Abstract
This multicentre retrospective study examined the effects of adjunct yoga-treatment in achieving composite cardiovascular goals for type 2 diabetes (T2D), set forth by the American Diabetes Association (ADA) in rural Indian settings. Records were extracted for 146 T2D patients, aged ≥20–70 years, and treated under the “Apollo Total Health Programme” for rural diabetes management, for the period April 2016 to November 2016. The study cohort comprised of two treatment groups (n = 73 each); non-yoga group (standard of care) and yoga group (adjunct yoga-treatment). Propensity score matching was applied between the study groups to define the cohort. Composite cardiovascular scores were based on the combination of individual ADA goals; A1c < 7%, blood pressure (BP) < 140/90 mmHg, stringent BP (<130/80 mmHg) and lipid, LDL-C < 100 mg/dl [risk factor for atherosclerotic cardiovascular disease]. Logistic regression was used to compare between the two treatment groups. Compared to standard of care, adjunct yoga-treatment was found to significantly facilitate the attainment of ADA composite score by 8-fold; A1c, ~2-fold; LDL-C, ~2-fold; BP < 140/90 mmHg and <130/80 mmHg by ~8-and ~6-fold respectively. This study provides the first evidence for significant efficacy of adjunct yoga-treatment for the attainment of favourable treatment goals for T2D in rural Indian settings. Clinical Trial Registration Number: CTRI/2020/02/0232790
Similar content being viewed by others
Introduction
Type 2 Diabetes (T2D) is a chronic progressive metabolic disease, pathophysiologically hallmarked by insulin resistance and hyperglycemia, and clinically underlined by associated severe macrovascular and microvascular ramifications1. According to the current estimates of the 8th edition of the atlas, International Diabetes Federation (IDF), 425 million people are afflicted by T2D across the globe2. As well-reflected in the current IDF estimates of 2018, with 72.95 million resident T2D populations, India is one of the most severely afflicted countries with the epidemic. Urbanization and change of lifestyle are attributed as the major underlying causes of this rising epidemic1,3,4.
Efficient diabetes care is a crucial aspect of the disease owing to its progressive nature5,6,7. Intensive glycemic control delays development and aids in prevention of late T2D complications5,8. However, glycemic control is not a stand-alone measure for efficient T2D care6,7. The compound pathophysiology of T2D is associated with many other deranged metabolic indices contributing to the development of cardiovascular comorbidities1,9. The most effective approach towards reduced mortality and morbidity in T2D appears to be comprehensive risk factor reduction targeting glycemic control, management of blood pressure and dyslipidemia9,10. These factors also underlie the guidelines for Standards of Medical Care issued towards efficient cardiovascular control in T2D by American Diabetes Association (ADA) which are updated annually in the month of January7. ADA guidelines recommend a combined target for [A1c < 7% and blood pressure (BP) < 140/90 mmHg (older cut off for BP < 130/80 mmHg) for diabetes care. Though the recent guidelines of lipid management do not specify LDL-C targets, the guidelines recommended LDL-C cut-off as <100 mg/dl for effective cardiovascular control against atherosclerotic cardiovascular disease7. Despite of these guidelines, at least one-third of patients with T2DM fail to achieve their ADA goals11,12,13. The ultimate success of treatment algorithms of T2D is strongly associated with concomitant synergistic lifestyle changes along with pharmacotherapy14. According to current ADA guidelines, lifestyle management, with medical nutrition therapy and physical activity, is a fundamental component of diabetes care6. These guidelines also recommend incorporation of yoga, the ancient skillset of Indian origin, into the regimen of physical activity based on individual preferences5. Yoga is an ancient Indian practice that emphasizes balancing of various aspects (like physical, mental, emotional, and spiritual) of an individual.
