Abstract
Metabolic diseases are increasing among adolescents with obesity. Although the reported prevalence of metabolic syndrome is approximately 30% worldwide, its prevalence is largely unknown among New Zealand adolescents. Therefore, we assessed the health of adolescents with obesity (BMI ≥ 30 kg/m2) enrolled in a randomised clinical trial (Gut Bugs Trial), to identify the prevalence of undiagnosed comorbidities. Assessments included anthropometry, 24-h ambulatory blood pressure monitoring, and insulin sensitivity. We report on baseline data (pre-randomisation) on 87 participants (14–18 years; 59% females), with mean BMI 36.9 ± 5.3 kg/m2 (BMI SDS 3.33 ± 0.79). Approximately 40% of participants had undiagnosed metabolic syndrome, which was twice as common among males. Half (53%) had pre-diabetes and 92% a reduction in insulin sensitivity. Moreover, 31% had pre-hypertension/hypertension, 69% dyslipidaemia, and 25% abnormal liver function. Participants with class III obesity had a greater risk of metabolic syndrome than those with classes I/II [relative risk 1.99 (95% CI 1.19, 3.34)]. Risks for pre-hypertension/hypertension and inflammation were also greater among those with class III obesity. We identified a high prevalence of undiagnosed comorbidities among adolescents with obesity in New Zealand. As adolescent obesity tracks into adulthood, early interventions are needed to prevent progression to overt cardiometabolic diseases.
Similar content being viewed by others
Introduction
With over 120 million affected children and adolescents worldwide, paediatric obesity has become one of the largest health concerns of the modern world1. In 2016, the World Health Organization (WHO) estimated that, globally, the prevalence of paediatric overweight and obesity was 18%2. In New Zealand, an even higher rate was reported for the same year, whereby nearly 40% had overweight or obesity (> 16% with obesity)3. In 2019, 22% of New Zealand adolescents were overweight while 12% had obesity4, which is higher than in many parts of the world such as Australia (combined rate of overweight/obesity is 25%)5, Denmark (22%)6, and China (26%)7 but lower than the US (40%)8. While the prevalence of paediatric obesity seems to have plateaued in many countries9 as in New Zealand10, the prevalence of adolescents with obesity remains high in New Zealand, particularly among Māori (New Zealand's indigenous people) and Pacific adolescents, and those from areas of greater socioeconomic deprivation4,11. Of note, within a 5-year period from 2007 to 2012, there was a rapid increase in the prevalence of Pacific adolescents with obesity (from 27% to 34%) and severe obesity (9% to 14%)11.
Adolescence is a period of accelerated growth characterised by rapid physiological, hormonal, and developmental changes, with marked alterations in body composition and weight gain12. There are changes in the hormonal regulation of appetite and satiety in both sexes, as well as increases in adiposity and changes in fat distribution among females, which contribute to a tendency to gain weight in adolescence12,13. For some adolescents, the normal changes observed in puberty can be magnified, leading to greater weight gain and metabolic dysfunction, including persistence of insulin resistance14. As 90% of adolescents with obesity continue to have obesity as adults15, early intervention is crucial.
Consistent with the rise in obesity, cardiometabolic comorbidities such as metabolic syndrome and type 2 diabetes mellitus (T2DM) are increasing in children and adolescents16. Increasing body mass index (BMI) is associated with an increased risk of metabolic syndrome17, which includes increased abdominal obesity, hypertension, impaired fasting glycaemia, dyslipidaemia, and is associated with insulin resistance16. The prevalence of metabolic syndrome among adolescents with obesity has been reported to be as high as 60%18, and it is associated with the development of T2DM19, cardiovascular diseases20, and a two-fold increase in the risk of coronary artery disease and stroke, and a 1.5-fold increase in the risk of all-cause mortality21. In the US, a national cross-sectional study reported that T2DM is increasingly diagnosed among adolescents and accounted for 40% of adolescent diabetes, with more than a third of T2DM cases undiagnosed prior to the study22. In New Zealand, the number of children with T2DM is increasing at approximately 5% per year, and this disease disproportionally affects high-risk ethnic groups (Māori and Pacific)23. Apart from serious cardiometabolic complications, paediatric obesity has been associated with increased mortality even in early adulthood24. This is likely due to increased systemic inflammation, insulin resistance, impaired cardiovascular function, and the development of non-alcoholic fatty liver disease25,26. Moreover, many of these children face bullying27 and social isolation28, as well as increased rates of depression29, suicide and self-harm24.
