Abstract
The ratio between the length of second and fourth digits (2D:4D) is a putative biomarker for prenatal testosterone and estrogen exposure. The aim of the study was to examine the association between 2D:4D and women’s general and reproductive health. This analysis was conducted within a prospective pregnancy cohort study. The study population included 187 women. 2D:4D was measured directly in both hands using a digital caliper. Multivariable linear and logistic models were used to study the associations between digit ratio and the studied health characteristics. Mean age of the participants was 30.7 ± 4.9 years. The mean age at menarche was 12.9 ± 1.4 years. Right hand 2D:4D mean ± SD was 0.965 ± 0.03. Left hand 2D:4D mean ± SD was 0.956 ± 0.03. An association was found between right 2D:4D and age at menarche, with older age in women with 2D:4D ≥ mean versus 2D:4D < mean (13.2 ± 1.5 and 12.8 ± 1.3 respectively, b = 0.48, 95%CI:0.06–0.91) while controlling for ethnicity. Higher 2D:4D was also associated with heavier menses bleeding and dysmenorrhea. There is an association between 2D:4D and sub optimal reproductive characteristics, including later age at menarche, heavier menses bleeding and dysmenorrhea. These findings support the association between the intrauterine period and reproductive characteristics. Further studies are required to support our findings.
Similar content being viewed by others
Introduction
The ratio between lengths of the second and the fourth digits (index and ring fingers) (2D:4D) is a putative biomarker of prenatal testosterone and estrogen exposure1. 2D:4D is sexually dimorphic, and males’ 2D:4D is relatively shorter than females’2,3. 2D:4D is observed at as early as the end of the first trimester4,5. Relative digit length is considered steady at ages 2 to 256, although other studies suggest that 2D:4D does mildly increase during childhood but remains steady during puberty7,8.
2D:4D was suggested to be associated with Hox gene family2,3. Homeobox genes Hox a and Hox d may indirectly influence the prenatal production of androgen by controlling the differentiation of the urogenital system as well as digit development. Considering this, it was suggested that there may be an association between prenatal hormonal function and digit formation, and 2D:4D was proposed as an indicator of first trimester testosterone and estrogen levels, reflecting the Hox genes’ action on differentiation9,10.
Environmental exposure to toxicants is critical during early development stages, such as the perinatal period, in which there is a heightened vulnerability to exposures due to potential permanent effect on health and development11. Previous research showed association between prenatal hormonal environment and exposure to endocrine disrupting chemicals and 2D:4D in animals12,13 and humans2,10,14,15,16. Conversely, some studies found no support for such association17,18,19.
Assessing the prenatal hormonal environment directly from the fetus in utero is challenging because of the risk for the fetus. Therefor other methods have been used to evaluate prenatal androgen exposure, such as 2D:4D7. Various studies found associations between 2D:4D and reproductive characteristics in humans, including age at menarche20,21,22,23, puberty characteristics24, reproductive period20, age at menopause25, polycystic ovary syndrome26, severity of premenstrual symptoms27 and estradiol levels across menstrual cycle28,29. Several studies found 2D:4D to be associated with reproductive cancers25,30,31. As for general health characteristics, 2D:4D was associated with various cancers32,33, idiopathic pulmonary hypertension34 and other morbidities such as systemic lupus erythematosus35, autism spectrum disorders36, and congenital adrenal hyperplasia37,38.
Not all studies however found an association between 2D:4D in women and reproductive39,40,41,42,43 and health characteristics44,45 and there is some inconsistency in the literature regarding the direction of the association. For instance, several large studies found a negative association between 2D:4D and age at menarche20,22,23, while another found a positive association21. Due to this inconsistency the goal of the current study was to assess the association between women’s general and reproductive health and 2D:4D. Moreover, in the present cohort we studied a new population in which 2D:4D was not yet researched – women from Israel. This study aims to clarify previously disparate findings regarding the association and direction of 2D:4D and reproductive and health characteristics in women. Furthermore, by inspecting a new population it also aims to replicate previously reported associations between 2D:4D and reproductive and general health characteristics.
