Abstract
The increasing use of new and emerging tobacco products has raised public health concern worldwide. This study aimed to assess the association between tobacco product use and the risk of allergic diseases. We used cross-sectional data of 58,336 students aged 12–18 years from the 2018 Korea Youth Risk Behavior Survey. This study considered three tobacco products, namely cigarettes, electronic cigarettes (e-cigarettes), and heated tobacco products. Descriptive analyses, as well as simple and multinomial logistic regression analyses with a complex sampling design, were performed. Multiple tobacco use had an association with the risk of each allergic disease. Use of each tobacco product was significantly associated with an increased risk of multi-morbidity of asthma, allergic rhinitis, and atopic dermatitis. Furthermore, lifetime use of each tobacco product was associated with the prevalence of atopic dermatitis. This highlights the importance of paying close attention to smoking by adolescents and its association with allergy epidemics. Future research should consider intensity of smoking and/or severity of allergic symptoms.
Similar content being viewed by others
Introduction
Allergic diseases have been considered as a serious public health concern, as they place significant economic burden on health services and lead to diminished quality of life1. Allergic diseases, such as asthma, allergic rhinitis (AR), and atopic dermatitis (AD), are often associated with sleep disturbance, intellectual dysfunction, and activity restriction, leading to physical and mental suffering2. In addition, the onset of such allergic diseases in childhood or adolescence may persist into adulthood3,4, requiring an integrated approach to proper treatment and management.
During the past decade (2009–2018), the prevalence of asthma, AR, and AD among high school students in Korea increased from 7.4% to 8.9%, 29.6% to 38.7%, and 18.2% to 26.1%, respectively5. The socioeconomic costs of allergic diseases in Korea were calculated to be approximately $1.8 billion, equivalent to 0.15% of the nation’s total gross domestic product of $1.3 trillion. In 2014, the socioeconomic costs of AR reached $1.1 billion (58.6%), while those of asthma and AD amounted to $0.62 billion (33.2%) and $0.16 billion (8.3%)6.
Tobacco smoke exposure, either active or passive, has been identified as a factor that increases the prevalence of asthma, AR, and AD7,8,9. Numerous toxic chemical and carcinogens, which contribute to respiratory irritation, such as acrolein, acetaldehyde, and formaldehyde, have been found in cigarette smoke10. According to laboratory studies with animal models11,12 and a literature review study13, tobacco smoke could affect inflammatory processes, leading to an increase in eosinophils, collagen production, and airway remodeling.
Unlike combusted cigarettes, electronic cigarettes (e-cigarettes) heat a metal coil to aerosolize a liquid mixture of nicotine, glycerol, in addition to flavoring agents14. The vapor produced by e-cigarettes has been reported to induce oxidative stress and suppress immune-related gene expression, leading to toxicity and impaired host defense mechanisms15,16,17. A plethora of research18 has been conducted on the association of tobacco smoke exposure with asthma, AR, and AD, whereas only a few studies focusing on the association between e-cigarettes and allergic diseases have been published.
Heated tobacco products (HTPs), the latest type of tobacco product, heat a processed tobacco leaf, not a liquid, up to 350 °C19. According to certain studies20,21, HTPs have the same harmful constituents as conventional cigarettes. Additionally, recent findings22 show that they can potentially cause impairments in lung cells by altering mitochondrial functionality, inducing oxidative stress, and limiting airflow. These impairments are often associated with asthma and chronic obstructive pulmonary disease. A recent in vitro study23 confirmed that HTP aerosols had adverse effects on human bronchial epithelial cells and that their cytotoxicity was higher than that of e-cigarettes, but less than that of conventional cigarettes.
This study aimed to assess the impact of tobacco use, including HTPs, on asthma, AR, and AD in Korean adolescents. The use of multiple tobacco products and comorbidity of allergic diseases were also considered in this study. To the best of our knowledge, this is the very first study to evaluate the effects of tobacco product use on asthma, AR, and AD with respect to multiple tobacco product use and development of multiple morbidities.