Overall, there are limited data on the prevalence of obesity-related comorbidities among adolescents with obesity in New Zealand30,31. Due to the numerous complications associated with obesity, early identification particularly in high-risk populations is necessary so that targeted interventions can be implemented. Therefore, we aimed to assess the metabolic health of a group of adolescents with obesity enrolled in a clinical trial and identify the prevalence of undiagnosed metabolic syndrome and other obesity-related cardiometabolic comorbidities.
Methods
Ethics
This study reported on baseline data (pre-randomisation) from a randomised placebo-controlled trial (Gut Bugs Trial) to evaluate the effectiveness of faecal microbiome transfer for treatment of adolescent obesity in Auckland, New Zealand32. The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12615001351505); ethics approval was granted by the Northern A Health and Disability Ethics Committee (16/NTA/172). Participants provided verbal and written informed consents. All procedures in this study were conducted according to the ethical principles and guidelines laid down in the Declaration of Helsinki33.
Recruitment
Participants were recruited from social media through Facebook advertisements between 2017–2018. All were post-pubertal, aged 14–18 years, with BMI ≥ 30 kg/m2, who were not diagnosed with diabetes or chronic diseases that could affect weight or metabolism32.
Clinical assessments
Clinical assessments included medical and physical examinations previously described in the trial’s protocol32, and briefly summarised here.
Height, weight, and waist and hip circumferences were measured32. BMI values were converted into standard deviation score (SDS) using WHO standards34. For comparison within our study population, BMI was stratified using the adult criteria for obesity: Class I (BMI ≥ 30 but < 35 kg/m2); Class II (≥ 35 but < 40 kg/m2); and Class III (≥ 40 kg/m2)35. Body composition was assessed using whole-body dual-energy X-ray absorptiometry (DXA; Lunar Prodigy and Lunar iDXA; GE Medical Systems, Chicago, Illinois, USA).
Clinic resting systolic and diastolic blood pressures (BP) were measured using an automated BP monitor (Ri-champion N; Riester, Jungingen, Germany). 24-h ambulatory BP monitoring (24hABPM) was performed using an oscillometric device (Spacelabs OnTrak; Spacelabs Medical Inc, Redmond, Washington, USA).
Participants underwent a 75-g oral glucose tolerance test (OGTT)32. Insulin sensitivity was assessed by homeostatic model assessment of insulin resistance (HOMA-IR)36 and Matsuda index37, as previously described32. Other key markers of glucose metabolism measured were fasting insulin and fasting glucose, 2-h glucose, and glycated haemoglobin (HbA1c). From fasting blood samples, uric acid, high-sensitivity C-reactive protein (hsCRP), lipid profile, and liver function were measured32.
Health outcomes in this study were cardiometabolic comorbidities as defined in Table 1.
Assays
Insulin levels were measured by electrochemiluminescence immunoassay (ECLIA) on the Roche Cobas e411 analyser (Roche, Basel, Switzerland) with a coefficient of variation (CV) of 1.2%. Glucose, HbA1c, uric acid, hsCRP, lipid profile, and liver function were measured on the Roche/Hitachi Cobas e311 (Roche) with CVs 4.1–6.8%.
Data analyses
Data were analysed using SPSS v25 (IBM Corp, Armonk, NY, USA) and SAS v9.4 (SAS Institute, Cary, NC, USA). Baseline data were summarised as mean ± standard deviation (SD), median [quartile 1, quartile 3], or n (%), as appropriate. Differences in prevalence between obesity classes and sexes were examined with Chi-square tests or Fisher's exact tests, as appropriate. The likelihood of given comorbidities in participants with class III obesity was assessed with generalized linear regression models, using PROC GENMOD (SAS), adjusting for sex, and relative risk estimation by Poisson regression with robust error variance, and a log link38. The results were reported as relative risks (RR) with respective 95% confidence intervals (95% CI). Statistical tests were two-tailed, with significance levels maintained at p < 0.05.