Methods
Study design
This analysis was conducted in the framework of The Negev Pregnancy Cohort study.
Setting
Study population included pregnant women from the Negev region in Israel. Women were recruited at a nuchal translucency clinic at Soroka University Medical Center (SUMC) to which pregnant women attend at 11–13.5 gestational weeks for a nuchal translucency ultrasound, which is a screening test for major chromosomal and nuchal cord abnormalities. These tests are routinely recommended for all pregnant women and are covered by national health insurance law, by the health maintenance organizations. Women with multi fetal pregnancies in the current pregnancy were excluded from the study. As the current study is a part of a prospective cohort study which is aimed to conduct a long term follow up on participants and their offspring, women who did not plan to give birth at SUMC were also excluded.
The study protocol was approved by SUMC IRB committee. All methods were performed in accordance with the relevant guidelines and regulations. Recruitment period occurred from October 2017 to April 2018. All eligible women were offered to participate in the study and signed an informed consent. Participants underwent anthropometric measurements and completed a comprehensive questionnaire with a trained interviewer, which included background and socioeconomic characteristics, environmental exposures and reproductive and general health characteristics. Women were compensated for their participation.
Study variables
2D:4D was the independent variable, and was directly measured in both right and left hand using a digital caliper (resolution: 0.01 mm, manufactured by FST, Germany). Finger length was measured from the proximal palm crease to the fingertip as in Auger et al. who validated the method against hand radiographies46. Additional anthropometric measurements included weight, body mass index (BMI), waist and hip circumference. Height was self- reported. Each measurement was conducted twice by the same research assistant. If there was a difference of more than 10% between measurements, a third measure was taken and the two measurements with less than 10% difference were chosen for the analysis. The intraclass correlation coefficients between each measurement were high (rt. hand 2nd: r = 0.95; rt. hand 4th: r = 0.97; lt. hand 2nd: r = 0.96; lt. hand 4thr = 0.97; p < 0.001). The Kappa between each pair of measurements was also significant (p < 0.001). A mean of both measurements was calculated and used in the analysis. One observation of 2D:4D was excluded after a cutoff of an outlier (>2 standard deviations from the mean).
Data of background and outcome variables were obtained by comprehensive questionnaires. Background information included sociodemographic variables. Outcome variables included general and reproductive health characteristics. Reproductive information included age at menarche, cycle length, menses duration, menses bleeding degree (lighter than normal, normal, heavier than normal), dysmenorrhea (defined as menstrual pain and cramps), bleeding during current pregnancy, time to pregnancy, fertility treatments for current or previous pregnancy, complications in current pregnancy such as high blood pressure, diabetes and thyroid disorders etc. General health information included ever being told by a physician or diagnosed with any health problems, based on a pre-defined list of common morbidities Such as cardiovascular disease (CVD), Anemia, thyroid disorders, herpes, migraine/headache, faint, dizziness etc.
Statistical analysis
The completed questionnaires were reviewed to verify competence. Data were de-identified, coded and entered using ACCESS data management software, and were analyzed using SPSS software (version 23.0).
In order to validate the completeness and veracity of some reported reproductive health characteristics, several questions were repeated and their answers compared in the questionnaires, including age at menarche, cycle length and time to pregnancy. Additionally, one woman with an extreme value of age at menarche of 7 was excluded from the age at menarche analysis. This woman had the following digit ratios: rt.: 0.974, lt.: 0.942.
Univariate association between 2D:4D (as a continuous variable and as above versus below mean) and outcome variables was considered with t-test for continuous outcome variables and Chi-square test for categorical outcome variables. A multivariate analysis was conducted between 2D:4D and the variables found in the univariable level to be associated with 2D:4D. All analyses were two-sided with an alpha of 5%.
Ethics approval and consent to participate
The study protocol was approved by SUMC IRB committee (0272-16-SOR). All participants signed an informed consent form.
