Abstract
The incidence of asthma exacerbation depends on atmospheric conditions, including such meteorological factors as the ambient temperature, relative air humidity or concentration of atmospheric aerosols. An assessment of relations between the frequency of asthma exacerbation and environmental conditions was made according to the meteorological components, the biometeorological index UTCI (Universal Thermal Climate Index), as well as selected air quality parameters, including concentrations of PM10 and PM2.5. The study was conducted on the basis of a retrospective analysis of medical data collected at the Independent Public Hospital of Tuberculosis and Pulmonary Diseases in Olsztyn (Poland). Our analysis of patient data (from 1 January 2013 until 31 December 2017) showed a significant correlation between the number of asthma exacerbation and the UTCI value. More frequent asthma exacerbations are observed in patients aged over 65 years when air humidity increases. The UTCI values contained within class 5, describing thermoneutral conditions, correspond to an average frequency of asthma exacerbation. A decline in the UTCI value leads to a reduced number of asthma exacerbation, while a rise makes the cases of asthma exacerbations increase.
Similar content being viewed by others
Introduction
According to the definition provided by the Global Initiative for Asthma (GINA), asthma is a heterogenous disease induced by an inflammatory condition in the airways1. It is characterized by reversible respiratory obstruction, which is accompanied by such symptoms as cough, dyspnea and thoracic pain. The disease most often affects children and elderly people2. The mean incidence is 3–5% in developing countries and >20% in developed ones3. The available data as of 2016 allows us to estimate that globally around 339.4 million people suffer from asthma4. In Poland, the affected people represent circa 5–7% of the adult population, i.e. around 2 million people5. With regard to its etiology, asthma is divided into allergic (first symptoms typically occur in childhood) and non-allergic one (usually developing in adulthood). The etiopathogenesis of asthma takes into account the influence of such environmental factors as temperature, atmospheric pressure, air humidity, indicators of air pollution: ozone, carbon dioxide, sulphur dioxide and particulate matter6,7,8,9,10. Atmospheric aerosols, PM2.5 and PM10, are a mixture of air suspended particles with a diameter of no more than 2.5 and 10 µm, respectively. In susceptible people, particulate matter is responsible for respiratory tract symptoms such as cough and wheezing11,12. In vulnerable patients, they give rise to respiratory tract symptoms, including cough and wheezing.
The human organism is exposed to the influence of various elements of the atmospheric environment, which shape the thermal comfort of one’s body, affect well-being, and even influence health. A variety of methods and indices are employed in biometeorology to determine the relationship between atmospheric factors and human health13. An indicator which has been developed to achieve a standard measure for the assessment of external environmental conditions in various spatial scales is the UTCI (Universal Thermal Climate Index)14,15. This index is based on an analysis of the thermal balance of a human body, made according to the Fiala’s multi-node model of human heat transfer, providing information on actual body temperature regulatory processes, which are dependent on the ambient meteorological conditions16,17,18. In comparison with other biometeorological parameters, the UTCI is more sensitive to even small changes in temperature, solar radiation, air humidity and wind velocity15.
Changes in climate have always had and will continue to have strong influence (direct and indirect) on many sectors of economy and on other areas of human activity. Their impact will become stronger as the incidence of extreme weather events increases, and whenever there are situations where the weather typical of a given area occurs in an untypical season of the year (for example very warm winters in Poland). Research is undertaken to explore how the climate changes observed may affect the health of human populations in particular countries as well as globally19,20,21,22,23.
The intricate influence of climatic changes on the epidemiology of respiratory tract disorders has not been completely identified. The effect of global warming on the onset, duration and intensity of pollen season, associated with the incidence and severity of asthma exacerbation, has been described as well as the relationship with air pollution and infections of the airways24,25. Both short- and long-term exposure to PM2.5 and PM10 can be linked to a more frequent incidence of asthma symptoms or less effective asthma control26,27.
It was evidenced in the 1990s that both high and low air humidity, elevated atmospheric pressure, low ambient temperature, rainfalls and storms all had an effect on the occurrence of dysfunctions of the respiratory system28,29,30,31. Analysis of data obtained from literature references pertaining to the effect of ambient temperature on the occurrence of acute asthma exacerbation provides us with contradictory information. Fitzgerald et al. reports that high temperature contributes to more frequent asthma exacerbations, while Soneja et al. implicates such impact of low temperature32,33. Kaminsky et al. demonstrate that a change in ambient temperature may cause the activation of inflammatory pathways, inducing hyperactivity of bronchi, their remodeling and the narrowing of the airways, which consequently stimulates asthma exacerbation34. In turn, Epton et al. maintain that a rise in temperature can also contribute to a higher incidence of asthma exacerbations due to greater exposure to allergens35.