Results
Of all participants, 2.4% (1,443/58,336), 20.9% (11,884/58,336), and 7.2% (4,198/58,336) reported the diagnosis of asthma, AR, and AD within the past year, respectively (Table 1). In total, 25.8% of adolescents were affected by any of the three allergic diseases. Among the three allergic diseases, participants with AR had the oldest mean age of onset (15.2 years).
Conventional cigarettes, e-cigarettes, and HTPs had been used by 13.9% (8,129/58,336), 7.1% (4,114/58,336) and 2.4% (1,414/58,336) of participants (Table 2). The allergic disease group used conventional cigarettes, e-cigarettes, and HTPs more than the group without allergic diseases. Secondhand smoking at home and at school was more prevalent in the asthma, AR, and AD groups.
Table 3 shows that the three allergic diseases were more likely to be found among participants reporting that they had ever used conventional cigarettes or HTPs. Having asthma, AR, and AD was positively and significantly associated with secondhand smoking at home and school for five or more days per week. Regarding multiple tobacco product use, 57.1% of e-cigarette users were dual users of conventional cigarettes and e-cigarettes. Interestingly, 82.4% of HTP users were triple users of cigarettes, e-cigarettes, and HTPs, whereas 28.6% and 15.0% of ever e-cigarette and conventional cigarette users were triple users, respectively.
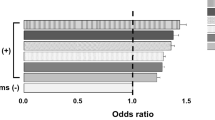
According to Table 4, even after adjusting for all other variables, the use of all three tobacco products was associated with a higher risk of asthma, AR, and AD (AOR = 1.59, 95% CI: 1.17–2.15; AOR = 1.22, 95% CI: 1.05–1.42; and AOR = 1.64, 95% CI: 1.36–1.98) (Table 4). Sole use of HTP was strongly associated with asthma (AOR = 3.59, 95% CI: 1.47–8.78), and so was dual use of cigarette and HTP (AOR = 4.38, 95% CI: 2.44–7.87).
Among the group of asthmatic participants, those diagnosed with asthma and AR accounted for 40.9%. Moreover, the three allergic diseases co-existed in 19.2% of asthmatic participants. However, 80.6% of AR participants were diagnosed solely with this disease.
In this study, an increased risk of multi-morbidity was attributable to the use of conventional cigarettes (AOR = 1.98, 95% CI: 1.45–2.70), e-cigarettes (AOR = 1.83, 95% CI: 1.25–2.68), and HTPs (AOR = 2.48, 95% CI: 1.48–4.13) (Table 5). The multinomial regression analysis indicated that adolescents using tobacco products were more likely to suffer from allergic multi-morbidity of asthma, AR, and AD altogether. In addition, the AOR for having only AD relative to the use of conventional cigarettes, e-cigarettes, and HTPs were 1.34 (95% CI: 1.20–1.50), 1.37 (95% CI: 1.17–1.61), and 1.80 (95% CI: 1.44–2.26).
Discussion
This study investigated the association between tobacco product use and allergic diseases in a school-based sample of adolescents in Korea.
In our study, active tobacco smoking in adolescents was associated with asthma. This result is in concordance with that of previous studies7,24,25,26. In a health study on 46,182 African American women, the incidence of asthma among current active smokers was higher than that among never smokers (HR: 1.43, 95% CI: 1.15–1.77)24. The effect of active cigarette smoking on adolescent-onset asthma symptoms was also shown in a German cohort study with the adjusted incidence risk ratio of 2.56 (95% CI: 1.55–4.21)25.
Our study pointed out the association between active smoking and AR. This result was consistent with that of some previous studies. For example, an epidemiological study26 of 14,578 French adolescents showed that those with active smoking were 2.95 times more likely to suffer from AR than the others (95% CI: 1.58–5.49). A recent meta-analysis of 97 studies on tobacco exposure and allergic conditions27 reported that active smoking among children and adolescents was significantly associated with the risk of AR.
