Abstract
To conduct a systematic review and meta-analyses on short-term outcomes between total hip arthroplasty (THA) through direct anterior approach (DAA) compared to THA through conventional approaches (CAs) in treatment of hip diseases and fractures. We performed a systematic literature search up to March 1, 2021 to identify RCTs, comparing THA through DAA with THA through CAs. We calculated mean differences (MDs) with 95% confidence intervals (CIs) for continuous outcomes, using the DerSimonian and Laird method and a random effects model. We calculated odds ratios (ORs) with 95% CIs for dichotomous outcomes, using the Mantel–Haenszel method and a random effects model. Ten RCTs met the criteria for final meta-analysis, involving 1053 patients. Four studies were blinded RCTs with a level I evidence, the other 6 studies were non-blinded RCTs with a level II evidence. DAA had a longer operation time than CAs (MD = 17.8, 95% CI 4.8 to 30.8); DAA had similar results compared to CAs for incision length (MD = − 1.1, 95% CI − 4.1 to 1.8), for intraoperative blood loss (MD = 67.2, 95% CI − 34.8 to 169.1), for HHS 3 months postoperatively (MD = 2.4, 95% CI − 0.7 to 5.5), for HHS 6 months postoperatively (MD = 0.8, 95% CI − 1.9 to 3.5), for HHS 12 months postoperatively (MD = 0.9, 95% CI − 0.7 to 2.5), for pain VAS 1 day postoperatively (MD = − 0.9, 95% CI − 2.0 to 0.15), for acetabular cup anteversion angle (MD = − 4.3, 95% CI − 5.2 to − 3.5), for acetabular cup inclination angle (MD = − 0.5, 95% CI − 2.1 to 1.1) and for postoperative complications (OR = 2.4, 95% CI 0.5 to 12.4). Considering the overall results of our meta-analysis, we can conclude that THA through DAA showed similar short-term surgical, functional, radiological outcomes and postoperative complications compared to THA through CAs.
Similar content being viewed by others
Introduction
Several systematic reviews and meta-analyses on short-term outcomes between total hip arthroplasty (THA) through direct anterior approach (DAA) compared to THA through conventional approaches (CAs)1,2,3,4,5,6,7,8,9 came to contradicting conclusions. While some of them found an advantage of DAA2,3,4,6,7,8, others showed indifferent results1,5,9. Most of those meta-analyses had relevant limitations. The 2015 meta-analysis by Higgins et al.1, comparing DAA with posterior approach, included 17 studies (2 RCTs, 10 retrospective, and 5 non-randomized prospective studies) with a total of 2302 patients. The 2019 meta-analysis by Jia et al.2, comparing DAA with posterior approach, included 20 studies (4 RCTs, 3 prospective studies and 13 retrospective studies) with a total of 7377 patients. The 2015 meta-analysis by Yue et al.7, the first meta-analysis comparing DAA with lateral approach, included 12 studies (2 RCTs and 10 non-RCTs) with 2,991 cases of THA through DAA and 1,910 cases of THA through lateral approach. Unfortunately, the inclusion of studies with a low level of evidence in these meta-analyses1,2,7 affects the validity of the end point estimates and overall results. The 2019 meta-analysis by Kucukdurmaz et al.3, comparing DAA with other approaches, included 18 RCTs with a total of 1,661 patients. Only this meta-analysis considered the influence of traction (fracture) table utilization in THA through DAA3. Unfortunately, navigated THA and THA through mini-incision approaches were pooled in one group, which presents a severe confounding factor. Furthermore, three relevant recent RCTs10,11,12 were not included in final meta-analysis. The 2018 meta-analysis by Miller et al.4, comparing DAA with posterior approach, included 13 prospective studies (7 RCTs and 6 non-RCTs) with 1,044 patients. This meta-analysis had a very short follow-up period of 3 months. Furthermore, some outcome parameters were grouped together, but measured at very different time points. The 2018 meta-analysis by Wang et al.6, the first meta-analysis comparing DAA with posterior approach, included 9 RCTs with a total of 854 patients. It was performed with high quality methods. The 2018 meta-analysis by Putananon et al.5, the first network meta-analysis comparing outcomes of different surgical approaches in THA, included 14 RCTs with a total of 1,201 patients. It investigated the outcomes of THA through DAA, lateral, posterior and posterior-2-incision approaches. This network meta-analysis limited their investigation to three outcome parameters: VAS, HHS and postoperative complications. Posterior and posterior-2-incision approaches were pooled based on only two studies. The systematic reviews by Kyriakopoulos et al. and Meermans et al. did not perform a meta-analysis8,9. In order to overcome these limitations of the related previous systematic reviews and meta-analyses1,2,3,4,5,6,7,8,9, a new meta-analysis was required with a more extensive literature search, with restriction to RCTs and with implementation of high-quality statistical methods.
