Abstract
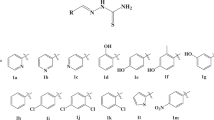
Carbapenems are vital antibiotics, but their efficacy is increasingly compromised by metallo-β-lactamases (MBLs). Here we report the discovery and optimization of potent broad-spectrum MBL inhibitors. A high-throughput screen for NDM-1 inhibitors identified indole-2-carboxylates (InCs) as potential β-lactamase stable β-lactam mimics. Subsequent structure–activity relationship studies revealed InCs as a new class of potent MBL inhibitor, active against all MBL classes of major clinical relevance. Crystallographic studies revealed a binding mode of the InCs to MBLs that, in some regards, mimics that predicted for intact carbapenems, including with respect to maintenance of the Zn(II)-bound hydroxyl, and in other regards mimics binding observed in MBL–carbapenem product complexes. InCs restore carbapenem activity against multiple drug-resistant Gram-negative bacteria and have a low frequency of resistance. InCs also have a good in vivo safety profile, and when combined with meropenem show a strong in vivo efficacy in peritonitis and thigh mouse infection models.

This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Livermore, D. M. et al. CTX-M: changing the face of ESBLs in Europe. J. Antimicrob. Chemother. 59, 165–174 (2007).
Kumarasamy, K. K. et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect. Dis. 10, 597–602 (2010).
Liu, Y. Y. et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect. Dis. 16, 161–168 (2016).
He, T. et al. Emergence of plasmid-mediated high-level tigecycline resistance genes in animals and humans. Nat. Microbiol. 4, 1450–1456 (2019).
Yahav, D. et al. New β-lactam-β-lactamase inhibitor combinations. Clin. Microbiol. Rev. 34, e00115-20 (2020).
Bush, K. Past and present perspectives on β-lactamases. Antimicrob. Agents Chemother. 62, e01076-18 (2018).
Rotondo, C. M. & Wright, G. D. Inhibitors of metallo-β-lactamases. Curr. Opin. Microbiol. 39, 96–105 (2017).
Bonomo, R. A. et al. Carbapenemase-producing organisms: a global scourge. Clin. Infect. Dis. 66, 1290–1297 (2018).
Wang, D. Y., Abboud, M. I., Markoulides, M. S., Brem, J. & Schofield, C. J. The road to avibactam: the first clinically useful non-β-lactam working somewhat like a β-lactam. Future Med. Chem. 8, 1063–1084 (2016).
Ehmann, D. E. et al. Avibactam is a covalent, reversible, non-β-lactam β-lactamase inhibitor. Proc. Natl Acad. Sci. USA 109, 11663–11668 (2012).
Lomovskaya, O. et al. Vaborbactam: spectrum of β-lactamase inhibition and impact of resistance mechanisms on activity in Enterobacteriaceae. Antimicrob. Agents Chemother. 61, e01443-17 (2017).
Langley, G. W. et al. Profiling interactions of vaborbactam with metallo-β-lactamases. Bioorg. Med. Chem. Lett. 29, 1981–1984 (2019).
Papp-Wallace, K. M., Mack, A. R., Taracila, M. A. & Bonomo, R. A. Resistance to novel β-lactam-β-lactamase inhibitor combinations: the ‘price of progress’. Infect. Dis. Clin. North Am. 34, 773–819 (2020).
Lohans, C. T., Brem, J. & Schofield, C. J. New Delhi metallo-β-lactamase 1 catalyzes avibactam and aztreonam hydrolysis. Antimicrob. Agents Chemother. 61, e01224-17 (2017).
Meini, M. R., Llarrull, L. I. & Vila, A. J. Overcoming differences: the catalytic mechanism of metallo-β-lactamases. FEBS Lett. 589, 3419–3432 (2015).
Drawz, S. M. & Bonomo, R. A. Three decades of β-lactamase inhibitors. Clin. Microbiol. Rev. 23, 160–201 (2010).
Davies, D. T. et al. ANT2681: SAR studies leading to the identification of a metallo-β-lactamase inhibitor with potential for clinical use in combination with meropenem for the treatment of infections caused by NDM-producing Enterobacteriaceae. ACS Infect. Dis. 6, 2419–2430 (2020).
King, A. M. et al. Aspergillomarasmine A overcomes metallo-β-lactamase antibiotic resistance. Nature 510, 503–506 (2014).
Liu, B. et al. Discovery of taniborbactam (VNRX-5133): a broad-spectrum serine- and metallo-β-lactamase inhibitor for carbapenem-resistant bacterial infections. J. Med. Chem. 63, 2789–2801 (2020).
Bush, K. & Bradford, P. A. Epidemiology of β-lactamase-producing pathogens. Clin. Microbiol. Rev. 33, e00047-19 (2020).
Sauvage, E. & Terrak, M. Glycosyltransferases and transpeptidases/penicillin-binding proteins: valuable targets for new antibacterials. Antibiotics 5, 12 (2016).