Results
Background information
A total of 187 women were included in the study. Participant’s age ranged between 20–42 years with mean age of 30.7 ± 4.9 years. The majority of the women, 83.1%, were Jewish and 13.4% were Muslims. All anthropometric measurements were characterized with a normal distribution. Right hand 2D:4D ranged between 0.852–1.064 with mean ± SD of 0.965 ± 0.03. Left hand 2D:4D ranged between 0.879–1.067 with mean ± SD of 0.956 ± 0.03. Table 1 presents selected background characteristics of the study population separately for each hand by above versus below mean digit ratio, including demographic and anthropometric information. As can be seen, the study groups did not differ in the background characteristics.
Reproductive and general health characteristics
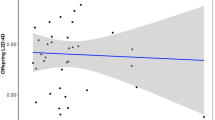
Table 2 presents reproductive and general health characteristics separately for each hand by above versus below mean digit ratio. The mean cycle length was 30.1 ± 12.3 days, the mean menses duration was 5.1 ± 1.5 days and the mean age at menarche was 12.9 ± 1.4 years. Age at menarche was associated with right 2D:4D and the correlation between age at menarche and 2D:4D (continuous format) was r (Pearson) = 0.17 (p = 0.034).
Table 3 presents the multivariable analysis for the association between 2D:4D and age at menarche. As can be seen, there was a significant association between right 2D:4D and age at menarche, while controlling for ethnicity (b = 0.48, 95%CI 0.06–0.91).
Among women who complained about heavy bleeding during menstrual period, accompanied with cramps and abdominal pain (n = 66 out of the 104 which did not take birth control pills), digit ratio was significantly higher as compared to women with no such complaints (0.96 ± 0.03 versus 0.94 ± 0.02, p < 0.01). As can be seen in Table 3, although the direction of the association between 2D:4D and heavy bleeding remained, it was no longer significant in the multivariable analysis. Women who reported having dysmenorrhea were more likely to have higher left hand 2D:4D. This association was marginally significant in the multivariable analysis (also presented in Table 3). The models were tested separately among the larger ethnic group in the study population (Jewish women), and results remained similar.
As for general health characteristics, prevalence of all morbidities was not associated with 2D:4D, besides thyroid disorders, which were more common among women with higher 2D:4D.
Discussion
In the current study an association was found between higher 2D:4D and sub-optimal reproductive characteristics, including: older age at menarche, heavy menses bleeding and dysmenorrhea.
Our study found a positive correlation between right 2D:4D and age at menarche, a result that replicates that of Oberg et al. who used a direct measurement of 2D:4D in a large study of 299 girls and found a lower median age at menarche in girls from the lowest 2D:4D tertile in comparing to the highest21. Older age at menarche may represent sub-optimal reproductive profile, and has been associated with subfecundity and infertility47. Additional studies reported an association between right 2D:4D and age at menarche, however the association they found was negative. Their findings are unlikely to have been underpowered. Kalichman et al. found in a sample of 674 women that women with 2D < 4D in both hands, had a higher age at menarche. The measurements were based on X-rays digitalized images20. Similarly, Manning et al. in a large population study of 70, 658 women found a negative association between right 2D:4D and age at menarche. Digit length measurements in that study were self-measured by the participants using a ruler23. Correspondingly, Matchock, in a study of 206 women, found that women with low right 2D:4D reported delayed age at menarche. Digit length measurements were obtained from photocopies22.
However, Muller et al. in a large study of 9,044 women25, Gooding et al. in a sample of 202 women40 and Helle in a study of 282 women41 found no association between 2D:4D and age at menarche. Digit length measurements in those studies were obtained from scans and photocopies. Likewise, Li et al.24 in a study of 318 girls found no association between 2D:4D and age at menarche using a direct measurement of the digit length. Nonetheless the study used a different measurement methodology than in the current study and examined only left hand digit ratio while left hand 2D:4D is less sensitive to prenatal hormonal environment10,23. Further studies with similar methodology are recommended to support the association and clarify its direction.