Our aim was to compare short-term outcomes of THA through DAA and THA through CAs in treatment of hip diseases and femoral neck fractures by performing a systematic literature review and meta-analysis of RCTs.
Methods
Literature search and study selection
Our review protocol was registered and approved with PROSPERO on 28 February 2021 (CRD42021233481). We followed the PRISMA-P guidelines to report our meta-analysis. Our search was performed up to March 1, 2021 in the following databases: PubMed, Embase, Web of Science, The Cochrane Library, SCOPUS, CINAHL, Clinical Trials. We used a BOOLEAN search strategy [(DAA) OR (direct anterior approach)], adapted to the syntax of the used databases. Furthermore, we checked citations of screened studies and Google Scholar for additional records. Titles and abstracts were screened to identify articles for further consideration, full text of the selected articles were screened again according to inclusion criteria. The study selection was determined by the consensus of two independent reviewers (NR and PL). Kappa coefficient was used to measure the agreement between the reviewers.
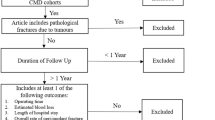
Inclusion/exclusion criteria and outcomes
Inclusion criteria were as follows: RCTs with no restriction to language and publication date, comparing outcomes in THA through DAA and THA through CAs. We included human participants with the following hip pathologies: osteoarthritis, avascular necrosis of the femoral head, dysplasia, femoral neck fracture. We excluded studies on THA through mini-incision approaches as well as surgical techniques, using a computer navigation system. The types of measured outcomes were the following: The operation time in min. was defined as the period of time from the beginning of skin incision to surgical closure. The incision length in cm was measured on graduated scale. The intraoperative blood loss in ml was the total amount of blood from the suction device. The pain Visual Analogue Scale (VAS)13,14 ranges from 0 to 10 points, with the pain intensity increasing with the number of points. Hip pain was evaluated at day 1 after surgery. The Harris Hip Score (HHS)15 ranges from 0 to 100 points, with hip function increasing with the number of points. It was evaluated at periodic time intervals after surgery. The acetabular cup anteversion and the inclination have ideal values for positioning: anteversion angle from 10° to 25° and inclination angle from 35° to 45°.
Data extraction and study quality assessment
We extracted data on study characteristics, methods, quality assessment, characteristics of participants, details of the interventions, and measured outcomes into a standard electronic spreadsheet. We contacted corresponding authors for missing data. In case that relevant data was still missing, the concerning study was excluded in order to guarantee a high quality inclusion of RCTs. Risk of bias and level of evidence assessment were performed according to the Cochrane’s Risk of Bias 2 (RoB 2) tool16 and the guidelines of the Centre for Evidence-Based Medicine17.
Statistical analysis
DAA represented the “experimental group” and CAs represented the “control group”. We tested both fixed and random effects models. The random effects model provided more reliable results, so we proceeded as follows: We calculated mean differences (MDs) with 95% confidence intervals (CIs) for continuous outcomes, using the DerSimonian and Laird method and a random effects model. We calculated odds ratios (ORs) with 95% CIs for dichotomous outcomes, using the Mantel–Haenszel method and a random effects model. A common τ2 was assumed for calculation of the random effects estimates. Study weighting was performed by inverse variance18. We evaluated the results and analysed them on basis of the Cochrane Handbook for Systematic Reviews of Interventions19. We did not pool study data that were clinically too diverse. Heterogeneity was assessed using a test on Cochrane’s Q statistic, which followed a distribution with k-degrees of freedom (p value < 0.10 is indicative of heterogeneity), and a Higgins’ test I2 (low heterogeneity, < 25%; moderate heterogeneity, 25–75%; and high heterogeneity, > 75%)20. We performed a traction table subgroup-analysis in order to examine the influence of traction table utilization in THA through DAA.