Bush, K. & Bradford, P. A. Interplay between β-lactamases and new β-lactamase inhibitors. Nat. Rev. Microbiol. 17, 295–306 (2019).
Dik, D. A., Fisher, J. F. & Mobashery, S. Cell-wall recycling of the Gram-negative bacteria and the nexus to antibiotic resistance. Chem. Rev. 118, 5952–5984 (2018).
Tipper, D. J. & Strominger, J. L. Mechanism of action of penicillins: a proposal based on their structural similarity to acyl-d-alanyl-d-alanine. Proc. Natl Acad. Sci. USA 54, 1133–1141 (1965).
Karawajczyk, A., Orling, K. M., de Vlieger, J. S. B., Rijnders, T. & Tzalis, D. The European Lead Factory: a blueprint for public–private partnerships in early drug discovery. Front. Med. 3, 75 (2017).
Besnard, J., Jones, P. S., Hopkins, A. L. & Pannifer, A. D. The Joint European Compound Library: boosting precompetitive research. Drug Discov. Today 20, 181–186 (2015).
Yan, Y. H., Li, G. & Li, G. B. Principles and current strategies targeting metallo-β-lactamase mediated antibacterial resistance. Med. Res. Rev. 40, 1558–1592 (2020).
Ju, L. C., Cheng, Z., Fast, W., Bonomo, R. A. & Crowder, M. W. The continuing challenge of metallo-β-lactamase inhibition: mechanism matters. Trends Pharmacol. Sci. 39, 635–647 (2018).
Brem J., et al. Inhibitors of metallo-beta-lactamases. World Patent WO2017093727A1 (2017).
Lohans, C. T. et al. Mechanistic Insights into β-lactamase-catalysed carbapenem degradation through product characterisation. Sci. Rep. 9, 13608 (2019).
King, D. T., Worrall, L. J., Gruninger, R. & Strynadka, N. C. J. New Delhi metallo-β-lactamase: structural insights into β-lactam recognition and inhibition. J. Am. Chem. Soc. 134, 11362–11365 (2012).
Feng, H. et al. The mechanism of NDM-1-catalyzed carbapenem hydrolysis is distinct from that of penicillin or cephalosporin hydrolysis. Nat. Commun. 8, 2242 (2017).
Raczynska, J. E., Shabalin, I. G., Minor, W., Wlodawer, A. & Jaskolski, M. A close look onto structural models and primary ligands of metallo-β-lactamases. Drug Resist. Update 40, 1–12 (2018).
Cahill, S. T. et al. Studies on the inhibition of AmpC and other β-lactamases by cyclic boronates. Biochim. Biophys. Acta Gen. Subj. 1863, 742–748 (2019).
Jiménez-Castellanos, J.-C. et al. Envelope proteome changes driven by RamA overproduction in Klebsiella pneumoniae that enhance acquired β-lactam resistance. J. Antimic. Chemother. 73, 88–94 (2017).
Krajnc, A. et al. Bicyclic boronate VNRX-5133 inhibits metallo- and serine-β-lactamases. J. Med. Chem. 62, 8544–8556 (2019).
Lisa, M.-N. et al. A general reaction mechanism for carbapenem hydrolysis by mononuclear and binuclear metallo-β-lactamases. Nat. Comm. 8, 538 (2017).
Brem, J. et al. Structural basis of metallo-β-lactamase, serine-β-lactamase and penicillin-binding protein inhibition by cyclic boronates. Nat. Commun. 7, 12406 (2016).
Richter, M. F. et al. Predictive compound accumulation rules yield a broad-spectrum antibiotic. Nature 545, 299–304 (2017).
Galán, J.-C., Morosini, M.-I., Baquero, M.-R., Reig, M. & Baquero, F. Haemophilus influenzae bla(ROB-1) mutations in hypermutagenic ΔampC Escherichia coli conferring resistance to cefotaxime and β-lactamase inhibitors and increased susceptibility to cefaclor. Antimic. Agents Chemother. 47, 2551–2557 (2003).
Theuretzbacher, U. et al. Critical analysis of antibacterial agents in clinical development. Nat. Rev. Microbiol. 18, 286–298 (2020).
Mojica, M. F., Bonomo, R. A. & Fast, W. B1-metallo-β-lactamases: where do we stand? Curr. Drug Targets 17, 1029–1050 (2016).
Brem, J. et al. Structural basis of metallo-4-lactamase inhibition by captopril stereoisomers. Antimic. Agents Chemother. 60, 142–150 (2015).
Brem, J. et al. Rhodanine hydrolysis leads to potent thioenolate mediated metallo-β-lactamase inhibition. Nat. Chem. 6, 1084–1090 (2014).
Pettinati, I., Brem, J., Lee, S. Y., McHugh, P. J. & Schofield, C. J. The chemical biology of human metallo-β-lactamase fold proteins. Trends Biochem. Sci 41, 338–355 (2016).