Like our study, several studies demonstrated that smoking was associated with a higher risk for AD. Saulyte et al.27 examined 91 studies on allergic dermatitis and revealed that both active and passive smoking were associated with allergic dermatitis in children and adolescents. In a Korean study28, adolescents who smoked more than 20 days/month were more likely to develop AD than non-smokers (AOR = 1.18, 95% CI: 1.07–1.29).
The link between conventional cigarette smoking and allergic diseases has been well studied, whereas little research has been conducted on the association of e-cigarettes or HTPs with allergic diseases. A recent cross-sectional study29 of youths found that e-cigarette users developed more asthmatic symptoms than non-smokers. Furthermore, since HTPs have recently been introduced to the tobacco market, the (likely) mechanisms that link HTP use to the onset of allergic diseases have not been elucidated.
According to the recent data in the US, multiple tobacco product use was prevalent among adolescents. In 2018, 11.3% of high school students (41.7% of current users) reported using two or more tobacco products30. Our findings pointed out that triple use was most prevalent among HTP users (nearly 82.4%). According to a study of US youths, irritable or restless feelings due to tobacco withdrawal were 1.3 times more likely to be reported among multiple tobacco product users than among those using only one type of product31. This suggested that multiple tobacco users were possibly dependent of nicotine. Furthermore, their frequency of tobacco use increased, suggesting increased nicotine exposure and vulnerability to negative tobacco-related health effects32.
In this study, triple use of tobacco products was significantly associated with the risk of asthma, AR, and AD respectively. Multiple use may have a significant detrimental effect on health due to increased exposure to nicotine and/or toxicants. To further assess the risk for developing any allergic disease, it is necessary to understand the characteristics of multiple tobacco users and their use patterns.
Either comorbidity or multi-morbidity in patients was associated with an increase in physician/nurse appointments, visits to emergency department, or prescribed medication load33. Asthma, AR, and atopic disease are known to be inter-related, and multi-morbidity of allergic disease is commonly observed in adolescents34,35,36. Multi-morbidity can be observed in any allergic disease; however, this study shows an increased risk of reporting three allergic diseases concomitantly in smokers, compared to non-smokers.
Additionally, ever use of any tobacco product was significantly associated with a sole diagnosis of AD in our study participants. AD commonly manifested as a beginning of the ‘atopic march’; it is often followed by subsequent development of allergic rhino-conjunctivitis and asthma37. Therefore, it is plausible that local cutaneous sensitization may induce the systemic immune response with migration of sensitized T cells into the mucous membranes of the nose and lung through the circulatory system. This activates eosinophils and epithelial cells, IgE production, proliferation of mast cell, and smooth muscle observed in asthmatic patients37,38.
Tobacco use, in any form, may induce an inflammatory and immune response associated with increased exposure to allergens. Although several pathophysiological possibilities have been suggested, multi-morbidity of allergic disease in smokers has not been widely considered. Given the increasing prevalence and the importance of allergic diseases in adolescents, further monitoring and investigation on this mechanism is needed.
Limitations
There are some limitations which should be considered. The cross-sectional design limited the possibility of establishing causal relationships between tobacco product use and allergic diseases, although this study had a large representative sample. A longitudinal research design would be more desirable to examine such causal relationships. Since our survey consisted of a large participants, objective indicators, such as serum IgE levels, eosinophil counts, or serum cotinine levels, could not be measured. Additionally, the questionnaire was not designed to investigate detailed features of allergic diseases (e.g. frequency, severity, or associated symptoms). Furthermore, adolescents tend to under-report their smoking behavior to conceal their delinquency, thus affecting the accuracy of measurement. Another limitation is that this study relied on diagnoses reported by patients rather than physician diagnoses. However, the generalizability of the study results is high because the study had a representative sample and design, as well as a high response rate of over 95%.