Results
Study identification and selection
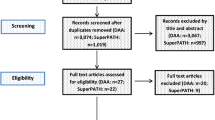
After removal of 824 duplicates, a total of 7,024 studies were found in initial literature search. Forty-one studies were assessed for eligibility after first screening procedure by title and abstract with disagreement between the reviewers concerning one study (κ = 0.98). Thirty-one studies were excluded after full-text screening according to inclusion criteria (κ = 1.0). Four of those studies were excluded because they did not provide any information on standard deviation of the outcome parameters examined21,22,23,24. A total of 10 studies on THA through DAA met the criteria for final meta-analysis10,11,12,25,26,27,28,29,30,31. Details of study identification, screening, and selection are given in a PRISMA flow diagram (Fig. 1).
Characteristics of the RCTs
Table 1 gives an overview of the main characteristics of the 10 included RCTs, published between 2009 and 2020, altogether involving 1,053 patients with 1,057 operated hip joints. Of these, 468 were operated through DAA and 585 through CAs. The sample size of the 10 studies ranged from 46 to 169 patients, all published in English language. Of the 10 studies, 4 included conventional THA through posterolateral approach10,25,30,31, one through posterior approach12, 5 through lateral transgluteal approach11,26,27,28,29. Three studies reported to have used traction table in THA through DAA10,12,25. Only one study included patients with bilateral THA31.
Risk of bias and level of evidence
Four out of 10 studies were rated with a low risk of bias10,12,28,31, 4 studies with a moderate risk of bias11,26,27,29 and 2 studies with a high risk of bias25,30 as shown in Table 2. Four out of 10 studies were blinded RCTs with a level I evidence10,12,28,31, the other 6 studies were non-blinded RCTs with a level II evidence11,25,26,27,29,30.
Outcomes
Operation time
Data on 672 patients were pooled from 7 RCTs (I2 = 90%, p < 0.01, Fig. 2). The operation time of THA through DAA was 17.8 min. longer than the operation time of THA through CAs (MD = 17.8, 95% CI 4.8 to 30.8).
Incision length
Data on 372 patients were pooled from 4 RCTs (I2 = 100%, p < 0.01, Fig. 2). There was no difference in incision length (MD = − 1.1, 95% CI − 4.1 to 1.8).
Intraoperative blood loss
Data on 418 patients were pooled from 4 RCTs (I2 = 87%, p < 0.01, Fig. 2). There was no difference in intraoperative blood loss (MD = 67.2, 95% CI − 34.8 to 169.1).
HHS
Data on 505 patients were pooled from 5 RCTs (I2 = 10%, p = 0.35, Fig. 3). There was no difference in HHS 3 months postoperatively (MD = 2.4, 95% CI − 0.7 to 5.5). Data on 406 patients were pooled from 4 RCTs (I2 = 0%, p = 0.82, Fig. 3). There was no difference in HHS 6 months postoperatively (MD = 0.8, 95% CI − 1.9 to 3.5). Data on 389 patients were pooled from 4 RCTs (I2 = 0%, p = 0.80, Fig. 3). There was no difference in HHS 12 months postoperatively (MD = 0.9, 95% CI − 0.7 to 2.5).
Pain VAS 1 day postoperatively
Data on 250 patients were pooled from 2 RCTs (I2 = 79%, p = 0.03, Fig. 3). There was no difference in pain VAS 1 day postoperatively (MD = -0.9, 95% CI − 2.0 to 0.15).
Acetabular cup positioning
Data on 203 patients were pooled from 2 RCTs (I2 = 0%, p = 0.34, Fig. 4). The acetabular cup anteversion angle of THA through DAA was 4.3° lower than the acetabular cup anteversion angle of THA through CAs (MD = − 4.3, 95% CI − 5.2 to − 3.5). Data on 576 patients were pooled from 6 RCTs (I2 = 83%, p < 0.01, Fig. 4). There was no difference in acetabular cup inclination angle (MD = − 0.5, 95% CI − 2.1 to 1.1).