Ehara et al. showed a positive relationship between the number of patients admitted to hospital with exacerbated asthma and a rise in atmospheric pressure as well as a decrease in the relative air humidity36. In another paper, Abdullah M. Al-Rubaish described the effect of wind blasts during a storm carrying bioaerosol, which due to a sudden release of spores and pollen contributed to the occurrence of asthma symptoms37.
To the best of our knowledge, no attempt has been made so far to describe an application of any complex biometeorological index to an analysis of factors affecting the incidence of asthma exacerbations. In our article, we suggest using the UTCI, an index measuring human thermal comfort as a complex and universal biometeorological indicator in an assessment of the frequency of asthma exacerbation. Another objective of this research was to analyze the incidence of asthma exacerbations relative to such atmospheric environmental factors as: temperature and humidity of air, wind velocity, and particulate matter parameters PM2.5 and PM10.
Material and Methods
Study population
The study was conducted on the basis of a retrospective analysis of medical data collected at the Independent Public Hospital of Tuberculosis and Pulmonary Diseases in Olsztyn (Poland) between 1 January 2013 and 31 December 2017. The hospital is the leading reference centre for pulmonary diseases in the Province of Warmia and Mazury. The patients included in the study were selected according to the ICD10 classification (comprising codes from group J45 or coexisting with J45 diseases). A database was created, containing 1 449 records (14.12% of the total number of 29 088 patients hospitalized in this period), including 574 (39.6%) records of patients aged over 65 years. Each case of hospitalization when asthma was not determined as the primary cause for hospitalization was verified based on the patient’s medical record for its exacerbation. The mean age of the entire population was 61.9 (±14.3 SD) years, women 61.7 (n = 770; ±14.6 SD) years, and men 62.2 (n = 679;±13.9 SD) years.
Meteorological data
The meteorological data from the time period subjected to the analysis (2013–3017) were acquired from a meteorological station of the Institute of Meteorology and Water Management in Olsztyn (Poland). These data included values of the mean daily, maximum and minimum temperatures, wind velocity, relative air humidity and atmospheric pressure for each day. The data of 12 UTC (coordinated universal time) regarding the meteorological parameters (air temperature, relative air humidity, actual vapor pressure, cloudiness, wind velocity) served to calculate values of the UTCI, whose procedures of calculation were provided by Fiala and Brode18,38. The UTCI is based on objective changes in an organism’s physiological parameters in response to environmental conditions. Values of the UTCI are expressed in degrees Celsius [°C], and are a measure of thermal load onto the human body.
On days with low air temperature, at high wind velocity, cold stress occurs (cold stress classes from 1 to 5 – the UTCI values ≤9.0 °C), whereas days with high air temperature and intensive solar radiation are conducive to heat stress (heat stress classes from 7 to 10, values of the UTCI > 26 °C). Thermal comfort conditions (thermoneutral) are ones where values of the UTCI are in a range of 9.1 a 26 °C (class 6)38.
The area covered by the research, according to the updated Köppen-Geiger climate classification, lies in the sphere of continental climates, without dry season and with warm summer (Dfb)39. It is characterized by high changeability of weather conditions between years, and by distinct seasonability in the course of a year, which determines the presence of 4 seasons of the year. The mean annual air temperature during the period of the study was 8.5 °C, with January being the coldest month having the mean temperature of −3.1 °C, while July was the warmest month, with the mean air temperature of 18.5 °C. The annual precipitation total was 660 mm, and the mean relative air humidity equaled 78%. The mean annual wind velocity reached 3 m/s, with the highest values observed in December and January.
During the analyzed period (01.01.2013–31.12.2017), there were no events of extreme cold stress or extreme heat stress, i.e. class 1 or class 10, respectively. Cold stress conditions occurred during 975 days (53.4%) (Table 1). Thermoneutral conditions appeared in 38.77% of time (n = 708 days), whereas heat stress was in 7.83% (n = 143) of the total days (Table 1). The analysis therefore excluded the UTCI classes absent during the research period, i.e. classes 1 and 10 (extreme cold stress and extreme heat stress), nor did it take into account classes 2, 8, 9 (very strong cold stress, strong heat stress, very strong heat stress, respectively), which did not coincide with any case of asthma exacerbation. Exacerbations of asthma appeared in patients on days corresponding to classes 3–7 of the UTCI.
The World Health Organization recommends a very strict approach to the emission of particulate matter, where the allowable daily concentration for PM10 is 50 µg/m3 and for PM2.5 25 µg/m3 40. During the analyzed time period, the average annual number of days when the permissible concentrations of PM2.5 and PM10 were exceeded equaled 2 and 6 days, respectively.
