Abstract
Oxidative stress plays a role in the progression of chronic heart failure (CHF). We investigated whether systemic oxidative stress is linked to exercise intolerance and skeletal muscle abnormalities in patients with CHF. We recruited 30 males: 17 CHF patients, 13 healthy controls. All participants underwent blood testing, cardiopulmonary exercise testing, and magnetic resonance spectroscopy (MRS). The serum thiobarbituric acid reactive substances (TBARS; lipid peroxides) were significantly higher (5.1 ± 1.1 vs. 3.4 ± 0.7 μmol/L, p < 0.01) and the serum activities of superoxide dismutase (SOD), an antioxidant, were significantly lower (9.2 ± 7.1 vs. 29.4 ± 9.7 units/L, p < 0.01) in the CHF cohort versus the controls. The oxygen uptake (VO2) at both peak exercise and anaerobic threshold was significantly depressed in the CHF patients; the parameters of aerobic capacity were inversely correlated with serum TBARS and positively correlated with serum SOD activity. The phosphocreatine loss during plantar-flexion exercise and intramyocellular lipid content in the participants' leg muscle measured by 31phosphorus- and 1proton-MRS, respectively, were significantly elevated in the CHF patients, indicating abnormal intramuscular energy metabolism. Notably, the skeletal muscle abnormalities were related to the enhanced systemic oxidative stress. Our analyses revealed that systemic oxidative stress is related to lowered whole-body aerobic capacity and skeletal muscle dysfunction in CHF patients.
Similar content being viewed by others
Introduction
Exercise intolerance is a cardinal symptom of chronic heart failure (CHF), leading to increased morbidity and mortality as well as a poor quality of life1. Reduced whole-body aerobic capacity in particular, characterized by a lower peak oxygen uptake (peak VO2) and lower VO2 at anaerobic threshold (AT VO2), is known as an independent predictor of all-cause mortality in CHF patients2,3. Among the various contributors to exercise tolerance, skeletal muscle function is a major determinant of the whole-body aerobic capacity as the skeletal muscles are the largest energy production sites during exercise. We and others have shown that abnormal skeletal muscle energy metabolism is responsible for the exercise intolerance in patients with CHF4,5,6.
Oxidative stress is generally caused by an imbalance between the production of reactive oxygen species (ROS) and the antioxidant defense capacity. Systemic oxidative stress has been shown to have prognostic value and is associated with heart failure (HF)-related symptoms evaluated by the New York Heart Association (NYHA) functional class in CHF patients7,8,9. However, the NYHA functional class is a subjective estimation of a patient's functional ability, and it is thus necessary to determine the roles and effects of systemic oxidative stress with a more objective estimation of functional capacity.
We conducted the present study to determine whether systemic oxidative stress evaluated by serum lipid peroxidation products and the antioxidant defense capacity is associated with lower whole-body aerobic capacity and with impaired skeletal muscle energy metabolism in patients with CHF.
Results
Patient characteristics
The baseline characteristics of the CHF and control groups are summarized in Table 1. There were no significant differences in age or any anthropometric parameters between the CHF and control groups. Of the 17 patients with CHF, 13 patients had dilated cardiomyopathy and four patients had other heart diseases including valvular heart disease and hypertensive heart disease. The rate of NYHA functional classes I, II, and III in the CHF group were 24%, 41%, and 35%, respectively. The fasting blood glucose, plasma insulin, homeostasis assessment model of insulin resistance (HOMA-IR), glycated hemoglobin (HbA1c), low-density lipoprotein (LDL)-cholesterol, triglycerides, and free fatty acids were similar between the CHF and control groups. The high-density lipoprotein (HDL)-cholesterol level was significantly lower in the CHF group compared to the control group. The peak VO2 and the AT VO2 were significantly decreased in the CHF group compared to the control group, indicating lower whole-body aerobic capacity in the CHF patients.