Postoperative complications
Data on 394 patients were pooled from 4 RCTs (I2 = 53%, p = 0.10, Fig. 4). There was no difference in postoperative complications (OR = 2.4, 95% CI 0.5 to 12.4).
Traction table subgroup analysis
A traction table was used in three10,12,25 out of 10 studies on THA through DAA. The utilization of traction table in THA through DAA showed no influence on the overall effect of the DAA group.
Discussion
Main findings
In order to overcome the limitations of the related previous systematic reviews and meta-analyses1,2,3,4,5,6,7,8,9, we conducted our meta-analysis with a more extensive literature search, with restriction to RCTs and with implementation of high-quality statistical methods, testing both fixed and random effects models. Our direct comparison in meta-analysis on short-term outcomes between THA through DAA and CAs included 10 RCTs and 1,053 patients. Four out of 10 studies were blinded RCTs with a level I evidence10,12,28,31, the other 6 studies were non-blinded RCTs with a level II evidence11,25,26,27,29,30. THA through DAA showed overall similar surgical, functional, radiological outcomes and postoperative complications compared to THA through CAs. Both approaches showed overall sufficient results in acetabular cup positioning. THA through DAA showed a longer operation time compared to THA through CAs. We found no influence of traction table utilization on outcomes in THA through DAA.
Operation time
Our meta-analysis found that the operation time of THA through DAA was 17.8 min. longer than the operation time of THA through CAs. The mean operation time varied from 59.9 to 121.0 min. for DAA and from 45.7 to 78.2 min. for CAs. The meta-analyses by Kucukdurmaz et al. 3 and Yue et al.7 found similarly prolonged operation times in THA through DAA. In contrast, the meta-analyses by Higgins et al.1 and Wang et al.6 found no difference. Operation time is an outcome parameter that is very difficult to generalize, as there are certainly some confounding factors. During the surgeon's learning curve period, there usually is a prolonged operation time. However, it remains unclear whether THA through DAA were implanted by learners, skilled surgeons, or experts. It is possible to significantly reduce operation time in THA through DAA by acquisition of surgical skills32. The wide variation in operation times in THA through DAA from 59.9 to 121 min. supports the idea that the surgeon’s proficiency plays an important role and shows that there is potential for a shorter operation time.
Incision length
Our meta-analysis found no difference in incision length of THA through DAA compared to THA through CAs. The mean incision length varied from 9.1 to 13.7 cm for DAA and from 10.4 to 14.8 cm for CAs. In contrast, the meta-analyses by Kucukdurmaz et al.3 found that THA through DAA had a 3.2 cm shorter incision length than THA through other approaches. The meta-analysis by Wang et al.6 showed a 3.5 cm shorter incision length of THA through DAA than THA through posterior approach.
Intraoperative blood loss
Our meta-analysis found no difference in intraoperative blood loss of THA through DAA compared to THA through CAs. The mean intraoperative blood loss varied from 165.9 to 1344.0 ml for DAA and from 123.8 to 1644.0 ml for CAs. The meta-analysis by Higgins et al.1 also showed no difference in intraoperative blood loss. The meta-analysis by Wang et al.6 showed a lower postoperative blood loss of 67 ml in THA through DAA compared to THA through posterior approach. The meta-analysis by Yue et al.7 showed no difference in postoperative blood transfusion rates between THA through DAA and THA through lateral approach. However, sufficient conclusions about the extent of the tissue trauma cannot be drawn only by determining the intraoperative blood loss. Further outcome parameters such as total blood loss and laboratory parameters such as CRP, IL-6, IL-10, IL-1a, ESR, and CK must also be considered.
