Abstract
Maternal periconceptional folic acid supplementation (FAS) has been documented to be associated with decreased risk of nonsyndromic oral clefts (NsOC). However, the results remain inconclusive. In this population-based case–control study of 807 singletons affected by NsOC and 8070 healthy neonates who were born between October 2010 and September 2015 in Chengdu, China, we examined the association of maternal FAS with the risk of nonsyndromic cleft lip with or without cleft palate (NsCL/P), and cleft palate (NsCP). Unconditional logistic regression analysis was used to estimate the crude and adjusted odds ratios (ORs) and 95% confidential intervals (CI). Significant associations were found between maternal periconceptional FAS and decreased risk of NsCL/P (aOR = 0.41, 95% CI 0.33–0.51). This protective effect was also detected for NsCL (aOR = 0.42, 95% CI 0.30–0.58) and NsCLP (aOR = 0.41, 95% CI 0.31–0.54). Both maternal FAS started before and after the last menstrual period (LMP) were inversely associated with NsCL/P (before LMP, aOR = 0.43, 95% CI 0.33–0.56; after LMP, aOR = 0.41, 95% CI 0.33–0.51). The association between NsCP and maternal FAS initiating before LMP was also found (aOR = 0.52, 95% CI 0.30–0.90). The findings suggest that maternal periconceptional FAS can reduce the risk of each subtype of NsCL/P in offspring, while the potential effect on NsCP needs further investigations.
Similar content being viewed by others
Introduction
Oral clefts (OC), resulting from the incomplete fusion of primary palate and/or secondary palate during the 7th to 10th week of pregnancy, usually include syndromic or nonsyndromic cleft lip with or without cleft palate (CL/P) and cleft palate (CP)1. Depending on geographic regions and races, oral clefts affect 1 in 500 to 2500 births1. The nonsyndromic clefts (NsOC) are one of most common birth defects in China2. The reported prevalence of NsOC can be as high as 1.8/1000 in some provinces of China, causing huge disease burden on family and society2,3,4.
Maternal folic acid supplementation (FAS) before and during early pregnancy is a well-established prevention approach for neural tube defects (NTDs). As facial mesenchyme is derived from neural crest, the protective effect of maternal FAS on oral clefts has been studied in various populations, but the findings are inconclusive5,6,7,8. Most observational studies conducted in Europe9,10,11,12,13,14, America15,16,17, and Asia18,19,20,21, have shown that maternal FAS during early pregnancy is associated with decreased risk of nonsyndromic CL/P (NsCL/P), while other investigations in these areas did not22,23,24,25,26,27. Some of them revealed a preventive effect for nonsyndromic cleft palate (NsCP)9,13,14,15, whereas a few studies suggested maternal FAS or multivitamin intake as risk factor of NsCL/P and NsCP28. Though two recent meta-analyses support the potential preventive effect of maternal FAS against NsCL/P and NsCP7,8, the currently available evidence is insufficient and conflicting, particularly for some cleft subtypes29,30,,30. In fact, population-based evidence from China is relatively scarce. With the exception of one cohort in three provinces18, a population-based case–control study in Shenyang city21, and a propensity-matched study in Shaanxi province26, almost all the observational studies in China have been hospital-based31,32,33,34,35.
Chengdu, the capital of Sichuan province, is a megacity located in the southwest of China where the prevalence of OCs is higher than the national average3. Following the Guide of National Folic Acid Supplementation Program2, Chengdu has provided free folic acid alone (400 μg/day) for women of childbearing age who reside in the area with a plan to be pregnant since 2010. The information regarding maternal folic use, prenatal exposures, perinatal health care and birth outcomes are prospectively collected by the Chengdu Maternal and Infant Health Surveillance system (CMIHS). These data allowed us to examine additional effect of maternal FAS on NsOC subtypes by performing a population-based case–control study.
Results
General characteristics of the study subjects
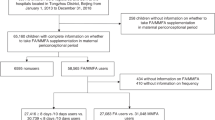
During October 2010 to September 2015, a total of 807 singletons with nonsyndromic clefts from CMIHS were available for the current analysis, including 247 NsCLs, 369 NsCLPs, and 191 NsCPs. Table 1 shows the maternal and infantile characteristics of the cases and 8070 controls. Compared with the control mothers, more NsCL/P mothers were under the age of 25 years or older than 35 years of age at the time of delivery. NsCL/P mothers were less educated (≤ 9 years), or more overweighted (BMI ≥ 24.0) than control mothers. Much more NsCL/P mothers exposed to environmental risks. Male predominance in NsCL/P and female excess in NsCP were identified. No significant difference was found between cases and controls regarding the distribution of parity, and maternal medical conditions in the first trimester.