Pallett, A. & Hand, K. Complicated urinary tract infections: practical solutions for the treatment of multiresistant Gram-negative bacteria. J. Antimicrob. Chemother. 65, iii25–iii33 (2010).
Acknowledgements
We thank the ELF Screening partners for efforts leading to the initial hits, the current and past ENABLE Portfolio Management Committee (PMC) members and EFPIA partners for guidance, and the Diamond Light Source synchrotron for access to the IO3, IO4 and IO4-1 beamlines. J.U.H. thanks N. Sipari from the Viikki Metabolomics Unit (Helsinki Institute of Life Science, University of Helsinki and Biocenter Finland) for her expertise with the liquid chromatography–mass spectroscopy analyses. L.E. thanks Y. Zhou for help in the laboratory, and H. Saif, R. Farzana, E. Portal, K. Sands, K. Thomson and B. Hassan for providing strains for the Enterobacterales collection. The ELF work and the ENABLE project that led to these results were supported by the Innovative Medicines Initiative Joint Undertaking (grant agreements no. 115489 and no. 115583), which have financial contributions from the European Union’s Seventh Framework Programme (FP7/2007–2013), and the EFPIA companies’ in-kind contributions. The ENABLE project is financially supported by contributions from Academic and SME partners. The Oxford work was also supported by Cancer Research UK (C9047/A24759), the Medical Research Council, the Biotechnology and Biological Research Council (BB/S50676X/1) and the Ineos Oxford Institute for Antimicrobial Research (C.J.S.). This research was funded in whole, or in part, by the Wellcome Trust (grant no. 106244/Z/14/Z and no. 099141/Z/12/Z). The Bristol work was also supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (NIH) grant R01AI100560 (J.S. and P.H.) (the content is the responsibility of the authors and does not necessarily represent official views of the NIH) and the BrisSynBio Biosuite (UK Biotechnology and Biological Sciences (BBSRC) and Engineering and Physical Sciences (EPSRC) Research Councils (BB/L01386X/1) and BBSRC ALERT14 initiative (BB/M012107/1).
Author information
Authors and Affiliations
Contributions
J.B., T.P., J.H., P.D., A.J.M.F., K.S., G.G.C., P.K., S.S., D.K., R.K.L., Juliane Schmidt (Adrian), D.L., A.G.B., J.R., L.R., A.M.R., S.D.S.P., A.D.P., M.M., M.P., A.K.B., Peter Brandt, J.Y.-K., E.B., M.G.P.P., Fredrik Björkling, P.S.J., E.S., A.M. and C.J.S. conducted the medicinal chemistry analysis and/or chemical synthesis. J.U.H., E.L., E.I.N., J.K. and S.G. led the safety and/or in vivo efficacy experiments. A.E., M.B. and Pawel Baranczewski led or conducted the physicochemical and ADME testing. L.E., M.-C.T., A.F.A., J.C.J.-C., E.W. and J.M.T. conducted the microbiological experiments under the guidance of M.B.A., M.G., R.C., Fernando Baquero, and T.R.W. K.C., M.E.K., G.W.L., M.S., A.M.R., I.H.N., P.A.L., S.P.M. and J.B. conducted the biochemical or biophysical testing. P.H., M.A.M., T.M.L., James Spencer and J.B. conducted the X-ray crystallography work and analysis. J.B. oversaw all the studies. J.B. and C.J.S. wrote the first draft of the manuscript with subsequent input from all the authors.
Corresponding authors
Ethics declarations
Competing interests
A patent has been filed concerning the indole carboxylates as MBL inhibitors (WO2017093727A1)29. The inventors may benefit financially from the work. The work described in the manuscript was carried out prior to these employments, which are not relevant to the work. G.W.L. is an employee of Charles River Laboratories, M.S., J.R., L.R., S.P.M., P.S.J. and A.M. are employees of BioAscent Discovery Ltd, A.M.R. is an employee of AstraZeneca and E.B. is an employee of Evotec.
Additional information
Peer review information Nature Chemistry thanks Hongzhe Sun and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–16, Tables 1–31 and Methods.
Rights and permissions
About this article
Cite this article
Brem, J., Panduwawala, T., Hansen, J.U. et al. Imitation of β-lactam binding enables broad-spectrum metallo-β-lactamase inhibitors. Nat. Chem. 14, 15–24 (2022). https://doi.org/10.1038/s41557-021-00831-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41557-021-00831-x
This article is cited by
-
Identification and characterization of CIM-1, a carbapenemase that adds to the family of resistance factors against last resort antibiotics
Communications Biology (2024)
-
Porin-independent accumulation in Pseudomonas enables antibiotic discovery
Nature (2023)
-
Structural insights into RNase J that plays an essential role in Mycobacterium tuberculosis RNA metabolism
Nature Communications (2023)
-
Inhibiting metallo-β-lactamases
Nature Reviews Drug Discovery (2022)
-
A hydroxide lock for metallo-β-lactamases
Nature Chemistry (2022)