Harris hip score
Our meta-analysis showed no difference in HHS 3, 6 and 12 months postoperatively in THA through DAA compared to THA through CAs. The mean HHS 3 months postoperatively varied from 85.9 to 94.6 points for DAA and from 79.6 to 92.8 points for CAs. The mean HHS 6 months postoperatively varied from 90.1 to 95.8 points for DAA and from 89.1 to 95.9 points for CAs. The mean HHS 12 months postoperatively varied from 92.4 to 97.5 points for DAA and from 91.4 to 97.3 points for CAs. The meta-analysis by Higgins et al.1 examined several different scores (HHS, HOOS, S&R, SF, WOMAC, Oxford Hip Score, Japanese Orthopedic Association Hip Score) describing the functional outcome. The follow-up time for functional outcome varied from 1.5–3 months postoperatively. The overall results showed a weak tendency towards better outcome in THA through DAA compared to THA through posterior approach. The meta-analysis by Kucukdurmaz et al.3 found a 5.6 points higher HHS and a 3.1 points lower WOMAC 1.5 months postoperatively in THA through than THA through other approaches. In contrast to the HHS, in WOMAC a lower result is considered as better and a higher result as worse. The meta-analysis by Miller et al.4 showed an overall 0.3 point higher HHS in THA through DAA than THA through posterior approach. The HHS was measured at different time points 3 months postoperatively. The network meta-analysis by Putananon et al.5 ranked four hip approaches in order from best to fourth best with regard to the HHS 1–1.5 months postoperatively as follows: DAA, lateral approach, posterior and posterior-2-incision approach. THA through DAA had a 2.6 points higher HHS than THA through lateral approach, a 4.8 points higher HHS than THA through posterior approach and a 10.8 higher HHS than THA through posterior-2-incision approach. The meta-analysis by Wang et al.6 found that THA through DAA had a 7.4 higher HHS 0.5 months postoperatively than THA through posterior approach and a 6.8 points higher HHS 1.5 months postoperatively than THA through posterior approach. The meta-analysis by Yue et al.7 examined several different scores (HHS, SF-36, UCLA, DAQ, WOMAC, LEFS, and LASA) describing the functional outcome. The follow-up time for functional outcome varied from 1.5 months up to years postoperatively. They stated an overall better functional outcome of THA through DAA compared to THA through lateral approach. The improved functional outcome, which several meta-analyses found in THA through DAA, follows the lower tissue and muscle damage, presumably due to operating in a muscle-sparing anatomical plane. Lower tissue and muscle damage in DAA was determined by measuring the levels of relevant laboratory parameters such as CRP, IL-6, IL-10, IL-1a, ESR, and CK in several studies28,31,33,34.
VAS 1 day postoperatively
The mean pain VAS 1 day postoperatively varied from 2.6 to 4.0 points for DAA and from 4.0 to 4.5 points for CAs. Our meta-analysis showed no difference in pain VAS 1 day postoperatively. In contrast, several related meta-analyses found a lower pain VAS in THA through DAA compared to THA through CAs3,4,6. The meta-analysis by Kucukdurmaz et al.3 found a 1.3 points lower pain VAS 1 day postoperatively in THA through DAA compared to THA through other approaches. The meta-analysis by Miller et al.4 found a 0.4 points lower pain VAS in THA through DAA compared to THA through posterior approach, with pain recorded at various time points in a 3 months postoperative follow-up. The meta-analysis by Wang et al.6 found a 0.7, 1.5 and 1.6 points lower VAS 1,2 and 3 days postoperatively in THA through DAA compared to THA through posterior approach. The network meta-analysis by Putananon et al.5 ranked four hip approaches in order from best to fourth best with regard to the postoperative pain VAS as follows: lateral approach, DAA, posterior and posterior-2-incision approach. The pain was measured at any postoperative time point. The lower pain intensity in THA through DAA probably occurs for reasons similar to the better functional outcome: the lower tissue and muscle damage, presumably due to operating in a muscle-sparing anatomical plane.