Maternal periconceptional FAS
As shown in Table 2, about 91% of control mothers and 81% case mothers had FAS during periconceptional period. More NsCL/Ps and NsCPs mothers did not take FA than control mothers (20.6%, 12.5% vs 9.2%). Among mothers who had FAS, 23.7% of control mothers, 21.3% of NsCL/Ps mothers, and 17.3% of NsCPs mothers initiated FAS before LMP. In addition, pregnant women greater than 35 years of age, with lower education level, or with BMI ≥ 24.0, were more likely not to have FAS.
Association of maternal FAS and NsOC
As shown in Table 3, the crude odds ratio of maternal periconceptional FAS for NsCL/P was 0.39 (95% CI 0.32–0.48), and the adjusted OR was 0.41 (95% CI 0.33–0.51). Further stratification analysis showed that the associations remained significant for NsCL (aOR = 0.42, 95% CI 0.30–0.58) and NsCLP (aOR = 0.41, 95% CI 0.31–0.54). When analyzing according to the initiating time of maternal FAS, both maternal preconception and post-conception use could reduce the risks of NsCL/P and the subtypes (Table 3). Notably, maternal preconception FAS appeared to lower the risk of NsCP (aOR = 0.52, 95% CI 0.30–0.90). But the association between maternal periconceptional FAS and NsCP was nonsignificant. Several known risk factors such as advanced maternal age, higher maternal BMI, living in rural areas, exposure to environmental risks, nulliparity and male infants were positively associated with NsCL/P. Females were identified as risk factors of NsCP (Supplementary Table 1).
Discussion
In this population-based case–control study, we demonstrated that maternal periconceptional FAS was associated with a reduced risk of overall NsCL/P, and the reduced risk varied by cleft subtype and supplementation initiation timing. We did not identify the preventive effect of periconceptional FAS for NsCP, whereas we observed a significant association between maternal FAS started before LMP and NsCP, suggesting that earlier or longer supplementation may be protective.
Consistent with most previous studies in some western9,10,11,12,13,14,15,16,17,36 and Asian non-Chinese populations19,20, our results showed that maternal periconceptional FAS could reduce the risk of overall NsCL/P by approximately 60% regardless of the initiation timing. This preventive effect was observed for both NsCL and NsCLP. Similar associations have been noted in several epidemiological studies in China18,30,31,32,33,34. These investigations were hospital-based and mainly focused on the environmental risk factors rather than the effect of supplementation. So far, only one cohort study specifically evaluated the preventive effect of maternal FAS on oral clefts in China, and found that in the north of China maternal supplementation started before the LMP reduced the risk of NsCL/P (NsCL/P, aRR = 0.69, 95% CI 0.55–0.87; NsCL, aRR = 0.26, 95% CI 0.07–0.98; NsCLP, aRR = 0.19, 95% CI 0.07–0.50), while such effect was neither observed in the south of China nor for supplementation started on or after the LMP18,31,32,33,34,35. Another population-based case–control study in Shaanxi province reported a preventive effect of optimal FAS for overall birth defects (OR = 0.71, 95% CI 0.57–0.89), but not for oral clefts26. The authors thought that differences in study design, supplementation initiation timing and small sample size could explain differences studies18,26. A recent meta-analysis revealed the preventive effect of maternal FAS in early pregnancy against NsCL/P and NsCP, and identified publication bias in previously published researches7. However, another systematic review seemed not to support the preventive effect of daily FAS on oral clefts30. It can be seen that inconsistences among various studies are obvious. In fact, there is still a lack of reliable evidence on the preventive effect of folic acid on oral clefts, especially on the dose and initiation timing of supplementation.