Results
Participants
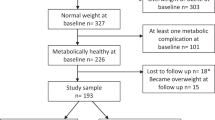
565 participants responded to advertisements; 328 (58%) were not eligible and 150 (27%) declined to participate. Thus, 87 participants (59% females) were recruited at a median age of 17.6 years (Table 2). 44% of our cohort were Māori or Pacific, and nearly 30% were from the most-deprived quintile of socioeconomic deprivation (Table 2). Their mean BMI was 36.9 kg/m2 (range 31.6–42.3 kg/m2), with mean BMI SDS 3.33 (range 2.10–6.38); 33%, 38%, and 29% of participants were classified as obesity class I, II, and III, respectively (Table 2). Mean total body fat was approximately 50% (Table 2).
Comorbidities
There was a high prevalence of undiagnosed comorbidities (Table 3). Notably, one in three participants (36%) had undiagnosed metabolic syndrome (Table 3), with this condition twice as common among males (50% vs 26%; p = 0.018).
In addition, 13% of participants had pre-hypertension and 8% had hypertension from clinic BP. From 24hABPM data, 17% were pre-hypertensive and 14% hypertensive with nocturnal pre-hypertension recorded in 18% and nocturnal hypertension in 10% of participants (Table 3).
Pre-diabetes was common, affecting approximately half of participants (52%): 29% females and 83% males (p < 0.0001). Fasting insulin was elevated in 94% of participants including all the males (Table 3). Most participants displayed a reduction in insulin sensitivity, as 92% had a high HOMA-IR when compared to a cohort of adolescents39, and 87% had a low Matsuda index when compared to healthy adults40 (Table 4).
Dyslipidaemia and abnormal liver function affected 74% and 25% of participants respectively (Table 3). Inflammatory markers were elevated, with 61% having hyperuricaemia and 28% with elevated hsCRP (Table 3).
BMI classes
There were marked differences in the prevalence of cardiometabolic comorbidities between obesity classes (Table 4). The risk of metabolic syndrome increased among those with class III obesity compared to those with a lesser degree of obesity [RR 1.99 (95% CI 1.19, 3.34); p = 0.0091] (Table 4). The prevalence of BP abnormalities was markedly higher in participants with class III obesity, with the relative risks of pre-hypertension/hypertension and loss of the nocturnal dipping BP status more than 3 times greater in this group (Table 4). A higher BMI was associated with an increased likelihood of inflammation, with the relative risk of hyperuricaemia and elevated hsCRP being 1.4 and 2.1 times greater in participants with class III obesity, respectively (Table 4).
Discussion
We identified a high prevalence of undiagnosed comorbidities amongst our cohort of adolescents with obesity. Notably, more than a third were diagnosed with metabolic syndrome, which was twice as common in males than in females. More than half (52%) of our cohort had pre-diabetes and more than 90% had fasting hyperinsulinaemia, with higher rates of these complications in males. In addition, almost all had a reduction in insulin sensitivity. Moreover, increased levels of adiposity were associated with a higher risk of metabolic syndrome, hypertension, and inflammation. The presence of these adverse cardiometabolic outcomes at a relatively young age is alarming, and along with published data documenting the tracking of weight-related comorbidities from childhood into adulthood41, further reaffirms that obesity in adolescence is far from a benign condition.
A description of comorbidities among 239 children and adolescents with obesity in New Zealand was provided by Anderson et al. in 201630. In that study, 1 in 10 had elevated blood pressure, 1 in 4 had increased inflammation, and nearly half had dyslipidaemia and abnormal liver function30. While their reported prevalence of obesity-related comorbidities were relatively high, they were lower than those observed in the present study30, probably because their study population was younger (mean age 10.7 vs 17.2 years in our study), leaner (mean BMI 3.09 vs 3.33 SDS), and had a different ethnic make-up with a much lower representation from those of Pacific descent (3% vs 23%) than ours.
Worldwide, the reported prevalence of metabolic syndrome among children and adolescents with obesity varied between 10 to 66%18,31,42,43,44,45,46,47,48,49,50. In New Zealand, Grant et al. reported a lower rate of metabolic syndrome among 29 Pacific adolescents with obesity aged 15–18 years31 – 21% vs 36% in our study. In comparison, reported rates of metabolic syndrome in adolescents with obesity vary widely across the world: 15% to 50% in the US18,50, 23% to 60% in Latin America18,43,46,49, 12% to 42% in Asia18, and 14% to 44% in Europe18,44,45,47. The marked differences in prevalence among these studies could be attributed to variations in age distribution and ethnic composition of the respective study populations, as well as the definitions of metabolic syndrome used. Nonetheless, the findings from two systematic reviews clearly show increasing BMI as an important risk factor associated with the development of metabolic syndrome18,42, with this relationship also shown to occur at the upper end of the BMI spectrum by our stratified analyses.