Systemic oxidative stress
The CHF patients' serum levels of thiobarbituric acid reactive substances (TBARS) were significantly higher (5.1 ± 1.1 vs. 3.4 ± 0.7 μmol/L, p < 0.01) (Fig. 1A) and their serum superoxide dismutase (SOD) activity was significantly lower compared to the control group (9.2 ± 7.1 vs. 29.4 ± 9.7 units/L, p < 0.01) (Fig. 1B), indicating both increased lipid peroxidation products and reduced antioxidant capacity in the CHF patients.
Systemic oxidative stress. (A) Serum TBARS (lipid peroxides) and (B) serum SOD activity (an antioxidant defense capacity). White bars: Control subjects (n = 13). Black bars: CHF patients (n = 17). Data are mean ± SD. *p < 0.01 vs. Control. SOD: superoxide dismutase, TBARS: thiobarbituric reactive substances.
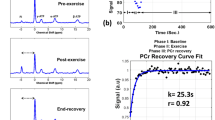
Skeletal muscle energy metabolism
The magnetic resonance spectroscopy (MRS) data are summarized in Table 2. The one repetition maximum (1-RM) of plantar-flexion exercise was significantly lower in the CHF group than the control group (40 ± 6 vs. 35 ± 6 kg, p = 0.02), and the workload (20% 1RM) of plantar-flexion exercise was set in each participant. In the 31phosphorus (31P)-MRS study, the standardized phosphocreatine at rest (PCrrest) in the calf muscle was comparable between the CHF and control groups. However, the standardized PCr level at the lowest during the plantar-flexion exercise (PCrlowest) was significantly reduced in the CHF group, and as a result, the muscle PCr loss during the exercise was significantly greater in the CHF cohort, indicating impaired intramuscular high-energy phosphate energy metabolism in the CHF patients. In the 1proton (1H)-MRS study, the intramyocellular lipid (IMCL) content in the resting leg muscle was significantly increased in the CHF cohort, indicating impaired fatty acid metabolism in the skeletal muscle of the CHF patients.
The association between systemic oxidative stress and whole-body aerobic capacity
The peak VO2 and the AT VO2 were inversely correlated with the serum TBARS level, whereas these two parameters were positively correlated with the serum SOD activity in the series of all participants (Fig. 2A,B), indicating that systemic oxidative stress is linked to reduced whole-body aerobic capacity. In addition, the peak VO2 was positively correlated with the serum SOD activity (r = 0.50, p = 0.04) in the CHF patients, but not with the patients' serum TBARS levels.
Linear relationship between systemic oxidative stress and whole-body aerobic capacity. (A) Systemic oxidative stress and peak VO2 and (B) systemic oxidative stress and AT VO2. White circles: Control subjects (n = 13). Black circles: CHF patients (n = 17). AT: anaerobic threshold, VO2: oxygen uptake.
The association between systemic oxidative stress and skeletal muscle energy metabolism
In the series of all participants, the muscle PCr loss during the plantar-flexion exercise had a positive correlation with the serum TBARS level and an inverse correlation with the serum SOD activity (Fig. 3A). The IMCL content also had a positive correlation with the serum TBARS level, although there was no significant correlation between the IMCL content and the serum SOD activity in the series of all participants (Fig. 3B).
Linear relationship between systemic oxidative stress and skeletal muscle energy metabolism. (A) Systemic oxidative stress and muscle PCr loss during the plantar-flexion exercise and (B) systemic oxidative stress and IMCL content. White circles: Control subjects (n = 13). Black circles: CHF patients (n = 17). IMCL: intramyocellular lipid, PCr: phosphocreatine.
Discussion
The results of our analyses demonstrated that CHF patients had higher serum TBARS and lower serum activities of SOD, indicating increased systemic oxidative stress in CHF. The whole-body aerobic capacity characterized by the peak VO2 and the AT VO2 was decreased, and the skeletal muscle energy metabolism evaluated by the muscle PCr loss during exercise and the IMCL content was impaired in the CHF patients. Notably, both the higher serum TBARS and the lower serum SOD activity were linked to either impaired maximal and submaximal aerobic capacity (i.e., lower peak VO2 and AT VO2) or impaired intramuscular high-energy phosphate metabolism (i.e., increased muscle PCr loss during exercise). In addition, the higher serum TBARS levels were linked to accumulated IMCL content in the leg muscle. This study is the first to reveal associations between systemic oxidative stress and both exercise intolerance and skeletal muscle abnormalities in patients with CHF.