Lower 2D:4D in our population, which is characterized as a more masculine digit ratio, was associated with earlier age at menarche. On one hand younger age at menarche can mean that reproduction can begin earlier. It is noteworthy to acknowledge the Belsky et al. evolutionary theory of socialization that considers the timing of puberty as an outcome of social experience. Drawing from evolutionary biology contending that humans adapt to circumstantial conditions in ways that will increase reproductive competence, they suggest early menarche can be related to early stress through biological reaction to social conditions. They suggest that early puberty may shorten the period between puberty and actual fertility consequently organizing menstrual cycle in a manner that enables lifespan with more conceptions48.
Younger age at menarche can also mean the depletion of the eggs reserve earlier. In previous research, earlier age at menarche was associated with an increased risk for various morbidities later in life such as CVD, type 2 diabetes, metabolic syndrome and reproductive cancers49,50. The association between 2D:4D and age at menarche may enable detecting a high risk group and improve their outcomes. Although earlier age at menarche by itself is not an adverse health finding, it is a possible character of women who are at greater risk for reproductive challenges and morbidities. Our findings suggest digit ratio, which has been identified as a marker of early life environment, is another indicator of these women at risk. However, as mentioned by Richards, 2D:4D cannot be applied at an individual level but may be helpful in observing statistical trends over large populations51.
Higher 2D:4D was also associated with heavier menses bleeding and dysmenorrhea. Women with a more feminine type right 2D:4D had a higher probability to report heavier menses bleeding as compared to women with a more masculine type digit ratio of 2D:4D and women who reported having dysmenorrhea were more likely to have higher left hand 2D:4D. Heavy menstrual bleeding may lead to iron deficiency and anemia. Additionally, heavy menstrual bleeding increases the use in health care services, along with higher surgical interventions rates52,53. Previous studies have found an association between 2D:4D and menstrual characteristics. McIntyre et al. and Richards et al. found a significant positive association between right 2D:4D and estradiol levels across menstrual cycle28,29, although Klimek et al. found no such correlation43. In addition, Kaneoke et al. found a negative association between right 2D:4D and severity of premenstrual symptoms27. These findings along with our finding regarding age at menarche support the association between 2D:4D and menses characteristics. Further studies are required to support the association between 2D:4D, menses bleeding and dysmenorrhea.
A strength of our study is a direct measure of digit length, as indirect measure may distort the 2D:4D46,54. Another strength of the study is that since the nuchal translucency ultrasound test is recommended for all pregnant women and covered by the health maintenance organizations according to health insurance law, women from varied socioeconomic backgrounds attended the clinic and were recruited. Yet, our study is not without limitations. There is an under representation of the Bedouin population in the study sample. Previous studies have shown that this population is characterized with higher rates of lack of prenatal care and tend to begin prenatal care around mid-pregnancy55,56. Due to the importance of collecting data at the beginning of pregnancy, recruitment to the study was done at the end of the first trimester. Another limitation in our study is that since recruitment took place in a clinic for pregnant women, all women in our study are fertile, and only a small number of the women were fertility challenged. An under representation of extreme cases of infertility or adverse reproductive outcomes is a possibility, potentially leading to an under estimation of the true association between 2D:4D and reproductive characteristics. Additionally, external validity of the cut points for dichotomizing 2D:4D is questionable, as the ratio is population specific, and the cut points used in the current study may not be relevant in other populations. Still our finding suggest high digit ratio is associated with sub optimal reproductive characteristics, a finding that has been reported in other populations.
To conclude, there is an association between 2D:4D and sub optimal reproductive characteristics, including later age at menarche, heavier menses bleeding and dysmenorrhea. These findings support the association between 2D:4D and reproductive characteristics in women. Our findings strengthen the association between the intrauterine period and reproductive characteristics. In order to support our findings and clarify the inconsistency in the literature, further studies in other populations are required.
Data availability
Due to ethics committee restrictions data is not available.
References
Manning, J. T. In Digit ratio: A pointer to fertility, behavior, and health (Rutgers University Press, 2002).
Manning, J. T., Scutt, D., Wilson, J. & Lewis-Jones, D. I. The ratio of 2nd to 4th digit length: a predictor of sperm numbers and concentrations of testosterone, luteinizing hormone and oestrogen. Hum. Reprod. 13, 3000–3004 (1998).