Reduction in insulin sensitivity as well as impaired glucose metabolism were common complications among our study population. Insulin resistance as assessed from the HOMA-IR values among our adolescents was more than 1.5 times higher when compared with adolescents with obesity in the US51 and Europe52. In addition, more than half of our participants had pre-diabetes (i.e. impaired fasting glycaemia, impaired glucose tolerance, and/or elevated glycated haemoglobin). It could be argued that our high rate of pre-diabetes could be attributed, at least in part, to our lower cut-off value for impaired fasting glycaemia (i.e. ≥ 5.6 mmol/L as recommended by the ADA53 and ISPAD54, rather than the WHO value ≥ 6.1 mmol/L55), as using the higher WHO cut-off, our pre-diabetes rate would have dropped from 52 to 38%. Nonetheless, when compared to previous studies in US and Europe that used the same cut-off values as ours, the prevalence of pre-diabetes in our study was still 4 times greater52,56. Moreover, due to the high risk of diabetes in our vulnerable study population and our aim to prevent worsening of their metabolic health through early identification and intervention, we contend that the lower threshold for abnormal fasting glycaemia was justified. Nichols et al. reported that without appropriate intervention, nearly one in ten adults with pre-diabetes will develop T2DM within 3.5 years, and the progression to T2DM could be accelerated by risk factors such as increased BMI, elevated blood pressure and triglyceride levels, and lower HDL levels, all of which were present in our participants57. As improvement in insulin sensitivity and reversal of pre-diabetes have been reported with therapeutic interventions58, early identification of pre-diabetes among adolescents with obesity becomes increasingly important.
Although small, our study population was likely representative of Auckland’s ethnic and socioeconomic make-up, with relatively similar demographics when compared to national census data59. Both ethnicity and socioeconomic status are factors known to be associated with an increased risk of obesity and obesity-related diseases60. As we were able to recruit adolescents with obesity but not with any pre-diagnosed chronic conditions from the general population, our findings may be extrapolated to describe the health of adolescents with obesity in Auckland.
A strength of our study was our robust clinical assessments. In particular, accurate measurement of clinic BP is challenging, with wide variations due to many environmental factors61. 24hABPM, is a far more robust method to identify BP abnormalities compared to commonly used clinic devices62. Notably, pre-hypertension/hypertension was underdiagnosed when measured using the clinic BP monitor; only one in five was diagnosed to have elevated BP whereas with a 24hABPM, more than a third were reported to have elevated BP. Moreover, nearly a third of participants were diagnosed to have nocturnal prehypertension/hypertension which would have been undetected during daytime clinic BP measurements, and further emphasized the importance of undertaking BP monitoring over a 24-h period. Participants also underwent an OGTT which provided a more comprehensive assessment of glucose homeostasis and insulin sensitivity53.
In conclusion, we identified a high prevalence of undiagnosed comorbidities among adolescents with obesity. Of note, the high prevalence of metabolic syndrome in our study population emphasises the importance of screening adolescents with obesity for these metabolic complications. Obesity is a complex chronic condition that once established is not only difficult to treat, but requires life-long support41. As a result, it is undeniable that prevention of obesity should be the primary focus in this health crisis. However, for adolescents with established obesity, early identification of individuals with poor metabolic health and implementation of early targeted interventions are important, with the aim of preventing the development of overt cardiometabolic disease.
Data availability
The clinical data cannot be made available in a public repository according to the strict conditions of the study's ethics approval. Nonetheless, anonymized and de-identified data could be made available to other investigators upon bona fide request, and following all the necessary approvals (including ethics) of the detailed study proposal and statistical analyses plan. Any queries should be directed to Prof Wayne Cutfield (w.cutfield@auckland.ac.nz).
References
NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390, 2627–2642, https://doi.org/10.1016/s0140-6736(17)32129-3 (2017).
World Health Organization. Obesity and Overweight-Key Facts. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (2020).
World Health Organization. Global Health Observatory (GHA) Data Repository—Overweight/Obesity. https://apps.who.int/gho/data/node.main.A896 (2016).
New Zealand Ministry of Health. Tier 1 Statistics 2018/2019: New Zealand Health Survey, https://www.health.govt.nz/publication/tier-1-statistics-2018-19-new-zealand-health-survey (2019).