South Asian ethnicity including Indians has been characterized as one of the most challenging population for diabetes care with suboptimal status3,14. Though initially considered a “disease of opulence”, the recent trends suggest that diabetes has significantly impacted rural India, characterized by inadequate health care, and poverty15,16. The recent visibility of T2D epidemic in rural India notifies an increasing trend in the prevalence estimates; escalated from 1% to 4–10% in the year and reaching as high as 13.2% in an earlier report16. India is an agricultural nation, with 72.2% of the population residing in its rural sector, hence the trending high prevalence of the rural diabetes epidemic are highly alarming16. Several distinct cultural and socioeconomic factors define the epidemic of T2D in rural India17. Response and efficacy of lifestyle interventions are governed by cultural practices as well as genetic/ethnic makeup18. India is a vast country and an amalgamation of various social, cultural and sub-ethnic groups. In view of the reported high receptivity of yoga on diabetes management in Asians Indians3, we aimed to evaluate the effectiveness of this cost-effective lifestyle treatment in the marginalized rural clinical settings of Southern India.
Results
Baseline Characteristics
Records of a total of 146 T2D patients were retrieved. The mean age of the study cohort was 55.61 ± 10.90 years, the majority were female 64.40% (n = 94) , and 76.03% (n = 111) belonged to low socioeconomic status. The recruited study cohort had an average duration of diabetes of ~6 years. According to the ADA criteria, 54.79% (n = 80) of the total study cohort was found to be above recommended A1c targets (≥7.0%, 53 mmol/ml), 81.51% (n = 119) above BP1 targets (≥130/80 mmHg), 47.26% (n = 69), above BP2 targets (≥140/90 mmHg) and 47.94% (n = 70) above lipid targets (LDL ≥ 100 mg/dl)19. Overall, at baseline, 93.83% (n = 137) and 85.62% (n = 125) of the study cohort was found to be above combined ADA composite scores 1 and 2, respectively. The cohort was also observed to have generalized obesity with a mean BMI of 26.69 ± 4.58 Kg/m2. Importantly, 85.62% (n = 125) of the study cohort was found to be overweight/obese according to the Asian cut off for BMI (≥23 kg/m2)20. At baseline, subjects in the yoga group had significantly lower DBP levels than the non-yoga group (yoga, 80.66 ± 9.30 mmHg vs. 84.52 ± 10.12 mmHg; P = 0.032) but were similar to the control group with respect to other parameters (Table 1).
Effect of Yoga treatment on the attainment of ADA-laid goals
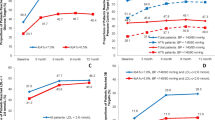
Yoga treatment was found to have a significant beneficial effect on attainment of the composite ADA goal, reflected by an increase of 2.74% [baseline, 6.85% (n = 5) to follow-up, 9.59% (n = 7)] in the number of subjects meeting the composite score 1, whereas the control group exhibited a pronounced deterioration by 4.11% [baseline (5.48%), n = 4) to follow-up (1.37%, n = 1) (Table 2)]. Similarly, there was an increase of 12.33% [baseline, 15.07% (n = 11) to follow-up, 27.40% (n = 20)] in the number of subjects meeting the composite score 2, whereas the control group exhibited a pronounced deterioration by 8.22% [baseline 13.70%, (n = 10) to follow-up 5.48%, (n = 4) (Table 2)]. When analysed by multiple regression, yoga treatment was found to be 10-fold (OR = 10.20, 95% CI = 0.69–174.19) borderline significant (P = 0.060) and ~8-fold (OR = 8.22, 95% CI = 2.02–33.49), statistically significant (P = 0.003), effective towards attaining the favourable composite ADA score 1 and 2, respectively (Table 2).
With respect to the status of A1C goals of ADA (<7%), 46.58% (n = 34) subjects were found to meet criteria for in the yoga group at baseline, however, the percentage increased to 54.79% (n = 40) at follow-up (Table 2). In the non-yoga group, the percentage of subjects with A1c criteria decreased from 43.84% (n = 32) to 36.99% (n = 27) (Table 2). The difference in the distribution between the patients meeting ADA criteria for A1c was statistically significant between yoga and non-yoga treatment groups at the follow-up (P = 0.046). When analysed by multiple logistic regression, modelled by covariates, age, sex, duration of diabetes, socioeconomic status, baseline A1c values, yoga treatment was found to be significantly associated with the ~2-fold (OR = 2.44, 95% CI = 1.19–5.00, P = 0.015) higher chances of attainment of favourable A1c cut off (<7%) as compared to standard of care (Table 2).