Nonsyndromic cleft palate has been regarded as a distinct condition from NsCL/P on embryologic origin and etiology. As noted in several previous investigation6,11,18,21,31, this study found a negative but nonsignificant association of maternal periconceptional FAS with NsCP. Interestingly, maternal FAS starting before LMP was significantly associated with decreased risk of NsCP, suggesting that earlier use may work or supplementation initiation timing may play a part. A few studies reported the preventive effect of FAS on NsCP7,32. Compared with NsCL/P, researches on FAS and NsCP produced more conflicting results. A cohort study in Norway reported an adjusted RR of 0.84 (95% CI 0.66–1.06) for maternal use of Vitamins/folic acid and NsCP, and a stronger association (RR = 0.63, 95% CI 0.45–0.88) for cleft palate in combination with other malformations24. On the contrary, a case–control study conducted in Northern Netherlands27 and another cohort study28 in Japan identified maternal FAS/multivitamin supplement use during the first trimester as a risk factor of NsCP. Whether the preventive effect of maternal FAS against NsCP can be observed in a certain population depends on various factors, including genetic background, maternal dietary folic acid intake, serum folate level and the compliance with FAS, etc. Considering the small number of NsCP cases in our analysis, the findings about maternal FAS and NsCP need to be further studied. These controversial results may be due to the heterogeneities in research design, population, sample size, exposure assessment, and other potential confounders7,18,21,31,32,33,34,35. Overall, more prospective studies are needed to elucidate the relationship between maternal FAS and NsCP.
Several strengths and limitations should be considered when interpreting our study results. The population-based nature and large sample size of Chinese cleft cases of the study ensure robust OR estimates for NsCL/P subtypes. In addition, the prospectively collected exposure data could minimize recall bias. When calculating the OR estimates for NsCP, there were potential bias due to low detection rate of syndromic CP but it could be minimal. Though information of maternal dietary and multivitamin intake was not available for analysis, the associations are less likely to be distorted because the OR estimates were based on randomly selected control data with adjustment for known risk factors such as maternal illness, social factors, environmental exposures, and maternal illness.
In conclusion, our study provides additional evidence that maternal FAS during periconceptional period can reduce the risk of NsCL/P. Larger-sample-size studies are warranted to elucidate the association with NsCP and to determine whether women can benefit more from supplementation starting before LMP. It is of paramount importance for women of childbearing age to become aware of that maternal FAS can not only reduce the risk of NTD, but also reduce the risk of NsCL/P.
Methods
Data source and study subjects
Data for this study were abstracted from the CMIHS. According to the “Maternal and Infant Health Care Protocol of Sichuan Province”37, every pregnant woman was required to have at least five prenatal medical examinations during her pregnancy and three postnatal clinical visits (on the 7th, 28th and 42nd day after delivery). The results of examinations or visits, risk factors (maternal diseases, family history, other medical conditions), and pregnancy outcomes (spontaneous abortion, stillbirth, live birth, birth defects, etc.), were recorded in the CMIHS system. The medical examination, data collecting, checking and auditing were performed by well-trained obstetricians and nurses. CMIHS adopted the diagnosis criterions, case ascertainment, quality assurance, data collection and encoding of birth defects proposed by Chinese Birth Defects Monitoring Network (CBDMN)38. In detail, nonsyndromic clefting referred a cleft case without any non-cleft malformations, while the syndromic cleft was defined as a case occurred in association with other congenital anomalies. The diagnosis was made by at least one obstetrician or pediatrician, and confirmed by a senior doctor at the hospital level. Following the CBDMN guide, the diagnosis was finally coded by CMIHS stuff according to International Classification of Diseases, Tenth Revision. Prenatally diagnosed cases must be rechecked and confirmed after birth. Between October 2010 and September 2015, 807 singletons with NsOCs were included in as the cases, for each case ten controls were randomly selected from the healthy singletons born in the same period.
Folic acid intake and covariates
Briefly, women who joined in the prevention program were followed once a month by local community healthcare workers, and their registration dates, last menstrual period (LMP), dates of starting and ending use, and the information of folic acid supplementation (folic acid alone) were recorded. In the CMIHS system, a woman’s FAS information was linked to her medical records once she had her first prenatal exam in any of the local hospitals.
In this study, pregnant women who regularly took folic acid (400 μg/day) during the periconceptional period for at least 1 month were defined as “periconception users”. Of them, those who started intake before their LMP were termed as “preconception users”, while those who started on or after their LMP were named as “post-conception users”. On the contrary, pregnant women who did not have folic acid intake, or took it continuously less than 1 month were considered as “non-users”. Other variables included maternal age, nationality, education, residence, parity, medical condition and environmental exposures in the first trimester. Specifically, the maternal medical condition referred to any of such conditions as positive result of syphilis, human immunodeficiency virus and hepatitis B virus testing, anemia, chronic kidney, liver and heart diseases, diabetes (type I or II), primary hypertension disorders. The environmental exposure was an indicator (yes or no) to show whether the mothers had smoking, alcohol drinking, drug abuse, or exposure to radiation and hazardous substances. The variables of infants included gestational age, date of birth, birth weight, sex, birth defects and infant outcomes. Data used in this study were extracted anonymously, with a few variables as identifiers (e.g. date of birth). This research was approved by the Ethics Committee of West China Second University Hospital, Sichuan University. All methods were performed in accordance with relevant regulations and the individual informed consent was waived.