Olds, T. S., Tomkinson, G. R., Ferrar, K. E. & Maher, C. A. Trends in the prevalence of childhood overweight and obesity in Australia between 1985 and 2008. Int. J. Obes. (London) 34, 57–66. https://doi.org/10.1038/ijo.2009.211 (2010).
Pearson, S., Hansen, B., Sørensen, T. I. & Baker, J. L. Overweight and obesity trends in Copenhagen schoolchildren from 2002 to 2007. Acta Paediatr. 99, 1675–1678. https://doi.org/10.1111/j.1651-2227.2010.01897.x (2010).
Zhang, J. et al. Trends in the prevalence of overweight and obesity among Chinese school-age children and adolescents from 2010 to 2015. Child Obes. 14, 182–188. https://doi.org/10.1089/chi.2017.0309 (2018).
Skinner, A. C., Ravanbakht, S. N., Skelton, J. A., Perrin, E. M. & Armstrong, S. C. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 141, https://doi.org/10.1542/peds.2017-3459 (2018).
Rokholm, B., Baker, J. L. & Sørensen, T. I. A. The levelling off of the obesity epidemic since the year 1999—A review of evidence and perspectives. Obes. Rev. 11, 835–846. https://doi.org/10.1111/j.1467-789X.2010.00810.x (2010).
New Zealand Ministry of Health. Obesity Statistics. https://www.health.govt.nz/nz-health-statistics/health-statistics-and-data-sets/obesity-statistics (2019).
Utter, J., Denny, S., Teevale, T., Peiris-John, R. & Dyson, B. Prevalence and recent trends in overweight, obesity, and severe obesity among New Zealand adolescents. Child Obes. 11, 585–589. https://doi.org/10.1089/chi.2014.0151 (2015).
Patton, G. C. & Viner, R. Pubertal transitions in health. Lancet 369, 1130–1139. https://doi.org/10.1016/s0140-6736(07)60366-3 (2007).
Jasik, C. B. & Lustig, R. H. Adolescent obesity and puberty: The “perfect storm”. Ann. N. Y. Acad. Sci. 1135, 265–279 (2008).
Kelsey, M. M. & Zeitler, P. S. Insulin resistance of puberty. Curr. Diab. Rep. 16, 64. https://doi.org/10.1007/s11892-016-0751-5 (2016).
Gordon-Larsen, P., The, N. S. & Adair, L. S. Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity (Silver Spring) 18, 1801–1804. https://doi.org/10.1038/oby.2009.451 (2010).
Zimmet, P. et al. The metabolic syndrome in children and adolescents–An IDF consensus report. Pediatr. Diabetes 8, 299–306. https://doi.org/10.1111/j.1399-5448.2007.00271.x (2007).
Carnethon, M. R. et al. Risk factors for the metabolic syndrome: The Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2001. Diabetes Care 27, 2707–2715. https://doi.org/10.2337/diacare.27.11.2707 (2004).
Tailor, A. M., Peeters, P. H., Norat, T., Vineis, P. & Romaguera, D. An update on the prevalence of the metabolic syndrome in children and adolescents. Int. J. Pediatr. Obes. 5, 202–213. https://doi.org/10.3109/17477160903281079 (2010).
Mayer-Davis, E. J. et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N. Engl. J. Med. 376, 1419–1429. https://doi.org/10.1056/NEJMoa1610187 (2017).
Isomaa, B. et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24, 683–689. https://doi.org/10.2337/diacare.24.4.683 (2001).
Engin, A. The definition and prevalence of obesity and metabolic syndrome. Adv. Exp. Med. Biol. 960, 1–17. https://doi.org/10.1007/978-3-319-48382-5_1 (2017).
Demmer, R. T., Zuk, A. M., Rosenbaum, M. & Desvarieux, M. Prevalence of diagnosed and undiagnosed type 2 diabetes mellitus among US adolescents: Results from the continuous NHANES, 1999–2010. Am. J. Epidemiol. 178, 1106–1113. https://doi.org/10.1093/aje/kwt088 (2013).
Sjardin, N. et al. Increasing incidence of type 2 diabetes in New Zealand children <15 years of age in a regional-based diabetes service, Auckland, New Zealand. J. Paediatr. Child Health 54, 1005–1010. https://doi.org/10.1111/jpc.13924 (2018).
