Abstract
Diabetes is a common comorbidity in patients hospitalized for acute heart failure (AHF), but the relationship between admission glucose level, glycemic gap, and in-hospital mortality in patients with both conditions has not been investigated thoroughly. Clinical data for admission glucose, glycemic gap and in-hospital death in 425 diabetic patients hospitalized because of AHF were collected retrospectively. Glycemic gap was calculated as the A1c-derived average glucose subtracted from the admission plasma glucose level. Receiver operating characteristic (ROC) curves were used to determine the optimal cutoff value for glycemic gap to predict all-cause mortality. Patients with glycemic gap levels >43 mg/dL had higher rates of all-cause death (adjusted hazard ratio, 7.225, 95% confidence interval, 1.355–38.520) than those with glycemic gap levels ≤43 mg/dL. The B-type natriuretic peptide levels incorporated with glycemic gap could increase the predictive capacity for in-hospital mortality and increase the area under the ROC from 0.764 to 0.805 (net reclassification improvement = 9.9%, p < 0.05). In conclusion, glycemic gap may be considered a useful parameter for predicting the disease severity and prognosis of patients with diabetes hospitalized for AHF.
Similar content being viewed by others
Introduction
Diabetes is a common comorbidity in acute heart failure (AHF) patients and accounts for 30–40% of the overall population1,2. Diabetes may cause cardiac dysfunction in the absence of overt macrovascular disease, the formation of atherosclerosis and hypertension, and complications in response to therapy1,3. Hyperglycemia is a common problem in patients with AHF and is an independent risk factor of short-term mortality in non-diabetic patients but not in patients with diabetes4,5. Several studies suggest that hyperglycemia was associated with more severe symptoms and worse New York Heart Association (NYHA) functional classification and that in patients with AHF, especially those with previously diagnosed diabetes, hyperglycemia was related to higher in-hospital fatality6,7. However, the relationship between admission hyperglycemia and mortality in diabetic patients with AHF or critical illness remains controversial2,8,9. Those discrepancies could be partly attributed to long-term glycemic control in diabetic patients. Critical illness can induce stress-induced hyperglycemia (SIH), which results from the excess release of counter-regulatory hormones and anti-inflammatory cytokines, leading to augmented gluconeogenesis and insulin resistance10,11,12,13. In diabetic patients with acute illness, the phenomenon of admission hyperglycemia could be connected with acute physiological stress, poorer glycemic controls, or a combination of both14.
It is necessary to think about background glycemic control when exploring the relationships between admission hyperglycemia and clinical outcomes. Recent studies have shown that hemoglobin A1c (HbA1c)-based adjusted glycemic variables, including glycemic gap and stress hyperglycemia ratio, were linked to severity of disease and unfavorable prognosis in diabetic patients with some infectious diseases, cardiovascular diseases and critical illness15,16,17,18,19,20,21.
We hypothesized that a higher glycemic gap would be linked to unfavorable outcomes in diabetic patients with AHF. The present investigation was aimed at assessing the relationships between glycemic gap and adverse clinical outcomes in diabetic patients who were hospitalized due to AHF.
Methods
Study participants
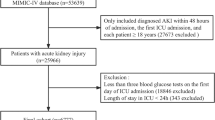
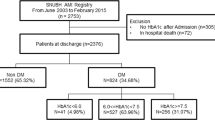
The use of the clinical data for this study was approved by Institutional Review Board of Tri-Service General Hospital, National Defense Medical Center and waived the requirement for informed consent. This retrospective observational study pooled data of all patients with diabetes hospitalized for AHF between June 1, 2011 and December 31, 2017. We searched the International Classification of Diseases (9th revision) codes 428.0–9 and 250.2–8 to identify the patients with diabetes and AHF. The patients’ medical records were then reviewed manually to enroll only those patients with AHF who had data for admission plasma glucose levels and HbA1c levels within 1 month before or after admission. Diagnosis of diabetes was defined if a patient was discharged from a hospital with a diagnosis of diabetes and/or at least 1 prescription for insulin or an oral antidiabetic agent and/or had an HbA1c level ≥6.5% in the preceding 2 months22,23.