Systemic oxidative stress is reported to play a crucial role in disease progression in patients with CHF8,10. Previous studies have shown that several circulating oxidative stress markers may predict adverse clinical events including all-cause death and hospitalization in CHF patients9,11. Because exercise intolerance is related to the morbidity and mortality of CHF patients, our present findings of associations of systemic oxidative stress with lowered whole-body aerobic capacity and impaired skeletal muscle energy metabolism may contribute to the understanding of the potential roles and effects of enhanced systemic oxidative stress in the progression of heart failure.
There are some possible mechanisms by which systemic oxidative stress is enhanced in CHF patients. First, excessive ROS production in a failing heart may increase the level of circulating free radicals. Clinical and experimental studies have demonstrated enhanced ROS production and oxidative stress in the failing heart12,13,14,15. The evidence of an increased number of ROS-loaded blood cells in the coronary sinus compared to that in the peripheral veins in patients with CHF suggests an increased rate of circulating blood cells exposed by myocardial ROS when they pass through the heart16. Indeed, we have observed that mitochondrial ROS in circulating blood cells were elevated in symptomatic CHF patients in relation to systemic oxidative stress10.
Second, skeletal muscles can be a source of ROS in CHF, which supports the hypothesis that increased myocellular ROS directly impair skeletal muscle energy metabolism. We and others have shown that HF-model rodents had enhanced mitochondrial oxidative stress in their skeletal muscle17,18. We also demonstrated that one-leg immobilization for 2 weeks induced excessive ROS production accompanied by impaired mitochondrial respiratory capacity in the immobilized leg muscles of humans19. Accordingly, physical inactivity as well as the intrinsic impairment of skeletal muscle function under the condition of CHF seems to contribute to greater ROS production in the skeletal muscles, leading to the enhanced systemic oxidative stress in CHF patients.
Finally, physical inactivity itself may reduce the body's systemic antioxidant defense capacity20. Although we did not evaluate the participants' daily physical activity in the present study, exercise intolerance can induce a poor quality of life with a reduction of physical activity, which may result in lowered serum SOD activity in CHF patients. Further studies are needed to clarify the mechanisms underlying the enhanced systemic oxidative stress in CHF patients.
We investigated skeletal muscle energy metabolism by using MRS, which is a well-validated and noninvasive method. We measured the PCr loss in the calf muscle during the plantar-flexion exercise with the constant load of 20% 1-RM to assess the intramuscular high-energy phosphate metabolism using 31P-MRS. The PCr is an important energy source and works as an energy buffer, because the PCr can be promptly converted into ATP to maintain the ATP at a constant level during exercise. Since exercise with the load of 20% 1-RM is low-intensity exercise without a decrease in muscle pH (i.e., aerobic exercise), our finding that the muscle PCr loss during the plantar-flexion exercise was increased in the CHF patients might indicate impaired muscle oxidative metabolism.
We also measured the IMCL content in the resting leg muscle by 1H-MRS. The IMCL content is commonly defined by an imbalance between the uptake of fatty acids into the muscle and the intramuscular fatty acid oxidation. In this study, the free fatty acid levels were comparable between the CHF patients and control subjects, and thus the accumulated IMCL in the CHF patients might be attributable mainly to the impaired fatty acid oxidation in the skeletal muscle.
Heart failure-related myopathy characterized by impaired skeletal muscle energy metabolism and altered muscle structure (e.g., muscle atrophy and muscle fiber type switch) is a major contributor to the exercise intolerance of CHF patients5,6,21. It has been shown that exercise training improves skeletal muscle function and augments systemic and intramuscular antioxidant capacity in patients with CHF22. Accordingly, exercise training may be beneficial for the restoration of the redox balance as well as the improvement of cardiorespiratory fitness in these patients.