Acetabular cup positioning
The acetabular cup anteversion angle varied from 17.1° to 20.1° in THA through DAA and the acetabular cup inclination angle varied from 37.0° to 47.1° in THA through DAA. The acetabular cup anteversion angle varied from 21.3° to 25.8° in THA through CAs and the acetabular cup inclination angle varied from 39.6° to 42.4° in THA through CAs. Since the ideal values for acetabular cup positioning range from 10° to 25° for anteversion and from 35° to 45° for inclination, both approaches seem to show sufficient results regarding the safe zone with clinically irrelevant differences between each other. However, THA through DAA showed a slight tendency towards a too flat inclination angle (outlier rate: 5%). The related meta-analyses by Higgins et al.1, Jia et al.2 by Yue et al.7 showed no differences in acetabular cup positioning. A 2017 systematic review by Seagrave et al.33 found that broad conclusions regarding a definitive target zone for cup positioning in THA still cannot be drawn. The ideal target zone for each patient varies, influenced by several confounding factors. The acetabular cup positioning within a target zone cannot eliminate the risk of dislocation35.
Postoperative complications
Our meta-analysis found no difference in postoperative complications of THA through DAA compared to THA through CAs. Bon et al.10 found one case (2%) of dislocation and 8 cases (16%) of neuropraxia of the lateral cutaneous nerve of the thigh in 50 patients, operated through DAA. Complications did not occur (0%) in 50 patients, operated through CAs. Moerenhout et al.12 found one case (3.6%) of infection in 28 patients, operated through DAA. Two cases (7.4%) of periprosthetic fracture occurred in 27 patients, operated through CAs. D’Arrigo et al.26 found 2 cases (10%) of periprosthetic fracture, one case (5%) of rupture of m. tensor fasciae latae, and 2 cases (10%) of haematoma in 20 patients, operated through DAA. One case (0.7%) of periprosthetic fracture, one case (0.7%) of cup malposition, and one case (0.7%) of infection occurred in 149 patients, operated through CAs. Nistor et al.29 found one case (2.9%) of periprosthetic fracture, one case (2.9%) of haematoma and 2 cases (5.7%) of neuropraxia of the lateral cutaneous nerve of the thigh in 35 patients, operated through DAA. Two cases (5.7%) of haematoma, and one case (2.9%) of suture granuloma occured in 35 patients, operated through CAs.
Traction table utilization
In subgroup analysis our study showed that there was no influence of traction table utilization on outcomes in THA through DAA. A recent 2020 systematic review on DAA by Sarraj et al. included 44 studies with a total of 26,353 patients36. The study found no relevant difference in outcome between traction table versus standard table THA through DAA.
Limitations
We identified the following limitations to our study: First, the long-term outcomes in THA were not considered. Second, due to insufficient data, important outcome parameters such as hospitalization time, postoperative drainage volume and postoperative gait analysis could not be considered. Third, we did not consider the possible influence of the surgeon operating skills, the utilization of tranexamic acid and anticoagulants, bone cement or the types of implants for THA. Lastly, conventional approaches were summarized in one group, although they differ greatly from one another.
Conclusion
Considering the overall results of our meta-analysis, we can conclude that THA through DAA showed similar short-term surgical, functional, radiological outcomes and postoperative complications compared to THA through CAs.
Data availability
The data are available from the corresponding author upon reasonable request.
Abbreviations
- CI:
-
Confidence intervals
- CA:
-
Conventional approach
- CK:
-
Creatine kinase
- CRP:
-
C-reactive protein
- DAA:
-
Direct anterior approach
- ESR:
-
Erythrocyte sedimentation rate
- HHS:
-
Harris hip score
- IL-1a:
-
Interleukin 1a
- IL-6:
-
Interleukin 6
- IL-10:
-
Interleukin 10
- MD:
-
Mean difference
- RCT:
-
Randomized controlled trial
- RoB:
-
Risk of bias
- OR:
-
Odds ratio
- THA:
-
Total hip arthroplasty
- VAS:
-
Visual analogue scale
References
Higgins, B. T., Barlow, D. R., Heagerty, N. E. & Lin, T. J. Anterior vs posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J. Arthroplasty. 30(3), 419–434. https://doi.org/10.1016/j.arth.2014.10.020 (2015).
Jia, F. et al. A comparison of clinical, radiographic and surgical outcomes of total hip arthroplasty between direct anterior and posterior approaches: A systematic review and meta-analysis. Hip Int. 29(6), 584–596. https://doi.org/10.1177/1120700018820652 (2019).