Statistical analyses
Differences in maternal and infant characteristics between cases and controls were examined with Pearson chi-square tests for categorical variables. Non-conditional logistic regression analysis was used to calculate the crude and adjusted odds ratios (ORs) and 95% confidence intervals (CI). Statistical analyses were performed with R 3.5.3 (R Development Core Team 2019) and packages “rms”.
References
Mossey, P. A. & Modell, B. Epidemiology of oral clefts 2012: An international perspective. Front. Oral Biol. 16, 1–18 (2012).
MOH. National stocktaking report on birth defect prevention (2012), (Ministry of Health, 2012).
Wang, M. et al. Prevalence of orofacial clefts among live births in China: A systematic review and meta-analysis. Birth Defects Res. 109, 1011–1019 (2017).
Dai, L. et al. Time trends in oral clefts in Chinese newborns: Data from the Chinese National Birth Defects Monitoring Network. Birth Defects Res. A Clin. Mol. Teratol. 88, 41–47 (2010).
Tolarova, M. Periconceptional supplementation with vitamins and folic acid to prevent recurrence of cleft lip. Lancet 2, 217 (1982).
Millacura, N., Pardo, R., Cifuentes, L. & Suazo, J. Effects of folic acid fortification on orofacial clefts prevalence: A meta-analysis. Public Health Nutr. 20, 2260–2268 (2017).
Jahanbin, A., Shadkam, E., Miri, H. H., Shirazi, A. S. & Abtahi, M. Maternal folic acid supplementation and the risk of oral clefts in offspring. J. Craniofac. Surg. 29, e534–e541 (2018).
Zhou, Y. et al. Folate intake, markers of folate status and oral clefts: An updated set of systematic reviews and meta-analyses. Birth Defects Res. 112, 1699–1719 (2020).
Czeizel, A. E. The primary prevention of birth defects: Multivitamins or folic acid?. Int. J. Med. Sci. 1, 50–61 (2004).
van Rooij, I. A. et al. Periconceptional folate intake by supplement and food reduces the risk of nonsyndromic cleft lip with or without cleft palate. Prev. Med. 39, 689–694 (2004).
Wilcox, A. J. et al. Folic acid supplements and risk of facial clefts: National population based case-control study. BMJ 334, 464 (2007).
Kelly, D., O’Dowd, T. & Reulbach, U. Use of folic acid supplements and risk of cleft lip and palate in infants: A population-based cohort study. Br. J. Gen. Pract. 62, e466-472 (2012).
Czeizel, A. E., Toth, M. & Rockenbauer, M. Population-based case control study of folic acid supplementation during pregnancy. Teratology 53, 345–351 (1996).
Chevrier, C. et al. Fetal and maternal MTHFR C677T genotype, maternal folate intake and the risk of nonsyndromic oral clefts. Am. J. Med. Genet. A 143A, 248–257 (2007).
Carmichael, S. L. et al. Reduced risks of neural tube defects and orofacial clefts with higher diet quality. Arch. Pediatr. Adolesc. Med. 166, 121–126 (2012).
Figueiredo, R. et al. The role of the folic acid to the prevention of orofacial cleft: An epidemiological study. Oral Dis. 21, 240–247 (2015).
Itikala, P. R., Watkins, M. L., Mulinare, J., Moore, C. A. & Liu, Y. Maternal multivitamin use and orofacial clefts in offspring. Teratology 63, 79–86 (2001).
Li, S. et al. Folic acid use and nonsyndromic orofacial clefts in China: A prospective cohort study. Epidemiology 23, 423–432 (2012).
Golalipour, M. J., Vakili, M. A. & Kaviani, N. Reduction in non syndromic oral clefts following mandatory flour fortification with folic acid in Northern Iran. Med. J. Islam Repub. Iran 28, 29 (2014).
Dien, V. H., McKinney, C. M., Pisek, A. & Pitiphat, W. Maternal exposures and risk of oral clefts in South Vietnam. Birth Defects Res. 110, 527–537 (2018).
Wang, W., Guan, P., Xu, W. & Zhou, B. Risk factors for oral clefts: A population-based case-control study in Shenyang, China. Paediatr. Perinat. Epidemiol. 23, 310–320 (2009).