Clinical diagnosis of AHF was made according to the presence of classic clinical history and physical examination, i.e., rapid-onset dyspnea and fatigue possibly leading to pulmonary and/or splanchnic congestion and/or peripheral edema, with further confirmation by laboratory measurement of B-type natriuretic peptide (BNP) ≥100 pg/ml, 12-lead electrocardiogram, chest radiography or echocardiography24,25. All included patients were admitted to the cardiology ward or intensive care unit (ICU) and were treated with intravenous therapy (inotropes, vasodilators, or diuretics). Patients were excluded based on the following criteria: age ≤18 years, hypoglycemia (plasma glucose <70 mg/dL) at initial presentation, or an admission diagnosis of diabetic ketoacidosis or hyperosmolar hyperglycemic state. Patients with hemoglobin variants (e.g., sickle cell anemia, thalassemia) or with hematologic conditions (e.g., hemolytic anemia) that could interfere with the accuracy of the HbA1c assay were also excluded.
Study design
We retrospectively reviewed patients’ medical records to determine age; sex; underlying comorbidities; etiology of AHF; current left ventricular ejection fraction (LVEF); laboratory data, including plasma glucose level at initial presentation and HbA1c levels (measured within 1 month before or after admission); and stays in the ICU and hospital. The NYHA functional class was used to assess the severity of AHF, and all the included patients were class III or IV at admission. Ejection fraction (EF) was measured by conventional transthoracic echocardiography according to international standard criteria. Cardiogenic shock was defined as severe hypotension of an acute cardiac cause despite adequate filling status (need for vasopressor therapy to maintain systolic blood pressure ≥90 mmHg). Acute respiratory failure (ARF) was defined as a patient with respiratory distress requiring noninvasive positive pressure ventilation (NIPPV) or endotracheal intubation with mechanical ventilation; acute kidney injury (AKI) was defined as serum creatinine elevated >0.3 mg/dL or 50% from baseline26; and upper gastrointestinal bleeding (UGIB) was defined as melena with positive occult blood examination, bright-red blood discharged from the nasogastric tube, or endoscopic evidence of mucosal bleeding. The primary endpoints were all-cause mortality during index hospitalization. Cardiovascular mortality was a composite of cardiac death attributed to cardiogenic shock, ventricular arrhythmia or myocardial infarction.
Measurements of admission glucose, HbA1c, and HbA1c-based adjusted glycemic gap
The admission glucose level was defined as initial plasma glucose levels upon admission to the emergency department. HbA1c was measured using high-performance liquid chromatography on a blood analyzer (Primus CLC 385; Primus Corporation, Kansas City, MO, USA). The long-term average glucose levels can be derived from the HbA1c values by using an equation from an international multicenter study of HbA1c-derived average glucose (ADAG). The estimated chronic average glucose levels (eAG) over the past 3 months was calculated from the equation AG = 28.7 × HbA1c − 46.727. Glycemic gap was calculated as the ADAG level subtracted from the admission glucose level.
Statistical analysis
Continuous data are expressed as the means ± standard deviations and were analyzed using the two-tailed Student’s t test. Categorical data are expressed as frequencies (%) and were compared using the chi-square test or Fisher’s exact test. A receiver operating characteristic (ROC) curve was plotted to calculate the area under the ROC (AUROC). Analyses were performed on Statistical Package for the Social Sciences version 22.0 statistical software (IBM Corp., Armonk, NY, USA), and differences with p values < 0.05 were considered statistically significant. Multivariate Cox proportional hazard models were applied to determine independent predictors of in-hospital all-cause mortality for AHF. The covariates included in the multivariable regression models were chosen as potential confounding factors based on their significance in univariable analyses. The log-rank test was performed to determine the statistical significance of the effects of all-cause mortality and cardiovascular mortality on Kaplan–Meier survival curves. The net reclassification improvement (NRI), a function of MATLAB (MathWorks, Natick, MA, USA), was performed to evaluate the improvement in overall predictive capacity after adding parameters28.