Conclusion
In conclusion, our study findings indicated that the use of multiple tobacco products, including HTPs, might be a risk factor for asthma, allergic rhinitis, and atopic dermatitis. Additionally, the consistent use of each tobacco product we examined was linked to multi-morbidity of asthma, allergic rhinitis, and atopic dermatitis. An initial diagnosis of atopic dermatitis can lead to a subsequent systemic immune response. Healthcare professionals should pay close attention to smoking in adolescents because it is a potential contributor to the development of allergic diseases. To examine whether these associations are transient, further research with a longitudinal study design should be conducted.
Materials and Methods
Data and study participants
The present study used data from the Korea Youth Risk Behavior Survey of students aged 12–18 years from middle and high schools in Korea conducted in 2018. This government-approved survey39 has been annually performed since 2005. It is used by the Korea Centers for Disease Control and Prevention for monitoring adolescent health behaviors, including alcohol consumption, smoking, obesity, and physical activity. The survey was developed to produce a nationally representative sample of Korean adolescents with a stratified multi-stage cluster sampling design.
Initially, 400 middle schools and 400 high schools were randomly selected from 117 strata formed based on the administrative divisions and school types. Then, one class in each grade were randomly selected at each selected school. Out of a total of 2,850,118 students, a representative sample of 62,823 was selected from 5625 schools (middle and high) in Korea. Among the representative sample of 62,823 students recruited, 60,040 students agreed to participate in the survey, giving a high response rate of 95.6%. Besides, any student not providing information about their height or weight was excluded from the study. Therefore, the final study participants included 58,336 students (Fig. 1).
Students filled in online informed consent forms before participating in the survey in computer rooms. Parental consent was waived, as the survey was carried out by the Ministry of Education at schools with large numbers of students. The institutional Review Board of the Catholic University of Korea approved this study (as exempted from review, MC19ZESI0073).
Measures
As the study outcomes, allergic diseases (asthma, AR, or AD) were identified based on the participant’s self-reported diagnoses. Participants were asked the following question: ‘Within the past 12 months, have you been diagnosed with asthma/allergic rhinitis/atopic dermatitis by a medical doctor?’(yes, no).
This study considered three tobacco products, namely conventional cigarettes, e-cigarettes, and HTPs. Students were determined to have a history of cigarette use if they answered ‘yes’ to the question ‘Have you ever smoked a cigarette in your lifetime, even one puff?’. To identify a history of e-cigarette or HTP use, we asked the students if they had ever used an e-cigarette or a heated tobacco product (e.g., IQOS, glo, or lil), excluding conventional cigarettes and e-cigarettes in their lives. Ever use of two or three of the tobacco products was defined as dual or triple use. Secondhand smoking at home was assessed by the following question: ‘Within the past seven days, how many days have you spent time with someone who smoked in your home (either family member or guest)?’ Meanwhile, secondhand smoking at school was investigated according to the question: ‘In the past seven days, have you ever been in close contact with an active smoker at school?’ Secondhand smoking at home and school was divided into three groups: 0 day/week; 1–4 days/week; and ≥5 days/week.
General characteristics, such as age, sex, obesity, residential area, family economic status, and physical activity, were also assessed and used as covariates in the logistic regression models. In terms of body mass index (kg/m2), the study participants were divided into four groups according to the Centers for Disease Control and Prevention guidelines for children and teenagers40. Four groups included obese (≥95th percentile), overweight (≥85th percentile and <95th percentile), normal or healthy weight (≥5th percentile and <85th percentile), and underweight (<5th percentile). The ‘residential area’ variable had three values, including large cities, medium or small cities, and provinces. Students were asked “What is the economic condition of your family?” in the questionnaire. Five levels of family economic status were specified in the questionnaire as high, mid-high, middle, mid-low, and low, and they were regrouped as high, middle, and low for the sake of analysis. Physical activity was evaluated as the number of days per week with ≥60 minutes of moderate-intensity activity that caused a slight increase in one’s breathing or pulse rate. Students were asked “During the last seven days, on how many days did you do more than 60 minutes of moderate-intensity physical activity per day?”. Responses regarding the frequency of physical activity ranged from none to seven days per week. Participants engaging in moderate-intensity activity at least five days per week were considered as physically active. Physical activity criteria were based on the moderate level physical activity guideline stated in the International Physical Activity Questionnaire.