There are some study limitations to consider. First, the number of participants was small (n = 30). Second, the correlations between systemic oxidative stress and exercise intolerance or impaired skeletal muscle energy metabolism were not significant except for the correlation between the serum SOD activity and peak VO2 when we analyzed only the data of the CHF patients. Because the range of parameters of exercise capacity and skeletal muscle energy metabolism within the CHF group was small, we could not detect a significant correlation. Third, we could not identify the causality of the relationships between systemic oxidative stress and exercise intolerance or skeletal muscle dysfunction. Further studies with larger numbers of participants are necessary to clarify the causal relationships among these parameters.
In summary, this study demonstrated for the first time that systemic oxidative stress was related to exercise intolerance and skeletal muscle abnormalities in patients with CHF. Our findings suggest that restoration of the redox balance is beneficial in the treatment of CHF.
Methods
Participants
Thirty male participants were recruited at Hokkaido University Hospital: 17 stable CHF patients who had a history of hospitalization due to worsening HF defined by the Framingham Criteria23 and 13 age-matched healthy subjects as a control group. We excluded patients who had difficulty performing maximal exercise due to a physical problem including orthopedic disease, stroke, severe pulmonary disease, and peripheral artery disease, and patients with diabetes or severe chronic kidney disease. Patients who had been assessed as being NYHA functional class IV were also excluded. The present report is part of an MRS study targeting lifestyle disorders and cardiovascular diseases, and thus some of the data used herein were obtained from the same patients whose data were published previously but in a different context4. The protocol was approved by the Medical Ethics Committee of Hokkaido University Hospital, and written informed consent was obtained from each participant before the study. All investigations conformed to the principles outlined in the Declaration of Helsinki.
Study protocol
The participants underwent blood tests for the analyses of blood biochemistry and systemic oxidative stress after a 10-h overnight fast, followed by clinical and anthropometric measurements, echocardiography, and a 1H-MRS study to measure the IMCL content in the resting leg muscle. The participants also underwent cardiopulmonary exercise testing (CPET) to assess their exercise capacity. On another day, a 31P-MRS study was conducted to assess the high-energy phosphate metabolism in the calf muscle during plantar-flexion exercise.
Blood testing
Fasting blood glucose, plasma insulin, HbA1c, HDL-cholesterol, LDL-cholesterol, triglyceride, and free fatty acids were measured in all participants, and the plasma levels of brain natriuretic peptide (BNP) were measured in only the CHF patients by routine in-house analyses. The HOMA-IR was calculated as described24. To assess systemic oxidative stress, we measured the serum TBARS and the enzymatic activity of SOD by conducting fluorometric analyses in all participants as described25.
Echocardiography
Cardiac function was evaluated by echocardiography in the CHF patients as described26. The left ventricular ejection fraction (LVEF) was measured from apical four- and two-chamber images using the biplane method of disks.
CPET
The participants performed cardiopulmonary exercise testing (CPET) using an upright bicycle ergometer (Aerobike 75XLII; Combi Wellness, Tokyo) with a ramp protocol (10–25 watts/min) as described27,28. A respiratory gas analysis was simultaneously performed with a breath-by-breath apparatus (Aeromonitor AE-300S; Minato Medical Science, Osaka, Japan). The peak VO2 was defined as the VO2 attained at the maximal point during symptom-limited incremental exercise (i.e., at the point of leveling-off despite the increased workload). The AT VO2 was determined by the V-slope method by at least two CPET experts.