Lindberg, L., Danielsson, P., Persson, M., Marcus, C. & Hagman, E. Association of childhood obesity with risk of early all-cause and cause-specific mortality: A Swedish prospective cohort study. PLoS Med. 17, e1003078. https://doi.org/10.1371/journal.pmed.1003078 (2020).
Zabarsky, G. et al. Impact of severe obesity on cardiovascular risk factors in youth. J. Pediatr. 192, 105–114. https://doi.org/10.1016/j.jpeds.2017.09.066 (2018).
Daniels, S. R. Complications of obesity in children and adolescents. Int. J. Obes. (Lond.) 33(Suppl 1), S60-65. https://doi.org/10.1038/ijo.2009.20 (2009).
van Geel, M., Vedder, P. & Tanilon, J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the correlation between weight status and bullying. Int. J. Obes. (Lond.) 38, 1263–1267, https://doi.org/10.1038/ijo.2014.117 (2014).
Gortmaker, S. L., Must, A., Perrin, J. M., Sobol, A. M. & Dietz, W. H. Social and economic consequences of overweight in adolescence and young adulthood. N. Engl. J. Med. 329, 1008–1012. https://doi.org/10.1056/nejm199309303291406 (1993).
Quek, Y. H., Tam, W. W. S., Zhang, M. W. B. & Ho, R. C. M. Exploring the association between childhood and adolescent obesity and depression: A meta-analysis. Obes. Rev. 18, 742–754. https://doi.org/10.1111/obr.12535 (2017).
Anderson, Y. C. et al. Prevalence of comorbidities in obese New Zealand children and adolescents at enrolment in a Community-based obesity programme. J. Paediatr. Child Health 52, 1099–1105 (2016).
Grant, A. M. et al. Body mass index status is effective in identifying metabolic syndrome components and insulin resistance in Pacific Island teenagers living in New Zealand. Metabolism 57, 511–516. https://doi.org/10.1016/j.metabol.2007.11.013 (2008).
Leong, K. S. W. et al. Protocol for the Gut Bugs Trial: A randomised double-blind placebo-controlled trial of gut microbiome transfer for the treatment of obesity in adolescents. BMJ Open 9, e026174. https://doi.org/10.1136/bmjopen-2018-026174 (2019).
World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310, 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013).
de Onis, M. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 85, 660–667, https://doi.org/10.2471/blt.07.043497 (2007).
World Health Organization. Body Mass Index-BMI. https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (2006).
Wallace, T. M., Levy, J. C. & Matthews, D. R. Use and abuse of HOMA modeling. Diabetes Care 27, 1487–1495. https://doi.org/10.2337/diacare.27.6.1487 (2004).
Matsuda, M. & DeFronzo, R. Insulin sensitivity indices obtained from oral glucose tolerance testing: Comparison with the euglycemic insulin clamp. Diabetes Care 22, 1462–1470. https://doi.org/10.2337/diacare.22.9.1462 (1999).
Spiegelman, D. & Hertzmark, E. Easy SAS calculations for risk or prevalence ratios and differences. Am. J. Epidemiol. 162, 199–200. https://doi.org/10.1093/aje/kwi188 (2005).
Keskin, M., Kurtoglu, S., Kendirci, M., Atabek, M. E. & Yazici, C. Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics 115, e500–e503. https://doi.org/10.1542/peds.2004-1921 (2005).
Kernan, W. N. et al. Pioglitazone improves insulin sensitivity among nondiabetic patients with a recent transient ischemic attack or ischemic stroke. Stroke 34, 1431–1436. https://doi.org/10.1161/01.Str.0000071108.00234.0e (2003).
Lakshman, R., Elks, C. E. & Ong, K. K. Childhood obesity. Circulation 126, 1770–1779. https://doi.org/10.1161/circulationaha.111.047738 (2012).
Friend, A., Craig, L. & Turner, S. The prevalence of metabolic syndrome in children: A systematic review of the literature. Metab. Syndr. Relat. Disord. 11, 71–80. https://doi.org/10.1089/met.2012.0122 (2013).
Eyzaguirre, F. et al. Prevalence of metabolic syndrome in children and adolescents who consult with obesity. Rev. Med. Chil. 139, 732–738. https://doi.org/10.4067/S0034-98872011000600006 (2011).