Results
Patient study population and clinical outcomes
We initially enrolled 425 hospitalized patients with diabetes and AHF. Patients were eliminated owning to admission hypoglycemia (n = 30). Ultimately, we identified 395 patients after a detailed medical record review. Of these patients, 46.3% were men, 7.1% died during hospitalization, 43.3% were admitted to the ICU, 6.3% experienced cardiogenic shock, 20.8% experienced ARF, 17.0% experienced AKI, and 5.1% developed UGIB. A comparison of the baseline characteristics of the enrolled patients between survivors and nonsurvivors during hospitalization is shown in Table 1. The glycemic gap levels were significantly higher in nonsurviving patients (109.6 ± 68.1 mg/dL) than in surviving patients (49.3 ± 96.8 mg/dL). The admission glucose levels were 262.2 ± 94.1 mg/dL in nonsurvivors and 221.5 ± 107.4 mg/dL in survivors, without a statistically significant difference. The mean ages were significantly older in nonsurvivors (83.3 ± 12.6 years) than in survivors (75.1 ± 12.2 years). Nonsurvivors had a greater likelihood of ischemic etiology of AHF, prior stroke and peripheral arterial occlusive disease than survivors. Moreover, nonsurvivors had higher levels of BNP and aspartate aminotransferase (AST) and lower levels of albumin than survivors and were more likely to develop cardiogenic shock, ventricular fibrillation (VF) or ventricular tachycardia (VT), ARF and UGIB than survivors.
Association between glycemic gap and heart failure (HF)
We performed a ROC analysis to determine the cutoff values of glycemic gap to maximize the predictive value for the incidence rates of all-cause and cardiovascular mortality. In both analyses, the optimal cutoff value of the glycemic gap was 43 mg/dL, with maximum AUROC of 0.738 (95% CI = 0.667–0.809) (sensitivity 85.7% and specificity 54.2%) in all-cause mortality, 0.767 (95% CI = 0.692–0.842) (sensitivity 91.3% and specificity 54.0%) in cardiovascular mortality and 0.758 (95% CI = 0.699–0.818) (sensitivity 81.3% and specificity 59.7%) in ARF. Moreover, glycemic gap produced higher AUROC values than did admission glucose for predicting all-cause mortality, cardiovascular mortality and ARF (Fig. 1).
Compared with patients with a glycemic gap level of ≤43 mg/dL, patients with a glycemic gap level of >43 mg/dL had a significantly increased risk of all-cause mortality, cardiovascular mortality, cardiogenic shock, ARF, and ICU admission with prolonged ICU and total hospital stays (Table 2). A Kaplan–Meier survival curve revealed that all-cause and cardiovascular mortality rates during hospitalization had significantly higher associations with a glycemic gap level >43 mg/dL than with a glycemic gap level ≤43 mg/dL (log-rank test, p < 0.05, Fig. 2). In a univariate Cox proportional hazards regression analysis, patients with a glycemic gap level >43 mg/dL [hazard ratio (HR), 4.568; 95% confidence interval (CI), 1.574–13.258; p = 0.005] had significantly increased in-hospital mortality but not admission glucose. In addition, increased age (HR, 1.048; 95% CI, 1.010–1.087; p = 0.01), prior stroke (HR, 2.744; 95% CI, 1.182–6.369; p = 0.02), greater log BNP level (HR, 6.299; 95% CI, 1.725–22.999; p = 0.005), higher AST level (HR, 1.001; 95% CI, 1.000–1.003; p = 0.04), and lower albumin level (HR, 0.344; 95% CI, 0.166–0.715; p = 0.004) showed values with p < 0.05 in univariate analyses and were included in the multivariate analysis. In multivariate Cox proportional hazards regression, patients with a glycemic gap >43 mg/dL presented a 7.22-fold greater risk of in-hospital mortality than those with a gap ≤43 mg/dL after adjusting for age, sex, prior stroke and levels of log BNP, AST and albumin. In addition to elevated glycemic gap levels, increased age, greater log BNP levels and lower albumin levels independently predicted in-hospital mortality in multivariate analyses (Table 3).
Correlation between glycemic gap and BNP
The correlations were statically significant but weak between glycemic gap and BNP levels (r = 0.184, p < 0.05, Fig. 3). Incorporating glycemic gap with BNP increased the discriminative performance of BNP for predicting all-cause mortality and raised the AUROC from 0.764 (95% CI = 0.673– 0.854) to 0.805 (95% CI = 0.729– 0.880) (NRI = 9.9%, P < 0.05, Fig. 4).
Discussion
Our data indicated that 1) compared to acute hyperglycemia and HbA1c, glycemic gap had greater discriminative power for predicting in-hospital mortality and the development of ARF in patients with diabetes admitted to the hospital due to AHF, and 2) incorporating glycemic gap could further increase the discriminative power of BNP, thus strengthening the clinical significance of glycemic gap in AHF.
