventory and processing. This research has been conducted using the CU-Med Biobank Resource under Request ID ‘R20221008’. Q.S., Q.L., J.Z., Z.X., Y.K.Y., W.T., L.Z., Y.K.Y., C.L., M.Z., C.P.C., H.M.T., F.K.L.C. and S.C.N are partially or fully supported by InnoHK, The Government of Hong Kong, Special Administrative Region of the People’s Republic of China. S.C.N. is also supported by the Croucher Senior Medical Research Fellowship. R.I.L. received additional support from the Hong Kong Ph.D. Fellowship Scheme (HKPFS).
Author information
Authors and Affiliations
Contributions
Q.S. and Q.L. conceived the study, developed algorithms, ran analyses and took responsibility for the integrity of the data and preparation of the manuscript. R.I.L., J.W.Z., Z.X., Y.K.Y, W.T, L.Z, J.Q.L. contributed to part of the data analysis. Y.K.Y., J.YZ., C.L., M.Z. contributed to metagenomic sequencing. J.Y.Z. .contributed to publicly available data management. J.Y.L.C., TWHL, C.P.C. contributed to participant recruitment, sample collection and biobank management. H.M.T., J.Y. and F.K.L.C. contributed to the study design and data interpretation. S.C.N. contributed to the study design, data analysis and manuscript writing. All authors gave final approval for the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The Chinese University of Hong Kong has filed a provisional patent application in connection with this work on which S.C.N., F.K.L.C., S.Q. and Q.L. are inventors. F.K.L.C. and S.C.N. are the scientific co-founders and sit on the board of Directors of GenieBiome Ltd. S.C.N. has served as an advisory board member for Pfizer, Ferring, Janssen, and Abbvie and a speaker for Ferring, Tillotts, Menarini, Janssen, Abbvie, and Takeda. She has received research grants from Olympus, Ferring, and Abbvie. F.K.L.C. has served as an advisor and lecture speaker for Eisai Co. Ltd., AstraZeneca, Pfizer Inc., Takeda Pharmaceutical Co., and Takeda (China) Holdings Co. Ltd. ZX, W.T., J.Q.Y.L. are part-time employee of GenieBiome Ltd. All other co-authors have no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Su, Q., Liu, Q., Lau, R.I. et al. Faecal microbiome-based machine learning for multi-class disease diagnosis. Nat Commun 13, 6818 (2022). https://doi.org/10.1038/s41467-022-34405-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-022-34405-3
This article is cited by
-
Gut microbiome for predicting immune checkpoint blockade-associated adverse events
Genome Medicine (2024)
-
A novel infant microbiome formula (SIM03) improved eczema severity and quality of life in preschool children
Scientific Reports (2024)
-
The long-term health outcomes, pathophysiological mechanisms and multidisciplinary management of long COVID
Signal Transduction and Targeted Therapy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.