The percentage of subjects who met the ADA-criteria with respect to favourable LDL-C, < 100 mg/dl, increased from 52.05% (n = 38) to 54.79% (n = 40) in the yoga group (Table 2). However, in the non-yoga group, there was a decrease from 52.05% (n = 38) to 38.36% (n = 28) in the number of subjects who met the LDL-C criteria (Table 2). The distribution of patients with favourable LDL-C values was not significant between yoga and non-yoga groups at the follow-up (Table 2). However, when analysed by logistic regression, adjusted for covariates and, baseline lipid status, yoga treatment was found to be significantly associated with the ~2-fold (OR = 2.22, 95% CI = 1.06–4.68, P = 0.035) increased chances for the attainment of favourable LDL-C outcome (<100 mg/dl) as compared to standard of care alone (Table 2).
We assessed the BP outcomes with old and revised favourable cut-offs recommended by ADA (Table 3). When analysed with old cut-off (<130/80 mm Hg), we could observe a pronounced increase in the percentage of subjects meeting the favourable BP outcome from 21.92% (n = 16) to 34.25% (n = 25) in the yoga group (Table 2). On the contrary, in the non-yoga group, the number of T2D patients who met BP criteria of <130/80 mm Hg decreased from 15.07% (n = 11) to 8.22% (n = 6) (Table 2). When analysed by logistic regression, yoga treatment was found to be associated with ~6.4-fold (OR = 6.37, 95% CI = 2.24–18.08, P = 0.001) increase the chances of favourable BP cut-offs (<130/80) at follow-up. When analysed with revised new BP cut-off (<140/90 mm Hg), we could observe a pronounced increase in the percentage of subjects meeting the favourable BP outcome from 60.27% (n = 44) to 84.93% (n = 62) in the yoga group (Table 2), yoga treatment was also found to be associated with 8.28-fold (95% CI, 3.52–19.48, P < 0.0001) increased chances for the revised favourable BP cut-offs,. In the non-yoga group, the number of T2D patients who met BP criteria decreased from 45.21% (n = 33) to 39.73% (n = 29) (Table 2).
We also analysed the status of cardiovascular control for the subgroup of study cohort with uncontrolled diabetes (A1c ≥ 8.0%), n = 44. We could observe 63.16% success towards attainment of lipid goal (LDL < 100 mg/dl) and 26.32% for BP targets (130/80 mmHg) 89.47% for BP target (140/90) by 6-months of yoga treatment (data not shown). However, the controls exhibited deterioration with respect to these goals (data not shown).
Effect of yoga treatment as compared to standard of care was demonstrated with respect to the attainment of favourable BMI cut-off (<23 Kg/m2) for Asians (Table 2). When analysed by logistic regression, yoga treatment was found to be associated with 62-fold (OR = 61.73, 95% CI = 3.19–1193) increased chances of attainment of the favourable BMI cut-off over a period of 6 months (Table 2).
Outcomes in continuous measures
Over the study period of around 6-months, the yoga-group exhibited significant within-group beneficial mean changes and percent changes in A1c, −0.50%, (−5.03%); FBS, −11.27 mg/dL (−8.00%); PPBS, −25.51 (−−11.44%); Wt., −2.91 (-4.18%); BMI, −1.14 Kg/m2 (−4.04%); SBP, −5.30 (−3.02%); DBP, −4.57 (−4.60%); TC, −2.94 mg/dl (−1.49%), HDL-c, −0.70 mg/dl (−1.49%) (Table 3). With respect to triglyceride (TG), we could observe an unexpected increase in the mean TG levels in the yoga group, 11.74 ± 3.72 mg/dl (31.94%) (Table 3). We observed pronounced worsening of the metabolic variables in the non-yoga group (Table 3). We could observe a deteriorating trend in the mean difference of these variables from baseline in the non-yoga group (Table 3). Significant within-group differences were also observed in the non-yoga group for FBS, 11.14 mg/dl (18.31%); BMI, 0.76 Kg/m2 (4.06%); HDL-c, −2.51 mg/dl (−4.72%), and TG, 67.70 mg/dl (59.01%). Between-study group differences between yoga group and non-yoga group very significant with respect to all the studied parameters (Table 3).