Kucukdurmaz, F., Sukeik, M. & Parvizi, J. A meta-analysis comparing the direct anterior with other approaches in primary total hip arthroplasty. Surgeon. 17(5), 291–299. https://doi.org/10.1016/j.surge.2018.09.001 (2019).
Miller, L. E. et al. Does surgical approach affect outcomes in total hip arthroplasty through 90 days of follow-up? A systematic review with meta-analysis. J. Arthroplasty. 33(4), 1296–1302. https://doi.org/10.1016/j.arth.2017.11.011 (2018).
Putananon, C. et al. Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: network meta-analysis. Eur. J. Orthop. Surg. Traumatol. 28(2), 255–267. https://doi.org/10.1007/s00590-017-2046-1 (2018).
Wang, Z. et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J. Orthop. Surg. Res. 13(1), 229. https://doi.org/10.1186/s13018-018-0929-4 (2018).
Yue, C., Kang, P. & Pei, F. Comparison of direct anterior and lateral approaches in total hip arthroplasty: A systematic review and meta-analysis (PRISMA). Medicine (Baltimore) 94(50), e2126. https://doi.org/10.1097/MD.0000000000002126 (2015).
Kyriakopoulos, G., Poultsides, L. & Christofilopoulos, P. Total hip arthroplasty through an anterior approach: The pros and cons. EFORT Open Rev. 3(11), 574–583. https://doi.org/10.1302/2058-5241.3.180023 (2018).
Meermans, G., Konan, S., Das, R., Volpin, A. & Haddad, F. S. The direct anterior approach in total hip arthroplasty: A systematic review of the literature. Bone Joint J. 99(6), 732–740. https://doi.org/10.1302/0301-620X.99B6.38053 (2017).
Bon, G. et al. Does the direct anterior approach allow earlier recovery of walking following total hip arthroplasty? A randomized prospective trial using accelerometry. Orthop. Traumatol. Surg. Res. 105(3), 445–452. https://doi.org/10.1016/j.otsr.2019.02.008 (2019).
Reichert, J. C. et al. A prospective randomized comparison of the minimally invasive direct anterior and the transgluteal approach for primary total hip arthroplasty. BMC Musculoskelet. Disord. 19(1), 241. https://doi.org/10.1186/s12891-018-2133-4 (2018).
Moerenhout, K. et al. Direct anterior versus posterior approach for total hip arthroplasty: a multicentre, prospective, randomized clinical trial. Can. J. Surg. 63, E412–E417 (2020).
Gould, D. et al. Visual analogue scale (VAS). J. Clin. Nurs. 10, 697–706 (2001).
Huskisson, E. C. Measurement of pain. Lancet 2, 1127–1131 (1974).
Harris, W. H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Jt. Surg. Am. 51, 737–755 (1969).
Sterne, J.A.C., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898. (2019) Available from www.riskofbias.info (10.01.2020)
Centre for Evidence-Based Medicine. Levels of evidence (March 2009). Available at: https://www.cebm.net/2009/06/oxford-centre-evidence-basedmedicine-levels-evidence-march-2009/. Accessed 28 January 2021.
Deeks, J.J., Higgins, J.P.T., Altman, D.G. (eds) Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook. Accessed 15 October 2020.
Schünemann, H.J., et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A. (eds). Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Brismar, B. H., Hallert, O., Tedhamre, A. & Lindgren, J. U. Early gain in pain reduction and hip function, but more complications following the direct anterior minimally invasive approach for total hip arthroplasty: A randomized trial of 100 patients with 5 years of follow up. Acta Orthop. 89(5), 484–489. https://doi.org/10.1080/17453674.2018.1504505 (2018).
Cheng, T. E. et al. A prospective randomized clinical trial in total hip arthroplasty-comparing early results between the direct anterior approach and the posterior approach. J. Arthroplasty. 32(3), 883–890. https://doi.org/10.1016/j.arth.2016.08.027 (2017).
Christensen, C. P. & Jacobs, C. A. Comparison of patient function during the first six weeks after direct anterior or posterior total hip arthroplasty (THA): A randomized study. J. Arthroplasty. 30(9 Suppl), 94–97. https://doi.org/10.1016/j.arth.2014.12.038 (2015).