Manning, J. T. Resolving the role of prenatal sex steroids in the development of digit ratio. Proceedings of the National Academy of Sciences 108, 16143–16144 (2011).
Galis, F., Ten Broek, C. M., Van Dongen, S. & Wijnaendts, L. C. Sexual dimorphism in the prenatal digit ratio (2D: 4D). Arch. Sex. Behav. 39, 57–62 (2010).
Ronalds, G., Phillips, D., Godfrey, K. M. & Manning, J. T. The ratio of second to fourth digit lengths: a marker of impaired fetal growth? Early Hum. Dev. 68, 21–26 (2002).
Manning, J. T., Henzi, P. & Bundred, P. E. The ratio of 2nd to 4th digit length: a proxy for testosterone, and susceptibility to HIV and AIDS? Med. Hypotheses 57, 761–763 (2001).
McIntyre, M. H. The use of digit ratios as markers for perinatal androgen action. Reprod. Biol. Endocrinol. 4, 10 (2006).
Trivers, R., Manning, J. & Jacobson, A. A longitudinal study of digit ratio (2D: 4D) and other finger ratios in Jamaican children. Horm. Behav. 49, 150–156 (2006).
Manning, J. T. & Bundred, P. E. The ratio of 2nd to 4th digit length: a new predictor of disease predisposition? Med. Hypotheses 54, 855–857 (2000).
Lutchmaya, S., Baron-Cohen, S., Raggatt, P., Knickmeyer, R. & Manning, J. T. 2nd to 4th digit ratios, fetal testosterone and estradiol. Early Hum. Dev. 77, 23–28 (2004).
Mallozzi, M., Bordi, G., Garo, C. & Caserta, D. The effect of maternal exposure to endocrine disrupting chemicals on fetal and neonatal development: A review on the major concerns. Birth Defects Res. C. Embryo. Today 108, 224–242 (2016).
Auger, J. et al. Environmental levels of oestrogenic and antiandrogenic compounds feminize digit ratios in male rats and their unexposed male progeny. Proceedings of the Royal Society of London B: Biological Sciences 280, 20131532 (2013).
Zheng, Z. & Cohn, M. J. Developmental basis of sexually dimorphic digit ratios. Proceedings of the National Academy of Sciences, 201108312 (2011).
Wainstock, T. et al. Exposure to PBB-153 and Digit Ratio. Early Hum. Dev. 103, 33–35 (2016).
Ventura, T., Gomes, M. C., Pita, A., Neto, M. T. & Taylor, A. Digit ratio (2D: 4D) in newborns: influences of prenatal testosterone and maternal environment. Early Hum. Dev. 89, 107–112 (2013).
Barona, M., Kothari, R., Skuse, D. & Micali, N. Social communication and emotion difficulties and second to fourth digit ratio in a large community-based sample. Molecular autism 6, 68 (2015).
Hickey, M. et al. Maternal and umbilical cord androgen concentrations do not predict digit ratio (2D: 4D) in girls: a prospective cohort study. Psychoneuroendocrinology 35, 1235–1244 (2010).
Hollier, L. P. et al. Adult digit ratio (2D: 4D) is not related to umbilical cord androgen or estrogen concentrations, their ratios or net bioactivity. Early Hum. Dev. 91, 111–117 (2015).
Slama, N., Warner, M., Mocarelli, P., Brambilla, P. & Eskenazi, B. The 2nd to 4th digit length ratio (2D: 4D) among children of Seveso women exposed to 2, 3, 7, 8-tetrachlorodibenzo-p-dioxin. Early Hum. Dev. 131, 45–50 (2019).
Kalichman, L., Batsevich, V. & Kobyliansky, E. 2D: 4D finger length ratio and reproductive indices in a Chuvashian population. Am. J. Hum. Biol. 25, 617–621 (2013).
Oberg, A. S. & Villamor, E. Low digit ratio predicts early age at menarche in Colombian schoolgirls. Paediatr. Perinat. Epidemiol. 26, 448–455 (2012).