Discussion
Type 2 diabetes is associated with vascular complications and enhanced risk of cardiovascular events. Therefore, ADA has suggested a multifactorial targeted approach towards efficient management of T2D [glycemic, lipid, and blood pressure]5,7. Use of such composite endpoints in clinical studies also help in the better understanding of the net effect of an intervention or a therapy rather than individual endpoints21,22. Further, studies targeting composite endpoints have been reported to have higher statistical efficiency as compared to those with individual endpoints22. We hereby highlight the grim status of diabetes management with respect to the attainment of the ADA laid primary treatment goals, in rural Indian settings. At baseline of the study, 54.79% was found to be above ADA laid A1c targets (≥7.0%), 47.26% was found to be above lipid targets (LDL-C > 100 mg/dl) and 81.51% were found to be above BP cut-offs of>130/80 mmHg, and 47.26% were found to be above the revised BP cut-offs (<140/90 mmHg)5. Overall, only 6.16% (n = 9) of the total study cohort was found to be meeting the composite score of all the three treatment targets at the baseline. However, a prior report by Menon et al.15, indicated only 1–3% of Indian T2D population achieving the combined treatment goals of ADA in an urban clinical setup. The pathophysiological link between obesity and T2D was also evident in the study cohort, wherein, 62.33% (n = 91) of the cohort sample was found to be obese. As majority of the cohort sample (~80%), belonged to low socioeconomic status23, this poor status of cardiovascular risk control could be attributed to lack of pharmacologic management, governed by poor awareness and socioeconomic status in the rural Indian settings.
Lifestyle management plays an essential role in the efficient control of diabetes status6,24. Yoga, as a lifestyle intervention has been reported to lead to beneficial health outcomes related to cardiovascular and metabolic disorders including T2D25,26. Based on its high reported receptivity and cost-effectiveness, yoga holds a strong potential as a lifestyle management skill in Indian scenario3. This is the first report wherein the efficacy of yoga treatment was assessed in aiding the cardiovascular fitness with respect to achievement of ADA laid primary treatment goals of T2D in rural Indian settings. Our findings reflect a magnitude of success of 10.96% attained by 6-months of yoga treatment on overweight/obese T2D Indian rural cohort. However, Ikramuddin et al. reported a success rate of 19% with respect to ADA composite endpoint over a period of 12 months on patients with uncontrolled T2D27. Further, compared to usual care, 6-months of yoga treatment was also found to be associated with 8-fold higher (OR = 8.22, 95% CI = 2.02–33.49) success towards the attainment of ADA composite scores (with revised BP cut-off of 140/90 mmHg) in rural Indian settings. With respect to individual composite goals, 6 months of yoga treatment was found to have a higher likelihood of attainment of A1c goal by ~2-fold (OR = 2.44, 95% CI = 1.19–5.00); LDL-C by ~2-fold (OR = 2.22, 95% CI = 1.06–4.68); blood pressure<140/90 mmHg by ~8-fold [OR = 8.28, 95% CI, 3.52–19.48)] in rural T2D population compared to standard of care. The observed 2-fold higher potential of yoga-treatment as compared to standard of care towards attainment of LDL-c targets in the rural Indian T2DM cohort deserves clinical attention. Control of dyslipidemia in Indian T2DM patients has been reported to be very poor; with almost half of them not reaching their LDL-C goal28. These findings are important as Coronary Artery Disease (CAD) mortality remains high in the Indian patients with T2DM. Similarly, the observed 8-fold increased impact of yoga on BP control as compared to standard of care is an important clinical outcome. Hypertension is a prevalent co-morbidity in T2D patients associated with an increased risk of cardiovascular events and mortality29,30. This coexistence has been reported to enhance the risks of nephropathy and retinopathy31,32.
As previously reported by Ikramuddin et al., intense lifestyle intervention could aid in 31% success towards attainment of glycemic, 70% for lipid and 70% for BP targets (130/80 mmHg) over a period of 12 months in a mixed ethnic population of uncontrolled T2D (HbA1c ≥ 8.0%)27. Interestingly, in the present subgroup of patients with uncontrolled T2D, HbA1c ≥ 8.0% yoga treatment of 6 months duration was found to be effective with 26.32% success in attainment of glycaemic control, 63.16% for lipid, and 26.32% for BP goals (130/80 mmHg). These findings indicate that if assessed for long-term effects, yoga treatment could match the magnitude of the potential of intense lifestyle-interventions as described for overweight/obese uncontrolled T2D patients27.