Restrepo, C., Parvizi, J., Pour, A. E. & Hozack, W. J. Prospective randomized study of two surgical approaches for total hip arthroplasty. J. Arthroplasty. 25(5), 671–9.e1. https://doi.org/10.1016/j.arth.2010.02.002 (2010).
Barrett, W. P., Turner, S. E. & Leopold, J. P. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J. Arthroplasty. 28(9), 1634–1638. https://doi.org/10.1016/j.arth.2013.01.034 (2013).
D’Arrigo, C., Speranza, A., Monaco, E., Carcangiu, A. & Ferretti, A. Learning curve in tissue sparing total hip replacement: Comparison between different approaches. J. Orthop. Traumatol. 10(1), 47–54. https://doi.org/10.1007/s10195-008-0043-1 (2009).
De Anta-Díaz, B., Serralta-Gomis, J., Lizaur-Utrilla, A., Benavidez, E. & López-Prats, F. A. No differences between direct anterior and lateral approach for primary total hip arthroplasty related to muscle damage or functional outcome. Int. Orthop. 40(10), 2025–2030. https://doi.org/10.1007/s00264-015-3108-9 (2016).
Mjaaland, K. E., Kivle, K., Svenningsen, S., Pripp, A. H. & Nordsletten, L. Comparison of markers for muscle damage, inflammation, and pain using minimally invasive direct anterior versus direct lateral approach in total hip arthroplasty: A prospective, randomized, controlled trial. J. Orthop. Res. 33(9), 1305–1310. https://doi.org/10.1002/jor.22911 (2015).
Nistor, D. V. et al. Transitioning to the direct anterior approach in total hip arthroplasty. Is it a true muscle sparing approach when performed by a low volume hip replacement surgeon?. Int. Orthop. 41(11), 2245–2252. https://doi.org/10.1007/s00264-017-3480-8 (2017).
Rykov, K., Reininga, I. H. F., Sietsma, M. S., Knobben, B. A. S. & Ten Have, B. L. E. F. Posterolateral vs direct anterior approach in total hip arthroplasty (POLADA trial): A randomized controlled trial to assess differences in serum markers. J. Arthroplasty. 32(12), 3652-3658.e1. https://doi.org/10.1016/j.arth.2017.07.008 (2017).
Zhao, H. Y. et al. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: A randomized controlled trial. J. Arthroplasty. 32(11), 3421–3428. https://doi.org/10.1016/j.arth.2017.05.056 (2017).
Van Den Eeden, Y. & Van Den Eeden, F. Learning curve of direct anterior total hip arthroplasty: a single surgeon experience. Acta Orthop. Belg. 84(3), 321–330 (2018).
Bergin, P. F. et al. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J. Bone Jt. Surg. Am. 93, 1392 (2011).
Kwak, S., Chun, Y., Rhyu, K., Cha, J. & Cho, Y. Quantitative analysis of tissue injury after minimally invasive total hip arthroplasty. Clin. Orthop. Surg. 6, 27984 (2014).
Seagrave, K. G., Troelsen, A., Malchau, H., Husted, H. & Gromov, K. Acetabular cup position and risk of dislocation in primary total hip arthroplasty. Acta Orthop. 88(1), 10–17. https://doi.org/10.1080/17453674.2016.1251255 (2017).
Sarraj, M., Chen, A., Ekhtiari, S. & Rubinger, L. Traction table versus standard table total hip arthroplasty through the direct anterior approach: a systematic review. Hip Int. 6, 662–672. https://doi.org/10.1177/1120700019900987 (2020).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
N.R. and P.L. performed literature search and data extraction. S.B. and N.R. did the statistics. N.R. wrote the manuscript. N.R. created the tables. S.B. and N.R. created the figures. N.R. and D.D. checked the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramadanov, N., Bueschges, S., Lazaru, P. et al. A meta-analysis on RCTs of direct anterior and conventional approaches in total hip arthroplasty. Sci Rep 11, 20991 (2021). https://doi.org/10.1038/s41598-021-00405-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00405-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.