Statistical analyses
First, descriptive statistics of general characteristics among participants were presented as unweighted frequencies and weighted percentages. In addition, chi-square tests were used to examine the difference in the prevalence of each allergic disease by general characteristics, smoking-related characteristics, and tobacco use type. Subsequently, simple logistic regression analyses were conducted to calculate odds ratios (ORs) and adjusted ORs (aORs) for asthma, AR, and AD in the past 12-months based on the use of tobacco product; 95% confidence intervals (CI) were also calculated. Finally, multinomial logistic regression analyses were performed to identify the associations of tobacco product use with risk of allergic diseases. Bonferroni for post-hoc analysis was used for multiple comparisons. Adjusted models included age, sex, obesity, residential area, family economic status, and physical activity as covariates. Complex sampling modules were reflected and recommended weights were applied in this study. All statistical analyses were performed using SPSS version 26.0 (IBM, Armonk, NY, USA). The level of statistical significance was set at p < 0.05.
Data availability
The datasets analyzed during the current study are publicly available. Individual researchers need to gain access to download the dataset via the official website http://yhs.cdc.go.kr.
References
Baiardini, I., Braido, F., Brandi, S. & Canonica, G. W. Allergic diseases and their impact on quality of life. Ann Allergy Asthma Immunol 97, 419–429, https://doi.org/10.1016/S1081-1206(10)60928-3 (2006).
Holgate, S. T. The epidemic of allergy and asthma. Nature 402, 2, https://doi.org/10.1038/35037000 (1999).
Burgess, J. A. et al. Childhood allergic rhinitis predicts asthma incidence and persistence to middle age: A longitudinal study. J Allergy Clin Immunol 120, 863–869, https://doi.org/10.1016/j.jaci.2007.07.020 (2007).
Margolis, J. S., Abuabara, K., Bilker, W., Hoffstad, O. & Margolis, D. J. Persistence of Mild to Moderate Atopic Dermatitis. JAMA Dermatol 150, 593–600, https://doi.org/10.1001/jamadermatol.2013.10271 (2014).
Korea Centers for Disease Control and Prevention. The Statistics of 14th Korea Youth Risk Behavior Survey(KYRBS). Seoul, Korea: Korea Centers for Disease Control and Prevention (2018).
Lee, E. H., Cha, S. H. & Kim, W. Socioeconomic Burden due to Allergic Diseases. Gyeonggi Research Institute (2016).
Kim, S. Y., Sim, S. & Choi, H. G. Active, passive, and electronic cigarette smoking is associated with asthma in adolescents. Sci Rep 7, 17789 (2017).
Yao, T.-C. et al. Exposure to tobacco smoke and childhood rhinitis: a population-based study. Sci Rep 7, 42836, https://doi.org/10.1038/srep42836 (2017).
Krämer, U. et al. The effect of environmental tobacco smoke on eczema and allergic sensitization in children. Br J Dermatol 150, 111–118, https://doi.org/10.1111/j.1365-2133.2004.05710.x (2004).
Fowles, J. & Dybing, E. Application of toxicological risk assessment principles to the chemical constituents of cigarette smoke. Tob Control 12, 424–430, https://doi.org/10.1136/tc.12.4.424 (2003).
Botelho, F. M. et al. Cigarette Smoke Differentially Affects Eosinophilia and Remodeling in a Model of House Dust Mite Asthma. Am J Respir Cell Mol Biol 45, 753–760, https://doi.org/10.1165/rcmb.2010-0404OC (2011).
Blacquière, M. J. et al. Maternal smoking during pregnancy induces airway remodelling in mice offspring. Eur Respir J 33, 1133, https://doi.org/10.1183/09031936.00129608 (2009).