Studies regarding admission glucose and mortality in patients hospitalized with AHF and diabetes are still controversial8,29. Some studies have indicated that SIH is linked to unfavorable clinical outcomes in a variety of critical illnesses14,30,31,32. A previous study also indicated that acute fluctuations in glucose concentrations are related to elevated mortality in acutely ill patients, independent of mean glucose concentration33. Patients without diabetes who died during the hospitalization period for AHF had, on average, higher first plasma glucose values than those who survived5. However, several studies have reported that the association between SIH and severity of disease is relatively slight in diabetic patients with critical illness34,35,36,37. The association between acute hyperglycemia, in terms of time-weighted glucose levels, and ICU mortality was stronger in patients without diabetes than in patients with diabetes38. A recent study showed that the maximum glucose levels in the first 24 h of ICU admission did not predict hospital fatality in a medical ICU39. These discordant findings led to the question of whether hyperglycemia contributes to increased mortality or is merely a marker of increased illness severity. Patients with diabetes presenting with acute illness could have a spectrum of premorbid glycemic control, from satisfactory to poor13. In patients with diabetes, acute hyperglycemia at admission could be the result of SIH, chronic poor glucose control or a combination of both. HbA1c levels are useful for assessing long-term overall glycemic control over the preceding 2–3 months, as they have characteristics of lesser biological variability and are relatively not interfered by acute stress23. By using HbA1c-adjusted glycemic variables, we were able to get rid of the possible interference of long-term hyperglycemia in patients with diabetes. In the current study, glycemic gap rather than admission glucose levels predicted hospital fatality in patients with diabetes and AHF. Similar findings were disclosed in patients with diabetes-sustained liver abscess15, community-acquired pneumonia16, ICU mortalities17, acute myocardial infarction (AMI)19, acute ischemic stroke21 and chronic obstructive lung disease with acute exacerbation20. The use of glycemic gap could explain the “diabetes paradox” and controversies about the association between admission hyperglycemia, chronic glycemic control, and adverse events40.
The prognosis for patients with HF is worse in those with diabetes than in those without diabetes, independent of the presence of coronary artery disease or its associated risk factors41. However, poorer glycemic control was not correlated with worse clinical outcomes in critically ill patients33,38,42. Glycemic control impacts the clinical outcomes in patients with HF and diabetes in a U-shaped relationship with poorer survival at low and high mean HbA1c levels43. Optimal chronic glycemic control occurs at a range of HbA1c from 7.1 to 8.0% for patients with diabetes who have HF43,44. Among HF patients with LVEF ≤ 45% who were not receiving antihyperglycemic drugs, those with HbA1c > 6.7% had greater mortality than those with HbA1c ≤ 6.7%45. Despite these data, studies examining the relationship between HbA1c and clinical outcomes in diabetic patients with HF have also disclosed discrepant results. Eshaghian et al. demonstrated that HbA1c levels >7.0 were associated with improved survival in patients with diabetes and advanced HF compared with HbA1c levels ≤7.046. In our study, the HbA1c levels did not correlate with hospital death in diabetic patients with AHF. Further investigation is necessary to determine the relationship between HbA1c and adverse events in diabetic patients with AHF.
Patients who had AHF complicated with ARF could further have SIH. Severe hyperglycemia was significantly correlated with hospital fatality in patients with cardiogenic shock47. In the current study, glycemic gap >43 mg/dL had a higher prevalence of ARF and cardiogenic shock than glycemic gap ≤43 mg/dL, further supporting the positive correlation between glycemic gap and severity of AHF. The levels of plasma BNP are closely related to HF severity, and BNP is used as a diagnostic and prognostic tool in both acute and chronic settings by international guidelines25. HF patients with diabetes had higher levels of BNP than those without diabetes in the chronic setting but not in the acute care setting48,49. BNP levels negatively correlate with systolic and diastolic cardiac function in patients with diabetes50. In accordance with our findings, a recent large study demonstrated that BNP levels and age were the strongest predictors of death in patients with HF51. We hypothesized that glycemic gap might represent acute physiological stress due to AHF and found that BNP levels correlated positively with glycemic gap levels. Furthermore, we revealed that incorporating glycemic gap with BNP levels could further increase the discriminative powers of BNP levels to predict in-hospital mortality in AHF patients with diabetes. Serum albumin has many physiological properties, including anti-inflammatory, antioxidant, antiplatelet and colloid osmotic effects52,53. The low plasma oncotic pressure related to hypoalbuminemia can lead to a fluid shift from the intravascular to the interstitial space and facilitate acute pulmonary edema in patients with AHF. Hypoalbuminemia was associated with higher NYHA class and BNP levels and served as an independent prognostic factor for predicting in-hospital death for elderly patients with AHF54,55. Our findings are consistent with previous studies, and serum albumin levels remain a strong and independent predictor of in-hospital mortality in diabetic patients with AHF even after adjusting for BNP levels and age.