Galera-Martínez, R. et al. Prevalence of metabolic syndrome among adolescents in a city in the Mediterranean area: Comparison of two definitions. Nutr. Hosp. 32, 627–633. https://doi.org/10.3305/nh.2015.32.2.9278 (2015).
Guijarro de Armas, M. A., Monereo Megías, S., Merino Viveros, M., Iglesias Bolaños, P. & Vega Piñero, B. Prevalence of metabolic syndrome in a population of obese children and adolescents. Endocrinol. Nutr. 59, 155–159, https://doi.org/10.1016/j.endonu.2012.01.003 (2012).
Romero-Velarde, E. et al. Prevalence of metabolic syndrome and associated factors in children and adolescents with obesity. Rev. Med. Inst. Mex. Seguro Soc. 54, 568–575 (2016).
Šimunović, M., Božić, J., Milić, L., Unić, I. & Škrabić, V. The prevalence of metabolic syndrome and cardiovascular risk factors in obese children and adolescents in dalmatia: A hospital based study. Int. J. Endocrinol. 2016, 1823561. https://doi.org/10.1155/2016/1823561 (2016).
Calcaterra, V. et al. Prevalence of metabolic syndrome (MS) in children and adolescents with varying degrees of obesity. Clin. Endocrinol. (Oxf.) 68, 868–872. https://doi.org/10.1111/j.1365-2265.2007.03115.x (2008).
Gobato, A. O., Vasques, A. C., Zambon, M. P., Barros Filho Ade, A. & Hessel, G. Metabolic syndrome and insulin resistance in obese adolescents. Rev. Paul Pediatr. 32, 55–62, https://doi.org/10.1590/s0103-05822014000100010 (2014).
Weiss, R. et al. Obesity and the metabolic syndrome in children and adolescents. N. Engl. J. Med. 350, 2362–2374. https://doi.org/10.1056/NEJMoa031049 (2004).
Lee, J. M., Okumura, M. J., Davis, M. M., Herman, W. H. & Gurney, J. G. Prevalence and determinants of insulin resistance among U.S. adolescents: a population-based study. Diabetes Care 29, 2427–2432, https://doi.org/10.2337/dc06-0709 (2006).
Koutny, F. et al. Prevalence of prediabetes and type 2 diabetes in children with obesity and increased transaminases in European German-speaking countries. Analysis of the APV initiative. Pediatr. Obes. 15, e12601, https://doi.org/10.1111/ijpo.12601 (2020).
American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes 2018. Diabetes Care 41, S13–S27. https://doi.org/10.2337/dc18-S002 (2018).
Mayer-Davis, E. J. et al. ISPAD Clinical Practice Consensus Guidelines 2018: Definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr. Diabetes 19(Suppl 27), 7–19. https://doi.org/10.1111/pedi.12773 (2018).
World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: Report of a WHO/IDF consultation. in Report No. 9241594934 (Geneva, Switzerland, 2006).
Lee, A. M., Fermin, C. R., Filipp, S. L., Gurka, M. J. & DeBoer, M. D. Examining trends in prediabetes and its relationship with the metabolic syndrome in US adolescents, 1999–2014. Acta Diabetol. 54, 373–381. https://doi.org/10.1007/s00592-016-0958-6 (2017).
Nichols, G. A., Hillier, T. A. & Brown, J. B. Progression from newly acquired impaired fasting glucose to type 2 diabetes. Diabetes Care 30, 228–233. https://doi.org/10.2337/dc06-1392 (2007).
Garnett, S. P. et al. Improved insulin sensitivity and body composition, irrespective of macronutrient intake, after a 12 month intervention in adolescents with pre-diabetes; RESIST a randomised control trial. BMC Pediatr. 14, 289. https://doi.org/10.1186/s12887-014-0289-0 (2014).
Stats NZ. 2013 Census Tables About a Place. https://archive.stats.govt.nz/Census/2013-census/data-tables/tables-about-a-place.aspx (2013).
Woo Baidal, J. A. et al. Risk factors for childhood obesity in the first 1,000 days: A systematic review. Am. J. Prev. Med. 50, 761–779, https://doi.org/10.1016/j.amepre.2015.11.012 (2016).
O’Brien, E., Waeber, B., Parati, G., Staessen, J. & Myers, M. G. Blood pressure measuring devices: Recommendations of the European Society of Hypertension. BMJ 322, 531–536. https://doi.org/10.1136/bmj.322.7285.531 (2001).