Strzelak, A., Ratajczak, A., Adamiec, A. & Feleszko, W. Tobacco Smoke Induces and Alters Immune Responses in the Lung Triggering Inflammation, Allergy, Asthma and Other Lung Diseases: A Mechanistic Review. Int J Environ Res Public Health 15, 1033 (2018).
Chun, L. F., Moazed, F., Calfee, C. S., Matthay, M. A. & Gotts, J. E. Pulmonary toxicity of e-cigarettes. Am J Physiol Lung Cell Mol Physiol 313, L193–L206, https://doi.org/10.1152/ajplung.00071.2017 (2017).
Martin, E. M. et al. E-cigarette use results in suppression of immune and inflammatory-response genes in nasal epithelial cells similar to cigarette smoke. Am J Physiol Lung Cell Mol Physiol 311, L135–L44 (2016).
Moses, E. et al. Molecular Impact of Electronic Cigarette Aerosol Exposure in Human Bronchial Epithelium. Toxicol Sci 155, 248–257, https://doi.org/10.1093/toxsci/kfw198 (2017).
Lerner, C. A. et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One 10, e0116732, https://doi.org/10.1371/journal.pone.0116732 (2015).
Kantor, R., Kim, A., Thyssen, J. P. & Silverberg, J. I. Association of atopic dermatitis with smoking: A systematic review and meta-analysis. J Am Acad Dermatol 75, 1119–1125, https://doi.org/10.1016/j.jaad.2016.07.017 (2016).
IQOS. About IQOS. 2019. Available, https://kr.iqos.com/en/products/iqos/what-is# (2019).
Farsalinos, K. E. et al. Carbonyl emissions from a novel heated tobacco product (IQOS): comparison with an e-cigarette and a tobacco cigarette. Addiction 113, 2099–2106, https://doi.org/10.1111/add.14365 (2018).
Auer, R., Concha-Lozano, N., Jacot-Sadowski, I., Cornuz, J. & Berthet, A. Heat-Not-Burn Tobacco Cigarettes: Smoke by Any Other Name. JAMA Intern Med 177, 1050–1052, https://doi.org/10.1001/jamainternmed.2017.1419 (2017).
Sohal, S. S., Eapen, M. S., Naidu, V. G. M. & Sharma, P. IQOS exposure impairs human airway cell homeostasis: direct comparison with traditional cigarette and e-cigarette. ERJ Open Res 5, 00159–2018, https://doi.org/10.1183/23120541.00159-2018 (2019).
Leigh, N. J., Tran, P. L., O’Connor, R. J. & Goniewicz, M. L. Cytotoxic effects of heated tobacco products (HTP) on human bronchial epithelial cells. Tob Control 27(Suppl 1), s26, https://doi.org/10.1136/tobaccocontrol-2018-054317 (2018).
Coogan, P. F. et al. Active and Passive Smoking and the Incidence of Asthma in the Black Women’s Health Study. Am J Respir Crit Care Med 191, 168–176, https://doi.org/10.1164/rccm.201406-1108OC (2015).
Genuneit, J. et al. Smoking and the incidence of asthma during adolescence: results of a large cohort study in Germany. Thorax 61, 572–578, https://doi.org/10.1136/thx.2005.051227 (2006).
Annesi-Maesano, I. et al. Increased prevalence of asthma and allied diseases among active adolescent tobacco smokers after controlling for passive smoking exposure. A cause for concern? Clin Exp Allergy 34, 1017–1023, https://doi.org/10.1111/j.1365-2222.2004.02002.x (2004).
Saulyte, J., Regueira, C., Montes-Martínez, A., Khudyakov, P. & Takkouche, B. Active or passive exposure to tobacco smoking and allergic rhinitis, allergic dermatitis, and food allergy in adults and children: a systematic review and meta-analysis. PLoS Med 11, e1001611, https://doi.org/10.1371/journal.pmed.1001611 (2014).