Hashmi, S. S., Waller, D. K., Langlois, P., Canfield, M. & Hecht, J. T. Prevalence of nonsyndromic oral clefts in Texas: 1995–1999. Am. J. Med. Genet. A 134, 368–372 (2005).
Gildestad, T. et al. Maternal use of folic acid and multivitamin supplements and infant risk of birth defects in Norway, 1999–2013. Br. J. Nutr. 124, 316–329 (2020).
Gildestad, T. et al. Folic acid supplements and risk for oral clefts in the newborn: A population-based study. Br. J. Nutr. 114, 1456–1463 (2015).
Godwin, K. A. et al. Changes in frequencies of select congenital anomalies since the onset of folic acid fortification in a Canadian birth defect registry. Can. J. Public Health 99, 271–275 (2008).
Qu, P. et al. A propensity-matched study of the association between optimal folic acid supplementation and birth defects in Shaanxi province, Northwestern China. Sci. Rep. 9, 5271 (2019).
Rozendaal, A. M. et al. Periconceptional folic acid associated with an increased risk of oral clefts relative to non-folate related malformations in the Northern Netherlands: A population based case-control study. Eur. J. Epidemiol. 28, 875–887 (2013).
Yoshida, S., Takeuchi, M., Kawakami, C., Kawakami, K. & Ito, S. Maternal multivitamin intake and orofacial clefts in offspring: Japan Environment and Children’s Study (JECS) cohort study. BMJ Open 10, e035817 (2020).
Johnson, C. Y. & Little, J. Folate intake, markers of folate status and oral clefts: Is the evidence converging?. Int. J. Epidemiol. 37, 1041–1058 (2008).
De-Regil, L.M., Pena-Rosas, J.P., Fernandez-Gaxiola, A.C. & Rayco-Solon, P. Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst. Rev. CD007950 (2015).
Hao, Y. et al. Association of parental environmental exposures and supplementation intake with risk of nonsyndromic orofacial clefts: A case-control study in Heilongjiang Province, China. Nutrients 7, 7172–7184 (2015).
Jia, Z. L. et al. Maternal malnutrition, environmental exposure during pregnancy and the risk of non-syndromic orofacial clefts. Oral Dis. 17, 584–589 (2011).
Xu, D. P. et al. A study on environmental factors for nonsyndromic cleft lip and/or palate. J. Craniofac. Surg. 29, 364–367 (2018).
Xu, L. F. et al. A case-control study of environmental risk factors for nonsyndromic cleft of the lip and/or palate in Xuzhou, China. Biomed. Environ. Sci. 28, 535–538 (2015).
Lin, Y., Shu, S. & Tang, S. A case-control study of environmental exposures for nonsyndromic cleft of the lip and/or palate in eastern Guangdong, China. Int. J. Pediatr. Otorhinolaryngol. 78, 544–550 (2014).
Wehby, G. L. et al. High dosage folic acid supplementation, oral cleft recurrence and fetal growth. Int. J. Environ. Res. Public Health 10, 590–605 (2013).
Jie, P. U., Shujuan, Z. H. & Ping, Q. I. Survey on awareness and demand for preconception care of women in Chengdu. West China Med. J. 28, 1055–1058 (2013).
Zhu, P., Du, X. & Li, M. Prevalence of low birthweight and its influencing factors from 2008 to 2014 in Chengdu. Mod. Prev. Med. 44, 1428–1432 (2017).
Acknowledgements
This work was supported by the Grants from National Key R&D Program of China (2017YFC0907304) and National Natural Foundation of China (81072375).
Funding
This work was supported by the Grants from National Key R&D Program of China (2017YFC0907304), National Natural Foundation of China (81072375), and Ministry of Health.
Author information
Authors and Affiliations
Contributions
W.X. performed statistical work and drafted the manuscript. L.Y., C.D., Z.Z., L.R., Z.R., S.Z., T.Z. and G.Z. participated in the data collection and preparation. L.R. and G.Z. provided data access. H.L. and L.D. designed research plan and revised the manuscript. All authors had read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, W., Yi, L., Deng, C. et al. Maternal periconceptional folic acid supplementation reduced risks of non-syndromic oral clefts in offspring. Sci Rep 11, 12316 (2021). https://doi.org/10.1038/s41598-021-91825-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91825-9
This article is cited by
-
Genetics and orofacial clefts: a clinical perspective
British Dental Journal (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.