Lurbe, E. et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34, 1887–1920. https://doi.org/10.1097/HJH.0000000000001039 (2016).
Eisenmann, J. C. Waist circumference percentiles for 7- to 15-year-old Australian children. Acta Paediatr. 94, 1182–1185. https://doi.org/10.1111/j.1651-2227.2005.tb02071.x (2005).
Frithioff-Bøjsøe, C. et al. Glucose metabolism in children and adolescents: Population-based reference values and comparisons to children and adolescents enrolled in obesity treatment. Pediatr. Diabetes 20, 538–548. https://doi.org/10.1111/pedi.12859 (2019).
NCEP Expert Panel. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 285, 2486–2497, https://doi.org/10.1001/jama.285.19.2486 (2001).
European Atherosclerosis Society. Strategies for the prevention of coronary heart disease: A policy statement of the European Atherosclerosis Society. Eur. Heart J. 8, 77–88. https://doi.org/10.1093/oxfordjournals.eurheartj.a062165 (1987).
Thefeld, W., Hoffmeister, H., Busch, E.-W., Koller, P. & Vollmar, J. Normal values of serum uric acid depending on age and sex with one new enzymatic uric acid color test. Dtsch. Med. Woschenschr. 98, 380–384. https://doi.org/10.1055/s-0028-1106819 (1973).
Schlebusch, H., Liappis, N., Kalina, E. & Klein, C. High sensitive CRP and creatinine: reference intervals from infancy to childhood. J. Lab. Med. 26, 341–346. https://doi.org/10.1046/j.1439-0477.2002.02071.x (2002).
Dati, F. et al. Consensus of a group of professional societies and diagnostic companies on guidelines for interim reference ranges for 14 proteins in serum based on the standardization against the IFCC/BCR/CAP reference material (CRM 470). Eur. J. Clin. Chem. Clin. Biochem. 34, 517–520 (1996).
Klein, G., Lehmann, P., Michel, E. & Regenauer, H. Comparison of the IFCC methods for ALT, AST and GGT at 37 °C with the established standard methods at 25 °C and 37 °C. Lab. Med. 18, 403–404 (1994).
Thefeld, W., Hoffmeister, H., Busch, E.-W., Koller, P. & Vollmar, J. Reference values for the determinations of the transaminases GOT and GPT as well as serum alkaline phosphatase using optimized standard methods. Dtsch. Med. Wochenschr. 99, 343–351. https://doi.org/10.1055/s-0028-1107760 (1974).
Thomas, L. et al. Consensus of DGKL and VDGH for interim reference intervals on enzymes in serum. J. Lab. Med. 29, 301–308. https://doi.org/10.1515/JLM.2005.041 (2005).
Exeter, D., Browne, M. M., Crengle, S., Lee, A. & Zhao, J. New Zealand indices of multiple deprivation (IMD). PLoS ONE 12, e0181260. https://doi.org/10.1371/journal.pone.0181260 (2016).
Funding
This study was funded by the Rockfield Trust and A Better Start-National Science Challenge. V Chiavaroli was supported (in part) by a European Society for Paediatric Endocrinology (ESPE) Research Fellowship, sponsored by Novo Nordisk A/S; TN Jayasinghe received a University of Auckland Scholarship; and BB Albert was supported by Rutherford and Maurice Paykel Research Fellowships.
Author information
Authors and Affiliations
Contributions
W.S.C. and J.O.S. supervised all aspects of the research study. W.S.C. and J.O.S. led the Gut Bugs Trial conception and design. All authors contributed to the Gut Bugs Trial conception and design. K.S.W.L. and J.G.B.D. compiled the data, which were analysed by K.S.W.L. and J.G.B.D. All authors contributed to the interpretation of the results. K.S.W.L., J.G.B.D., and W.S.C. wrote the manuscript with critical input from all other authors. W.S.C. and J.O.S. had full access to all the data in the trial and had final responsibility for the decision to submit the trial for publication. All authors have approved the final version of this manuscript and have agreed to be accountable for all aspects of this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leong, K.S.W., Jayasinghe, T.N., Wilson, B.C. et al. High prevalence of undiagnosed comorbidities among adolescents with obesity. Sci Rep 10, 20101 (2020). https://doi.org/10.1038/s41598-020-76921-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-76921-6
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.