The exceeded threshold of PM10 and PM2.5 concentrations appeared only during the house heating season, i.e. from late autumn to early spring (October–March), with the highest incidence in the months from December to March, when it happened on an average of 3 and 11 days, respectively for PM10 and PM2.5.
Statistical analysis
Statistical analysis was performed to reveal the relationship between asthma exacerbation cases among the hospitalized patients and meteorological variables as well as air pollutants. The explanatory variables (daily mean air temperature, UTCI and UTCI classes 3–7, wind velocity, relative air humidity, atmospheric pressure, rainfall sum, PM2.5 and PM10) were employed for the Generalized Linear Model (GLM) assuming the Poisson’s distribution and using a logarithm as the link function41. The contribution of the predictors for two groups of patients with asthma, aged <= 65 and >65, was evaluated by testing individual coefficients with the Wald’s test at p ≤ 0.05.
For the data observed to be considered statistically significant, the ±95% confidence interval (CI) was calculated. Statistical analyses were performed with STATISTICA 13.1 for Windows.
Ethics statement
The study presented in this paper is a retrospective analysis of data from medical histories of patients. The data required to make the analysis were collected having received the consent of the hospital’s authorities. The researchers did not use or process any personal data of the hospitalized patients. The research did not require a permit from a bioethics committee.
All the experimental protocols for involving human data in the study were in accordance with national Polish guidelines. According to Ethics Committee of the University of Warmia and Mazury in Olsztyn, Poland this research, as a blinded retrospective analysis, does not required a separate consent from the bioethics committee. Informed consent for subject was waived by the Ethics Committee of the University of Warmia and Mazury in Olsztyn, Poland.
Exemption for the study
According to Ethics committee University of Warmia and Mazury In Olsztyn, Poland this research does not meet the criteria of a medical experiment and therefore does not require a separate consent from the bioethics committee.
Consent waiver
According to Ethics committee University of Warmia and Mazury In Olsztyn, Poland this research, as a blinded retrospective analysis, does not required a separate consent from the bioethics committee.
Results
Table 2 presents the analysis of covariance between the number of hospital admissions due to asthma (exacerbations and de novo diagnosis) and the analyzed biometeorological factors. From among categorical predictors (UTCI classes), class 6 representing thermoneutral conditions was considered as the baseline level. To recognize the effect of other meteorological parameters and air pollution on the quality of the model (GLM) we employed the following continuous covariables: average wind velocity, average air humidity, average daily temperature, average atmospheric pressure, daily rainfall total, average PM2.5 concentration and average PM10 concentration (atmospheric aerosols containing particles with a diameter of no more than 2.5 µm and 10 µm, respectively).
The analysis of the frequency of hospital admissions due to asthma, against the background of meteorological parameters and mutual interactions between these variables, shows that it is reversely proportional to the UTCI values and average relative humidity of air (p = 0.030 and p = 0.002, respectively).
Moreover, it has been demonstrated that the distribution of incidence of asthma exacerbation is related to the UTCI classes 3 and 7. The distribution of data in ranges of confidence intervals (CI = ±95%) is illustrated in Fig. 1.
Figure 2 shows the distribution of asthma exacerbation against the backdrop of the course of mean daily UTCI values in the multi-annual period of 2013–2017. The sinusoidal course of both curves depicts a reverse amplitude of the course of the UTCI coefficient and the occurrence of asthma exacerbations. In the summer period, extremely high UTCI values, i.e. heat stress, are accompanied by ‘peaks’ in the incidence of asthma. In winter, due to cold stress, there is an increase in the number of asthma exacerbations.
Furthermore, the analyzed population was divided into two age groups: aged ≤65 years and >65 years of life (Table 2). The incidence of exacerbated asthma among younger patients was also higher at higher UTCI coefficients (p = 0.015), that is when heat stress occurred.
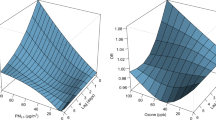
In turn, the subpopulation of patients aged over 65 years was found to present a statistically significant negative relationship between the frequency of asthma exacerbation and the presence of strong cold stress. Regression analysis revealed a direct relationship between the number of hospitalizations due to asthma and concentrations of PM2.5 and PM10; however, only in the older patient group (Fig. 3).
Analogous regression analysis performed for relative humidity did not reveal statistically significant correlations (not shown in the graph). It should be stressed that concentrations of PM2.5 and PM10 are higher with lower outdoor temperature and lower UTCI (Fig. 4).
Discussion
Research dealing with the influence of meteorological factors on the incidence of exacerbation of asthma and other respiratory tract diseases is gaining greater interest 42,43. Most researchers approach the issue through the prism of atmospheric contamination. Papers referring to basic or more complex biometeorological parameters are less numerous, and we were unable to detect a single study that would employ the UTCI for this purpose.