Glycemic control is the primary target of diabetes management strategies towards prevention of the devastating complications such as blindness, kidney failure and amputations7,9. We could observe significant absolute decrease in mean A1c% by 0.5 in the yoga group over a period of 6 months. The magnitude of reduction by 0.5% in A1c holds strong clinical significance, based on the reported epidemiological association between 1% reduction in the A1c value with 14% reduction in myocardial infarction (MI), 21% reduction in diabetes-related mortality and 37% reduction in microvascular complications33. Further significant and beneficial yoga treatment-induced mean percentage reductions in SBP (4.33%); DBP (5.66%); and TC (1.65%) could also be observed in the present study. These findings support earlier reported beneficial cardiovascular effects of yoga25,26.
Weight loss remains a major challenge in diabetes due to the complex interplay between metabolic, neuroendocrine and psychological factors34. In a prior study intensive lifestyle intervention of 1 year was reported to achieve an average 8.6% weight loss along with significant reduction of A1C, and CVD risk factors, with sustained effects up to 4 years24. In the present study, we could observe a 4.18% reduction in weight over a period of 6 months under yoga-treatment. Our results highlight the equivalent potential of yoga to intense weight-loss intended lifestyle interventions in overweight/obese T2D patients. A favourable and differential effect of 61-fold (OR = 61.73, 95% CI = 3.19–1193) was also observed for BMI outcome of <23 kg/m2 in the yoga group against standard of care. The observed significant impact of yoga-treatment on BMI outcome in diabetes bears strong clinical relevance as weight management is an important component of efficient diabetes care7. Further, weight loss through lifestyle changes remains the first-line therapy for T2DM34. Available observational evidence suggest various clinical benefits of weight loss in diabetes including improvement in glycemic control, reduced risk of cardiovascular events alongwith improvements in quality of life, mobility, and physical function35,36. However, we could not assess the sustenance of weight-related effects of yoga in this short-duration study. Based on the proposed self-regulation modality of yoga, wherein yoga could lead to repatterning of hedonic neurocircuitries, we speculate sustained weight-loss effects with long-term yoga-treatment37.
The study is limited by its observational nature. The difference-in-means method used to establish the equivalence between the study groups could be limited in its capacity to control the confounding by baseline variables. To this end, we conducted propensity score matching with “nearest neighbour” method for matching of the treatment groups for key covariates. Further, logistic regression was also done to adjust for the effect of the covariates to assess the study outcomes. The observed poor outcome in the standard of care group deserves attention of physicians and clinicians working in the rural sector of India. The poor outcome could possibly be attributed to poor adherence to medication and prescribed physical activity in the rural T2D population suggesting that there is a need to explore strategies to facilitate adherence with the patients/caregivers17. Since Indian patients were found to be receptive to yoga, yoga-based treatment could be a pragmatic solution for effective diabetes management. Based on the epidemic proportions of T2DM in India, there is an urgent need to conduct a large, prospective, long-term study of the efficacy of yoga on attaining all of the ADA goals in the rapidly increasing T2DM population. Early initiation of yoga treatment to target adequate diabetes care has the potential to prevent the devastating complications including not just the microvascular but also loss of time from work and quality of life.