Kim, S. Y., Sim, S. & Choi, H. G. Atopic dermatitis is associated with active and passive cigarette smoking in adolescents. PLoS ONE 12, e0187453, https://doi.org/10.1371/journal.pone.0187453 (2017).
Cho, J. H. & Paik, S. Y. Association between Electronic Cigarette Use and Asthma among High School Students in South Korea. PLoS ONE 11, e0151022, https://doi.org/10.1371/journal.pone.0151022 (2016).
Gentzke, A. S. et al. Vital signs: tobacco product use among middle and high school students—United States, 2011–2018. MMWR Morb Mortal Wkly Rep 68, 157–164 (2019).
Apelberg, B. J. et al. Symptoms of Tobacco Dependence Among Middle and High School Tobacco Users: Results from the 2012 National Youth Tobacco Survey. Am J Prev Med 47, S4–S14, https://doi.org/10.1016/j.amepre.2014.04.013 (2014).
Bombard, J. M., Pederson, L. L., Koval, J. J. & O’Hegarty, M. How are lifetime polytobacco users different than current cigarette-only users? Results from a Canadian young adult population. Addict Behav 34, 1069–1072, https://doi.org/10.1016/j.addbeh.2009.06.009 (2009).
Jantunen, J. et al. Multimorbidity in Asthma, Allergic Conditions and COPD Increase Disease Severity, Drug Use and Costs: The Finnish Pharmacy Survey. Int Arch Allergy Immunol 179, 273–280, https://doi.org/10.1159/000498861 (2019).
Ballardini, N. et al. Development and comorbidity of eczema, asthma and rhinitis to age 12 – data from the BAMSE birth cohort. Allergy 67, 537–544, https://doi.org/10.1111/j.1398-9995.2012.02786.x (2012).
Lack, G. Pediatric allergic rhinitis and comorbid disorders. J Allergy Clin Immunol 108, S9–S15, https://doi.org/10.1067/mai.2001.115562 (2001).
Yuksel, H. et al. Prevalence and comorbidity of allergic eczema, rhinitis, and asthma in a city in western Turkey. J Investig Allergol Clin Immunol 18, 31–35 (2008).
Spergel, J. M. & Paller, A. S. Atopic dermatitis and the atopic march. J Allergy Clin Immunol 112, S118–S127, https://doi.org/10.1016/j.jaci.2003.09.033 (2003).
Brunner, P. M. et al. Increasing Comorbidities Suggest that Atopic Dermatitis Is a Systemic Disorder. J Invest Dermatol 137, 18–25, https://doi.org/10.1016/j.jid.2016.08.022 (2017).
Kim, Y. et al. Data Resource Profile: The Korea Youth Risk Behavior Web-based Survey (KYRBS). Int J Epidemiol 45, 1076–1076e, https://doi.org/10.1093/ije/dyw070 (2016).
Centers for Disease Control and Prevention. About Child & Teen BMI, https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html (2019).
Author information
Authors and Affiliations
Contributions
A.L. and K.-S.L. designed the study. A.L. conducted the analyses and wrote the manuscript. K.-S.L. and S.L. advised on data interpretation and revised the manuscript. All authors reviewed the manuscript and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, A., Lee, S.Y. & Lee, KS. The Use of Heated Tobacco Products is Associated with Asthma, Allergic Rhinitis, and Atopic Dermatitis in Korean Adolescents. Sci Rep 9, 17699 (2019). https://doi.org/10.1038/s41598-019-54102-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-54102-4
This article is cited by
-
Immunology in COPD and the use of combustible cigarettes and heated tobacco products
European Journal of Medical Research (2023)
-
Association of cigarette smoking with increased use of heated tobacco products in middle-aged and older adults with self-reported chronic obstructive pulmonary disease, asthma, and asthma-COPD overlap in Japan, 2022: the JASTIS study
BMC Pulmonary Medicine (2023)
-
Risk factors of asthma in the Asian population: a systematic review and meta-analysis
Journal of Physiological Anthropology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.