It should be stressed that the impact of global warming on local atmospheric conditions, and as a further consequence on the epidemiology of various diseases, depends on the geographical location of a study, that is on the local climate.
Considering the baseline level of UTCI class 6 as thermoneutral conditions (ANCOVA, p < 0.05), statistically higher UTCI values (class 7) and an increase in the mean daily temperature (Table 2) predispose to a higher number of hospital admissions (age ≤ 65) due to asthma. On days identified as belonging to UTCI class 3, that is on days with strong cold stress, the incidence of asthma exacerbation declines particularly among the elderly (Table 2). In our opinion, this dependence is direct and it is not distorted by changes in atmospheric dust concentrations. Although the concentrations of PM10 and PM2.5 found in Poland are among the highest in the European Union countries, events of excessive particulate matter concentrations in air in Olsztyn (a beneficial geographical location, favoring air circulation) were noted only sporadically44. This enabled us to reveal in our data the direct impact of cold stress and heat stress on the function of the respiratory system. The results of ANCOVA analysis revealed that the impact on the UTCI class on the number of hospitalizations due to asthma may be limited by the increase in the concentration of PM10 (covariate variable) in the air (Table 2). Higher concentrations of PM2.5 and PM10 occuring in lower air temperatures, and thus at the lower UTCI (Fig. 4) may increase the number of hospitalizations due to asthma (Fig. 3), especially among older patients. This effect is, however, insufficient to eliminate the impact of cold stress.
In a number of articles dedicated to cold-induced asthma, authors focus on the influence of cold air on airway patency45. The spastic effect induced by cold air is particularly well known among athletes, when during physical exertion, as a result of hyperventilation, and through an increase in the osmolarity of fluid in airways, the direct influence of cold air on reducing the patency of bronchi becomes distinctly manifested46. When cold stress is present, the breathing pattern is altered. Diesel et al. demonstrated that a decrease in ambient temperature from 18 to 4 °C led to a decrease in respiratory rate by 25%, while tidal volume rose by 35%47. An average person exposed to cold stress tries to breath more slowly and deeply rather than hyperventilating. Moreover, a change in air temperature, under physiological conditions with no physical effort, is set off by the upper airways (the nose) and has no effect on the lower respiratory tract. Sthurman-Ellstein et al. showed that if asthma patients were breathing through the nose during an effort stress test, there was no bronchial constriction appearing in response to the physical effort48. Bronchoconstriction is unobserved in people taking ice baths either49. Moreover, an increase in the level of catecholamines, which are expected to widen the bronchi, is emphasized. The UTCI, an indicator developed to describe the impact of atmospheric conditions on the human body, reflects very well the influence of both cold and heat stress. Basic parameters, such as ambient temperature, wind velocity, relative air humidity, are sufficient to describe the weather conditions, but the UTCI proves to be a valuable tool in the type of research presented in this article. To the best of our knowledge, this is the first study that describes the relationship between the cases of asthma exacerbations and the UTCI.
In their meta-analysis of 81 studies, Cong et al. noted that a decrease in temperature contributed to a higher incidence of asthma cases, but only in a population of children, while no such dependence was observed among adults50. This finding among the under-age population might be associated with greater physical activity among children, which more often causes hyperventilation (same as among athletes), especially when we consider the fact that air flow through children’s respiratory tract takes a shorter time (the anatomical structure).
These epidemiological data, not entirely coherent, might have other roots in the epidemiology of upper respiratory tract infections. Infections with Rhinovirus (RV) are responsible for over half of cases of URT infections, and may cause episodes of asthma in predisposed patients51. Such infections occur in mass numbers in our climatic zone after the first autumn weather break. However, their further spread does not depend on the weather conditions, but progresses in line with the general laws of epidemics52.
Global urbanization also leads to an increase in the environmental pollution caused by combustion of fossil fuels, biomass, emissions from agriculture, and windborne mineral dusts as well as organic matter. Solid particles in air, such as PM2.5–10, that is a mixture of particles emitted from numerous sources, may contribute to the activation of cytokine pathways and activation of an inflammatory response in the airways53,54. PM2.5 alone can induce an allergic reaction due to overproduction of IgE mediated by Th2 and Th17 lymphocytes, and thus contribute to a higher incidence of asthma exacerbations55,56. Based on the data submitted to our analysis, we have been able to demonstrate that a higher PM10 concentration leads to an increased frequency of acute asthma exacerbation in elderly patients (Table 2). With age, the epithelium of bronchi becomes thinner, which means that particles larger in diameter can penetrate with air into the bronchi, settle down in the airways and induce local inflammatory response57,58.