The 31P-MRS study
Before the study, the 1-RM of plantar-flexion exercise, i.e., the maximal weight of exercise that can be done only once, was determined with the participant in the supine position as described4,28. After a ≥ 30-min rest, the high-energy phosphate metabolism in the calf muscle was measured during plantar flexion exercise in the supine position on the original apparatus equipped with a 1.5-T whole-body scanner system (Magnetom Vision VB33G, Siemens, Erlangen, Germany) using 31P-MRS as described4,28. The exercise protocol was a constant load of 20% 1-RM at the pace of 40 times/min for 4 min. Usually, immediately after the initiation of the plantar-flexion exercise, the PCr level in the calf muscle started to decrease and was finally stabilized within a few minutes. The PCr was standardized as [PCr] / ([PCr] + [Pi]) on the basis of the notion that [PCr] + [Pi] is constantly equal both at rest and during exercise, where [PCr] indicates the concentration of PCr and [Pi] indicates the concentration of inorganic phosphate (Pi). The degree of PCr change (i.e., the PCr loss) during exercise was calculated as PCr loss = standardized PCrrest − standardized PCrlowest.
The 1H-MRS study
We measured the IMCL content in the resting tibialis anterior muscle at the level of the muscle belly of the calf using 1H-MRS on a 1.5-T whole-body scanner system (Signa Horizon LX, GE Medical Systems, Milwaukee, WI) as described4,28.
Statistical analyses
Data are expressed as the mean ± standard deviation (SD) or n (%). We used Student's t-test for continuous variables and the χ2 test for categorical variables to compare the data between the CHF and control groups. We examined correlations by performing a linear regression analysis using Pearson's correlation coefficient. Statistical analyses were performed using GraphPad Prism ver. 8 (GraphPad Software, San Diego, CA), and significance was defined as p < 0.05.
References
Del Buono, M. G. et al. Exercise intolerance in patients with heart failure: JACC state-of-the-art review. J. Am. Coll. Cardiol. 73, 2209–2225 (2019).
Gitt, A. K. et al. Exercise anaerobic threshold and ventilatory efficiency identify heart failure patients for high risk of early death. Circulation 106, 3079–3084 (2002).
Mancini, D. M. et al. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation 83, 778–786 (1991).
Hirabayashi, K. et al. Intramyocellular lipid is increased in the skeletal muscle of patients with dilated cardiomyopathy with lowered exercise capacity. Int. J. Cardiol. 176, 1110–1112 (2014).
Mancini, D. M. et al. Contribution of intrinsic skeletal muscle changes to 31P NMR skeletal muscle metabolic abnormalities in patients with chronic heart failure. Circulation 80, 1338–1346 (1989).
Okita, K. et al. Skeletal muscle metabolism limits exercise capacity in patients with chronic heart failure. Circulation 98, 1886–1891 (1998).
Keith, M. et al. Increased oxidative stress in patients with congestive heart failure. J. Am. Coll. Cardiol. 31, 1352–1356 (1998).
Kobayashi, S. et al. Urinary 8-hydroxy-2’-deoxyguanosine reflects symptomatic status and severity of systolic dysfunction in patients with chronic heart failure. Eur. J. Heart Fail. 13, 29–36 (2011).
Tang, W. H. et al. Prognostic value and echocardiographic determinants of plasma myeloperoxidase levels in chronic heart failure. J. Am. Coll. Cardiol. 49, 2364–2370 (2007).
Shirakawa, R. et al. Mitochondrial reactive oxygen species generation in blood cells is associated with disease severity and exercise intolerance in heart failure patients. Sci. Rep. 9, 14709 (2019).
Tang, W. H. et al. Diminished antioxidant activity of high-density lipoprotein-associated proteins in systolic heart failure. Circ. Heart Fail. 4, 59–64 (2011).
Ide, T. et al. Direct evidence for increased hydroxyl radicals originating from superoxide in the failing myocardium. Circ. Res. 86, 152–157 (2000).
Inoue, T. et al. Time-dependent changes of myocardial and systemic oxidative stress are dissociated after myocardial infarction. Free Radic. Res. 43, 37–46 (2009).
Maack, C. et al. Oxygen free radical release in human failing myocardium is associated with increased activity of rac1-GTPase and represents a target for statin treatment. Circulation 108, 1567–1574 (2003).
Sam, F. et al. Increased reactive oxygen species production and functional alterations in antioxidant enzymes in human failing myocardium. J. Card. Fail. 11, 473–480 (2005).