Matchock, R. L. Low digit ratio (2D: 4D) is associated with delayed menarche. Am. J. Hum. Biol. 20, 487–489 (2008).
Manning, J. T. & Fink, B. Is low digit ratio linked with late menarche? Evidence from the BBC internet study. Am. J. Hum. Biol. 23, 527–533 (2011).
Li, T. et al. The associations between left-hand digit ratio (2D: 4D) and puberty characteristics among Chinese girls. Early Hum. Dev. 130, 22–26 (2019).
Muller, D. C. et al. Second to fourth digit ratio (2D: 4D), breast cancer risk factors, and breast cancer risk: a prospective cohort study. Br. J. Cancer 107, 1631 (2012).
Cattrall, F. R., Vollenhoven, B. J. & Weston, G. C. Anatomical evidence for in utero androgen exposure in women with polycystic ovary syndrome. Fertil. Steril. 84, 1689–1692 (2005).
Kaneoke, Y., Donishi, T., Iwahara, A. & Shimokawa, T. Severity of premenstrual symptoms predicted by second to fourth digit ratio. Frontiers in medicine 4, 144 (2017).
Richards, G., Klimek, M., Jasienska, G. & Marcinkowska, U. M. Digit ratio (2D: 4D) and circulating testosterone, oestradiol, and progesterone levels across the menstrual cycle. Early Hum. Dev. 117, 68–73 (2018).
McIntyre, M. H., Chapman, J. F., Lipson, S. F. & Ellison, P. T. Index‐to‐ring finger length ratio (2D: 4D) predicts levels of salivary estradiol, but not progesterone, over the menstrual cycle. American Journal of Human Biology: The Official Journal of the Human Biology Association 19, 434–436 (2007).
Hong, L. et al. Digit ratio (2D:4D) in Chinese women with breast cancer. Am. J. Hum. Biol. 26, 562–564 (2014).
Brabin, L., Roberts, S. A., Farzaneh, F., Fairbrother, E. & Kitchener, H. C. The second to fourth digit ratio (2D:4D) in women with and without human papillomavirus and cervical dysplasia. Am. J. Hum. Biol. 20, 337–341 (2008).
Bunevicius, A. et al. Digit ratio (2D:4D) in primary brain tumor patients: A case-control study. Early Hum. Dev. 103, 205–208 (2016).
Nicolas Hopp, R. et al. Digit ratio (2D:4D) is associated with gastric cancer. Early Hum. Dev. 89, 327–329 (2013).
Yamamoto, T. et al. Relationship between digit ratio and idiopathic pulmonary arterial hypertension in Japanese Women. Journal of Vascular Medicine & Surgery (2015).
Doe, K. et al. Second-to-fourth Digit Ratio in Systemic Lupus Erythematosus. J. Rheumatol. 42, 826–828 (2015).
Masuya, Y. et al. Sex-different abnormalities in the right second to fourth digit ratio in Japanese individuals with autism spectrum disorders. Mol. Autism 6, 34–x. eCollection 2015 (2015).
Brown, W. M., Hines, M., Fane, B. A. & Breedlove, S. M. Masculinized finger length patterns in human males and females with congenital adrenal hyperplasia. Horm. Behav. 42, 380–386 (2002).
Ökten, A., Kalyoncu, M. & Yariş, N. The ratio of second-and fourth-digit lengths and congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Early Hum. Dev. 70, 47–54 (2002).
Velez, M. P., Arbuckle, T. E., Monnier, P. & Fraser, W. D. Female digit length ratio (2D: 4D) and time-to-pregnancy. Human Reproduction 31, 2128–2134 (2016).
Gooding, D. C. & Chambers, B. H. Age of pubertal onset and 2nd to 4th digit ratios: Preliminary findings. Early Hum. Dev. 116, 28–32 (2018).
Helle, S. Does second‐to‐fourth digit length ratio (2D: 4D) predict age at menarche in women? Am. J. Hum. Biol. 22, 418–420 (2010).