Global warming entails longer pollen seasons, increased amounts of pollen produced and its higher allergenicity59. These factors add to a rise in the incidence of asthma exacerbation59,60. Higher air temperatures in winter, earlier spring season, earlier autumn, as well as delayed winter lengthen the duration of exposure to fungal endospores. Particulate matter and mould spores are basic allergens, implicated as factors in the etiopathogenesis of asthma8. Particulate matter, that is fine powder-like substances with grains of the size 2–10 µm in diameter (PM2,5; PM10) can easily permeate into the airways. They are also easily carried by wind over large distances and therefore can affect people being far from their source of emission. One of the findings reported by Ziska L et al., who in 2009 analyzed data from several centres (8 located in the USA and 2 from Canada), there was the increased length of ragweed pollen season by over 3 weeks in comparison with the year 199559. In Poland, it has been proven that the season of pollination by autumn weeds has been prolonged in the past few decades, mainly as a result of the winter-autumn period lasting longer61.
Literature provides contradictory information on the relationship between asthma morbidity and air humidity. Some researchers notice a significant increase in asthma exacerbation cases under the weather conditions characterized by higher ambient air humidity, and link this fact to higher counts of fungal spores61,62,63. Kwon et al. associated this phenomenon with the occurrence of fog, which often accompanies higher air humidity, and which alone – by being acid aerosol – is yet another air pollutant64. Others emphasize an increase in hospital admissions due to asthma on days with lower air humidity65. Our regression analysis performed for air pollution humidity and the number of asthma exacerbations (Fig. 3) does not indicate a direct statistically significant (p < 0.05) relationship between these variables. However, relative humidity (as a covariate) weakens (p < 0.001) the correlation between the UTCI class (fixed effect) and the number of asthma cases, as was revealed by covariance analysis (Table 2).
Conclusions
The increase in the number of hospitalizations due to asthma is related to UTCI values. In moderate heat stress (UTCI class 7) the frequency of asthma cases increases in younger patients. The number of hospital admissions decreases with a decrease of the UTCI value to class 3, that is in the conditions of strong cold stress, especially among patients over 65 year old. This happens despite increased concentrations of PM2.5 and PM10 in wintertime, that are directly responsible for the increase in hospitalizations due to asthma among these patients.
Limitations
The results presented above originate from the data collected from one centre, the Independent Public Hospital of Tuberculosis and Pulmonary Diseases in Olsztyn. Characteristic symptoms of asthma such as dyspnea and chest tightness require a differential diagnosis for cardiological and pulmonary causes. Due to the inadequate health care system, patients with these symptoms are first admitted to Emergency Departments in different hospitals, where they are diagnosed and then referred to Pulmonary Departments. This can translate into 1- to 2-day delays in our data. Hence, all meteorological parameters included in our study were analyzed in weekly intervals rather than on a daily basis. It was important for us in this study to focus attention on an older age group of patients; hence we do not present analyses as regards other possible age subgroups, analyses regarding gender etc.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Global Initiative for Asthma. Global Initiative for Asthma, https://ginasthma.org/ (2020).
IHME. Institute for Health Metrics and Evaluation, http://www.healthdata.org/.
Holgate, T. S. & Thomas, M. In Middleton’s Allergy Essentials (eds. O’Hehir, R. E., Holgate, S. T. & Sheikh, A.) Ch. 7, 151–204 (Elsevier, 2017).
Network, G. A. (Auckland, New Zealand, 2018).
Liebhart, J. et al. Prevalence and risk factors for asthma in Poland: results from the PMSEAD study. J Investig Allergol Clin Immunol 17, 367–374 (2007).
Xu, Z. et al. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occup Environ Med 70, 730–735, https://doi.org/10.1136/oemed-2013-101538 (2013).
Lian, H., Ruan, Y., Liang, R., Liu, X. & Fan, Z. Short-Term Effect of Ambient Temperature and the Risk of Stroke: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health 12, 9068–9088, https://doi.org/10.3390/ijerph120809068 (2015).
Wang, W. Progress in the impact of polluted meteorological conditions on the incidence of asthma. J Thorac Dis 8, E57–61, https://doi.org/10.3978/j.issn.2072-1439.2015.12.64 (2016).
Mortimer, K. M., Neas, L. M., Dockery, D. W., Redline, S. & Tager, I. B. The effect of air pollution on inner-city children with asthma. Eur Respir J 19, 699–705, https://doi.org/10.1183/09031936.02.00247102 (2002).
Darçın, M. Association between air quality and quality of life. Environmental Science and Pollution Research 21, 1954–1959 (2014).