Limitations
This study has a number of limitations. First, it was a single-center, retrospective investigation and may introduce selection bias. A prospective study using glycemic gap should be conducted in patients both with and without diabetes for further clarification. Second, the sufficiency of glycemic control while in hospital and the use of antidiabetic drugs might have interfered the outcomes. In the current study, we did not specifically investigate the influences of glycemic control during hospitalization. Intensive glucose-lowering therapy has no significant effect on the incidence of cardiac mortality or HF in patients with diabetes56. Marik et al. demonstrated that tight glycemic control does not remedy health care outcomes57. Third, insulin resistance or hyperinsulinemia is an independent predictor for AHF in cases of diabetes58,59. Several studies have reported that elevated leptin levels and reduction of adiponectin predict acute cardiovascular events60,61 and that the leptin/adiponectin ratio correlates well with insulin resistance in patients with diabetes62. Since the serum levels of insulin, leptin and adiponectin were not routinely measured in AHF patients, we could not clarify the relationship between glycemic gap and insulin resistance. Further prospective studies to incorporate serum insulin levels and leptin/adiponectin ratios into the glycemic gap may attain a clearer perception of the pathophysiology of SIH in diabetic patients with AHF.
Conclusion
Elevated glycemic gap was an independent predictor of in-hospital mortality and ARF. The levels of glycemic gap might be used to estimate the severity of critical illness and clinical outcomes in patients with diabetes presenting with AHF.
References
Thomas, M. C. Type 2 Diabetes and Heart Failure: Challenges and Solutions. Curr Cardiol Rev (2016).
Lazzeri, C., Valente, S. & Gensini, G. F. Hyperglycemia in acute heart failure: an opportunity to intervene? Current heart failure reports 11, 241–245, https://doi.org/10.1007/s11897-014-0205-9 (2014).
Yilmaz, S., Canpolat, U., Aydogdu, S. & Abboud, H. E. Diabetic Cardiomyopathy; Summary of 41 Years. Korean circulation journal 45, 266–272, https://doi.org/10.4070/kcj.2015.45.4.266 (2015).
Lazzeri, C. et al. Admission Glycaemia and Acute Insulin Resistance in Heart Failure Complicating Acute Coronary Syndrome. Heart, lung & circulation, https://doi.org/10.1016/j.hlc.2015.04.171 (2015).
de Miguel-Yanes, J. M. et al. First plasma glucose value after urgent admission and in-hospital mortality in acutely decompensated heart failure. Heart & lung: the journal of critical care 44, 137–140, https://doi.org/10.1016/j.hrtlng.2014.11.006 (2015).
Suskin, N. et al. Glucose and insulin abnormalities relate to functional capacity in patients with congestive heart failure. European heart journal 21, 1368–1375, https://doi.org/10.1053/euhj.1999.2043 (2000).
Targher, G. et al. Prognostic impact of in-hospital hyperglycemia in hospitalized patients with acute heart failure: Results of the IN-HF (Italian Network on Heart Failure) Outcome registry. Int J Cardiol 203, 587–593, https://doi.org/10.1016/j.ijcard.2015.10.207 (2015).
Kosiborod, M. et al. Elevated admission glucose and mortality in elderly patients hospitalized with heart failure. Circulation 119, 1899–1907, https://doi.org/10.1161/circulationaha.108.821843 (2009).
Lazzeri, C. et al. Admission Glycaemia and Acute Insulin Resistance in Heart Failure Complicating Acute Coronary Syndrome. Heart, lung &. circulation 24, 1074–1080, https://doi.org/10.1016/j.hlc.2015.04.171 (2015).
Marik, P. E. & Raghavan, M. Stress-hyperglycemia, insulin and immunomodulation in sepsis. Intensive Care Med 30, 748–756, https://doi.org/10.1007/s00134-004-2167-y (2004).
McCowen, K. C., Malhotra, A. & Bistrian, B. R. Stress-induced hyperglycemia. Crit Care Clin 17, 107–124 (2001).