Ijsselmuiden, A. J. et al. Circulating white blood cells and platelets amplify oxidative stress in heart failure. Nat. Clin. Pract. Cardiovasc. Med. 5, 811–820 (2008).
Seiler, M. et al. Skeletal muscle alterations are exacerbated in heart failure with reduced compared with preserved ejection fraction: Mediated by circulating cytokines?. Circ. Heart. Fail. 9, e003027 (2016).
Tsutsui, H. et al. Enhanced generation of reactive oxygen species in the limb skeletal muscles from a murine infarct model of heart failure. Circulation 104, 134–136 (2001).
Gram, M. et al. Skeletal muscle mitochondrial H2O2 emission increases with immobilization and decreases after aerobic training in young and older men. J. Physiol. 593, 4011–4027 (2015).
Bouzid, M. A., Hammouda, O., Matran, R., Robin, S. & Fabre, C. Influence of physical fitness on antioxidant activity and malondialdehyde level in healthy older adults. Appl. Physiol. Nutr. Metab. 40, 582–589 (2015).
Anker, S. D. et al. Wasting as independent risk factor for mortality in chronic heart failure. Lancet 349, 1050–1053 (1997).
Sties, S. W. et al. Influence of exercise on oxidative stress in patients with heart failure. Heart Fail. Rev. 23, 225–235 (2018).
McKee, P. A., Castelli, W. P., McNamara, P. M. & Kannel, W. B. The natural history of congestive heart failure: The Framingham study. N. Engl. J. Med. 285, 1441–1446 (1971).
Matthews, D. R. et al. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Yokota, T. et al. Systemic oxidative stress is associated with lower aerobic capacity and impaired skeletal muscle energy metabolism in patients with metabolic syndrome. Diabetes Care 36, 1341–1346 (2013).
Tsujinaga, S. et al. Diastolic intra-left ventricular pressure difference during exercise: Strong determinant and predictor of exercise capacity in patients with heart cailure. J. Card. Fail. 25, 268–277 (2019).
Abe, T. et al. Type 2 diabetes is an independent predictor of lowered peak aerobic capacity in heart failure patients with non-reduced or reduced left ventricular ejection fraction. Cardiovasc. Diabetol. 19, 142 (2020).
Yokota, T. et al. Lower aerobic capacity was associated with abnormal intramuscular energetics in patients with metabolic syndrome. Hypertens. Res. 34, 1029–1034 (2011).
Acknowledgements
This study was partly supported by grants from the Center of Innovation Program from the Japan Science and Technology Agency (JPMJCE1301 to T.Y.) and KAKENHI Grants-in-Aid for Scientific Research (18K08022 to T.Y.). We thank Masashi Omokawa (Hokusho University, Ebetsu, Japan), Kuniaki Harada (Sapporo Medical University, Sapporo, Japan), Masaaki Hattori (Tokai University, Sapporo, Japan), and Yoshinao Nakagawa (Otaru University, Otaru, Japan) for their technical assistance in the MRS study.
Author information
Authors and Affiliations
Contributions
T.Y., S.K., K.H., K.O., and H.T. contributed to the conception and design of the work. T.Y., K.H., M.Y., S.T., T.S., and S.M. researched data and contributed to the discussion. I.N. analyzed data and contributed to the discussion. T.Y. wrote the manuscript. S.K., A.F., K.O., and H.T. contributed to the discussion and reviewed/edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yokota, T., Kinugawa, S., Hirabayashi, K. et al. Systemic oxidative stress is associated with lower aerobic capacity and impaired skeletal muscle energy metabolism in heart failure patients. Sci Rep 11, 2272 (2021). https://doi.org/10.1038/s41598-021-81736-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-81736-0
This article is cited by
-
Are sarcopenia and its individual components linked to all-cause mortality in heart failure? A systematic review and meta-analysis
Clinical Research in Cardiology (2023)
-
The treatment of chronic anemia in heart failure: a global approach
Clinical Research in Cardiology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.