Methods
Cohort identification
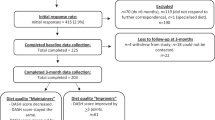
The study was part of an ongoing service activity defined as the “Total Health Programme” (THP) India’s first integrated rural healthcare service delivery network, initiated by the Apollo Group (https://www.apollohospitals.com/corporate/initiatives/csr-at-apollo/total-health-programme). THP aimed at patients for various diseases across the adopted villages for effective disease management in collaboration with Swami Vivekananda Yoga Anusandhana Samsathana (S-VYASA) (http://svyasa.edu.in/). During the month of April/May 2016, 324 adults diagnosed with T2D, aged ≥20 years to 70 years, from 12 nearby villages of the Chittoor district, Andhra Pradesh, India, were originally referred to the Apollo health scheme for diabetes management. T2D was defined as per the American Diabetes Association criteria19. When the records were screened, out of 277 initially referred patients, only 150 were found to complete regular supervised yoga treatment, and amongst them 73 only had sufficient laboratory data until November 2016. Figure 1 details the steps involved in cohort selection. Medical records of these 73 patients were retrieved for the study. Patients undergoing insulin treatment, pregnant or breastfeeding, or who had severe vascular, hepatic, renal diseases or cancer were excluded from the study. Patients with atherosclerotic cardiovascular disease (ASCVD)7 were also excluded. Records of an equal number of T2D patients were retrieved as a non-yoga group who opted for only standard of care treatment at the rural Apollo clinics during the same period of time. Difference-in-means of the age, the proportion of sex and blood A1c levels were matched between yoga and non-yoga groups before finalizing the selection of the cohort sub-groups (n = 73 each). This was followed by matching the sub-groups through propensity score matching. Thus, we defined a cohort of 146 T2D patients, diagnosed with T2D as per ADA criteria19. Both yoga and non-yoga groups were followed from the (index date; date of first check up with prescribed treatment) until the end of 6 months. Parameters of interest were included at the time of admission/index date (baseline) and at an average of 6 months of follow-up. Written consent was obtained from the study subjects and the study was approved by the Institutional Ethics Committee of Swami Vivekananda Yoga Anusandhana Samsathana, Bengaluru, India. Informed consent was obtained from all the study subjects. All methods were performed in accordance with the relevant guidelines and regulations. The study was registered with ClinicalTrials.gov (NCT01212133); registration number: (CTRI/2020/02/0232790).
Measures
The duration of yoga- treatment was approximately six months. Primary parameters of interest were the follow-up status of revised ADA laid treatment goals of diabetes;A1C < 7.0% (<53 mmol/mol), and BP cut- offs (<140/90 mmHg). Additionally based on ADA definition of risk factors of Atherosclerotic Cardiovascular Disease (ASCVD)7, the treatment goals also included <100 mg/dl of LDL-C, and stringent BP goals (<130/80 mmHg). Composite score was defined based on the meeting of all the target goals. Secondary outcomes were continuous measures of A1c, FBS (fasting blood glucose), PPBS (postprandial blood glucose), LDL-Cholesterol (LDL-C), SBP, DBP, weight, total cholesterol (TC), triglyceride (TG) diastolic blood pressure (DBP), and body mass index (BMI). Patient demographic and anthropometric information including age, sex, socioeconomic status, duration of diabetes, medication, weight, blood pressure, height was also extracted. BMI was calculated as weight in kilograms divided by the square of height in meters. Asian cut-off for BMI (≥25 kg/m2) was used to define obesity20.
Intervention
The administration of yoga was carried out at Apollo rural and satellite clinics (https://www.apollohospitals.com/corporate/initiatives/csr-at-apollo/total-health-programme) for T2D patients from nearby villages. Non-yoga group, the T2D patients received the standard of care for diabetes as per ADA guidelines from a physician-coordinated team5. The patients were also referred for diabetes self-management education and support for strengthening and empowering their diabetes knowledge and self-care behaviors as per ADA guidelines. The yoga treatment given to the patients was derived from a validated integrated yoga module developed by Angadi et al.38. The treatment protocol included daily supervised administration of yoga sessions for one hour. The yoga module was comprised of loosening practices, asanas, pranayama, relaxation techniques, and meditation; (detailed protocol has been appended as a supplement table no. 1). Only certified yoga therapists were involved in the administration of the yoga-treatment. Both the yoga and non-yoga treatment groups were followed from the date of admission into the clinics, till November 2016.