Leonidou, L. et al. Cytokine production and hospital mortality in patients with sepsis-induced stress hyperglycemia. J Infect 55, 340–346, https://doi.org/10.1016/j.jinf.2007.05.177 (2007).
Dungan, K. M., Braithwaite, S. S. & Preiser, J. C. Stress hyperglycaemia. Lancet 373, 1798–1807, https://doi.org/10.1016/s0140-6736(09)60553-5 (2009).
McAlister, F. A. et al. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes care 28, 810–815 (2005).
Liao, W. I. et al. An elevated gap between admission and A1C-derived average glucose levels is associated with adverse outcomes in diabetic patients with pyogenic liver abscess. PloS one 8, e64476, https://doi.org/10.1371/journal.pone.0064476 (2013).
Chen, P. C. et al. An Elevated Glycemic Gap is Associated With Adverse Outcomes in Diabetic Patients With Community-Acquired Pneumonia. Medicine 94, e1456, https://doi.org/10.1097/md.0000000000001456 (2015).
Liao, W. I. et al. Usefulness of Glycemic Gap to Predict ICU Mortality in Critically Ill Patients With Diabetes. Medicine 94, e1525, https://doi.org/10.1097/md.0000000000001525 (2015).
Roberts, G. W. et al. Relative Hyperglycemia, a Marker of Critical Illness: Introducing the Stress Hyperglycemia Ratio. J Clin Endocrinol Metab 100, 4490–4497, https://doi.org/10.1210/jc.2015-2660 (2015).
Liao, W. I. et al. An Elevated Glycemic Gap is Associated with Adverse Outcomes in Diabetic Patients with Acute Myocardial Infarction. Scientific reports 6, 27770, https://doi.org/10.1038/srep27770 (2016).
Yang, C. J. et al. Glycated hemoglobin A1c-based adjusted glycemic variables in patients with diabetes presenting with acute exacerbation of chronic obstructive pulmonary disease. International journal of chronic obstructive pulmonary disease 12, 1923–1932, https://doi.org/10.2147/copd.s131232 (2017).
Yang, C. J. et al. Usefulness of glycated hemoglobin A1c-based adjusted glycemic variables in diabetic patients presenting with acute ischemic stroke. Am J Emerg Med 35, 1240–1246, https://doi.org/10.1016/j.ajem.2017.03.049 (2017).
Standards of medical care in diabetes–2014. Diabetes Care 37(Suppl 1), S14–80, https://doi.org/10.2337/dc14-S014 (2014).
Gillett, M. J. International Expert Committee report on the role of the A1c assay in the diagnosis of diabetes: Diabetes Care 2009; 32(7), 1327–1334. The Clinical biochemist. Reviews/Australian Association of Clinical Biochemists 30, 197–200 (2009).
Yancy, C. W. et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 128, 1810–1852, https://doi.org/10.1161/CIR.0b013e31829e8807 (2013).
Ponikowski, P. et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European journal of heart failure 18, 891–975, https://doi.org/10.1002/ejhf.592 (2016).
Thomas, M. E. et al. The definition of acute kidney injury and its use in practice. (Kidney Int. 2014 Oct 15. https://doi.org/10.1038/ki.2014.328).
Nathan, D. M. et al. Translating the A1C assay into estimated average glucose values. Diabetes care 31, 1473–1478, https://doi.org/10.2337/dc08-0545 (2008).
Pencina, M. J., D’Agostino, R. B. Sr., D’Agostino, R. B. Jr. & Vasan, R. S. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Statistics in medicine 27, 157–172; discussion 207–112, https://doi.org/10.1002/sim.2929 (2008).
Targher, G. et al. In-hospital and 1-year mortality associated with diabetes in patients with acute heart failure: results from the ESC-HFA Heart Failure Long-Term Registry. European journal of heart failure 19, 54–65, https://doi.org/10.1002/ejhf.679 (2017).
Kamouchi, M. et al. Prestroke glycemic control is associated with the functional outcome in acute ischemic stroke: the Fukuoka Stroke Registry. Stroke; a journal of cerebral circulation 42, 2788–2794, https://doi.org/10.1161/STROKEAHA.111.617415 (2011).
Rueda, A. M. et al. Hyperglycemia in diabetics and non-diabetics: effect on the risk for and severity of pneumococcal pneumonia. J Infect 60, 99–105, https://doi.org/10.1016/j.jinf.2009.12.003 (2010).