Lujan, M. E., Podolski, A. J., Chizen, D. R., Lehotay, D. C. & Pierson, R. A. Digit ratios by computer-assisted analysis confirm lack of anatomical evidence of prenatal androgen exposure in clinical phenotypes of polycystic ovary syndrome. Reproductive Biology and Endocrinology 8, 156 (2010).
Klimek, M. et al. Digit ratio (2D: 4D) does not correlate with daily 17β‐estradiol and progesterone concentrations in healthy women of reproductive age. Am. J. Hum. Biol. 27, 667–673 (2015).
Kyriakidis, I., Papaioannidou, P., Pantelidou, V., Kalles, V. & Gemitzis, K. Digit ratios and relation to myocardial infarction in Greek men and women. Gend. Med. 7, 628–636 (2010).
Wu, X. et al. The ratio of second to fourth digit length (2D: 4D) and coronary artery disease in a Han Chinese population. International journal of medical sciences 10, 1584 (2013).
Auger, J. & Eustache, F. Second to fourth digit ratios, male genital development and reproductive health: a clinical study among fertile men and testis cancer patients. Int. J. Androl. 34, 49 (2011).
Guldbrandsen, K. et al. Age of menarche and time to pregnancy. Human Reproduction 29, 2058–2064 (2014).
Belsky, J., Steinberg, L. & Draper, P. Childhood experience, interpersonal development, and reproductive strategy: An evolutionary theory of socialization. Child Dev. 62, 647–670 (1991).
Walvoord, E. C. The timing of puberty: is it changing? Does it matter? Journal of Adolescent Health 47, 433–439 (2010).
Luijken, J., van der Schouw, Yvonne, T., Mensink, D. & Onland-Moret, N. C. Association between age at menarche and cardiovascular disease: A systematic review on risk and potential mechanisms. Maturitas 104, 96–116 (2017).
Richards, G. Some Questions About the Replicability and Practical Applications of Digit Ratio (2D: 4D) Research (2019).
Davies, J. & Kadir, R. A. Heavy menstrual bleeding: An update on management. Thromb. Res. 151, S70–S77 (2017).
Bitzer, J., Heikinheimo, O., Nelson, A. L., Calaf-Alsina, J. & Fraser, I. S. Medical management of heavy menstrual bleeding: a comprehensive review of the literature. Obstet. Gynecol. Surv. 70, 115–130 (2015).
Ribeiro, E., Neave, N., Morais, R. N. & Manning, J. T. Direct versus indirect measurement of digit ratio (2D: 4D) a critical review of the literature and new data. Evolutionary Psychology 14, 1474704916632536 (2016).
Abu-Ghanem, S. et al. Lack of prenatal care in a traditional community: trends and perinatal outcomes. Arch. Gynecol. Obstet. 285, 1237–1242 (2012).
Sheiner, M., Hallak, I. & Twizer, M. Mazor, Miriam Katz, Ilana Shoham-Vardi, E. Lack of prenatal care in two different societies living in the same region and sharing the same medical facilities. Journal of Obstetrics and Gynaecology 21, 453–458 (2001).
Acknowledgements
The authors wish to acknowledge Hilel Vardi from the Department of Public Health, Faculty of Health Sciences, Ben-Gurion University of the Negev, for his assistance and statistical advice. The Environment and Health Fund (EHF) Israel [grant number RPGA 1603]; The Environment and Health Epidemiology (EHE) Research Center, Faculty of Health, Ben-Gurion University of the Negev, Israel, supported this work.
Author information
Authors and Affiliations
Contributions
M.T. designed, collected, analyzed, interpreted and drafted the initial manuscript. E.S. designed, collected and interpreted data. T.W. designed, collected, analyzed and interpreted data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tabachnik, M., Sheiner, E. & Wainstock, T. The association between second to fourth digit ratio, reproductive and general health among women: findings from an Israeli pregnancy cohort. Sci Rep 10, 6341 (2020). https://doi.org/10.1038/s41598-020-62599-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-62599-3
This article is cited by
-
Thyroid diseases and second to fourth digit ratio in Polish adults
Scientific Reports (2021)
-
Second to fourth (2D:4D) digit ratio and their relationships among a mother and child population in Ghana
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.