Statistical analyses
Missing data were minimal. Continuous variables were tested for normality with the Shapiro-Wilk test. We used descriptive statistics with mean and 95% confidence intervals [CIs]), and standard, or percentages (numbers) for representation of T2D patient’s baseline characteristics. Categorical variables were described using frequencies. Socioeconomic status was determined by using Kuppuswamy’s scale22. Outcome measures were compared using Analysis of covariance (ANCOVA) to adjust for baseline measures and to provide an unbiased estimate of the mean group differences. A General linear model (GLM) for multivariate analysis was developed with covariates of baseline values of the outcome variables, age, medication and duration of diabetes. P-value of < 0.05 was set as significant and < 0.0001 was set as highly significant. Statistical analysis was performed using SPSS version 21.0, Microsoft Excel-2013 and R studio version 1.1.423. For comparisons within treatment groups from baseline to follow-up, a Wilcoxon signed rank test was performed. Propensity scores were calculated for each subject based on primary baseline covariates known to be associated with diabetes treatment and/or the study outcomes, including age, sex, socioeconomic status, disease duration, medication, and biochemical parameters using the “nearest neighbour” method (Appendix, supplementary material). Logistic regression was then used to identify predictors of successful achievement of the favourable ADA and BMI outcomes. Models of the relationships were created with independent variable including age, sex, duration of diabetes, yoga treatment vs. non-yoga treatment, baseline values of variables of biological relevance.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Kahn, S. E. et al. Pathophysiology and treatment of type 2 diabetes: perspectives on thepast, present, and future. Lancet. 383, 1068–83 (2014).
International Diabetes Federation. IDF diabetes atlas.8th ed. IDF, www.diabetesatlas.org (2017).
Bhurji, N. et al. Improving management of type 2 diabetes in South Asian patients: a systematic review of intervention studies. BMJ Open. 6, e008986z (2016).
Hills, A. P. et al. Epidemiology and determinants of type 2 diabetes in south Asia. Lancet Diabetes Endocrinol. 6, 966–978 (2018).
American Diabetes Association. Standards of Medical Care in Diabetes—2017 Abridged for Primary Care Providers. Clin Diabetes. 35, 5–26 (2017).
American Diabetes Association. Lifestyle Management: Standards of Medical Care in Diabetes—2019. Diabetes Care. 42(Supplement 1), S46–S60 (2019).
American Diabetes Association. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2018. Diabetes Care. 41(Supplement 1), S86–S104 (2018).
The ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 358, 2560–2572 (2008).
American Diabetes Association. Foundations of Care and Comprehensive Medical Evaluation. Diabetes Care. 39(Suppl 1), S23–35 (2016).
Janssen, P. G. et al. Randomised controlled trial of intensive multifactorial treatment for cardiovascular risk in patients with screen-detected type 2 diabetes: 1-year data from the ADDITION Netherlands study. Br J Gen Pract. 59, 43–8 (2009).
López-Simarro, F. et al. Inertia and treatment compliance in patients with type 2 diabetes in primary care. Med Clin (Barc). 138, 377–384 (2012).
Stark Casagrande S, et al. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care. 201z 36, 2271–9.
Menon, A. S. & Ahluwalia, A. I. The ABC of diabetes. How many patients are able to achieve the goal laid down by American Diabetes Association? Med J Armed Forces India. 71, 132–4 (2015).
Stolar MW. Defining and achieving treatment success in patients with type 2 diabetes mellitus. Mayo Clin Proc. 2010; 85(12 Suppl): S50–9.
Anjana, R. M. et al. Prevalence of diabetes and prediabetes (impaired fasting glucose or/and impaired glucose tolerance) in rural and urban India: Phase 1 results of the Indian Council of Medical Research-INdiaDIABetes (INDIAB) study. Diabetologia. 54, 3022–3027 (2011).
Misra, P. et al. A review of the epidemiology of diabetes in rural India. Diabetes Research and Clinical Practice. 92, 303–311 (2011).
Little, M. et al. Decoding the Type 2 Diabetes Epidemic in Rural India. Med Anthropol. 36, 96–110 (2017).
Haughton, C. F. et al. Racial/ethnic representation in lifestyle weight loss intervention studies in the United States: A systematic review. Prev Med Rep. 9, 131–137 (2018).
American Diabetes Association. Standards of Medical Care in Diabetes—2015 Abridged for Primary Care Providers. Clinical Diabetes. 33, 97–111 (2015).
Misra, A. Ethnic-Specific Criteria for Classification of Body Mass Index: A Perspective for Asian Indians and American Diabetes Association Position Statement. Diabetes Technol Ther. 17, 667–71 (2015).
Unnikrishnan, A. G. et al. Importance of achieving the composite endpoints in diabetes. Indian J Endocrinol Metab. 17(5), 835–843 (2013).
Leslie, D. B. et al. Efficacy of the Roux-en-Y gastric bypass compared to medically managed controls in meeting the American Diabetes Association composite end point goals for management of type 2 diabetes mellitus. Obes Surg. 22, 367–74 (2012).