Oswald, G. A., Smith, C. C., Betteridge, D. J. & Yudkin, J. S. Determinants and importance of stress hyperglycaemia in non-diabetic patients with myocardial infarction. Br Med J (Clin Res Ed) 293, 917–922 (1986).
Egi, M., Bellomo, R., Stachowski, E., French, C. J. & Hart, G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology 105, 244–252 (2006).
Falciglia, M., Freyberg, R. W., Almenoff, P. L., D’Alessio, D. A. & Render, M. L. Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med 37, 3001–3009, https://doi.org/10.1097/CCM.0b013e3181b083f7 (2009).
Lheureux, O. & Preiser, J. C. Year in review 2013: Critical Care–metabolism. Crit Care 18, 571, https://doi.org/10.1186/s13054-014-0571-4 (2014).
Krinsley, J. S. et al. Diabetic status and the relation of the three domains of glycemic control to mortality in critically ill patients: an international multicenter cohort study. Crit Care 17, R37, https://doi.org/10.1186/cc12547 (2013).
Sechterberger, M. K. et al. The effect of diabetes mellitus on the association between measures of glycaemic control and ICU mortality: a retrospective cohort study. Crit Care 17, R52, https://doi.org/10.1186/cc12572 (2013).
Egi, M. et al. The interaction of chronic and acute glycemia with mortality in critically ill patients with diabetes. Crit Care Med 39, 105–111, https://doi.org/10.1097/CCM.0b013e3181feb5ea (2011).
Freire, A. X., Bridges, L., Umpierrez, G. E., Kuhl, D. & Kitabchi, A. E. Admission hyperglycemia and other risk factors as predictors of hospital mortality in a medical ICU population. Chest 128, 3109–3116, https://doi.org/10.1378/chest.128.5.3109 (2005).
Krinsley, J. S. & Fisher, M. The diabetes paradox: diabetes is not independently associated with mortality in critically ill patients. Hospital practice (1995) 40, 31–35, https://doi.org/10.3810/hp.2012.04.967 (2012).
Lehrke, M. & Marx, N. D Mellitus and Heart Failure. Am J Med, https://doi.org/10.1016/j.amjmed.2017.04.010 (2017).
Egi, M. et al. Blood glucose concentration and outcome of critical illness: the impact of diabetes. Crit Care Med 36, 2249–2255, https://doi.org/10.1097/CCM.0b013e318181039a (2008).
Elder, D. H. et al. Mean HbA and mortality in diabetic individuals with heart failure: a population cohort study. European journal of heart failure, https://doi.org/10.1002/ejhf.455 (2015).
Bahtiyar, G., Gutterman, D. & Lebovitz, H. Heart Failure: a Major Cardiovascular Complication of Diabetes Mellitus. Current diabetes reports 16, 116, https://doi.org/10.1007/s11892-016-0809-4 (2016).
Goode, K. M. et al. Elevated glycated haemoglobin is a strong predictor of mortality in patients with left ventricular systolic dysfunction who are not receiving treatment for diabetes mellitus. Heart 95, 917–923, https://doi.org/10.1136/hrt.2008.156646 (2009).
Eshaghian, S., Horwich, T. B. & Fonarow, G. C. An unexpected inverse relationship between HbA1c levels and mortality in patients with diabetes and advanced systolic heart failure. American heart journal 151, 91, https://doi.org/10.1016/j.ahj.2005.10.008 (2006).
Kataja, A. et al. The association of admission blood glucose level with the clinical picture and prognosis in cardiogenic shock- Results from the CardShock Study. Int J Cardiol 226, 48–52, https://doi.org/10.1016/j.ijcard.2016.10.033 (2017).
Cunha, F. M. et al. Natriuretic Peptide System Activation in Acute Heart Failure Patients with Diabetes. J Diabetes Res 2017, 1426705, https://doi.org/10.1155/2017/1426705 (2017).
van der Horst, I. C. et al. Neurohormonal profile of patients with heart failure and diabetes. Neth Heart J 18, 190–196 (2010).
Albertini, J. P., Cohen, R., Valensi, P., Sachs, R. N. & Charniot, J. C. B-type natriuretic peptide, a marker of asymptomatic left ventricular dysfunction in type 2 diabetic patients. Diabetes Metab 34, 355–362, https://doi.org/10.1016/j.diabet.2008.02.004 (2008).