Guarnieri, M. & Balmes, J. R. Outdoor air pollution and asthma. Lancet 383, 1581–1592, https://doi.org/10.1016/S0140-6736(14)60617-6 (2014).
Habre, R. et al. The effects of PM2.5 and its components from indoor and outdoor sources on cough and wheeze symptoms in asthmatic children. J Expo Sci Environ Epidemiol 24, 380–387, https://doi.org/10.1038/jes.2014.21 (2014).
Epstein, Y. & Moran, D. S. Thermal comfort and the heat stress indices. Ind Health 44, 388–398, https://doi.org/10.2486/indhealth.44.388 (2006).
McGregor, G. R. Special issue: Universal Thermal Comfort Index (UTCI). Int J Biometeorol 56, 419, https://doi.org/10.1007/s00484-012-0546-6 (2012).
Blazejczyk, K., Epstein, Y., Jendritzky, G., Staiger, H. & Tinz, B. Comparison of UTCI to selected thermal indices. Int J Biometeorol 56, 515–535, https://doi.org/10.1007/s00484-011-0453-2 (2012).
Fiala, D., Lomas, K. J. & Stohrer, M. A computer model of human thermoregulation for a wide range of environmental conditions: the passive system. J Appl Physiol (1985) 87, 1957–1972, https://doi.org/10.1152/jappl.1999.87.5.1957 (1999).
Fiala, D., Lomas, K. J. & Stohrer, M. Computer prediction of human thermoregulatory and temperature responses to a wide range of environmental conditions. Int J Biometeorol 45, 143–159, https://doi.org/10.1007/s004840100099 (2001).
Fiala, D., Havenith, G., Brode, P., Kampmann, B. & Jendritzky, G. UTCI-Fiala multi-node model of human heat transfer and temperature regulation. Int J Biometeorol 56, 429–441, https://doi.org/10.1007/s00484-011-0424-7 (2012).
Haines, A., Kovats, R. S., Campbell-Lendrum, D. & Corvalan, C. Climate change and human health: impacts, vulnerability and public health. Public Health 120, 585–596, https://doi.org/10.1016/j.puhe.2006.01.002 (2006).
Gosling, S. N., McGregor, G. R. & Paldy, A. Climate change and heat-related mortality in six cities part 1: model construction and validation. Int J Biometeorol 51, 525–540, https://doi.org/10.1007/s00484-007-0092-9 (2007).
Gosling, S. N., McGregor, G. R. & Lowe, J. A. Climate change and heat-related mortality in six cities Part 2: climate model evaluation and projected impacts from changes in the mean and variability of temperature with climate change. Int J Biometeorol 53, 31–51, https://doi.org/10.1007/s00484-008-0189-9 (2009).
Ebi, K. L. Health in the new scenarios for climate change research. Int J Environ Res Public Health 11, 30–46, https://doi.org/10.3390/ijerph110100030 (2013).
Paterson, J., Berry, P., Ebi, K. & Varangu, L. Health care facilities resilient to climate change impacts. Int J Environ Res Public Health 11, 13097–13116, https://doi.org/10.3390/ijerph111213097 (2014).
D’Amato, G. et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J 8, 25, https://doi.org/10.1186/s40413-015-0073-0 (2015).
Campbell-Lendrum, D. & Pruss-Ustun, A. Climate change, air pollution and noncommunicable diseases. Bull World Health Organ 97, 160–161, https://doi.org/10.2471/BLT.18.224295 (2019).
Mann, J. K. et al. Short-term effects of air pollution on wheeze in asthmatic children in Fresno, California. Environ Health Perspect 118, 1497–1502, https://doi.org/10.1289/ehp.0901292 (2010).
Jacquemin, B. et al. Air pollution and asthma control in the Epidemiological study on the Genetics and Environment of Asthma. J Epidemiol Community Health 66, 796–802, https://doi.org/10.1136/jech.2010.130229 (2012).
Bury, J. D. Climate and chest disorders. Br Med J 4, 613, https://doi.org/10.1136/bmj.4.5840.613-c (1972).
Waller, R. E. Asthma and weather. Lancet 2, 452, https://doi.org/10.1016/s0140-6736(83)90410-5 (1983).
Greenburg, L., Field, F., Reed, J. I. & Erhardt, C. L. Asthma and temperature change. II. 1964 and 1965 epidemiological studies of emergency clinic visits for asthma in three large New York City hospitals. Arch Environ Health 12, 561–563, https://doi.org/10.1080/00039896.1966.10664433 (1966).
Sutherland, A. & Hall, I. P. Thunderstorms and asthma admissions. Lancet 344, 1503–1504, https://doi.org/10.1016/s0140-6736(94)90320-4 (1994).