Kumar, B. P. R., Dudala, S. R. & Rao, A. R. Kuppuswamy’s socio-economic status scale’s revision of economic parameter for. Int J of Res Dev Health. 1, 2–4 (2012).
The Look AHEAD Research Group. Long Term Effects of a Lifestyle Intervention on Weight and Cardiovascular Risk Factors in Individuals with Type 2 Diabetes: Four Year Results of the Look AHEAD Trial. Arch Intern Med. 170, 1566–1575 (2010).
Thind, H. et al. The effects of yoga among adults with type 2 diabetes: A systematic review and meta-analysis. Prev Med. 105, 116–126 (2017).
Innes, K. E. & Selfe, T. K. Yoga for Adults with Type 2 Diabetes: A Systematic Review of Controlled Trials. J Diabetes Res. 2016, 6979370 (2016).
Ikramuddin, S. et al. Durability of Addition of Roux-en-Y Gastric Bypass to Lifestyle Intervention and Medical Management in Achieving Primary Treatment Goals for Uncontrolled Type 2 Diabetes in Mild to Moderate Obesity: A Randomized Control Trial. Diabetes Care. 39, 1510–8 (2016).
Mithal, A. et al. Prevalence of dyslipidemia in adult Indian diabetic patients: A cross sectional study (SOLID). Indian J Endocrinol Metab. 18, 642–7 (2014).
Passarella, P., Kiseleva, T. A., Valeeva, F. V. & Gosmanov, A. R. Hypertension Management in Diabetes: 2018 Update. Diabetes Spectr. 31, 218–224, https://doi.org/10.2337/ds17-0085 (2018).
Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. Bmj. 317, 703–13 (1998).
Adler, A. I. et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 321(7258), 412–419 (2000).
Gosmanov, A. R. et al. Synergistic association of combined glycemic and blood pressure level with risk of complications in US veterans with diabetes. J Hypertens. 34, 907–913 (2016).
Stratton, I. M. et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321, 405–412 (2000).
Pi-Sunyer, F. X. Weight loss in type 2 diabetic patients. Diabetes Care. 28, 1526–1527 (2005).
Pi-Sunyer, X. et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care. 30, 1374–83 (2007).
Wing, R. R. et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 34, 1481–1486 (2011).
Gard, T. et al. Potential self-regulatory mechanisms of yoga for psychological health. Front. Hum. Neurosci. 8, 770 (2014).
Angadi, P. et al. Adherence to yoga and its resultant effects on blood glucose in Type 2 diabetes: A community-based follow-up study. Int J Yoga 10, 29–36 (2017).
Acknowledgements
We are thankful to the “Apollo Total Health Group’ for the financial support provided to conduct the study. We acknowledge the support and continued involvement of the chairman, doctors, researchers and field workers of ‘Apollo Total Health Group’ and yoga therapists of S-VYASA University in the study. The funding sponsor contributed in design of the study, data collection and data analysis. A special thanks to Sai Lakshmi Prasanna M, senior yoga therapist. We have not paid to write this article to any pharmaceutical company or other agency. We also thank the USV (PVT) Ltd for the generous donation of digital BP measurement machines which were utilized in this study.
Author information
Authors and Affiliations
Contributions
G.A. contributed to the study design, planned the cohort, data collection and analysis. N.R. revised the experiment design, and reviewed the manuscript. V.M. analysed the data and wrote the manuscript. S.M. is the chief advisor of Total Health-A CSR initiative of Apollo Hospitals enterprise limited. R.S. and R.S. are the project and deputy medical directors of Total Health, respectively. S. M., R.S., and R.S. planned the cohort, designed the study and contributed to the data collection. V.S. R reviewed the manuscript. N.H.R. contributed to the discussion section and reviewed the manuscript. We also declare Dr. Nagarathana R as the guarantor of the entire study. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arumugam, G., Nagarathna, R., Majumdar, V. et al. Yoga-based lifestyle treatment and composite treatment goals in Type 2 Diabetes in a rural South Indian setup- a retrospective study. Sci Rep 10, 6402 (2020). https://doi.org/10.1038/s41598-020-63133-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-63133-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.