York, M. K. et al. B-Type Natriuretic Peptide Levels and Mortality in Patients With and Without Heart Failure. Journal of the American College of Cardiology 71, 2079–2088, https://doi.org/10.1016/j.jacc.2018.02.071 (2018).
Zhang, W. J. & Frei, B. Albumin selectively inhibits TNF alpha-induced expression of vascular cell adhesion molecule-1 in human aortic endothelial cells. Cardiovascular research 55, 820–829 (2002).
Lam, F. W. et al. Histone induced platelet aggregation is inhibited by normal albumin. Thromb Res 132, 69–76, https://doi.org/10.1016/j.thromres.2013.04.018 (2013).
Kinugasa, Y. et al. A simple risk score to predict in-hospital death of elderly patients with acute decompensated heart failure–hypoalbuminemia as an additional prognostic factor. Circ J 73, 2276–2281 (2009).
Horwich, T. B., Kalantar-Zadeh, K., MacLellan, R. W. & Fonarow, G. C. Albumin levels predict survival in patients with systolic heart failure. American heart journal 155, 883–889, https://doi.org/10.1016/j.ahj.2007.11.043 (2008).
Fang, H. J. et al. Effects of intensive glucose lowering in treatment of type 2 diabetes mellitus on cardiovascular outcomes: A meta-analysis of data from 58,160 patients in 13 randomized controlled trials. Int J Cardiol 218, 50–58, https://doi.org/10.1016/j.ijcard.2016.04.163 (2016).
Marik, P. E. & Bellomo, R. Stress hyperglycemia: an essential survival response! Crit Care 17, 305, https://doi.org/10.1186/cc12514 (2013).
Packer, M. Potentiation of Insulin Signaling Contributes to Heart Failure in Type 2 Diabetes: A Hypothesis Supported by Both Mechanistic Studies and Clinical Trials. JACC Basic Transl Sci 3, 415–419, https://doi.org/10.1016/j.jacbts.2018.04.003 (2018).
Jia, G., DeMarco, V. G. & Sowers, J. R. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nature reviews. Endocrinology 12, 144–153, https://doi.org/10.1038/nrendo.2015.216 (2016).
Lekva, T. et al. Leptin and adiponectin as predictors of cardiovascular risk after gestational diabetes mellitus. Cardiovascular diabetology 16, 5, https://doi.org/10.1186/s12933-016-0492-4 (2017).
Kotani, K., Sakane, N., Saiga, K. & Kurozawa, Y. Leptin: adiponectin ratio as an atherosclerotic index in patients with type 2 diabetes: relationship of the index to carotid intima-media thickness. Diabetologia 48, 2684–2686, https://doi.org/10.1007/s00125-005-0015-4 (2005).
Inoue, M., Maehata, E., Yano, M., Taniyama, M. & Suzuki, S. Correlation between the adiponectin-leptin ratio and parameters of insulin resistance in patients with type 2 diabetes. Metabolism: clinical and experimental 54, 281–286, https://doi.org/10.1016/j.metabol.2004.09.006 (2005).
Acknowledgements
This study was supported by grants from Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan (TSGH-C107-044 and TSGH-C107-047), National Defense Medical Center, Taipei, Taiwan (MAB-107-012 and MAB-108-017) and the Ministry of Science and Technology, Taiwan (MOST 107-2314-B-016-043 and MOST 107-2314-B-016-061).
Author information
Authors and Affiliations
Contributions
W.I.L. and C.M.C. took part in the data analyses and performed statistical analyses; C.S.L., S.J.C. and S.H.T. designed the study; W.I.L. and S.H.T. wrote the manuscript; and C.C.H., J.C.W. and C.J.Y. collected the data. All authors gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liao, WI., Wang, JC., Lin, CS. et al. Elevated Glycemic Gap Predicts Acute Respiratory Failure and In-hospital Mortality in Acute Heart Failure Patients with Diabetes. Sci Rep 9, 6279 (2019). https://doi.org/10.1038/s41598-019-42666-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-42666-0
This article is cited by
-
Stress hyperglycemia is predictive of clinical outcomes in patients with spontaneous intracerebral hemorrhage
BMC Neurology (2022)
-
Admission blood glucose level and outcome in patients requiring venoarterial extracorporeal membrane oxygenation
Clinical Research in Cardiology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.