Fitzgerald, E. F., Pantea, C. & Lin, S. Cold spells and the risk of hospitalization for asthma: New York, USA 1991–2006. Lung 192, 947–954, https://doi.org/10.1007/s00408-014-9645-y (2014).
Soneja, S. et al. Exposure to extreme heat and precipitation events associated with increased risk of hospitalization for asthma in Maryland, USA. Environ Health 15, 57, https://doi.org/10.1186/s12940-016-0142-z (2016).
Kaminsky, D. A., Bates, J. H. & Irvin, C. G. Effects of cool, dry air stimulation on peripheral lung mechanics in asthma. Am J Respir Crit Care Med 162, 179–186, https://doi.org/10.1164/ajrccm.162.1.9806079 (2000).
Epton, M. J. et al. Climate and aeroallergen levels in asthma: a 12 month prospective study. Thorax 52, 528–534, https://doi.org/10.1136/thx.52.6.528 (1997).
Ehara, A. et al. Are high barometric pressure, low humidity and diurnal change of temperature related to the onset of asthmatic symptoms? Pediatr Int 42, 272–274, https://doi.org/10.1046/j.1442-200x.2000.01228.x (2000).
Al-Rubaish, A. M. Thunderstorm-associated bronchial asthma: a forgotten but very present epidemic. J Family Community Med 14, 47–51 (2007).
Brode, P. et al. Deriving the operational procedure for the Universal Thermal Climate Index (UTCI). Int J Biometeorol 56, 481–494, https://doi.org/10.1007/s00484-011-0454-1 (2012).
Peel, M. C., Finlayson, B. L. & McMahon, T. A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. 11, 1633–1644, https://doi.org/10.5194/hess-11-1633-2007 (2007).
World Health Organization. Air Quality Guidelines Global Update 2005, https://www.who.int/phe/health_topics/outdoorair/outdoorair_aqg/en/ (2005).
McCullagh, A. & Nelder, J. A. Generalized Linear Models. (Chapman and Hall, 1989).
Poole, J. A. et al. Impact of weather and climate change with indoor and outdoor air quality in asthma: A Work Group Report of the AAAAI Environmental Exposure and Respiratory Health Committee. J Allergy Clin Immunol 143, 1702–1710, https://doi.org/10.1016/j.jaci.2019.02.018 (2019).
Shoraka, H. R., Soodejani, M. T., Abobakri, O. & Khanjani, N. The Relation between Ambient Temperature and Asthma Exacerbation in Children: A Systematic Review. J Lung Health Dis 3, 2–9 (2019).
European Environment Agency. Air quality in Europe — 2017 report. Luxembourg 2017, https://www.eea.europa.eu/publications/air-quality-in-europe-2017 (2017).
Anderson, S. D. & Daviskas, E. The mechanism of exercise-induced asthma is. J Allergy Clin Immunol 106, 453–459, https://doi.org/10.1067/mai.2000.109822 (2000).
Koskela, H. O. Cold air-provoked respiratory symptoms: the mechanisms and management. Int J Circumpolar Health 66, 91–100, https://doi.org/10.3402/ijch.v66i2.18237 (2007).
Diesel, D. A., Tucker, A. & Robertshaw, D. Cold-induced changes in breathing pattern as a strategy to reduce respiratory heat loss. J Appl Physiol (1985) 69, 1946–1952, https://doi.org/10.1152/jappl.1990.69.6.1946 (1990).
Shturman-Ellstein, R., Zeballos, R. J., Buckley, J. M. & Souhrada, J. F. The beneficial effect of nasal breathing on exercise-induced bronchoconstriction. Am Rev Respir Dis 118, 65–73, https://doi.org/10.1164/arrd.1978.118.1.65 (1978).
Leppaluoto, J., Korhonen, I. & Hassi, J. Habituation of thermal sensations, skin temperatures, and norepinephrine in men exposed to cold air. J Appl Physiol (1985) 90, 1211–1218, https://doi.org/10.1152/jappl.2001.90.4.1211 (2001).
Cong, X. et al. Temperature drop and the risk of asthma: a systematic review and meta-analysis. Environ Sci Pollut Res Int 24, 22535–22546, https://doi.org/10.1007/s11356-017-9914-4 (2017).
Vandini, S., Biagi, C., Fischer, M. & Lanari, M. Impact of Rhinovirus Infections in Children. Viruses 11, https://doi.org/10.3390/v11060521 (2019).
Romaszko, J. et al. Applicability of the universal thermal climate index for predicting the outbreaks of respiratory tract infections: a mathematical modeling approach. Int J Biometeorol 63, 1231–1241, https://doi.org/10.1007/s00484-019-01740-y (2019).
Clifford, R. L. et al. Inhalation of diesel exhaust and allergen alters human bronchial epithelium DNA methylation. J Allergy Clin Immunol 139, 112–121, https://doi.org/10.1016/j.jaci.2016.03.046 (2017).
Brandt, E. B. et al. Exposure to allergen and diesel exhaust particles potentiates secondary allergen-specific memory responses, promoting asthma susceptibility. J Allergy Clin Immunol 136, 295–303 e297, https://doi.org/10.1016/j.jaci.2014.11.043 (2015).
Nel, A. Atmosphere. Air pollution-related illness: effects of particles. Science 308, 804–806, https://doi.org/10.1126/science.1108752 (2005).
Nel, A. E., Diaz-Sanchez, D., Ng, D., Hiura, T. & Saxon, A. Enhancement of allergic inflammation by the interaction between diesel exhaust particles and the immune system. J Allergy Clin Immunol 102, 539–554, https://doi.org/10.1016/s0091-6749(98)70269-6 (1998).
Kling, K. M., Lopez-Rodriguez, E., Pfarrer, C., Muhlfeld, C. & Brandenberger, C. Aging exacerbates acute lung injury-induced changes of the air-blood barrier, lung function, and inflammation in the mouse. Am J Physiol Lung Cell Mol Physiol 312, L1–L12, https://doi.org/10.1152/ajplung.00347.2016 (2017).
Lee, S. W. et al. Short-term effects of multiple outdoor environmental factors on risk of asthma exacerbations: Age-stratified time-series analysis. J Allergy Clin Immunol 144, 1542–1550 e1541, https://doi.org/10.1016/j.jaci.2019.08.037 (2019).
Ziska, L. et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc Natl Acad Sci USA 108, 4248–4251, https://doi.org/10.1073/pnas.1014107108 (2011).
Palczynski, C. et al. The position paper of the Polish Society of Allergology on climate changes, natural disasters and allergy and asthma. Postepy Dermatol Alergol 35, 552–562, https://doi.org/10.5114/ada.2017.71273 (2018).
Bogawski, P., Grewling, L., Nowak, M., Smith, M. & Jackowiak, B. Trends in atmospheric concentrations of weed pollen in the context of recent climate warming in Poznan (Western Poland). Int J Biometeorol 58, 1759–1768, https://doi.org/10.1007/s00484-013-0781-5 (2014).
Dales, R. E. et al. Influence of ambient fungal spores on emergency visits for asthma to a regional children’s hospital. Am J Respir Crit Care Med 162, 2087–2090, https://doi.org/10.1164/ajrccm.162.6.2001020 (2000).
Dales, R. E. et al. The role of fungal spores in thunderstorm asthma. Chest 123, 745–750, https://doi.org/10.1378/chest.123.3.745 (2003).
Kwon, J. W. et al. Emergency Department Visits for Asthma Exacerbation due to Weather Conditions and Air Pollution in Chuncheon, Korea: A Case-Crossover Analysis. Allergy Asthma Immunol Res 8, 512–521, https://doi.org/10.4168/aair.2016.8.6.512 (2016).
Lee, C. C., Sheridan, S. C. & Lin, S. Relating weather types to asthma-related hospital admissions in New York State. Ecohealth 9, 427–439, https://doi.org/10.1007/s10393-012-0803-5 (2012).
Author information
Authors and Affiliations
Contributions
A.R.W. designed the study, conceived the original idea, acquis the data, wrote the manuscript. I.C. designed the study, conceived the original idea, prepared the data to analysis, wrote the manuscript. E.D. wrote the manuscript, reviewed the final manuscript. A.D. supervised the project, reviewed the final manuscript. J.R. wrote the manuscript, reviewed the final manuscript. K.G.L. conducted all statistical analyses, reviewed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Romaszko-Wojtowicz, A., Cymes, I., Dragańska, E. et al. Relationship between biometeorological factors and the number of hospitalizations due to asthma. Sci Rep 10, 9593 (2020). https://doi.org/10.1038/s41598-020-66746-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-66746-8
This article is cited by
-
Mucus Transpiration as the Basis for Chronic Cough and Cough Hypersensitivity
Lung (2024)
-
Spatial distribution of hospital admissions for asthma in the central area of Asturias, Northern Spain
BMC Public Health (2023)
-
Hospital admission tendencies caused by day-to-day temperature changes during summer: a case study for the city of Novi Sad (Serbia)
International Journal of Biometeorology (2023)
-
The effects of summer ambient temperature on total mortality in Serbia
International Journal of Biometeorology (2023)
-
Associations between ambient temperature and adult asthma hospitalizations in Beijing, China: a time-stratified case-crossover study
Respiratory Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.